Abstract
Elder abuse is an increasingly intangible phenomenon that has created numerous ethical issues for care teams and caregivers. Although different studies have concentrated on various ethical issues regarding abuse, no study has arrived at a comprehensive conclusion. Therefore, the present study aimed to determine the existing ethical challenges in this context.
For this purpose, two researchers familiar with systematic search approach examined national and international journals on PubMed, Excerpta Medica Database (EMBASE), Scientific Information Database (SID) and similar databases between January and February 2017. They were able to find 116 articles that met the inclusion and exclusion criteria, and finally selected 15 articles based on the predesigned questions.
The findings were classified in five subtitles as follow: 1) the common definition of elder abuse, 2) a comprehensive legislation on elder abuse, 3) comprehensive ethical principles about elder abuse, 4) ethical considerations regarding patients without competency, and 5) reporting and sharing information about elder abuse. The study results revealed no common definition and no legislation about elder abuse, and also showed that health care providers’ observance of ethical principles depends on the ethical and legal conditions of the community.
Nowadays, elder abuse is a serious problem in many countries. Cultural and religious differences are the reasons for lack of a common definition and legislations, which comprises the biggest obstacle to protecting the rights of elderly people. It is clear that ethical principles should be respected as far as a person has competency. Furthermore, localization of clinical guidelines related to this issue leads to proper functioning of health care providers, especially nurses as the first line of treatment.
Key Words: Elder abuse, Elder maltreatment, Ethics
Introduction
Abuse is among the most common challenging issues in both developed and developing countries around the world (1, 2). Presently, elder abuse is the most covert form of mistreatment that involves issues such as health, justice, ethics, and human rights (3). This phenomenon has been taken into consideration by World Health Organization (WHO) since 2002 (4).
Different definitions have been provided for abuse over time (5). Elder abuse may refer to an act or absence of a proper act that will cause harm or suffering to an older person, and it happens in a relationship that normally requires trust, and may be performed only once or several times (1,2,6).
While little information is available about elder abuse especially in developing nations, it is predicted to be on the rise in countries that experience the phenomenon of population aging. According to WHO estimations, one out of every six elderly people experiences abuse, and only 1 out of 24 abuse cases is reported (1). Since awareness of abuse is influenced by knowledge, expertise and preparedness of caregivers (3, 7), the care team and nurses as the first line of treatment are responsible to identify and report mistreatments and support vulnerable populations such as the elderly (8, 9). Elder abuse is an example of human rights and freedom violation (5) that leads to a serious loss of human dignity, independence and respect (6), and influences ethical principles such as autonomy, competency, beneficence, and non-maleficence (10).
Intervention in case of abuse is accompanied by ambiguity and ethical challenges, because lack of professional principles leads to personal, legal and ethical concerns (11). However, it is difficult for nurses and other members of the care team to perform a successful intervention for an elderly who is willing to stay in the abusive situation (12). Also, this phenomenon causes challenges for nurses and other care team members when legal commitments are not consistent with ethical principles (11). Questions and challenges in this context include: Are there any comprehensive ethical principles and regulations? Is it illegal to share the information and secrets of patients with the care team in order to reach a diagnosis or choose the appropriate intervention? Which ethical principle is violated in elder abuse? When is respect for autonomy not consistent with ethical principles? In what cases are beneficence and non-maleficence in conflict with the other ethical principles? In cases where the patient suffers from a cognitive disorder, what are the ethical considerations that need to be taken into consideration by the nurse? Should reporting elder abuse be a legal requirement? What ethical challenges will nurses face when the elderly are not willing to share information with the authorities?
Abuse by a family member or intimate partner is complex, because the elderly may be struggling against social, cultural and religious aspects of life to live with abusive people (12). According to College of Nurses of Ontario (CNO), ethical conflicts and challenges emerge when two or several ethical values relevant to a particular situation necessitate conflicting measures (13). Elder abuse causes physical harm, depression, increased referral to hospitals, frequent hospitalizations, and increased mortality (1,2,14,15). It also creates problems such as job burnout and ethical distress for nurses and care team members (16), who should have a thorough and accurate understanding of the ethical concepts and challenges involved in elder abuse and decide on the best intervention (17). In view of the importance of this issue, this study aimed to examine the ethical challenges pertaining to elder abuse according to evidence-based ethical principles.
Method
The present study was a systematic review to determine the ethical challenges involved in elder abuse and was conducted in 2017 by collecting related documents, articles, and sources.
Data sources and search method
To find articles, national and international journals from databases such as PubMed, EMBASE, ProQuest Central, Web of Science, SID, Magazine Iranian (Magiran) and Psychology Information (PsycINFO) were examined. For this purpose, journals were searched using Persian and English keywords according to MeSH. Important keywords included “elderly”, “aged”, “abuse”, “neglect”, “mistreatment”, “ethics”, “ethos”, “moral”, and “autonomy”. In order to increase sensitivity, general Persian and English keywords such as “violence” and “senior” were also used in the search process.
Article selection criteria
According to the inclusion and exclusion criteria, different articles available in the context of descriptive studies were examined. Since the nature of this issue is descriptive, articles with more evidence were selected.
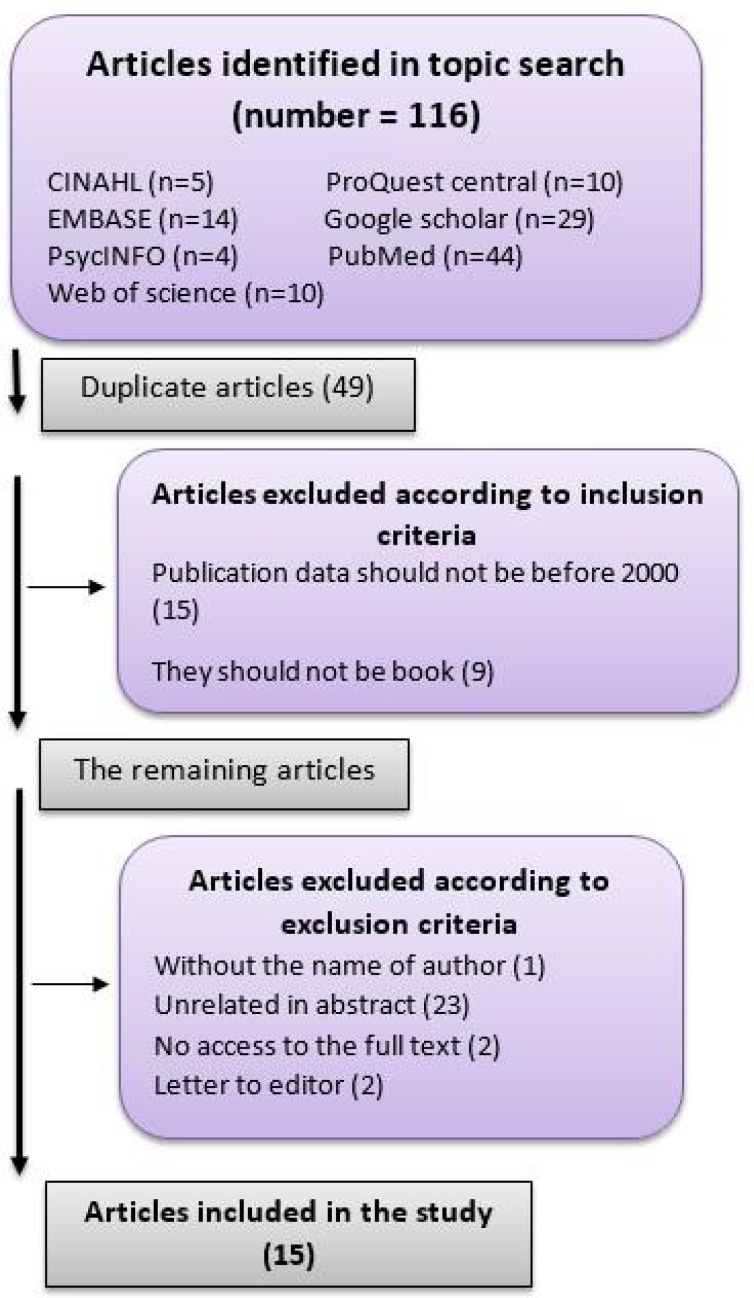
The search was performed by two researchers familiar with systematic search approach between January and February 2017 according to the keywords and databases, and the details were documented. In this regard, 116 articles were found as seen in Figure 1.
Figure 1.
Article examination flowchart
Forty-nine articles were identified by EndNote to be duplicates and were therefore excluded from the study. According to the inclusion criteria, articles published after 2000 and those cases that had not been published were included in the initial examination. The abstracts were then studied by the two researchers in order to exclude unrelated articles, obtain the full texts for the ones that were related, and extract data for two of the articles whose full texts were not available. Finally, 15 articles were entered in the study to answer the following questions: Has a common definition been offered for elder abuse so far? Is there a comprehensive ethical set of regulations about elder abuse? What ethical principle is violated in elder abuse? When is the autonomy of elder people in conflict with ethical principles?
In order to minimize error, the required information was extracted according to the checklist (Table 1) by the two researchers and the results were matched. Checklist variables included title, author, year, journal, place and objective, definition of elder abuse, method, concepts, ethical issues, and clinical points.
Table 1.
Characteristics of the reviewed articles on the ethical challenges in caring for elder abuse
| Objective | Type of Study |
Country | Year | Resource |
|---|---|---|---|---|
|
Updating moral considerations
regarding elder abuse in psychological domain Providing recommendations to improve problem solving related to elder abuse |
descriptive | The United States |
2012 | Scheiderer EM(5) |
|
Forms of elder abuse in nursing homes
Reasons for elder abuse in nursing homes Which ethical principles are violated in nursing homes? |
descriptive | The United States | 2011 | Bužgová R (28) |
|
Discussion about important ethical
perspectives on self-neglect among elderly people |
descriptive | The United States | 2011 | Mauk KL (10) |
|
Examining abused people according to
ethical codes and guidelines to enable psychologists to solve the problems of these people Helping to resolve challenges to reporting these cases and specifying certain standards for reporting. |
descriptive | The United States |
2011 | Zeranski (18) |
|
Solving the complications arising from
elder abuse Concentrating on informing social services experts about challenges resulting from ambiguity in laws and guidelines |
descriptive | Canada | 2010 | Donovanet (11) |
|
Examining the gap between the
existing laws about elder abuse, and implementing them Examining protection of elderly people against elder abuse |
descriptive | England | 2010 | Ash(21) |
|
Examining the existing texts about
elder abuse Suggesting preventive measurement to decrease the incidence of abuse |
descriptive | England | 2010 | Formanet (26) |
|
Examining the relationship between
cultural values such as individualism and identification of the ethical issues and consequences of policymaking; Discussing about similarities and differences in the reporting system |
descriptive | Korean- American |
2009 | Doe (19) |
|
Examining women’s understanding of
different economic and social conditions regarding elder abuse and the ethical problems in support systems |
descriptive | The United States |
2009 | Dakin (38) |
|
Determining who the people
experiencing abuse are, how they are identified, and which professionals are trying to resolve these conditions? |
descriptive- cross- sectional |
France | 2006 | François (39) |
|
Describing an ethical decision-making
model according to an empowerment framework for care service providers |
descriptive | The United States |
2006 | Koenig (22) |
|
Proposing the perspective of
psychologists on elder abuse, and the psychological and ethical issues regarding this subject |
descriptive | The United States |
2006 | Beaulieu (33) |
|
Stating the reasons for abuse according
to the statements of social workers in England |
descriptive | England | 2004 | Wilson (24) |
|
Discussing ethical concerns about
reporting or failure to report abuse Providing recommendations to help service providers in the decision- making process |
descriptive- case study |
The United States |
2003 | Bergeron (23) |
|
Establishment of a standard ethical
model to deal with elder abuse |
descriptive | The United States |
2000 | Johnson (40) |
After collecting the data based on the checklist, data quality was assessed by two experts. In order to prevent bogus, names of journals and authors were eliminated and the data were given to two experts. The publication years of 15 articles were between 2000 and 2012, 9 articles had been authored in the United States, 1 in Canada, 3 in the UK, 1 in France, and 1 was a Korean-American article. Articles were descriptive, cross-sectional, and case study. No Persian article was found by searching these keywords.
Results
Along with the proposed questions, the findings of the present study were classified in five subtitles as follow:
1. The Common definition of elder abuse
Question: Has a common definition been offered for elder abuse so far?
The researchers did not find any specific definition for the term. A study conducted in 2012 stated that concepts related to elder abuse are abstract and there is no widely accepted definition for it. This lack of definition poses challenging questions. US laws recognize cases such as physical abuse, neglect and financial abuse, but the definitions are not the same in various states and to all researchers and doctors (5). Another American study declares that all 50 states in the Unites States have laws concerning abuse, but the definitions for elder abuse and those who are covered by these laws are different (18).
In this regard, another study stated that in most US laws, physical, sexual, financial, and psychological/emotional abuse pertain to elder abuse, as does self-neglect, which is in concordance with the Older Adult Welfare Law (OAWL) definition of abuse (19).
Adult Protective Services (APS) has identified three misconducts in connection with vulnerable elderly people: abuse, financial exploitation, and neglect. Abuse is defined as intentional harm to people. Financial exploitation is an illegal process of using vulnerable elderly people to obtain assets without their conscious consent. Neglect is the inability of an elderly person for self-care (self-neglect) or failure of a caregiver to provide appropriate care (20). Other studies have pointed to the definition provided by WHO that states “elder abuse consists of committing an inappropriate action in a trustful relationship that causes harm to an elderly person”, and four studies did not address the definition of abuse (21, 22, 23, 24).
2. A comprehensive legislation on elder abuse
Question: Is there a comprehensive legislation about elder abuse?
Most US states combine elderly support laws and disabled adult laws. The laws are different in terms of classifications of abuse, but in general, elder abuse can be classified in five categories: physical abuse, psychological/emotional abuse, financial exploitation, neglect/self-neglect, and sexual abuse. Across the US, Elder Abuse Protection (EAP) laws share three common functions: 1) collecting the suspected abuse reports, statistical data management, and patients’ needs evaluation; 2) efforts to decrease or eliminate abuse risk for elderly people by providing instructions and interventions through referral to social services; 3) connection with courts and organizations that are responsible to execute the law in special cases (23, 25, 26).
The results of Bergeron and Gray’s study in 2003 revealed three major differences between the laws in different states of the US. First, in some states, it is mandatory to report suspected elder abuse. The second difference is the definition of “elderly” provided by law. In order to limit interventions in the private lives of citizens, some states have restricted their laws to vulnerable elderly people. The third difference is related to the authorization given to EAP staff in some states to conduct studies on abuse and make interventions in cases where abuse has been proved. For example, some states ask the EAP staff to receive permission from the victim in all research steps unless the victim lacks competency, while other states do not (23).
The National Association of Social Workers (NASW) and the Canadian Association of Social Workers (CASW) have specified values and principles as guidelines for the professional behavior of social services experts. These principles emphasize prioritization of the best interests of patients and protection of those who lack competency for decision-making. They also require that confidentiality of information be taken into consideration, which may be in conflict with abuse reporting responsibilities (11). Also in January 2004, OAWL established stable laws to offer protection services for elderly people such as 24-hour emergency phone lines to report abuse, standards to issue certificates for protective facilities, and professional standards to care for elderly people (19).
3. Comprehensive ethical principles about elder abuse
Question: Are there any comprehensive ethical principles about elder abuse?
A study conducted in the Unites States pointed out that when disclosing information, psychologists should use American Psychological Association (APA) codes (5, 27). In this regard, another study proposed that psychologists consider ethical commitments in addition to the legal aspects of abuse reporting.
Reporting suspected cases according to APA ethical codes should be in line with beneficence, non-maleficence, and respect for human rights and dignity. Code 4/02 is related to privacy limitation and code 4/05 pertains to disclosure of information regarding elder abuse. If the elderly suffers from cognitive disorders, psychologists should try to maintain the confidentiality of their information and contact legal authorities. According to code 4/02, they are allowed to disclose information in suspected abuse cases even without the patient’s consent. According to code 4/05, psychologists are allowed to share the private information of patients with the latter’s families or with other experts to protect patients against harm (18).
In a 2009 study by Doe et al., similarities and differences between the protection systems of Korea and the United States were investigated. The two countries are similar in that they both have national laws to prohibit elder abuse, and legal definitions include abuse and neglect. In addition, laws necessitate mandatory reporting by experts. As for the differences, in the United States, federal laws are executed by different federal systems that implement both the methods of reporting abuse and referral. Emergency cases enter triage from the very beginning and a protection plan is designed for abuse cases and other forms of mistreatment. Laws prosecute the guilty person and punishments are specified for failure to report. However, in Korea, the law is enforced by a centralized system that only implements the reporting of abuse. Emergency cases are triaged within 12 hours and care plan only exists for abuse cases. These laws allow the patient to file a civil complaint about abuse, but they do not specify any punishment for failure to report (19).
Question: What ethical principle is violated in elder abuse?
Findings showed that the principle of respect (dignity and autonomy) is almost violated in psychological abuse, and the principle of non-maleficence in cases of neglect and physical or financial abuse (28). In most cases, autonomy may be violated because self-neglect, beneficence and non-maleficence may come before it, and as for self-neglect, caregivers can delay the required interventions as far as possible (10).
Autonomy
Autonomy includes independent decision-making without any limitation, and respect for independence is a professional commitment (29). According to the American Nurses Association (ANA) autonomy not only means respect for patients’ decision-making, but also for the decision-making method (30), and patients have the right to participate in making decisions related to themselves (31). Another study stated that social workers are responsible for creating a balance between patients’ rights and the principle of autonomy, which aims to protect vulnerable populations. Nevertheless, in NASW, it is pointed out that social workers should have authority over patients’ right to autonomy when potential and actual actions of patients cause serious, predictable and unpredictable risks for themselves and others (11, 32). Also, another was consistent with the above-mentioned points and stated that autonomy to maintain independence is acceptable only as far as it is reasonably and ethically possible (10).
Negative autonomy emerges when the elderly prevents services and the caregivers accept this behavior, which is indeed a kind of neglect. Prevention is acceptable if the person has the capability for decision-making and his or her mental capacity is approved (33).
Beneficence and non-maleficence
Beneficence and non-maleficence are both based on ethical commitment toward others, and while the former focuses on the well-being of others, the function of the latter is to avoid harming them (29). Together, the two aspects provide more comprehensive principles to devise measures against elder abuse. For example, if a nurse considers a threat or damage serious and is convinced that measures are necessary to prevent harm, he or she will report the abuse to APS. Therefore, the nurse may use the principle of beneficence to promote health and ensure the best interests of the patient (10).
Justice
In the 15 papers that were examined in this study, the principle of justice had not been mentioned.
4. Ethical considerations regarding patients without competency
Question: In cases where the patient lacks competency, what ethical considerations should be taken into account by the nurse or the care team?
A study entitled “Capacity for decision-making in Alzheimer's disease: selfhood, positioning and semiotic people” showed that capacity and competency are often used interchangeably. Capacity has dimensions such as decision-making, self-care, self-protection, and execution. According to experts, competency can fluctuate. In dementia, there is memory impairment, but personality, values and long-term memory stay intact. Dementia patients can be extremely vulnerable under undesirable conditions and their right of decision-making for different aspects of their life is unfairly influenced (34).
Dementia diagnosis is not the only criterion for lack of competency (35, 36). For competent elderly people who expose themselves or others to harm, the caregiver may decide to work in support of beneficence, trying to achieve the best long-term results for the patient. It is noteworthy that one should consider interdisciplinary interventions, ethical principles, and cultural and gender differences when trying to determine decision-making capacity by means of valid and reliable measurements.
Dick suggests that nurses should note the cultural beliefs and patterns of adaptation of family members who neglect an elderly person’s personal and environmental health requirements rather than consider it a pathological finding (37). Nevertheless, according to most studies, when the elderly is incapable of decision-making due to cognitive impairment, the task can be left to another person. This person should support the patient and be aware of his/her needs. Most regional councils for elderly issues provide care services in which a group of competent people function as decision-makers for elderly people (5). In cases where decisions are related to the patient’s capacity, consultation with a group of interdisciplinary experts is necessary and the decisions should eventually be in favor of the elderly people (10).
5. Reporting and sharing information about elder abuse
Question: Is it illegal to report abuse and share the information of elderly people?
Respect for confidentiality and trust is one of the most important ethical principles that has to be taken into consideration by caregivers. However, the results of one study indicate that in cases where a serious harm is caused, the care team can disclose information without obtaining consent (11). These findings were confirmed by another study, which presented statements with similar wording. For example, in the United States, if a therapist is suspicious about abuse, he/she should report it to authorities such as APS despite his/her concerns over the patient’s privacy (26). Also, according to code 4/05, psychologists are allowed to disclose patients’ private information to protect them against harm (17). However, they should try to engage the patient in the reporting process and only report relevant data to observe the privacy of the patient as far as possible (26).
Discussion
Concepts related to elder abuse are complex and abstract, and therefore no common definition has been offered for this phenomenon (5). In most cases, the word abuse is replaced by maltreatment and mistreatment (41). One reason for lack of a common definition is related to cultural and religious differences among societies. Accordingly, people from different races have their own definition of abuse and its types based on their regional priorities (41, 42).
Care team members need a clear definition to identify and prevent elder abuse (43). When a suitable definition does not exist for the phenomenon, accurate statistics cannot be obtained, which makes it impossible to identify and report abuse; consequently, the prevalence of this phenomenon will remain obscure. Therefore, measures related to elder abuse should be specific to each region where authorities function as the main foundations.
Another duty of governments includes establishment of regulations and ethical principles related to elder abuse. Since comprehensive ethical and legal regulations have not been developed and there are many ambiguities and conflicts, abuse cases are not reported due to the inability of the care team to interpret the ethical and legal codes (5).
Based on the existing evidence, elder abuse is a general issue in Italy where different policies and laws exist for the phenomenon and lack of a national and comprehensive strategy is tangible. While certain laws are in place for child protection, there are no specific regulations for elderly people.
Lack of legislation is the biggest obstacle to protecting the rights of elderly people in many countries. Constitutions normally emphasize rights, freedom, dignity and equality for all people, with the main emphasis on the latter. Elderly people may not be able to defend their rights. Therefore when they become dependent, they may be vulnerable to abuse and misconduct (44).
The first federal law on elder abuse was codified as “The Elder Justice Act” in March 2010 including the following main articles: (a) formation of the elder justice council to suggest recommendations related to federal, regional and private agencies involved in elder abuse; (b) formation of a council to plan strategic programs on elder justice; (c) budget provision; (d) founding and supporting legal centers; (e) provision of budget for long-term treatment programs; (f) financial assistance to improve long-term treatment programs for staff; and (g) budget provision for national institutes (45, 46).
Moreover, laws related to APS aim to control elder abuse in home environments or institutes. Depending on the type of law, in each country there is a reporting system for elder abuse and social services provisions to support victims and change the conditions. Nevertheless, the aforementioned laws are mostly related to abuse of adults with disabilities and vulnerabilities rather than elder abuse (47).
Therefore, the availability of ethical principles and laws helps the care team deal with abuse. Ethical principles are laid down by experts to protect the profession, and social workers will be directed to implement the pertinent activities by standard establishment. This helps professionals defend themselves against Ethics Supervisory Boards as well (47).
Sometimes professionals deal with elderly people who experience conditions not directly specified by ethical standards, and this creates challenges (48). In such cases, members of the care team face controversial ethical and legal conditions in action. Ethical principles concentrate on rights and commitments against ethical challenges and specify what care team members should do in order to observe these principles. However, they may refrain from performing an ethical task for fear of the consequences, and may not implement any type of intervention in cases of abuse because they are concerned about violation of the patients’ rights (11).
Ethical principles are taught theoretically and when complications arise, care team members have a tendency to neglect ethical teachings, believing that theoretical teaching is one of the factors that complicate elder abuse (24). It is necessary for those who deal with elderly people to be aware of the professional, legal and ethical issues of elder abuse. In order to stay committed to caregiving values, the care team should have an effective performance and provide safety for elderly people and at the same time respect their dignity.
Important ethical principles that are violated in abuse are autonomy, beneficence, non-maleficence, and justice. This phenomenon not only involves elderly people, but also other vulnerable classes of the society such as women, children, people with disabilities, and people who suffer from mental disorders. Abuse creates challenges for the care team and puts them in dilemma. The question that now arises is: should the rights and freedom of an elderly person who has been abused be violated out of concern for his or her safety? In truth, the dual commitment of staff and other caregivers may violate the patient’s right to autonomy.
One study showed that professionals who are responsible for protecting patients should keep in mind that when an elderly person decides to reject services (autonomy) and continue to live in threatening conditions, logical thinking under critical circumstances will be a necessity (11). In a 2003 study by Healy the responses to a self-assessment by social services staff to ethical dilemmas concerning the decision-making capacity of elderly patients suffering from cognitive impairment are reported. In the section pertaining to house safety conditions, participants stated that they were faced with conflict when they had to force the person to go somewhere safe or respect his/her decision to continue in the existing conditions. In such cases, social workers face a decision-making challenge: to refrain from intervention and respect the person’s autonomy, or try to prevent harm to the person and introduce the culprit to the judiciary system (49).
However, discussion about ethical principles is complex, because they are based on the culture in each society. Autonomy should be respected as far as the person has competency and poses no risk for people and the community. The principles of beneficence and non-maleficence are no exception. When a patient’s decision jeopardizes individual and social interests, the two principles of beneficence and autonomy are in conflict, because respect for one principle violates the other. In these cases, the care team should select the best functional option according to regional interests, consultations and guidelines.
Another controversial issue relating to abuse is the principle of confidentiality. Confidentiality is one of the important principles ruling the relationship between patients and the care team, and one justification for it is respect for patient’s autonomy. The principle of autonomy emphasizes the patient’s right over all stages of life. Therefore, one’s personal information belongs to oneself and no one should be aware of it without permission. If confidentiality is violated, the patient’s autonomy will be violated too.
However, reporting abuse is another challenging issue. Discussion about elder abuse reporting is not limited to the social context, but it necessitates awareness about medication, law execution, and social services. All professionals who have relationships with elderly patients regarding treatment and law execution should assume the ethical responsibility to protect them against harm.
Rodriguez et al. conducted interviews in 2006 with primary health-care providers. They concluded that in Los Angles, physicians experience a conflicting relationship between life quality and obligatory reporting laws. Most respondents believed that the effects of abuse result in both improvement and harm for the patient, and experts’ tendency to promote patients’ life quality may decrease due to frequent reports (50).
The ethical principles of the American Counseling Association (ACA) emphasize the mandatory nature of consultation with other experts when counselors are not sure whether the case meets the reporting criteria or not. It should be mentioned that professionals should not only report suspected abuse, but they should be familiar with laws and regulations related to reporting, so that if a problem occurs, they can report it effectively (23).
Opponents of mandatory reporting argue that this type of reporting violates autonomy where the privacy of people is compromised (38). Evidence shows that social workers in Korea choose not to execute mandatory reporting because they feel that by modifying the conditions that cause abuse, family members can participate in providing care for the elderly at home. Social workers believe that providing care at home, improving the relationship between the elderly and their families and intermediation role provide a better cultural option for the elderly (19). There are concerns about receiving services from all ethnic groups. Studies on services showed that elderly people from various racial groups prefer to receive assistance from family members and friends to solve all types of problems except health and financial problems (23, 51). However, the mandatory reporting law should observe the dignity and privacy of people.
Now, the question is, what is the objective of the care team in reporting suspected abuse cases? The objective should not be to obtain or complete the statistics of abuse cases, but the principles of beneficence and non-maleficence should be prioritized. The reporting system is unique in every country and follows the ethical principles and laws of that country. Mandatory reporting is valued when there are protective systems and laws to help the elderly and rescue them from trouble. In countries where these laws do not exist, however, mandatory reporting does not promote a person’s quality of life, and even increases the gap between that person and his/her family members who have committed abuse. Since a support system is non-existent in these countries, the elderly has to continue to live with the abusive family member(s), who may do more harm to the elderly, and even cause their death, because no education, reward or punishment system is in place.
As for the competency of the elderly, the obvious point is that despite the availability of instruments such as the Mini-Mental State Examination (MMSE) that examines cognitive capacity, researchers should fully examine the cultural concerns associated with environmental and lifestyle patterns (52).
Finally, for decision-making the care team can benefit from the communication ethics approach, which is a participatory method comprising several stages: (a) the defense stage to clarify conditions and issues; (b) consultation; and (c) negotiation that leads to agreement (40).
Iranian Ethical Challenges
The definition of elder abuse varies in different societies. According to an Iranian study by Heravi et al. conducted in 2013, elder abuse may be defined as an act or absence of a proper action by family members or relatives, which may happen once or several times, and can cause harm or distress to an older person (53).
Comprehensive ethical and legal regulations have so far not been developed in Iran. According to investigations by a researcher in Iran, no specific law exists about reporting and handling elder abuse. The Secretariat National Council of the Elderly in Iran, established in 2004, is the only organization that is active in various fields related to the elderly, but it seems that no significant activity has been performed regarding elder abuse. Also, Social Emergency has been active in Iran since 2007 to prevent harms and also provide services in connection with elder abuse, but they have not mentioned any specific ethical principles for managing elder abuse, its identification and referral. It is clear that availability of ethical principles and laws can help the care team deal with abuse.
In chapter three of the Constitution of the Islamic Republic of Iran, the importance of autonomy and human dignity has been addressed. According to the constitution, respect for human dignity is a principle accepted by the Islamic Republic of Iran, obliging the government to provide care services to everyone (54). Accordingly, care services should be based on respect for rights and dignity of patients. Accordingly, the patient should choose and decide freely. Respect should be provided for the patient while receiving care services based on respect for patients’ privacy and confidentiality of information. In this regard, a study by Davis et al. showed that the possibility of decision-making is vital for elderly people, and lack of autonomy leads to depression (51).
Based on our Iranian-Islamic beliefs, confidentiality means trust, and it has to be protected. Sharing personal information with others indicates betrayal. Also, according to Article 648 of the Islamic Penal Code, disclosure of patients’ secrets is illegal except when personal or public interest is at risk (55).
In Iran, there is no particular penal code for elderly people, but according to Article 596 of the Islamic Penal Code on financial abuse, the abuser will be sentenced to 16 months to 2 years of imprisonment and payment of a fine. If the abuser is the guardian of the victim, in addition to the fine, the abuser will be sentenced to 3 to 7 years of imprisonment (56).
Thus, according to the above-mentioned points, elder abuse is a phenomenon that needs more attention from the government.
Conclusion
Abuse is a serious problem among elderly people. Although the care team is responsible for the support and promotion of the independence of elderly people, ethical challenges are the result of unsatisfactory performance of the care team and people who endanger themselves or the others.
In decision-making about measures related to elder abuse, ethical principles such as autonomy, beneficence, non-maleficence and competency should be taken into consideration. The care team should protect the autonomy of elderly people and consider their health and welfare. However, they should not impose their beliefs regarding living environments or social decision-making on the elderly.
As far as possible, the relationship between elderly people and family caregivers should be promoted. At the same time, protecting elderly people will not be possible unless the society can help them maintain their independence outside of the family system. This will allow the elderly to enjoy a positive relationship with members of their family who are also their caregivers. The achievement of these goals necessitates long-term coordination between services and institutes.
Some measures that can be effective in this context include: devising appropriate instructions for the care team, particularly nurses who deal with abuse issues; communication and consultation with other service providers while observing privacy and autonomy; commitment to follow instructions; observing ethical considerations regarding abuse; and conducting empirical studies.
Nurses as the first line of treatment and other care team members have an important role in this respect. Compilation or localization of clinical guidelines for the care team not only influences their perspectives into ethical issues, but also helps them perform properly and select the best functional option. Finally, clinical guidelines support the behavior and performance of the care team and serve as a criterion to assess the caregiving quality.
Acknowledgements
This article is part of a dissertation for a master's degree approved by Tehran University of Medical Sciences, Faculty of Nursing and Midwifery under the code of ethics 9411580003. The researcher declares her appreciation to the officials of the Nursing and Midwifery Faculty of Tehran University of Medical Sciences.
Notes:
Citation to this article:
Saghafi A, Bahramnezhad F, Poormollamirza A, Dadgari A, Navab E. Examining the ethical challenges in managing elder abuse: a systematic review J Med Ethics Hist. 2019; 12: 7.
Conflict of Interests
Authors declare no conflict of interest.
References
- 1.Anonymous Elder abuse World health organization. [cited 2017 June]. Available from: http://www.who.int/mediacentre/factsheets/fs357/en/.
- 2.Yunus RM, Hairi NN, Choo WY, et al. Mortality among elder abuse victims in rural Malaysia: a two-year population-based descriptive study. J Elder Abuse Negl. 2017;29(1):59–71. doi: 10.1080/08946566.2016.1260083. [DOI] [PubMed] [Google Scholar]
- 3.Luzny J, Jurickova L. Prevalence of elder ebuse and neglect in seniors with psychiatric morbidity - example from central moravia, Czech Republic. Iran J Public Health. 2012;41(8):27–32. [PMC free article] [PubMed] [Google Scholar]
- 4.Brandl B, Dyer CB, Dyer CB, Heisler CJ, Otto JM, Stiegel LA, Thomas RW. USA: Springer Publishing Company; 2006. Elder abuse detection and intervention: A Collaborative Approach, 1st ed. [Google Scholar]
- 5.Scheiderer EM. Elder abuse: ethical and related considerations for professionals in psychology. Ethics & Behavior. 2012;22(1):75–87. [Google Scholar]
- 6.Garnham B, Bryant L. Epistemological erasure: the subject of abuse in the problematization of ‘elder abuse’. J Aging Stud. 2017;41:52–9. doi: 10.1016/j.jaging.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Chan KL, Brownridge DA, Fong DY, Tiwari A, Leung WC, Ho PC. Violence against pregnant women can increase the risk of child abuse: a longitudinal study. Child Abuse Negl. 2012;36(4):275–84. doi: 10.1016/j.chiabu.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Adams JA, Bailey DE, Anderson RA, Docherty SL. Nursing roles and strategies in end-of-life decision making in acute care: a systematic review of the literature. Nurs Res Pract. 2011;2011:527834. doi: 10.1155/2011/527834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Almogue A, Weiss A, Marcus E-L, Beloosesky Y. Attitudes and knowledge of medical and nursing staff toward elder abuse. Arch Gerontol Geriatr. 2010;51(1):86–91. doi: 10.1016/j.archger.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Mauk KL. Ethical perspectives on self‐neglect among older adults. Rehabil Nurs. 2011;36(2):60–5. doi: 10.1002/j.2048-7940.2011.tb00067.x. [DOI] [PubMed] [Google Scholar]
- 11.Donovan K, Regehr C. Elder abuse: Clinical, ethical, and legal considerations in social work practice. Clinical Social Work Journal. 2010;38(2):174–82. [Google Scholar]
- 12.Finfgeld-Connett D. Intimate partner abuse among older women: Qualitative systematic review. Clin Nurs Res. 2014;23(6):664–83. doi: 10.1177/1054773813500301. [DOI] [PubMed] [Google Scholar]
- 13.Anonymous Practice standard: ethics. [cited 2017 June]. Available from: http://www.cno.org/globalassets/docs/prac/41034_ethics.pdf.
- 14.Lowenstein A. Caregiving and elder abuse and neglect—developing a new conceptual perspective. Ageing International. 2010;35(3):215–27. [Google Scholar]
- 15.Schofield MJ, Mishra GD. Three year health outcomes among older women at risk of elder abuse: women's health Australia. Quality of Life Research. 2004;13(6):1043–52. doi: 10.1023/B:QURE.0000031343.15372.a5. [DOI] [PubMed] [Google Scholar]
- 16.Swagerty DL, Takahashi PY, Evans JM. Elder mistreatment. American Family Physician. 1999;59(10):2804–08. [PubMed] [Google Scholar]
- 17.Olson JM, Hoglund BA. Elder Abuse: speak out for justice. J Christ Nurs. 2014;31(1):14–21. doi: 10.1097/cnj.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 18.Zeranski L, Halgin RP. Ethical issues in elder abuse reporting: a professional psychologist's guide. Professional Psychology: Research and Practice. 2011;42(4):294–300. [Google Scholar]
- 19.Doe SS, Han HK, McCaslin R. Cultural and ethical issues in Korea's recent elder abuse reporting system. J Elder Abuse Negl. 2009;21(2):170–85. doi: 10.1080/08946560902780009. [DOI] [PubMed] [Google Scholar]
- 20.Mohebbi L, Zahednejad S, Javadi Pour S, Saki A. Domestic elder abuse in rural area of Dezful, Iran and its relation with their quality of Life. Iranian Journal of Ageing. 2016;10(4):50–9. [Google Scholar]
- 21.Ash A. Ethics and the street-level bureaucrat: implementing policy to protect elders from abuse. Ethics and Social Welfare. 2010;4(2):201–9. [Google Scholar]
- 22.Koenig TL, Rinfrette ES, Lutz WA. Female caregivers’ reflections on ethical decision-making: the intersection of domestic violence and elder care. Clinical Social Work Journal. 2006;34(3):361–72. [Google Scholar]
- 23.Bergeron LR, Gray B. Ethical dilemmas of reporting suspected elder abuse. Soc Work. 2003;48(1):96–105. doi: 10.1093/sw/48.1.96. [DOI] [PubMed] [Google Scholar]
- 24.Wilson G. Dilemmas and ethics: social work practice in the detection and management of abused older women and men. Journal of Elder Abuse & Neglect. 2004;14(1):79–94. [Google Scholar]
- 25.Simon ML. An Exploratory Study of Adult Protective Services Programs' Repeat Elder Abuse Clients. USA: American Association of Retired Persons; 1992. [Google Scholar]
- 26.Forman JM, McBride RG. Counselors' role in preventing abuse of older adults: Clinical, ethical, and legal considerations. Adult Span Journal. 2010;9(1):4–13. [Google Scholar]
- 27.Anonymous Guidelines for psychological practice with older adults. [cited 2017 June]. Available from: https://www.apa.org/pubs/journals/features/older-adults.pdf.
- 28.Bužgová R, Ivanová K. Elder abuse and mistreatment in residential settings. Nurs Ethics. 2009;16(1):110–26. doi: 10.1177/0969733008097996. [DOI] [PubMed] [Google Scholar]
- 29.Childress JF, Beauchamp TL. Principles of Biomedical Ethics, 5th ed. UK: Oxford University Press; 2001 pp. [Google Scholar]
- 30.Marsha F. Guide to the Code of Ethics for Nurses: With Interpretive Statements: Development, Interpretation, and Application, 2nd ed. USA: American Nurses Association; 2001. [Google Scholar]
- 31.Regehr C, Antle B. Coercive influences: informed consent in court-mandated social work practice. Social Work. 1997;42(3):300–6. [Google Scholar]
- 32.Anonymous Highlighted revisions to the code of ethics. [cited 2017 August]. Available from: https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Highlighted-Revisions-to-the-Code-of-Ethics.
- 33.Beaulieu M, Leclerc N. Ethical and psychosocial issues raised by the practice in cases of mistreatment of older adults. J Gerontol Soc Work. 2006;46(3-4):161–86. doi: 10.1300/J083v46n03_10. [DOI] [PubMed] [Google Scholar]
- 34.Sabat SR. Capacity for decision-making in Alzheimer's disease: selfhood, positioning and semiotic people. Aust N Z J Psychiatry. 2005;39(11-12):1030–5. doi: 10.1080/j.1440-1614.2005.01722.x. [DOI] [PubMed] [Google Scholar]
- 35.Defanti C, Tiezzi A, Gasparini Mf, et al. Ethical questions in the treatment of subjects with dementia. part I. respecting autonomy: awareness, competence and behavioral disorders. Neurological Sciences. 2007;28(4):216–31. doi: 10.1007/s10072-006-0825-x. [DOI] [PubMed] [Google Scholar]
- 36.Gevers S. Dementia and the law. European journal of health law. 2006;13(3):209–17. doi: 10.1163/157180906778852385. [DOI] [PubMed] [Google Scholar]
- 37.Dick C. Self-neglect: diogenes syndrome and dementia. Kans Nurse. 2006;81(9):12–3. [PubMed] [Google Scholar]
- 38.Dakin E, Pearlmutter S. Older women's perceptions of elder maltreatment and ethical dilemmas in adult protective services: a cross-cultural, exploratory study. J Elder Abuse Negl. 2009;21(1):15–57. doi: 10.1080/08946560802571896. [DOI] [PubMed] [Google Scholar]
- 39.François I, Moutel G, Plu I, Pfitzenmeyer P, Hervé C. Concerning mistreatment of older people: clinical and ethical thoughts based on a study of known cases. Archives of Gerontology and Geriatrics. 2006;42(3):257–63. doi: 10.1016/j.archger.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 40.Johnson TF. Ethics in addressing mistreatment of elders: can we have ethics for all? Generations. 2000;24(2):81. [Google Scholar]
- 41.Dong X. Advancing the field of elder abuse: future directions and policy implications. J Am Geriatr Soc. 2012;60(11):2151–6. doi: 10.1111/j.1532-5415.2012.04211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cohen M, Levin SH, Gagin R, Friedman G. Elder abuse: disparities between older people's disclosure of abuse, evident signs of abuse, and high risk of abuse. J Am Geriatr Soc. 2007;55(8):1224–30. doi: 10.1111/j.1532-5415.2007.01269.x. [DOI] [PubMed] [Google Scholar]
- 43.Anetzberger GJ. The reality of elder abuse. Clinical Gerontologist. 2005;28(1-2):1–25. [Google Scholar]
- 44.Melchiorre MG, Chiatti C, Lamura G. Tackling the phenomenon of elder abuse in Italy: a review of existing legislation and policies as a learning resource. Educational Gerontology. 2012;38(10):699–712. [Google Scholar]
- 45.Quinn MJ, Heisler CJ. The legal response to elder abuse and neglect. Journal of Elder Abuse & Neglect. 2004;14(1):61–77. [Google Scholar]
- 46.Daly JM, Merchant ML, Jogerst GJ. Elder abuse research: a systematic review. J Elder Abuse Negl. 2011;23(4):348–65. doi: 10.1080/08946566.2011.608048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meara NM, Schmidt LD, Day JD. Principles and virtues: a foundation for ethical decisions, policies, and character. The counseling psychologist. 1996;24(1):4–77. [Google Scholar]
- 48.Schwiebert VL, Myers JE, Dice C. Ethical guidelines for counselors working with older adults. Journal of Counseling & Development. 2000;78(2):123–9. [Google Scholar]
- 49.Healy TC. Ethical decision making: Pressure and uncertainty as complicating factors. Health Soc Work. 2003;28(4):293–301. doi: 10.1093/hsw/28.4.293. [DOI] [PubMed] [Google Scholar]
- 50.Rodríguez MA, Wallace SP, Woolf NH, Mangione CM. Mandatory reporting of elder abuse: between a rock and a hard place. Ann Fam Med. 2006;4(5):403–9. doi: 10.1370/afm.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gelfand DE, Kutzik AJ, editors. Ethnicity and Aging: Theory, Research, and Policy. USA: Springer Publishing Company; 1979. [Google Scholar]
- 52.Xu G, Meyer JS, Thornby J, Chowdhury M, Quach M. Screening for mild cognitive impairment (MCI) utilizing combined mini‐mental‐cognitive capacity examinations for identifying dementia prodromes. Int J Geriatr Psychiatry. 2002;17(11):1027–33. doi: 10.1002/gps.744. [DOI] [PubMed] [Google Scholar]
- 53.Heravi-Karimooi M, Rejeh N, Foroughan M, Ebadi A. Designing and determining psychometric properties of the elder neglect checklist. Iranian Journal of Ageing. 2013;8(3):25–34. [Google Scholar]
- 54.Ramazani RK. Constitution of the Islamic Republic of Iran. Middle East Journal. 1980;34(2):181–204. [Google Scholar]
- 55.Meghdadi MM, Delavari MH. The Civil Liability Due to Revealing Medical Secrets in Iran's Law and Common Law. Medical Law Journal. 2014;8(30):99–145. [Google Scholar]
- 56.Akbari MA, Ramezani A. The status of delinquent infants and children in Iran criminal law. Survey of Malaysian Law. 2017;14(2):104–13. [Google Scholar]