Abstract
Background
Transmission of Mycoplasma (M.) suis mainly occurs via iatrogenic or zootechnical manipulations or due to ranking fights. Other transmission routes including ingestion of secretes/excretes; blood-sucking arthropods and intra-uterine transmission have thought to play an epidemiological role without being experimentally proven. To investigate a vertical transmission of M. suis under field conditions blood samples from pre-suckling piglets and their corresponding dam were examined for M. suis by quantitative polymerase chain reaction (qPCR) in 21 farms in Southern Germany.
Results
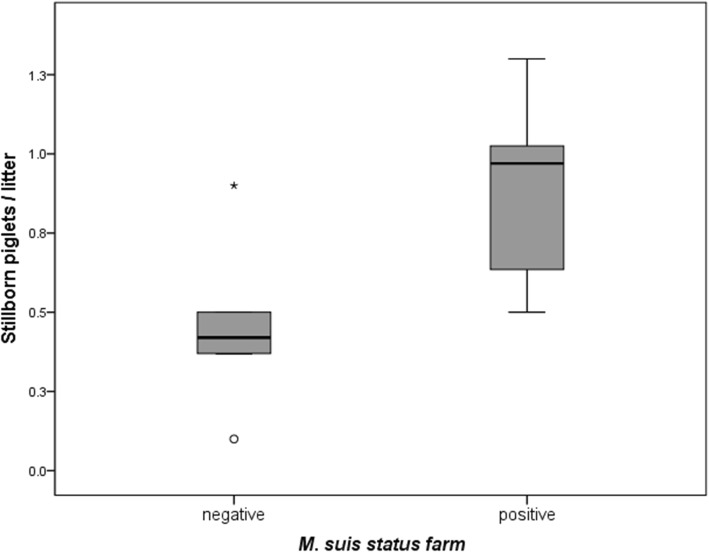
A total of 14.35% of the 474 blood samples from pre-suckling piglets reacted qPCR positive. Additionally, M. suis was detected in 65 (31.25%) of the 208 sows at farrowing. On farm level, 16 (76.2%) of the 21 farms had at least one M. suis positive animal. M. suis positive farms had an average of 0.41 more stillborn piglets per litter than M. suis negative farms (p = 0.007).
Conclusion
The present study provides further insights into M. suis infection dynamics as it is the first detection of M. suis in piglets immediately after birth prior to colostrum intake and the first large scale investigation of M. suis in sows at farrowing.
Keywords: Mycoplasma suis, Pre-suckling piglets, Vertical transmission
Background
M. suis, the causative agent of infectious anemia in pigs (IAP), is an important pathogen in modern intense pig production worldwide [1–5]. M. suis affects all age classes of pigs. In piglets, acute IAP manifests as life-threatening hemolytic anemia, general ill thrift, and hypoglycemia which could lead to acute death [2]. In sows, acute M. suis infections may cause sudden death due to hypoglycemic coma but also milder acute forms of the disease including decreased fertility, increased return to estrus and dysgalactia have been reported [1, 6–8]. However, main economic losses associated with M. suis infections in all age classes are related to chronic IAP with mild anemia, reduced growth rate, poor reproductive performance, increased antibiotic use and a higher susceptibility to secondary infections of the respiratory and enteric system [5].
M. suis belongs to the highly specialized group of hemotrophic mycoplasmas with special unique features including cell tropism to erythrocytes and endothelial cells, a reduced genome and a high metabolic host adaption [5, 9–12]. All previous efforts to cultivate M. suis in vitro have been unsuccessful so far, although a kind of maintenance after nanotransformation can be obtained in a cell free culture system [13].
Due to the inability to cultivate hemotrophic mycoplasmas, reliable prevalence data for M. suis are rare and restricted to the post-PCR era. Moreover, it is supposed that M. suis infections have been underdiagnosed due to the low sensitivity and specificity of former diagnostic methods like microscopic examination of blood smears coupled with whole blood which is rarely included in routine diagnostic submission, being the preferred sample type [6]. Nowadays, diagnostic of M. suis infection is mainly based on PCR techniques or serological examinations of relevant animal groups (whole cell ELISA or recombinant ELISAs) [4, 14–16]. In applying qPCR methods M. suis prevalence of 13.9 and 10.0% has been determined for weaned piglets and wild boars in Germany, respectively [3, 17] and of 18.2% in sows in Brazil [18]. Nevertheless, one key question that remains unknown is the introduction of M. suis into swine herds and the on-farm transmission between pigs. It is proven that transmission of infected blood occurs via iatrogenic or zootechnical procedures (vaccinations, contaminated needles, fixation procedures) or lacerations due to ranking fights within animal groups [19, 20]. Moreover, other transmission routes including ingestion of secretes and excretes, blood-sucking arthropods and intra-uterine transmission have thought to play an epidemiological role without however being experimentally proven [1, 7, 19, 21]. The aim of the present study was to determine the occurrence of vertical M. suis transmission from dams to their offspring under field conditions. Therefore, blood samples of sows at farrowing and their pre-suckling piglets were investigated by means of an M. suis-specific qPCR. Furthermore, the impact of M. suis infection on the piglet producing farms was evaluated by correlating the qPCR results to hematological findings as well as reproductive performance data.
Results
M. suis detection in sows at farrowing and pre-suckling piglets
In all farms no clinical signs of M. suis infections were obvious at the time of investigation. In 16 (76.2%) out of the 21 investigated farms M. suis was detected in at least one sow, in the remaining five farms (23.8%) all sows were qPCR-negative. On individual animal level, 31.25% (65 out of 208) of the sows were positive for M. suis. The number of M. suis positive sows within herds varied between 1 and 10 animals with a mean number of 3.05 (SD ± 2.99) positive sows per farm.
To investigate the vertical transmission of M. suis from sows to their offspring, all samples from pre-suckling piglets (n = 474) from the 16 M. suis positive farms with 65 M. suis positive sows and 94 M. suis negative sows were investigated for the presence of M. suis. Overall 68 (14.35%) of 474 pre-suckling piglets reacted qPCR positive. The 68 M. suis positive piglets originated from 47 litters. Table 1 gives an overview on the number of positive piglets according to the M. suis status of the sow in the 16 M. suis positive farms. Fifty (73.5%) piglets were born from 32 M. suis positive sows and 18 (26.5%) piglets from 15 sows that showed a PCR negative result at the time of sampling. Piglets born from a M. suis positive dam were significantly more often positive than piglets born from a M. suis negative dam (p < 0.001, OR: 3.8, 95% CI: 1.8, 8.5). Quantification of bacterial loads revealed a mean M. suis blood load of 3.15 × 107 M. suis/mL in sows (range.: 2.04 M. suis/mL to 1.94 × 109 M. suis/mL blood) and of 5.09 × 107 M. suis/mL blood in piglets, respectively (range: 1.02 M. suis/mL to 3.46 × 109 M. suis/mL blood). Bacterial blood loads of sows were associated with bacterial blood loads of piglets (p<0.001). No significant difference was observed between birth-weight of M. suis positive and negative pigs. The median birth weight was 1.35 kg for M. suis positive piglets and 1.40 kg for M. suis negative piglets. Furthermore, no significant association was found between the gender and the M. suis status of the piglet. Among the 65 M. suis positive sows, 7 sows originated from parity group 1, 31 sows from parity group 2 and 27 sows were in parity group 3. However, the parity of the sow was neither associated with the M. suis status of the sows nor with the number of positive piglets per sow.
Table 1.
Number of M. suis positive piglets per sows according to the M. suis status of the sow in the 16 M. suis positive farms
| Number of positive piglets per sow | M. suis positive sows (n = 65) | M. suis negative sows (n = 94) |
|---|---|---|
| 0 | 33 | 79 |
| 1 | 16 | 13 |
| 2 | 14 | 1 |
| 3 | 2 | 1 |
Immunoblot analysis
Sera from qPCR negative sows with M. suis positive piglets (n = 15) and from negative sows with M. suis negative piglets (n = 15) were investigated for the presence of M. suis-specific antibodies. Sera from all sows (100%) with M. suis positive piglets reacted positive in the M. suis-immunoblot, whereas only 1 of the 15 sows without M. suis positive piglets (6.66%) revealed a positive serological result. Detailed reaction patterns of the immunoblot-positive sows are given in Table 2.
Table 2.
Reaction patterns of all immunoblot positive sows
| M. suis specific antigena | qPCR negative sows with qPCR positive piglets (n = 15) | qPCR negative sow with qPCR negative piglets (n = 1) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16c | |
| p 83 | + b | |||||||||||||||
| p 73 | ||||||||||||||||
| p 70 | ||||||||||||||||
| p 61 | ||||||||||||||||
| p 57 | + | + | + | + | ||||||||||||
| p 45 | + | + | + | + | + | + | + | |||||||||
| p 40 | + | + | + | + | + | + | + | + | + | + | + | + | ||||
| p 33 | + | + | + | + | + | + | + | + | ||||||||
| p 31 | ||||||||||||||||
aM. suis antigen purified from experimentally infected animals at high bacteremia
bdistinct visible reactions with M. suis antigen and absent in the control antigen purified from the blood of M. suis negative sows
creaction pattern of the one immunoblot-positive sow of the control group. All other sera from the control group sows (n = 14) showed no reaction with any M. suis specific antigen and were thus not included in the table
Hematological findings and correlation between qPCR and hematological parameters
In the group of sows, no significant differences in hematological parameters (erythrocyte, leucocyte, PCV, hemoglobin and thrombocyte) could be observed between M. suis positive and M. suis negative animals. Additionally, no correlation between M. suis blood load of sows and hematological parameters was found. However, erythrocyte (p<0.001), PCV (p = 0.02) and hemoglobin count (p = 0.002) were negatively associated with the parity of the sow. M. suis positive piglets had significantly higher leucocyte counts (median: 6.49. g/l) than M. suis negative piglets (median: 5.60 g/l) (p<0.001). Additionally, birth weight was positively associated with leucocyte count (p = 0.001). The remaining hematological parameters (erythrocyte, PCV, hemoglobin and thrombocytes) did not differ significantly between M. suis positive and M. suis negative piglets. However, M. suis blood load of piglets was negatively correlated with erythrocyte count (r = − 0.243, p = 0.046) and positively correlated with leucocyte count (r = 0.548, p<0.001).
Reproductive parameters of M. suis positive and negative farms
Regarding reproductive parameters, sows on M. suis positive farms had significantly more stillborn piglets per litter (an average of 0.41 more) compared to M. suis negative farms (p = 0.007) (Fig. 1). Other evaluated reproductive parameters (i.e. live born piglets/sow, weaned piglets/sow, return to estrus rate) did not differ significantly between M. suis positive and negative farms.
Fig. 1.
Mean number of stillborn piglets per litter in M. suis positive and M. suis negative farms. Outliers are shown as O, extreme outliers as *
Discussion
This study reports the evidence of M. suis in sows at farrowing and their corresponding piglets without obvious clinical signs of infection at the time of investigation. However, M. suis is able to persist in asymptomatic carrier animals and reoccurrence of the disease can be provoked by immunosuppressive events (e.g. stress, transport, other infectious agents). Additionally, subclinically infected carrier animals can be regarded as the major reservoir of M. suis and play an important role in the epidemiology of infections [22]. The study involved a total of 208 sows from 21 piglet producing farms and 474 piglets from 16 M. suis positive farms. We found that 14.35% of the pre-suckling blood samples of newborn piglets from M. suis positive farms were qPCR positive indicating that the vertical route might play an important role in the transmission of M. suis within herds. Nearly 50% (32 out of 65) of the M. suis positive sows have born at least one M. suis positive piglet. This finding was unexpected because it is generally accepted that transmission of M. suis mainly occurs horizontally including an iatrogenic blood transfer due to contaminated instruments, small skin lesions due to hierarchy fights within animal groups or a transmission due to shedding via secretes and excretes [4, 19, 20]. So far, vertical transmission was discussed to play an epidemiological role without being experimentally proven. Only one previous study of Henderson et al. [7] suggested a vertical transmission as M. suis was detected in piglets shortly after birth but after colostrum intake and intensive contact between piglets and dam. Vertical transmission of hemotrophic mycoplasma has only been described so far in cattle [23, 24]. To the best of our knowledge, this is the first detailed study investigating M. suis infection in sows at farrowing and the potential vertical transmission of M. suis to piglets.
There are two main possibilities for the piglets to get infected: intra-uterine or due to blood or secret contact during birth passage (e.g. vaginal lesions or vaginal secret). The latter was supported by the detection of vaginal M. suis shedding in experimentally infected pigs [19]. However, according to the high M. suis mean blood load of 5.09 × 107 detected in piglets immediately after expulsion, amplification of the pathogen due to uptake of secretions or contamination with sow blood during parturition seems unlikely. Results from a previous experimental trial revealed lower mean M. suis blood loads of 1.35 × 103 and 5.36 × 105 on day 2 post infection in non splenectomized and splenectomized nursery pigs, respectively [2].
Basically, the M. suis blood loads found in the present study seem to be very high for both, the sows and the piglets. However, they are comparable to the loads found in 164 M. suis positive feeder pigs in Germany with a mean load of 7.62 × 107 M. suis/mL blood [3]. Interestingly, 18 M. suis positive piglets (26.5%) were born from PCR negative sows. However, we could detect M. suis specific antibodies in the sera of all M. suis negative sows with M. suis positive offspring indicating a prior exposure to M. suis or even a chronic M. suis infection with a bacterial blood load below the PCR detection limit of 10 M. suis per reaction [25]. Such an intermittent detection of M. suis has also been described previously [2]. Due to the high percentage of M. suis positive piglets derived from PCR positive sows it seems likely that the fetal outcome is dependent on the M. suis status of the sow. Future experimental studies are certainly needed to gain deeper insights into the mechanism by which M. suis transmits from the dam to her fetuses and to elucidate the pathogenesis of embryonal/fetal M. suis infection.
Twenty-one farms with 208 sows of different parities were included in the present study. The high detection rate of 76.2% M. suis positive piglet producing farms and 31.25% M. suis positive sows, indicates that subclinical M. suis-infection is widespread in clinically healthy sows. Comparable studies are rare. There is only one PCR based study in healthy sows from Brazil reporting 18.2% M. suis positive animals [18]. In feeder pigs 13.9% of the animals and 40.3% of the farms were M. suis PCR-positive in Germany [3]. Other studies on sows investigating M. suis-specific antibodies revealed inconsistent results including 59% seropositive sows in Portugal [26] as well as 39.2 to 40.6% seropositive replacement gilts and 47.0 to 48.2% seropositive multiparous sows in China, respectively [27, 28]. Various factors could be responsible for different prevalences, especially the chosen diagnostic method (PCR or serology) and the study design. One disadvantage of the PCR methodology used in the present study might be that, in contrast to pathogen isolation, non-viable bacteria can be detected. However, due to the lack of in vitro cultivation systems for M. suis and other hemotrophic mycoplasmas, PCR is currently the most sensitive detection method. Prevalence data can also be biased by other factors i.e. varying epidemiologic situation in different countries or the selected age group as M. suis prevalence is thought to increase with age [18, 26–28]. However, in contrast to Song et al. [28] who reported a higher prevalence in multiparous sows compared to gilts no parity dependent differences could be observed in our study. Additionally, the sampling point at farrowing might have influenced the detection rate of M. suis in our study as stress or immunosuppression is thought to increase the susceptibility for M. suis [4, 29].
Several clinical syndromes have been associated with M. suis infections in sows including acute and chronic anemia, pyrexia, anorexia, hypoglycemia, icterus but also reproductive disorders with decreased fertility, increased return to estrus, decreased number of live born and weaned piglets, abortion, mummies, and dysgalactia [1, 6]. In this study, clinical signs were not obvious at the time of investigation. However, the different courses of M. suis infections (acute, chronic or latent) are mainly dependent on endogenous or exogenous stress factors [22]. As clinical examination of sows was only performed once at the day of farrowing and reproductive performance was only assessed at farm level and not from individual animals further studies focusing on individual reproductive performance of M. suis positive sows are certainly needed. Additionally, no evidence linking M. suis infections to anemia in sows has been found. This lack of correlation is in accordance with Guimaraes et al. [18] who couldn’t determine significant differences in hematological parameters between infected and not infected sows. One possible explanation for non-observed differences in hematological parameters between positive and negative sows in the present study might be that alteration of hematological parameters in M. suis positive sows was overlaid by other factors eg. parity of the sow.
Interestingly, in the present study M. suis positive newborn piglets had significantly higher leucocyte counts than M. suis negative piglets and leucocyte counts were positively correlated with M. suis blood loads. Additionally, the negative correlation between M. suis blood loads and erythrocyte counts is in accordance with Ritzmann et al. [3] who showed that bacterial loads are significantly correlated with severity of anemia. The absence of obvious clinical signs in newborn piglets might also be attributed to the fact that in compliance with the German welfare legislation only clinically healthy piglets were included in the study. Further studies should focus on the clinical outcome of piglets born M. suis positive, particularly after stressing conditions (e.g. weaning).
In the present study M. suis positive farms had a significantly higher number of stillborn piglets compared to M. suis negative farms. Other reproductive parameters including return to estrus and number of live born/weaned piglets did not differ significantly between M. suis positive and negative farms. Reproductive performance of sows can be influenced by several infectious and non-infectious co-factors. Samples of the present study were also investigated for porcine circovirus type 2 resulting in a low prevalence in farrowing sows (1%) and no detection in suckling piglets as published by Eddicks et al. [30]. To investigate other potential coinfections that might influence the outcome of the present study samples were also examined for PRRSV indicating no link between PRRSV and M. suis infection (data not published). However, the higher number of stillborn piglets in M. suis positive farms must be interpreted cautiously as other infectious as well as non-infectious agents influencing reproductive parameter were not evaluated within the scope of this study.
Conclusion
In the present study the detection of M. suis in pre-suckling piglets indicates for the first time a potential vertical transmission of this pathogen. The high detection rate of M. suis in clinically healthy sows suggests that sows play a role in within herd transmission. Therefore, the present study increases our knowledge on M. suis infection dynamics and transmission, thus improving adequate and effective intervention strategies.
Methods
Sample and data collection
Out of a pool of 36 voluntary participating piglet producing farms 21 farms, regardless of their M. suis status, were randomly selected stratified by the density of piglet producing farms in Bavaria, Germany. The number of farms to sample was determined based on expert knowledge, average number of farms sampled in literature and considering financial and logistic constraints. The investigation of 200 sows allows the estimation of prevalence with accuracy up to ±7%. Accordingly, 10 sows per farm were sampled in the 21 selected farms. This kind of two stage cluster sampling is a frequently used sampling method that ensures high practicability and validity of observed data at the same time. On the other hand, the examination of 40 animals per farm allows the detection of a 10% minimal prevalence of M. suis DNA on a farm with a 98% confidence level. Therefore, 30 piglets per farm were sampled (three piglets per sow). The size of the farms varied between 100 and 840 sows with an average farm size of 294 sows. EDTA-anticoagulated blood samples and serum samples were collected from 9 or 10 sows at the time of farrowing from each farm (n = 208). Additionally, EDTA-anticoagulated blood samples were collected from three piglets of each sow (n = 622) before colostrum uptake as described by Eddicks et al. [30]. In accordance with the German animal welfare law only clinically healthy pre-suckling piglets were included in this investigation and subsequently piglets were raised as conventional pigs. To ensure that blood sampling of piglets was performed prior to the first suckling of the piglets the whole farrowing period was supervised by the investigators and piglets were sampled immediately after expulsion (< 30 s. between birth and sampling). Analysis of hematological parameters and qPCR analysis was performed from EDTA-anticoagulated blood samples. After analysis of hematological parameters EDTA-anticoagulated blood samples were stored at − 80 °C until further processing. Serum samples of sows were examined for M. suis specific antibodies by immunoblot analysis. Animal based data were collected including birth weigth and sex of each piglet. The parity group of each sow was recorded according to the following scheme: parity group 1 (gilts), group 2 (2nd-4th parity) and group 3 (≥5th parity) and sows were examined for obvious clinical signs of M. suis infection (anorexia, depression, anemia, icterus, pyrexia) at the day of farrowing. Additionally, reproductive parameters (return to estrus rate, live born piglets/sow/litter, stillborn piglets/sow/litter, weaned piglets/sow/year) were assessed at farm level on each farm. All procedures were performed in accordance with the German animal welfare law using a protocol officially approved by the appropriate authority (reference number: 55.2–154–2532.2-16-13).
DNA extraction
Two hundred microlitre of EDTA-anticoagulated blood samples were pre-treated as described previously [3, 31]. Afterwards, bacterial DNA was extracted from the samples using the GenElute™ Bacterial Genomic DNA Kit (Sigma-Aldrich, Steinheim, Germany) according to the manufacturer’s instructions. One PBS control was included in each DNA extraction run (1 control for 10 samples) to monitor for cross-contamination. DNA was stored at − 20 °C until use.
Quantitative SYBR green real time PCR
M. suis DNA was detected and quantified with the StepOne™ System (Applied Biosystems®) and the primers targeting the M. suis msg1: msg1-Fw 5'-ACAACTAATGCACTAGCTCCTATC-3' and msg1-Rv 5'-GCTCCTGTAGTTGTAGGAATAATTGA). Real-time PCR (qPCR) was performed by means of Fast SYBR® Green Master Mix (ThermoFisher Scientific) with 0.5 μM of each primer. The SYBR green PCR protocol comprised 95 °C for 10 min followed by 40 cycles of 95 °C for 15 s and 60 °C for 30 s. After each PCR a melting curve analysis was performed with melting temperatures of 76.0 ± 0.1 °C were considered as positive. Specificity testing of the SYBR green real time PCR assay was performed using DNA samples from the following bacteria: M. hyorhinis, M. hyopneumoniae, M. wenyonii, 'Candidatus M. haemobos', M. haemofelis, Salmonella Typhimurium, Escherichia coli, Pasteurella multocida, Streptococcus suis. Determination of the lower detection limit as well as quantification of M. suis blood loads in positive pigs was performed as described previously [25]. The detection limit of the SYBR green real time PCR assay was found to be 10 M. suis per PCR reaction.
Hematological and biochemical blood analyses
Hematological parameters including erythrocyte, hemoglobin, leucocyte and thrombocyte counts as well as packed cell volume (PCV), mean corpuscular volume (MCV), mean
corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration
(MCHC) were determined using the Vet Scil ABC tool (Scil Animal Care Company GmbH, Viernheim, Germany).
Immunoblot analysis
Serum samples were examined for antibodies against M. suis by immunoblot analysis as described by Hoelzle et al. [15]. Briefly, antigen preparations derived from M. suis-infected pigs and negative pigs were separated on sodium dodecyl sulfate-polyacrylamide gels according to their molecular weight and transferred to nitrocellulose membranes by standard methods. The immunoblots were probed with field sera from the sows diluted 1:100, horseradish peroxidase-labeled goat anti-pig IgG (Sigma-Aldrich), and with 4-chloro-1-naphthol as the chromogenic reagent. Immunoreactive protein bands were sized with reference to molecular size marker lanes (Page Ruler prestained Protein ladder, Thermofisher Scientific). Samples were considered positive if at least one of the three major immunogenic proteins p40, p45, and p70 was detected [15].
Statistical evaluation
Data were compiled and analyzed with Microsoft Office Excel 2013 and the statistic software IBM SPSS, Statistics 22.0 (IBM Corporation, USA) and RStudio (Version 1.1.453 with R Version 3.4.4.). A farm was considered positive if at least one animal tested positive. Data were tested for normal distribution using Kolmogorow Smirnow test. Multivariable analysis were carried out using linear mixed model (hematological parameters of piglets and sows, birth weight of piglets, bacterial load of sow and piglets) and logistic model (status sow, piglet, gender of the piglets, parity of the sows) accounting for repeated measures (farm and sow effect). Pearson correlation coefficient was used to determine a correlation between bacterial loads of sows respectively piglets and hematological parameters. The significance level of all statistical evaluations was 5% with a 95% confidence interval.
Acknowledgements
The authors wish to thank the colleagues from the Clinic for Swine who assisted at sample collection. The authors are grateful to the farmers who contributed to this study.
Abbreviations
- IAP
Infectious anemia in pigs
- M. suis
Mycoplasma suis
- MCH
Mean corpuscular hemoglobin
- MCHC
Mean corpuscular hemoglobin concentration
- MCV
Mean corpuscular volume
- PCV
Packed cell volume
- qPCR
Quantitative polymerase chain reaction
Authors’ contributions
JS participated in design of the study, wrote the ethical application, performed the study, analysed the data and drafted the manuscript. SW performed animal sampling and contributed to data analysis. ME reviewed the study protocol, assisted with performing the trial and with interpretation of the data and reviewed the manuscript. JA conducted qPCR and immunoblot analysis and assisted with analysis of the data. MR, KH and LEH designed the study protocol, reviewed the ethical application dossier and the manuscript and assisted with interpretation of the data. All the authors read, revised, and approved the final manuscript.
Funding
No funding was provided for the study.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Animal sampling was performed in accordance with the German animal welfare law using a protocol officially approved by the appropriate authority (reference number: 55.2–154–2532.2-16-13).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Julia Stadler, Phone: 004989218078900, Email: j.stadler@med.vetmed.uni-muenchen.de.
Stephan Willi, Email: Stephan.Willi@gmx.de.
Mathias Ritzmann, Email: Ritzmann@med.vetmed.uni-muenchen.de.
Matthias Eddicks, Email: M.Eddicks@med.vetmed.uni-muenchen.de.
Julia Ade, Email: julia.ade@uni-hohenheim.de.
Katharina Hoelzle, Email: Katharina.Hoelzle@uni-hohenheim.de.
Ludwig E. Hoelzle, Email: ludwig.hoelzle@uni-hohenheim.de
References
- 1.Messick JB. Hemotrophic mycoplasmas (hemoplasmas): a review and new insights into pathogenic potential. Vet Clin Pathol. 2004;33:2–13. doi: 10.1111/j.1939-165X.2004.tb00342.x. [DOI] [PubMed] [Google Scholar]
- 2.Stadler J, Jannasch C, Mack SL, Dietz S, Zols S, Ritzmann M, et al. Clinical and haematological characterisation of mycoplasma suis infections in splenectomised and non-splenectomised pigs. Vet Microbiol. 2014;172:294–300. doi: 10.1016/j.vetmic.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 3.Ritzmann M, Grimm J, Heinritzi K, Hoelzle K, Hoelzle LE. Prevalence of mycoplasma suis in slaughter pigs, with correlation of PCR results to hematological findings. Vet Microbiol. 2009;133:84–91. doi: 10.1016/j.vetmic.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Hoelzle LE. Haemotrophic mycoplasmas: recent advances in mycoplasma suis. Vet Microbiol. 2008;130:215–226. doi: 10.1016/j.vetmic.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 5.Hoelzle LE, Zeder M, Felder KM, Hoelzle K. Pathobiology of mycoplasma suis. Vet J (London, England : 1997) 2014;202:20–25. doi: 10.1016/j.tvjl.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 6.Strait EL, Hawkins PA, Wilson WD. Dysgalactia associated with mycoplasma suis infection in a sow herd. J Am Vet Med Assoc. 2012;241:1666–1667. doi: 10.2460/javma.241.12.1666. [DOI] [PubMed] [Google Scholar]
- 7.Henderson JP, O'Hagan J, Hawe SM, Pratt MC. Anaemia and low viability in piglets infected with Eperythrozoon suis. Vet Rec. 1997;140:144–146. doi: 10.1136/vr.140.6.144. [DOI] [PubMed] [Google Scholar]
- 8.Brownback A. Eperythrozoonosis as a cause of infertility in swine. Vet Med Small Anim Clin. 1981;76:375–378. [PubMed] [Google Scholar]
- 9.Groebel K, Hoelzle K, Wittenbrink MM, Ziegler U, Hoelzle LE. Mycoplasma suis invades porcine erythrocytes. Infect Immun. 2009;77:576–584. doi: 10.1128/IAI.00773-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sokoli A, Groebel K, Hoelzle K, Amselgruber WM, Mateos JM, Schneider MK, et al. Mycoplasma suis infection results endothelial cell damage and activation: new insight into the cell tropism and pathogenicity of hemotrophic mycoplasma. Vet Res. 2013;44:6. doi: 10.1186/1297-9716-44-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oehlerking J, Kube M, Felder KM, Matter D, Wittenbrink MM, Schwarzenbach S, et al. Complete genome sequence of the hemotrophic mycoplasma suis strain KI3806. J Bacteriol. 2011;193:2369–2370. doi: 10.1128/JB.00187-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neimark H, Johansson KE, Rikihisa Y, Tully JG. Proposal to transfer some members of the genera Haemobartonella and Eperythrozoon to the genus mycoplasma with descriptions of ‘Candidatus mycoplasma haemofelis’, ‘Candidatus mycoplasma haemomuris’, ‘Candidatus mycoplasma haemosuis’ and ‘Candidatus mycoplasma wenyonii’. Int J Syst Evol Microbiol. 2001;51:891–899. doi: 10.1099/00207713-51-3-891. [DOI] [PubMed] [Google Scholar]
- 13.Schreiner SA, Sokoli A, Felder KM, Wittenbrink MM, Schwarzenbach S, Guhl B, et al. The surface-localised alpha-enolase of mycoplasma suis is an adhesion protein. Vet Microbiol. 2012;156:88–95. doi: 10.1016/j.vetmic.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 14.Hoelzle K, Grimm J, Ritzmann M, Heinritzi K, Torgerson P, Hamburger A, et al. Use of recombinant antigens to detect antibodies against mycoplasma suis, with correlation of serological results to hematological findings. Clin Vaccine Immunol. 2007;14:1616–1622. doi: 10.1128/CVI.00345-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoelzle LE, Hoelzle K, Ritzmann M, Heinritzi K, Wittenbrink MM. Mycoplasma suis antigens recognized during humoral immune response in experimentally infected pigs. Clin Vaccine Immunol. 2006;13:116–122. doi: 10.1128/CVI.13.1.116-122.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu J, Zhou D, Cheng Z, Wang Z, Wang L, Wang S, et al. Development and evaluation of enzyme-linked immunosorbent assay based on recombinant inorganic pyrophosphatase gene antigen for the detection of mycoplasma suis antibodies. Res Vet Sci. 2012;93:48–50. doi: 10.1016/j.rvsc.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Hoelzle K, Engels M, Kramer MM, Wittenbrink MM, Dieckmann SM, Hoelzle LE. Occurrence of mycoplasma suis in wild boars (Sus scrofa L.) Vet Microbiol. 2010;143:405–409. doi: 10.1016/j.vetmic.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 18.Guimaraes AM, Biondo AW, Lara AC, Messick JB. Exploratory study of mycoplasma suis (Eperythrozoon suis) on four commercial pig farms in southern Brazil. Vet Rec. 2007;160:50–53. doi: 10.1136/vr.160.2.50. [DOI] [PubMed] [Google Scholar]
- 19.Dietz S, Mack SL, Hoelzle K, Becker K, Jannasch C, Stadler J, et al. Quantitative PCR analysis of mycoplasma suis shedding patterns during experimental infection. Vet Microbiol. 2014;172:581–585. doi: 10.1016/j.vetmic.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 20.Henry SC. Clinical observations on eperythrozoonosis. J Am Vet Med Assoc. 1979;174:601–603. [PubMed] [Google Scholar]
- 21.Prullage JB, Williams RE, Gaafar SM. On the transmissibility of Eperythrozoon suis by Stomoxys calcitrans and Aedes aegypti. Vet Parasitol. 1993;50:125–135. doi: 10.1016/0304-4017(93)90013-D. [DOI] [PubMed] [Google Scholar]
- 22.Hoelzle LE, Felder KM, Hoelzle K. Porcine eperythrozoonosis: from Eperythrozoon suis to mycoplasma suis. Tierarztl Prax Ausg G Grosstiere Nutztiere. 2011;39:215–220. doi: 10.1055/s-0038-1623062. [DOI] [PubMed] [Google Scholar]
- 23.Sasaoka F, Suzuki J, Hirata T, Ichijo T, Furuhama K, Harasawa R, et al. Vertical transmission of mycoplasma wenyonii in cattle, supported by analysis of the ribonuclease P RNA gene - short communication. Acta Vet Hung. 2015;63:271–274. doi: 10.1556/004.2015.025. [DOI] [PubMed] [Google Scholar]
- 24.Girotto-Soares A, Soares JF, Bogado ALG, de Macedo CAB, Sandeski LM, Garcia JL, et al. ‘Candidatus mycoplasma haemobos’: Transplacental transmission in dairy cows (Bos taurus) Vet Microbiol. 2016;195:22–24. doi: 10.1016/j.vetmic.2016.08.020. [DOI] [PubMed] [Google Scholar]
- 25.Hoelzle LE, Helbling M, Hoelzle K, Ritzmann M, Heinritzi K, Wittenbrink MM. First LightCycler real-time PCR assay for the quantitative detection of mycoplasma suis in clinical samples. J Microbiol Methods. 2007;70:346–354. doi: 10.1016/j.mimet.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 26.Perestrelo-Viera R, Heinritzi K, Perestrelo-Vieira H, Sobestiansky J, Abreu-Lopes JA. Eperythrozoon suis - first diagnosis in intensive pig units in Portugal. Rev Portuguesa Ciencias Vet. 1997;92(521):14–19. [Google Scholar]
- 27.Zhongyang L, Jiansong Z, Yijuan S, Yuting X, Yufeng L, Jiarong X. Seroprevalence of mycoplasma suis infection in pigs in eastern China as estimated by a blocking enzyme-linked immunosorbent assay. Can J Vet Res. 2017;81:313–317. [PMC free article] [PubMed] [Google Scholar]
- 28.Song Q, Zhang W, Song W, Liu Z, Khan MK, He L, et al. Seroprevalence and risk factors of mycoplasma suis infection in pig farms in Central China. Prev Vet Med. 2014;117:215–221. doi: 10.1016/j.prevetmed.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Heinritzi K. Eperythrozoon infection in swine as a disease factor. Berl Munch Tierarztl Wochenschr. 1989;102:337–342. [PubMed] [Google Scholar]
- 30.Eddicks M, Koeppen M, Willi S, Fux R, Reese S, Sutter G, et al. Low prevalence of porcine circovirus type 2 infections in farrowing sows and corresponding pre-suckling piglets in southern German pig farms. Vet Microbiol. 2016;187:70–74. doi: 10.1016/j.vetmic.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 31.Hoelzle LE, Adelt D, Hoelzle K, Heinritzi K, Wittenbrink MM. Development of a diagnostic PCR assay based on novel DNA sequences for the detection of mycoplasma suis (Eperythrozoon suis) in porcine blood. Vet Microbiol. 2003;93:185–196. doi: 10.1016/S0378-1135(03)00040-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.