Standfirst
A recent study shows that a history of rotating night shift work and an unhealthy lifestyle are associated with increased T2D risk, both independently and synergistically. This is the first large-scale, prospective study to quantify how a healthy lifestyle may partially offset T2D risk in shift workers.
Refers to: Shan, Z et al. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses BMJ 2018; 363 doi: https://doi.org/10.1136/bmj.k4641
The prevalence of Type 2 Diabetes mellitus (T2DM) has reached epidemic proportions globally. Therefore, identifying modifiable risk factors is critical. Shift work, especially night shift work, is now recognized as a T2DM risk factor; however, shift work is and will remain necessary, especially in health-related and safety-related sectors. Therefore, two options for T2DM prevention emerge: first, identify and implement healthier work schedules, which is currently subject to research; second, develop strategies to limit the adverse effects on glucose regulation (and other health effects) of the shift work schedules. Lifestyle interventions, including promoting a healthy weight, diet, non-smoking and physical activity, are well-known and effective paths to mitigate T2DM risk, although compliance and overall effectiveness in shift workers remain a challenge1. Furthermore, evidence regarding the independent and joint effects of shift work and lifestyle factors is virtually nonexistent. Such insight is important to determine the most effective approaches to improving metabolic health.
Zhilei Shan and colleagues2 have now carefully investigated the relative contribution of lifestyle factors and history of rotating night shift work exposure to T2DM risk in the Nurses’ Health Study and the Nurses’ Health Study 2, which followed-up >140,000 female nurses across >20 years. The authors calculated an unhealthy lifestyle score based on BMI, physical activity, diet quality, and smoking status, by point summation. For example, individuals with a BMI ≥25kg/m2, <30 min per day of moderate to vigorous physical activity, diet quality in the lower three quintiles of the Alternate Healthy Eating Index, and who currently smoke, would obtain a score of 4. Rotating night shift work history was reported once at baseline in the Nurses’ Health Studies, when women were in their mid-fifties. In the Nurses’ Health Study 2, women were younger, and every few years updated their shift work status. Shan and colleagues demonstrate that shift work and unhealthy lifestyle are independent predictors of T2DM, with 31% increased T2DM risk for each 5-year period of rotating night shift work exposure and 2.8-fold increased T2DM risk for each unhealthy lifestyle factor. An additional 11% of T2DM cases were attributed to the joint effects of shift work and an unhealthy lifestyle, which was largely attributed to the lifestyle factors (71% of the joint effects). The authors conclude that this finding suggests that T2DM prevention efforts in rotating shift workers should focus on lifestyle.
When comparing the association between each of the four lifestyle factors in this study (BMI, smoking, diet quality and physical activity) with T2DM, it is clear that body weight plays a dominant role. Women who were overweight or obese had an 8-times higher risk of developing T2DM than women with a BMI of <25kg/m2. Compared to BMI, physical activity, diet quality, smoking, as well as history of shift work, were more moderate risk factors for T2DM (∼10–50% increased relative risk). It is noteworthy that risk estimates for T2DM reported for shift work in this study are probably underestimating the association, as they were based on cumulative lifetime shift work history, but did not require current shift work. Indeed, in the Nurses’ Health Study, most nurses might not have been working rotating night shifts even at baseline, which the author suggest as a reason for the lower risk estimates for T2DM in the Nurses’ Health Study when compared with Nurses’ Health Study 2, in which >21% of women were still working shift work schedules. This discrepancy is relevant because adverse health risks seem to decrease after stopping shift work. Furthermore, the analyses comprised of women who were free of T2DM at baseline, which is necessary when estimating disease incidence. The women who were excluded at baseline, however, might be the ones most vulnerable to the influence of shift work on their health (a phenomenon known as the healthy worker effect), and exclusion of them from analyses has likely contributed further to the underestimation of the true effects of shift work.
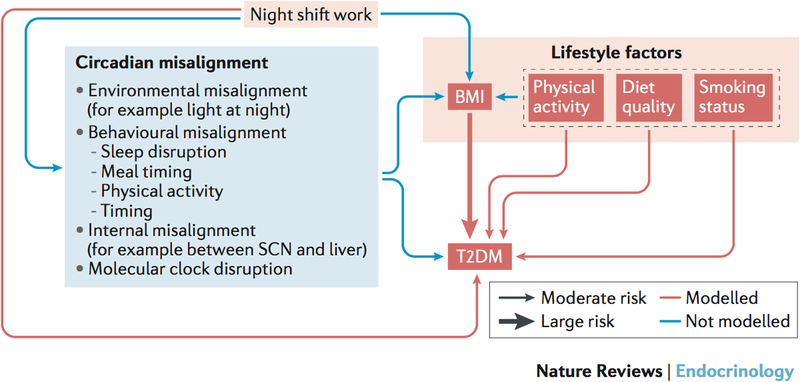
With BMI as dominating factor for T2DM risk among the unhealthy lifestyle factors, one question is whether or not it should be adjusted for when assessing the association between shift work and T2DM (adjustment for the other three lifestyle factors didn’t modify the shift work-T2D association). A substantial body of work has demonstrated that shift work itself is robustly associated with some measures of metabolic health, such as BMI, waist-to-hip ratio (WHR) and weight gain3, even after accounting for other established risk factors such as diet quality, calorie intake and physical activity. As such, body weight and overweight and/or obesity can be conceptualized as a (partial) mediator between shift work and T2D (Fig. 1).
Figure 1. Relationships between shift work, unhealthy lifestyle factors, and T2D.
Shan et al. show that a history of rotating night shifts moderately increases the risk of incident type 2 diabetes, with effect estimates of similar magnitude to that of each of three unhealthy lifestyle factors: lower physical activity, diet quality, and current smoking. By comparison, being overweight or obese was associated with a much larger relative risk for T2D, 8-fold higher compared to women who were lean (BMI≥25 vs. <25kg/m2). BMI is likely a (partial) mediator in the relationship between a history of shift work and T2D. Circadian misalignment, typical in night workers, is composed of environmental, behavioral, and internal misalignment, and can also result in molecular clock disruption. Circadian misalignment, including the consequential sleep disruption and mistimed meals, have been implicated in increased body mass as well as impaired glucose control, both risk factors for T2D. Note that other environmental, behavioral, social, and genetic risk factors are involved in this complex interaction. Abbreviations: SCN, suprachiasmatic nucleus; BMI, body mass index; T2DM, type 2 diabetes mellitus.
Mechanistic evidence from controlled laboratory studies has shown that circadian misalignment and sleep deprivation — which are typically experienced during shift work, especially when the schedule includes rotating night shifts (Fig. 1) — impair glucose metabolism, and are now considered emerging risk factors associated with T2DM risk4. Circadian and sleep disruption also might affect energy expenditure and increase energy intake, and is thereby a probable causal pathway from shift work to overweight and/or obesity, and thus to T2DM risk5,6 (Fig. 1). Some of the other factors captured in the unhealthy lifestyle score are also known to be influenced by circadian and sleep disruption. A 2018 pilot trial suggested that extending sleep duration in habitual short sleepers can reduce sugar, fat and carbohydrate intake.7 This result suggests that reduced sleep in shift workers might negatively affect diet quality and calorie intake. Furthermore, animal and human studies have shown that when we eat (both circadian time of food intake as well as fasting duration), in addition to what we eat, affects glucose control, weight regulation and long-term health outcomes8. For example, glucose tolerance, insulin sensitivity, pancreatic beta-cell function, and diet-induced thermogenesis are reduced in the biological evening compared to the biological morning.4 Links between shift work, as well as between circadian and sleep disruption, and smoking status and physical activity are less clear. However, shift work is expected to change the timing of physical activity and smoking, the former of which may affect glucose control. Taken together, Figure 1 illustrates the need for even more detailed analyses considering those existing and emerging inter-relationships, and can build on the important findings provided by Shan and colleagues2.
T2DM risk in the Nurses’ Health Study 2 has also been shown to be influenced by the interaction between history of rotating night shift work and chronotype (for example, early or late individual sleep timing, people in each category are sometimes referred to as larks or owls).9 Chronotype influences the extent of shift-specific sleep deprivation10, and thereby probably also secondarily lifestyle factors and their timing. Future studies exploring those inter-relationships might help to individually-tailor prevention and intervention strategies and thereby maximize interventions’ efficacy.
The inter-relationships between shift work, lifestyle, clock-regulated physiology, sleep behavior, and their effect on glucose control are clearly complex. The study by Shan and colleagues2 addresses this highly relevant topic, and provides first exciting results aiming at delineating these relationships. As our understanding of circadian biology advances, and is increasingly integrated with public health, translation medicine, and epidemiology (including the implementation of more formal assessment of circadian organization in those studies) our ability to quantify and track timing of environmental and behavioral risk factors, as well as consequential circadian disruption, are increasing. Incorporating timing of behaviors and exposures as an additional exposure dimension, in addition to quantity and quality, will allow us to maximize the potential of (timed) lifestyle and occupational interventions for health.
Acknowledgments
Competing interests
C.V. is a Nurses’ Health Studies investigator. F.A.J.L.S. has received speaker fees from Bayer HealthCare, Kellogg Company, Pfizer, Philips, Sentara Healthcare and Vanda Pharmaceuticals. F.A.J.L.S. and C.V. were supported in part by NIH grant R01DK105072; F.A.J.L.S. was also in part supported by NIH grants R01HL118601, R01DK099512, R01DK102696 and R01HL140574.
Footnotes
Quotes:
Shan and colleagues demonstrate that shift work and unhealthy lifestyle are independent predictors of T2DM
Future studies … might help to individually-tailor prevention and intervention strategies
References
- 1.Neil-Sztramko S, Pahwa M, Demers P & Gotay C Health-related interventions among night shift workers: a critical review of the literature. Scandinavian Journal of Work, Environment and Health 40, 543–556 (2014). [DOI] [PubMed] [Google Scholar]
- 2.Shan Z et al. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses. BMJ 363, doi: 10.1136/bmj.k4641 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Proper KI et al. The Relationship Between Shift Work and Metabolic Risk Factors. American Journal of Preventive Medicine 50, e147–e157, doi: 10.1016/j.amepre.2015.11.013 (2016). [DOI] [PubMed] [Google Scholar]
- 4.Jan Stenvers D, Scheer FAJL, Schrauwen P, la Fleur SE & Kalsbeek A Circadian clocks and insulin resistance. Nature Reviews Endocrinology, doi: 10.1038/s41574-018-0122-1 (2018). [DOI] [PubMed] [Google Scholar]
- 5.Broussard JL & Van Cauter E Disturbances of sleep and circadian rhythms: novel risk factors for obesity. Current Opinion in Endocrinology, Diabetes and Obesity 23, 353–359, doi: 10.1097/med.0000000000000276 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McHill AW & Wright KP Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obesity reviews : an official journal of the International Association for the Study of Obesity 18 Suppl 1, 15–24, doi: 10.1111/obr.12503 (2017). [DOI] [PubMed] [Google Scholar]
- 7.Al Khatib HK et al. Sleep extension is a feasible lifestyle intervention in free-living adults who are habitually short sleepers: a potential strategy for decreasing intake of free sugars? A randomized controlled pilot study. The American Journal of Clinical Nutrition 107, 43–53, doi: 10.1093/ajcn/nqx030 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattson MP et al. Meal frequency and timing in health and disease. Proceedings of the National Academy of Sciences of the United States of America 111, 16647–16653, doi: 10.1073/pnas.1413965111 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vetter C et al. Mismatch of Sleep and Work Timing and Risk of Type 2 Diabetes. Diabetes Care 38, 1707–1713, doi: 10.2337/dc15-0302 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vetter C Circadian disruption: What do we actually mean? The European journal of neuroscience, doi: 10.1111/ejn.14255 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]