ABSTRACT
Historically, neural tube defects (NTD) in Australia affected around 2 in every 1000 births; 42% higher for Aboriginal births. Following firm evidence of the protective effect of periconceptional folate, health promotion activities encouraged increased folate intake through diet and supplements and limited voluntary food fortification. A 30% reduction in NTD was observed in non-Aboriginal but not Aboriginal infants, widening the disparity between Aboriginal and non-Aboriginal rates. Mandatory flour fortification with folic acid in 2009, led to further reductions in overall NTD, and greater reduction among Aboriginal infants, such that rates in Aboriginal and non-Aboriginal infants were similar by 2010–2014. Elimination of this disparity will make a small but important contribution to the Australian government's Closing the Gap initiative to reduce disadvantage among Aboriginal people. Long-term, complete, high-quality surveillance data on NTD have been of great value in monitoring trends in and evaluation of public health interventions for NTD in Australia.
Keywords: neural tube defects, folic acid, Aboriginal, surveillance, health promotion, fortification, closing the gap
Neural tube defects
The embryonic neural tube is normally closed by the end of the sixth week after the last menstrual period. Neural tube defects (NTD) occur when closure of the neural tube is incomplete, resulting in serious brain (anencephaly, encephalocoele) and/or spinal anomalies (spina bifida). These anomalies can lead to fetal or perinatal death, and lifelong morbidity in survivors, including motor and sensory deficits, and bowel and bladder incontinence (1). Rates of NTD vary across the world, due to both variation in risk factors (such as socioeconomic status) and differences in surveillance measures (2). Because NTD are structural anomalies, they are detectable by ultrasound early in pregnancy and, in places where termination of pregnancy for fetal anomaly is permitted, many affected pregnancies are terminated. In order to measure the prevalence of NTD completely, it is therefore necessary to count NTD occurring in terminations of pregnancy as well as in live births and stillbirths (2). However, even with close to complete enumeration, rates in the 1980s and 1990s varied from 1.1 per 1000 births in mainland Europe and the USA and 1.58 per 1000 in Canada, to high rates in Ireland and the UK (2.4–3.8 per 1000) and China (4.8 per 1000) (1, 3–5).
Several cohort and case-control studies in the 1970s and 1980s reported a reduction in the risk of NTD with increased maternal folate intake in early pregnancy (6–9), and randomized controlled trials confirmed this observational evidence in the early 1990s (10, 11). A meta-analysis of the trials found that periconceptional folic acid supplementation prevented 79% of NTD (risk ratio 0.31; 95% CI: 0.17–0.64) (12).
NTD are multifactorial in origin, with contributions from both genetic and environmental factors. However, the genetic basis is not well understood, and questions remain concerning the mechanism by which folic acid prevents NTD. Maternal folate concentrations in most cases are not in the clinically deficient range, although there is an inverse relation between folate concentration and risk of NTD. Suboptimal folate may increase NTD risk in genetically susceptible individuals (13). Folate, a B vitamin, occurs naturally in vegetables (especially leafy greens), fruit and wholegrains and folic acid, the synthetic form, is used in supplements and fortified foods. Folate status can be measured through dietary questionnaires, estimating dietary intake of natural folate and synthetic folic acid. Dietary folate equivalents are used to account for the fact that natural folate is less bioavailable than folic acid. Blood folate concentrations can also be measured, using either chemiluminescent immunoassay or microbiological assay methods.
The preventive effects of folic acid have led to national policies and health promotion programs advocating that all women take periconceptional folic acid supplements (14). Because of the need to be folic-acid-sufficient so early in pregnancy and because many pregnancies are unplanned, consideration was also given to fortification of a staple food, such that all women would have increased folic acid regardless of pregnancy planning. Canada and the USA undertook mandatory fortification in 1996 and many others followed. Evaluation of these interventions have shown no effect of policy alone (14), limited effect of health promotion campaigns (15), and significant reductions in NTD following mandatory fortification (4, 16–18).
NTD in Australia
NTD affected around 2 per 1000 births prior to the 1990s in Australia, with the prevalence of around 1 per 1000 each for anencephaly and spina bifida (encephalocoeles are less common; 0.2 per 1000) (15). Following the publication of the randomized controlled trial evidence of prevention with folic acid, the Australian National Health and Medical Research Council (NHMRC) issued guidelines in 1994, advocating that all women planning a pregnancy take folic acid supplements periconceptionally, and that all women of childbearing age increase their intake of dietary folate (19). Health promotion programs were conducted, encouraging women to increase dietary intake of folate and take supplemental folic acid prior to pregnancy (20). Fortification of food with folic acid was not permitted in Australia at that time, but following an Expert Panel review of the evidence, voluntary fortification of certain foods was permitted in 1996. The uptake of voluntary fortification by industry was patchy, with mainly breakfast cereals being fortified (15). Evaluation of the effects of health promotion in Western Australia found increases in health professionals advising women to take folic acid supplements, sales of folic acid supplements increased, and by 2000, 30% of women reported taking periconceptional folic acid supplements (21). Over this period of health promotion and voluntary fortification, the overall rates of NTD fell by 30%, from around 2 per 1000 births to 1.5 per 1000. The rate fell to a similar degree for anencephaly, spina bifida, and encephalocoeles (15). However, periconceptional folic acid supplement use was much more common among women who were older, had planned their pregnancies, did not smoke, and engaged in other health-promoting activities. There were no such associations with the reported intake of voluntarily fortified foods, but very few women ate these fortified foods (21).
NTD in Australian Aboriginal people
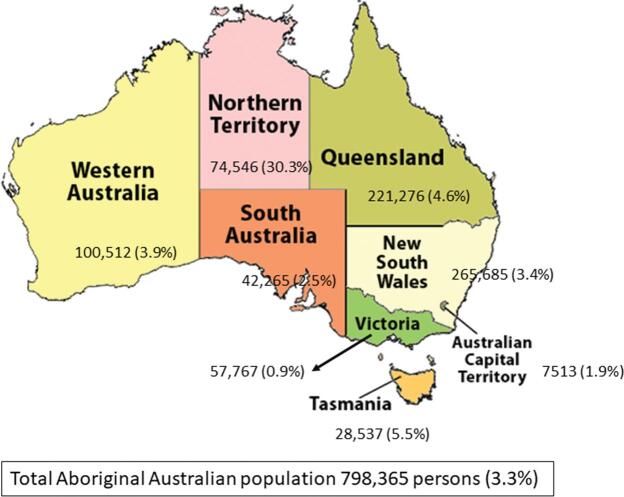
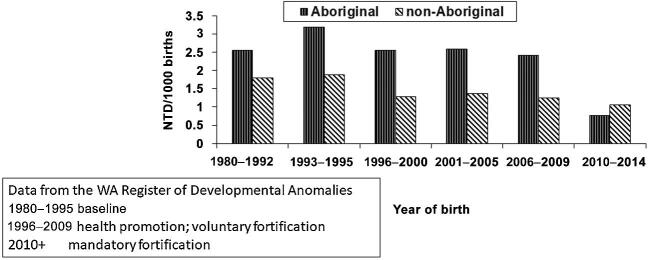
Around 3% of the Australian population identifies as Aboriginal or Torres Strait Islander (Figure 1). In this article, we use the term Aboriginal to cover both Aboriginal and Torres Strait Islander. A study reported in 1978 found a higher rate of NTD among part-Aboriginal children (3.35 per 1000; compared with 2.01 per 1000 for all births, 1965–1973) in the state of New South Wales (22) and a study from Western Australia, based on births 1980–1987, reported 2.68 NTD per 1000 births for Aboriginal infants and 1.87 per 1000 for non-Aboriginal infants (23). In both these studies, spina bifida occurred more commonly than anencephaly, and encephalocoeles were more frequently seen than in non-Aboriginal infants. Over the period of health promotion and voluntary fortification in Australia, the overall prevalence of NTD fell by 30%, based on data from Western Australia, but no fall in NTD prevalence was observed among Aboriginal infants (15, 24). Thus, the disparity between Aboriginal and non-Aboriginal rates of NTD widened – from a 42% difference prior to health promotion and voluntary fortification, to an almost 2-fold difference by 2005 (Figure 2).
FIGURE 1.
Aboriginal population by Australian state and territory: number of persons (% of state/territory population).
FIGURE 2.
Neural tube defects in Aboriginal and non-Aboriginal infants by grouped years of birth, Western Australia 1980–2005.
Clearly, the NHMRC policy, health promotion activities, and voluntary fortification were not working for Aboriginal populations. There were several potential reasons for this – the promotional messages to take folic acid supplements periconceptionally may not have been culturally appropriate, the cost may have been a barrier, and there may have been a high level of unplanned pregnancy. Also, the few voluntarily fortified foods available may not have been consumed by Aboriginal women of childbearing age. Furthermore, low folate status has been reported among Aboriginal people (25) and dietary intake of fruits and vegetables is lower in Aboriginal compared with non-Aboriginal people (26, 27).
Mandatory fortification with folic acid in Australia
Following several reviews, reports, and draft and final assessments, mandatory fortification of wheat flour for breadmaking with folic acid in Australia was agreed in 2007. There was a 2-y transition period, with folic acid fortification coming into effect in September 2009 (28). The need for increased folic acid being required so early in pregnancy and the fact that so many pregnancies are unplanned (around 40%), plus the observed limited effect of health promotion and voluntary fortification in reducing NTD, argued for mandatory fortification. The increasing gap between Aboriginal and non-Aboriginal rates of NTD was a major contributor to the decision to mandate fortification.
The requirement is for 200–300 µg folic acid to be added per 100 g wheat breadmaking flour. Organic wheat flour is exempt, and voluntary fortification was permitted to continue (except for flour). This public health intervention was expected to prevent ≤ 20% more NTD (29).
Evaluation of the effect of fortification in the Aboriginal population
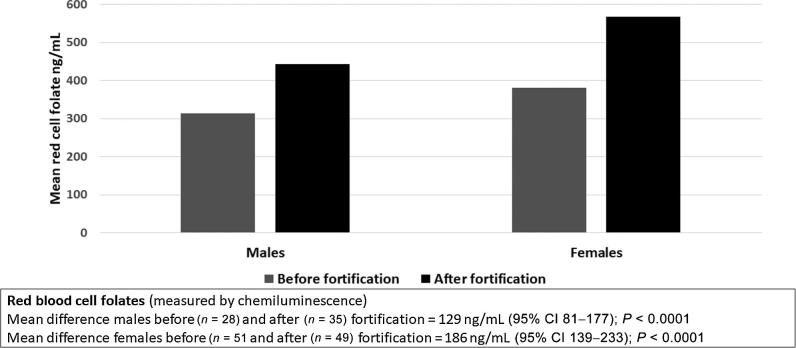
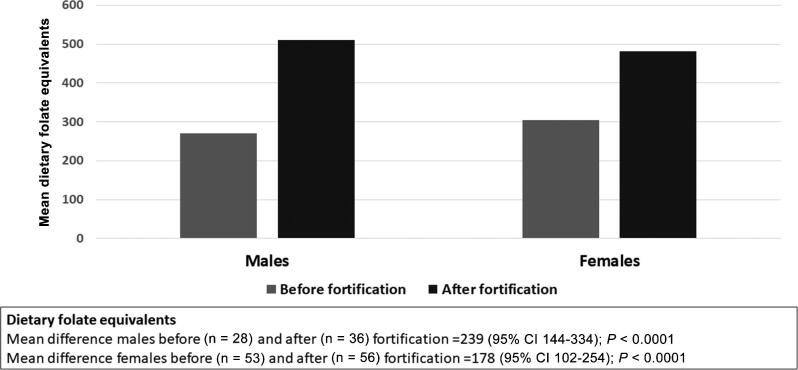
A research project in Western Australia estimated folate status among Aboriginal people before and after mandatory fortification with folic acid (30, 31). A rapid dietary assessment tool (32), adapted for use with Aboriginal people was used to estimate dietary folate intake, and a nonfasting sample of blood was taken to measure red blood cell folate. In summary, before mandatory fortification, estimated mean dietary folate equivalents (DFE) were 300 in women and 285 in men, and 10% of women and 26% of men had red blood cell folate deficiency (<250 ng/mL). Two years after fortification, there was a significant increase in DFE and in red blood cell folate for both men and women, and no participant in the study had a red blood cell folate estimate in the deficient range (Figures 3 and 4). Postfortification, mean red blood cell folate increased by 49% in women and 41% in men (31).
FIGURE 3.
Mean red blood cell folate before and after fortification; Aboriginal men and women aged 16–44 y, Western Australia (31).
FIGURE 4.
Mean dietary folate equivalents before and after fortification; Aboriginal men and women aged 16–44 y, Western Australia (31).
Importantly, there had been no change in vitamin supplement use (<7% before and after fortification), and there was continued high reported consumption of shop-bought bread (about half the men and women ate shop-bought bread daily and the majority ate it at least weekly). Women and men in the postfortification sample were estimated to have consumed 145 and 178 DFE daily, respectively, from fortified bread (31).
Using data from the Western Australian Register of Developmental Anomalies (33), and building on the prevalence estimates for 1980–2005, shown in Figure 1, the NTD prevalence in 2006–2009 (before mandatory fortification) for Aboriginal infants was 2.42 per 1000 (and 1.24 per 1000 for non-Aboriginal infants), still an almost 2-fold greater prevalence for Aboriginal infants. Postfortification (2010–2014), the NTD prevalence was 0.76 per 1000 for Aboriginal and 1.05 per 1000 for non-Aboriginal infants; a 68% reduction in Aboriginal NTD prevalence 15% decrease in non-Aboriginal NTD prevalence, resulting in a disappearance of the disparity (31).
Based on these findings, it was considered reasonable to assume that folic acid fortification of bread flour was responsible for the increases in folate status in Aboriginal people and for the reduction in NTD prevalence in both the Aboriginal and non-Aboriginal populations (31).
In 2016, similar findings were published using combined data from Western Australia and 4 other Australian states and territories (South Australia, Northern Territory, Queensland, New South Wales) (34). A 14.4% overall reduction in NTD prevalence was observed comparing these 2 time periods and, restricting the analysis to Aboriginal births, there was a reduction in NTD of 74%, again eliminating the gap between the Aboriginal and non-Aboriginal NTD prevalence.
Discussion
The public health intervention of mandatory fortification of wheat flour for breadmaking in Australia has been successful in achieving its aim of reducing NTD, and to the extent expected from the modeling conducted prior to its implementation (29). This intervention has been even more effective among Aboriginal children, for whom the prevalence of NTD was already higher, and who were more likely to be born with spina bifida or encephalocoele (15), conditions associated with lifelong disability.
However, because of the relatively small size of the Aboriginal population and its wide distribution across the country, their increased risk of NTD had not been widely recognized. This emphasizes the value and importance of population surveillance systems with complete ascertainment of cases over many years, as occurs in the Western Australian Register of Developmental Anomalies. Data from this register were also able to demonstrate the effectiveness of health promotion campaigns and voluntary fortification in reducing the overall prevalence of NTD and the absence of an effect on the prevalence among Aboriginal infants (24), and these findings were crucial in consideration of mandatory fortification in Australia.
Closing the gap
Aboriginal people in Australia have generally much poorer health and other outcomes and earlier mortality than non-Aboriginal Australians and this disparity has led to an initiative known as Closing the Gap. This initiative is an Australian government strategy, begun in 2009 (35, 36), that aims to reduce disadvantage among Aboriginal and Torres Strait Islander people with respect to life expectancy, child mortality, access to early childhood education, educational achievement, and employment outcomes. It is a formal commitment made by all Australian governments to achieve Aboriginal and Torres Strait Islander health equality within 25 y. A specific aim was to halve the infant mortality disparity within a decade. Whilst there is some variation in degree of health disparities between Aboriginal and non-Aboriginal populations by state and territory in Australia, the gaps are evident and large in all regions.
The Aboriginal infant mortality rate has more than halved from 13.5 per 1000 live births in 1998 to 6.3 per 1000 live births in 2017, and the gap has narrowed significantly (by 84%) from 9.1 per 1000 live births to 3.3 per 1000 live births over this period. Since 2008 (the baseline for the Closing the Gap strategy evaluation, and prior to fortification), the Aboriginal infant mortality rate has declined by 9%, which is encouraging but there has been no significant change in the gap since 2008, because non-Aboriginal infant mortality rates have also declined by a similar amount (37). Although NTD are relatively rare causes of infant mortality (other perinatal conditions and Sudden Infant Death Syndrome are the major ones), the reduction in NTD with folic acid fortification will have made a small and important contribution to this aim.
Acknowledgments
The authors’ responsibilities were as follows—HD'A and CB: wrote the manuscript, had responsibility for final content; and have read and approved the final manuscript.
Notes
The authors reported no specific funding for this work.
Author disclosures: HD'A and CB, no conflicts of interest.
Contributor Information
Heather D'Antoine, Aboriginal Programs; Division Leader, Education and Research Support, Menzies School of Health Research, Charles Darwin University, Casuarina, Northern Territory, Australia.
Carol Bower, Email: carol.bower@telethonkids.org.au, Telethon Kids Institute, Perth, Western Australia, Australia.
References
- 1. Botto LD, Moore CA, Khoury MJ, Erickson JD. Neural-tube defects [Review]. N Engl J Med 1999;341:1509–19. [DOI] [PubMed] [Google Scholar]
- 2. Blencowe H, Kancherla V, Moorthie S, Darlison MW, Modell B. Estimates of global and regional prevalence of neural tube defects for 2015: a systematic analysis. Ann N Y Acad Sci 2015;1414:31–6. [DOI] [PubMed] [Google Scholar]
- 3. Eurocat Prevalence of neural tube defects in 20 regions of Europe and the impact of prenatal diagnosis, 1980–1986. J Epidemiol Community Health 1991;45:52–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. De Wals P, Tairou F, Van Allen MI, Uh S, Lowry RB, Sibbald B, Evans JA, Van den Hof MC, Zimmer P, Crowley M et al.. Reduction in neural-tube defects after folic acid fortification in Canada. N Engl J Med 2007;357:135–42. [DOI] [PubMed] [Google Scholar]
- 5. Berry RJ, Li Z, Erickson JD, Li S, Moore CA, Wang H, Mulinare J, Zhao P, Wong LY, Gindler J et al.. Prevention of neural-tube defects with folic acid in China. N Engl J Med 1999;341:1485–90. [DOI] [PubMed] [Google Scholar]
- 6. Smithells RW, Sheppard S, Schorah CJ, Seller MJ, Nevin NC, Harris R, Read AP, Fielding DW. Apparent prevention of neural tube defects by periconceptual vitamin supplementation. Arch Dis Child 1981;56:911–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mulinare J, Cordero JF, Erickson JD, Berry RJ. Periconceptional use of multivitamins and the occurrence of neural tube defects. JAMA 1988;260:3141–5. [PubMed] [Google Scholar]
- 8. Milunsky A, Jick H, Jick SS, Willett W. Periconceptional use of multivitamins and the prevalence of neural tube defects. N Engl J Med 1990;322:1082–3. [DOI] [PubMed] [Google Scholar]
- 9. Bower C, Stanley FJ.. Dietary folate as a risk factor for neural-tube defects: evidence from a case-control study in Western Australia. Med J Aust 1989;150:613–9. [DOI] [PubMed] [Google Scholar]
- 10. MRC Vitamin Study Research Group Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. Lancet 1991;338:131–7. [PubMed] [Google Scholar]
- 11. Czeizel AE, Dudas I.. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 1992;327:1832–5. [DOI] [PubMed] [Google Scholar]
- 12. De-Regil LM, Peña-Rosas JP, Fernández-Gaxiola AC, Rayco-Solon P. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst Rev 2015;(12):CD007950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Greene NDE, Copp AJ. Neural tube defects. Annu Rev Neurosci 2014;37:221–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Botto LD, Lisi A, Bower C, Canfield MA, Dattani N, De Vigan C, De Walle H, Erickson DJ, Halliday J, Irgens LM et al.. Trends of selected malformations in relation to folic acid recommendations and fortification: an international assessment. Birth Defects Res A Clin Mol Teratol 2006;76:693–705. [DOI] [PubMed] [Google Scholar]
- 15. Bower C, D'Antoine H, Stanley F. Neural tube defects in Australia: trends in encephalocoeles and other neural tube defects before and after promotion of folic acid supplementation and voluntary food fortification. Birth Defects Res A Clin Mol Teratol 2009;85:269–73. [DOI] [PubMed] [Google Scholar]
- 16. Canfield MA, Collins JS, Botto LD, Williams LJ, Mai CT, Kirby RS, Pearson K, Devine O, Mulinare J, National Birth Defects Prevention Network . Changes in the birth prevalence of selected birth defects after grain fortification with folic acid in the United States: findings from a multi-state population-based study. Birth Defects Res A Clin Mol Teratol 2005;73:679–89. [DOI] [PubMed] [Google Scholar]
- 17. Lopez-Camelo JS, Orioli DM, Dutra MDG, Nazer-Herrera J, Rivera N, Ojeda ME, Canessa A, Wettig E, Fontannaz AM, Mellado C et al.. Reduction of birth prevalence rates of neural tube defects after folic acid fortification in Chile. Am J Med Genet A 2005;135a:120–5. [DOI] [PubMed] [Google Scholar]
- 18. Chen LT, Rivera MA.. The Costa Rican experience: reduction of neural tube defects following food fortification programs. Nutr Rev 2004;62:S40–3. [DOI] [PubMed] [Google Scholar]
- 19. NH&MRC Revised statement on the relationship between dietary folic acid and neural tube defects such as spina bifida. J Paediatr Child Health 1994;30:476–7. [DOI] [PubMed] [Google Scholar]
- 20. Bower C, Blum L, O'Daly K, Higgins C, Loutsky F, Kosky C. Promotion of folate for the prevention of neural tube defects: knowledge and use of periconceptional folic acid supplements in Western Australia, 1992–1995. Aust N Z J Public Health 1997;21:716–21, Erratum: Australian and New Zealand Journal of Public Health 1998;22:72. [DOI] [PubMed] [Google Scholar]
- 21. Bower C, Miller M, Payne J, Serna P. Promotion of folate for the prevention of neural tube defects: who benefits? Paediatr Perinat Epidemiol 2005;19:435–44. [DOI] [PubMed] [Google Scholar]
- 22. Field B. Neural tube defects in New South Wales, Australia. J Med Genet 1978;15:329–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bower C, Forbes R, Seward M, Stanley F. Congenital malformations in Aborigines and non-Aborigines in Western Australia, 1980–1987. Med J Aust 1989;151:245–8. [PubMed] [Google Scholar]
- 24. Bower C, Eades S, Payne J, D'Antoine H, Stanley F. Trends in neural tube defects in Western Australia in indigenous and non-indigenous populations. Paediatr Perinat Epidemiol 2004;18:277–80. [DOI] [PubMed] [Google Scholar]
- 25. Li M, McDermott R.. Smoking, poor nutrition, and sexually transmitted infections associated with pelvic inflammatory disease in remote North Queensland Indigenous communities, 1998–2005. BMC Womens Health 2015;15:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Australian Bureau of Statistics Australian Health Survey Canberra 2015. [Internet]. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4727.0.55.005∼2012-13∼Main%20Features∼Foods%20Consumed∼4 [accessed 3 June 2019]. [Google Scholar]
- 27. Australian Institute of Health and Welfare Aboriginal and Torres Strait Islander Health Performance Framework report 2018. [Internet]. Available from: https://www.aihw.gov.au/reports/indigenous-health-welfare/health-performance-framework [accessed 3 June 2019]. [Google Scholar]
- 28. Bower C, Halliday J.. Neural tube defects in Australia and food fortification with folic acid. In: Preedy VR, editor Handbook of Food Fortification and Health: from Concepts to Public Health Applications. New York: Springer; 2013. p. 361–71. [Google Scholar]
- 29. Bower C, de Klerk N, Hickling S, Ambrosini G, Flicker L, Geelhoed E, Milne E. Assessment of the potential effect of incremental increases in folic acid intake on neural tube defects in Australia and New Zealand. Aust N Z J Public Health 2006;30:369–74. [DOI] [PubMed] [Google Scholar]
- 30. Maxwell SJ, Brameld KJ, Bower C, D'Antoine H, Hickling S, Marley J, O'Leary P. Baseline investigations of folate status in Aboriginal and non-Aboriginal West Australians prior to the introduction of mandatory fortification. Aust N Z J Obstet Gynaecol 2013;53(1):26–31. [DOI] [PubMed] [Google Scholar]
- 31. Bower C, Maxwell S, Hickling S, D'Antoine H, O'Leary P. Folate status in Aboriginal people before and after mandatory fortification of flour for bread-making in Australia. Aust N Z J Obstet Gynaecol 2016;56(3):233–7. [DOI] [PubMed] [Google Scholar]
- 32. Hickling S, Knuiman M, Jamrozik K, Hung J. A rapid dietary assessment tool to determine intake of folate was developed and validated. J Clin Epidemiol 2005;58:802–8. [DOI] [PubMed] [Google Scholar]
- 33. Bower C, Baynam G, Rudy E, Quick J, Rowley A, Watson LF. Report of the Western Australian Register of Developmental Anomalies 1980–2014. Western Australia: Department of Health, Western Australia, WA Newborn Services; 2015. Issue No.: 22. [Google Scholar]
- 34. Hilder L. Neural tube defects in Australia, 2007–2011. In: National Perinatal Epidemiology and Statistics Unit UNSW, editor NSW: Commonwealth of Australia; 2016. [Google Scholar]
- 35. COAG National Indigenous Reform Agreement (closing the gap). Canberra: Council of Australian Governments; 2009. [Google Scholar]
- 36. Department of Families Housing Community Services and Indigenous Affairs Closing the Gap on Indigenous Disadvantage: The Challenge for Australia. Canberra: Commonwealth of Australia; 2009. [Google Scholar]
- 37. Australian Government Closing the Gap Report 2019; Chapter Two Infancy and Childhood. Canberra: Department of Prime Minister and Cabinet; 2019. [Google Scholar]