Abstract
A Depression is a prevalent mental healthcare problem and a common cause of disability worldwide. The purpose of this study was to determine the prevalence and risk factors of depression in individuals living in the UAE. We used a systematic review approach, searching PubMed and Scopus electronic databases to collect studies conducted between 2007 and 2017 on the UAE population (both citizens and expatriates) relating to depression. After evaluating and screening relevant articles, a review of 14 articles was conducted. The prevalence of depression and study populations varied widely across studies with some including students and workers and others limited to those with diabetes. The most common contributing factors were female sex, financial difficulties/low socioeconomic status, stressful life events, lack of social support, serious or chronic illness (e.g., diabetes, obesity, epilepsy, multiple sclerosis), and a history of eating disorders. Vitamin D deficiency was also highlighted as a risk factor for seasonal depression. Even though previous evidence has promulgated the role of numerous causative factors, the epidemiological studies including risk factors such as personal or family history of depression, low academic performance, and the use of alcohol remain lacking. Further research is needed to identify effective strategies for treating and preventing depression in the future.
Keywords: Depression, Prevalence, Risk Factors, Prevention and Control, Epidemiology, United Arab Emirates
Introduction
Mental disorders often pose a significant social and financial burden on individuals, families, and society as a whole. Depression is a predominant illness characterized by the loss of interest in activities that an individual usually enjoys and persistent sadness often accompanied by an inability to undertake daily activities.1 According to the World Health Organization (WHO), the proportion of the global population suffering from depression in 2015 was estimated to be 4.4%. Depression usually strikes more recurrently at a younger age and is more common among females (5.1%) than males (3.6%).2 However, the reasons are speculative, and research is inconclusive — hormonal fluctuations, and cultural influences have been suggested as possible causes. Epidemiological studies in the Middle East and North Africa regions have demonstrated depression rates ranging from 13 to 18%.3-7 Rates of depression in women are up to double than those in men.8 In the Gulf and Arab regions, the prevalence of depression varies substantially between published studies.9 A study conducted in Egypt on female adolescents demonstrated the prevalence of depression to be 15.3%, while in Omani high school students the prevalence was 17%, and 33.4% in Saudi Arabia.10-12
Among the population in the UAE, depression is a significant healthcare concern as it causes functional impairment, increased medical costs, and medical symptom burden.13 According to the Global Burden of Disease study (2010), in the UAE, the top three causes of disability-adjusted life years were major depressive disorder, road injury, and ischemic heart disease.14
Depression is a leading cause of death and morbidity. Depression is a major source of distress and can have a profound impact on the quality of life.15 Early treatment and identification of depression reduces the burden on caregivers and family member along with medical costs.16 A study conducted by Weyerer et al,17 suggested that depressive symptoms observed in the elderly are associated with advancing age, living alone, being female, low education level, divorce, comorbid physical illness, functionality disorder, alcohol and cigarette use, and lower level cognitive dysfunction.17 Another meta-analysis indicated that the existence of chronic illness and perception of low health increased depression risk.18 While females with high perceptions of economic concerns, low functionality conditions, as well as low life satisfaction were reported to be more depressive.19
The prevalence and epidemiological data of patients with depression are limited. Having this data is useful to assist policy development as well as plan and mobilize government mental health initiatives aimed at early interventions and screening. To date, a comprehensive review of depression has not been performed with respect to its burden and risk factors. Therefore, our study aimed to synthesize scientific information about the prevalence and risk factors of depression in the UAE.
Literature search
We conducted a systematic review of electronic databases to identify literature published on depression between January 2007 and December 2017. We used keywords and standard vocabulary including ‘depression’; ‘prevalence’; ‘risk factors’; ‘epidemiology’; ‘United Arab Emirates’; ‘Dubai’; ‘Ras Al Khaimah’; ‘Abu Dhabi’; ‘Ajman’; ‘Al Ain’; ‘Sharjah’; ‘Fujairah’; and ‘Umm Al Quwain’. The search was conducted using PubMed and Scopus databases. Boolean operators were used to link individual keywords and identify papers relating specifically to the subject area. Cross reference list of the relevant studies and local journals were also scanned to extract relevant articles to broaden and ensure a detailed literature search.
The review included original research papers published in peer-reviewed journals focusing on UAE population (both citizens and expatriates) and studies that had a direct impact on determining the prevalence and risk factors of depression. All literature conducted before 2007, on non-UAE populations, having unclear methods and study design, secondary articles (viewpoints, reviews, or editorials), studies with insufficient information reporting the risk factors and prevalence of depression were excluded from the analysis. No language restriction was applied.
Following a comprehensive review of 31 articles, the search culminated in the selection of 14 articles, conducted in different regions of the UAE [Figure 1]. The articles selected were predominantly concerned with the risk factors and prevalence of depression. Lastly, the eligible full-text articles were evaluated. This systematic review was performed as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.20 Characteristics of the studies are summarised in Table 1.
Figure 1.
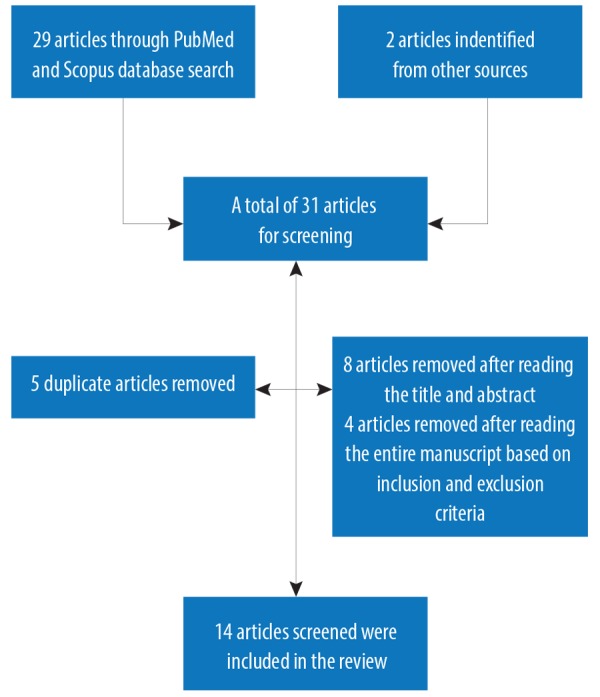
Flow chart of systematic review selection.
Table 1. Published papers on the prevalence and risk factors of depression in UAE from 2007–2017.
| Author/year/reference | Aim | Study design | Settings | Study population | Key findings | Future implications or study recommendations |
|---|---|---|---|---|---|---|
| Hamdan et al. 200821 |
Correlates and prevalence of depressive symptoms. | Cross-sectional study | Primary health care centers of Sharjah | 224 Arab women (aged 18 and above) | Prevalence, 33%: 14.7% moderately depressed and 18% severely depressed. Risk factors: Stressful life events. |
Intervention and prevention programs need to be developed in the future to address the mental health needs of Arab females. |
| Ahmed et al. 200922 |
Depression phenomenology and anxiety among medical doctors. | Cross-sectional study | Government hospitals (3), primary health care centers (3), and the students (all years) and staff of Dubai Medical College for Girls | 165 medical students and 93 doctors | Medical students: 28.7% presented anxiety; 28.6% exhibited depression (second-year students showing the highest anxiety and depression). Medical staff: 2.2% showed anxiety; 7.8% exhibited depression. |
More improved research designs are needed to illuminate the factors leading to anxiety and depression. |
| Al-Maskari et al. 201123 |
Suicidal behaviors and depression among male migrant workers. | Cross-sectional study | Labor camps, Al Ain city |
319 contacted workers; 239 fully completed the Depression, Anxiety and Stress Scales (DASS-42) | Prevalence score3 10 (depression) = 25.1% (60/239). Thoughts of suicide: 6.3% (20/261). Attempted suicide: 2.5% (8/265). Risk factors: Physical illness (97/301), less salary (203/314), working more than eight hours (213/315), and working in the construction industry (124/304). |
Implementation and interventions at policy levels are needed to improve working conditions, such as working hours and minimum wages regulation. |
| Sulaiman et al. 201024 |
Psychological distress prevalence and its correlates. | Cross-sectional study | Mini-clinics (primary health care centers), Sharjah hospitals |
347 diabetic; (65.4%) females | Approximately 12.5% of patients obtained a score of 19 or above (cut-off score) on the K6 questionnaire, indicating possible mental health concerns. 24% demonstrated diabetes complications. Mental health status and diabetic complications are strongly associated. |
Mental health needs improvement in comprehensive diabetes management plans to improve the long-term outcomes of these patients. |
| Ghubach et al. 201025 |
Association of physical and psychiatric disorders on life satisfaction. | Qualitative face to face interviews | UAE | 610 adults; > 60 years (347 males and 263 females) |
Depression (20.2%), anxiety (5.6%), hypochondriasis (4.4%), and organic brain syndrome with/ without dementia (3.6%). Depressive disorder was associated significantly with less life satisfaction. |
There is a need to develop interventions that help elderly patients deal more effectively with psychiatric disorders as well as its comorbidities. Family support is key to prevent this condition among the older population. |
| Mellal et al. 201426 |
Determine the prevalence of depression. | Cross-sectional study | Al Ain | 700 university students | Depression prevalence: 22.2%. Risk factors: Socioeconomic determinants: age (highest rate observed in the 17–25 age group), financial difficulties, overweight, and obesity. |
Mental health screening services should be offered to university students to identify individuals at a higher risk of developing depression. |
| Alsaadi et al. 201527 |
Depression and anxiety patients were screened to determine the rates of these conditions in patients with epilepsy and multiple sclerosis. | Cross-sectional study | Epilepsy and multiple sclerosis clinics in Abu Dhabi | 186 depressive patients and 160 with anxiety (aged 18–65 years) |
Epileptic patients were at a higher risk of depression. Anxiety and depression are probably encountered more frequently in epilepsy patients. |
Multicenter studies with a larger sample are needed in the future to confirm the shared pathogenic mechanisms between depression and epilepsy. |
| Alsaadi et al. 201528 |
The rates of anxiety and depression among epileptic patients were compared with the age- and sex-matched controls using standardized screening tools. |
Cross-sectional study | Epilepsy clinic (Sheikh Khalifa Medical City, UAE) | 186 patients | One-third of patients scored under the range of depression and anxiety. Two-thirds of patients with anxiety and depression did not prescribe to antianxiety or antidepressant medications. Epilepsy patients had an almost two-fold greater risk of having anxiety disorders and depression compared with controls. |
During the evaluation of epilepsy in all neurology clinics, screening for these strongly correlated conditions should be an adopted protocol. |
| Hawamdeh et al. 201329 |
To investigate the socio-demographic characteristics of UAE diabetic and depressed women; To explore the difference between non-depressed and depressed with regards to glycemic control. |
Cross-sectional study | UAE | 182 women; 92 with diabetes | Higher depression incidence was found in diabetic women than non-diabetic women. A positively significant relationship was found between higher depression levels and poor glycemic control. In UAE diabetic women sample, depression levels and national status were correlated; half showed poor glycemic control (HbA1C levels > 7.5). |
Early depression detection among women is essential to increase the adherence to treatment regimens and glycemic control. |
| Schulte et al. 201330 |
Relationship between body dissatisfaction, eating pathology symptoms, and depression was investigated. | Cross-sectional study | UAE | 361 (284 females, 77 males) undergraduates | Three quarters (73%) of the sample indicated body dissatisfaction (78% of females, 58% of males) and 20% scored above the clinical cutoff on the eating pathology scale (20% of females, 22% of males) In both genders, the depressive symptoms significantly predicted higher levels of eating pathology. |
Adequate prevention strategies locally should address the needs for both males and females, and potential depressive comorbidity should also be considered. |
| Alsaadi et al. 201731 |
To explore the potential factors that impact health-related quality of life among patient with epilepsy. | Cross-sectional study | Sheikh Khalifa Medical City | 160 epileptic adult patients | Depression, followed by seizure freedom, were known to be strongly correlated with health-related quality of life. | Screening for comorbid psychiatric disorders needs to be a crucial component of care standards, as well as an integrated plan of treatment for all patients suffering epilepsy. |
| Gariballa et al. 201832 |
To explore the impact of low muscle function measure by handgrip strength on the mental health of old individuals during recovery and acute illness. | Cross-sectional study | UAE | 432 randomly selected hospitalized older patients | 79% (308) had low muscle strength at baseline. After adjustment for gender, disability, age, comorbidities (including the severity of acute illness and body mass index), patients with low muscle strength had worse cognitive function, quality of life, and higher depression symptoms compared with those with normal muscle strength over six months. (p < 0.05). |
Clinical trials on humans in the future are needed to combine research with cellular and molecular investigations to understand the association between mental functions and muscles. Also, the role of optimizing dietary intake should be explored including protein and increase physical activity particularly following acute illness on muscle and mental functions in aging patients. |
| Thomas et al. 201133 |
To explore the relationship between mood and vitamin D deficiency. | Cross-sectional study | Students in Zayed University in Abu Dhabi, UAE | 197 female undergraduate students | Depressive symptoms peak during the summer months. Seasonal variations in the severity of depressive symptoms were observed. The mean depression scores of summer cohorts (16.85 ± 11.25) being higher than winter cohort (13.98 ± 7.98). |
Prevention of depressive illness and mental health promotion are warranted in future. |
| Thomas et al. 201834 |
Association between depressive symptoms and vitamin D deficiency. | Controlled pilot study | UAE citizens from a University in Abu Dhabi | 114 college women | Positive findings were observed for depressive symptoms. Behavioral activation and sun exposure are effective strategies to alleviate depressive symptoms and status of vitamin D deficiency. |
Sun exposure and behavioral activation appear to be a promising intervention. |
UAE: United Arab Emirates.
Fourteen studies met the inclusion criteria, including 12 cross-sectional studies, one randomized controlled pilot study, and one qualitative interview. Of these, six studies21-26 reported on depression prevalence and 11 reported on depression risk factors [Table 1].21,23,26-34
Prevalence
Two studies looking at the prevalence of depression were conducted in Sharjah,21,24 two in Al Ain,23,26 one in Dubai,22 and one was a national qualitative study that included different regions of the UAE.25 Prevalence scores ranged widely from 12.5–28.6% due to wide-ranging sample sizes. A cross-sectional study conducted in 2008 across primary health care centers of Sharjah including 224 Arab women indicated that 33% of women suffered depression symptoms of which 14.7% were moderately depressed and 18% were severely depressed.21 Another similar study conducted in 2010 across mini-clinics of primary health care centers in Sharjah reported the prevalence of depression in 347 diabetic patients (65.4% females).24 On an estimate, 12.5% of patients obtained a score of 19 or above (cut-off score) on the K6 questionnaire (a screening tool), while 24% had diabetes complications, mainly in the form of peripheral vascular disease, retinopathy, and peripheral neuropathy.24 The prevalence of depression among university students was estimated to be 22.2% in one study.26 The findings of an earlier study also demonstrated a prevalence of 25.1% among male migrant workers in the labor camps of Al Ain.23 The migrant workers included different nationalities including Indians (43.7%), Pakistanis (41.8%), Bangladeshis (9.2%), non-national Arabs (2.8%), and others (2.5%). The highest depression prevalence was noted among laborers from Bangladesh (40%), followed by non-national Arabs (37.5%), Pakistanis (30%), and Indians (13.8%). The highest prevalence of suicidal thoughts was reported by laborers from Pakistan (12.4%) compared to their counterparts from Indian sub-continent such as India (1.6%), and Bangladesh (0%). Ahmed et al,22 in 2009 conducted a cross-sectional survey recruiting 165 Dubai Medical College for girls medical students and 93 doctors from different government hospitals, colleges, and primary health care centers of Dubai; 28.6% of the medical students exhibited depressive symptoms, while only 7.8% of the medical staff reported suffering from depressive symptoms. The findings from a larger national qualitative interview study that enrolled 610 older adults reported that 20.2% suffered depressive symptoms.25 Depressive disorder was significantly associated with less life satisfaction.
Risk factors
Risk factors of depression studies (n = 11) explored financial difficulties, female sex, lack of social support, stressful life events, serious or chronic illness (e.g., diabetes, obesity, epilepsy, multiple sclerosis), and history of eating disorders [Table 1]. Of the 11 studies, all were cross-sectional except for one randomized controlled pilot study. The risk factor studies (n = 11) were conducted in different UAE states, including Al Ain, Sharjah, Dubai, and Abu Dhabi.
Psychosocial correlates of depressive symptoms among Arab women included having experienced stressful life events.21 Another study conducted on male migrant workers demonstrated an association between depression and long working hours and less salary.23 Moreover, construction workers may have conditions affecting their mood including burnout and depression. Furthermore, suicidal ideation is generally associated with depression and other mood disorders. Socioeconomic determinants of depression such as financial stress/difficulties and being overweight/obese were reported as significant risk factors.26 A common finding reported in some studies was that people who suffer from a chronic disease (e.g., epilepsy,27,28,31 multiple sclerosis,27 diabetes,29 eating disorders,30 and low muscle strength32) are more likely to suffer from depression. Depression can, therefore, lead to poor mental and physical functioning, leaving the patients less likely to follow required medication and diet plans for their chronic condition. However, treating their depression can give patients the ability to manage their chronic illnesses and improve health-related quality of life.31
A possible role for vitamin D in depression has also received considerable attention. Epidemiological evidence from the two other cross-sectional and pilot studies reviewed demonstrated an association of vitamin D deficiency with an elevation in depression.33,34
Discussion
The most significant risk factors involved included female sex, familial history of chronic diseases, financial difficulties/low socioeconomic status, stressful life events, and lack of social support.
The prevalence of depression reported in previous studies conducted in the UAE varies from 12.5–28.6% due to various population characteristics or differences in methodology. These findings are inconsistent with studies carried out on general population in the US, which reported a depression rate of 9% (range 6–12%).35 Previously conducted US-based studies reported a low prevalence compared with our results mostly among the young population. This may be because the young population tend to experience more stress concerning their future/employment and may be less pleased with their studies.36 Our results revealed that 28.6% of medical students22 and 22.2% of university students exhibited depression.26 Thus, being a student is a predisposing factor to depression (mainly due to lack of family support, financial difficulty, anxiety, and stressful events).
One of the most important determinants for depression was female gender. These findings correspond well to the literature, which suggests that women demonstrate a higher risk for depression compared to men. A comparable study conducted in Al Ain in 2002 found that lifetime rates of depression were 2.5% in males and 9.5% in females.37 In Arab countries, there is also evidence of this trend.29 The reasons for this difference are yet unknown. The results of comparable female to male prevalence ratios globally and across developed countries show that the differential risk may principally stem from biological sex differences and depend less on education, diet, culture, race, and other potentially confounding economic and social determinants.38
Other important risk factors found in this study are related to socioeconomic factors including stressful environments, financial problems, perceived low social status, greater daily stress leading to burnout in organizations and other cultural factors that may also play a substantial role in causing depression. Previous studies39-41 suggested that socioeconomic status and social support has a direct association with depressive symptoms. Al-Maskari et al,23 reported the same, signifying that migrant workers employed in the construction industry are most likely to be at risk.
Depression has also been associated with increased disease-related mortality and morbidity. This observation is consistent with previous evidence demonstrating that medical illnesses such as heart disease, stroke, cancer, and diabetes can increase the risk of depression.4 Our current review included studies showing an association between depression and epilepsy,27,28,31 multiple sclerosis,27 diabetes,29 eating disorders,30 and low muscle strength.32 Depression in individuals with physical and chronic illness is prevalent, which may adversely affect the course of disease in terms of functional impairments, health-related quality of life, and mortality.31 To identify depressive patients effectively, those with chronic illnesses should be identified at an early stage of the disease. Hence, patients with a higher risk of depression should be managed and monitored closely via comprehensive interventions composed of effective antidepressant treatments (based on drug interactions and adverse effects in terms of physical disorders treatment) along with supportive, collaborative care.
One potential contributing factor to women in Arab countries having depression and type 2 diabetes mellitus is vitamin D deficiency.
Two of the studies in the present review demonstrated an association between depression and vitamin D deficiency.33,34 Depressive symptoms were positively correlated with 25-hydroxyvitamin D (25(OH)D) levels. Seasonal variation was assessed for both vitamin D levels and depressive symptoms. The summer cohort having the highest levels of vitamin D deficiency reported greater levels of depressive symptomatology.33 Other international studies also report lower serum vitamin D level in individuals with psychological problems than those without.42
The role of government
The government of UAE has made remarkable and outstanding progress in reducing the impact of depression on the lives of the UAE population by supporting early recognition, appropriate treatment, and recovery. The government is also raising sufficient awareness through social marketing campaigns on the subject and delivering quality education across the emirates.43 This has encouraged people to seek treatment and become more responsive to depression.
The Ministry of Health and Prevention UAE is effectively supporting research and its dissemination, expertly conducting surveillance on mental health trends in the population, Mental Health Gap Action Programme by advocating integration of mental health into the primary and secondary health care and the capacity of the primary health care has also been strengthened to deliver excellent mental health programs and services.44 Another step towards this would be to develop registries on mental disorders within hospitals to collect systematic information over time to enable service improvements and quality healthcare for all.
Limitations
Although efforts were made to retrieve all relevant articles for inclusion in this review, we cannot be sure that all articles were found. Substantial statistical heterogeneity across studies was reported. We also tried to minimize bias by searching local and governmental reports and requesting the full-text relevant articles. Moreover, findings from cross-sectional studies do not inevitably indicate causality.
This is the first review, to our knowledge, to report the prevalence of depression and its associated determinants in the UAE. The findings of this review can be used by qualified professionals to formulate policies and identify gaps in research to better detect and manage late-life depression. The review also enclosed a thoughtful number of articles from all emirates. Local journals were carefully reviewed to include all articles related to the UAE. We also included cross-references from all included evidence to extract relevant articles to broaden and ensure a detailed literature search.
Conclusion
Depression is a common mental disorder that causes human distress and large costs to society. Our review highlights the overall prevalence of depressive symptoms and depression, which may have long been overlooked. Depression tends to adversely impact individual’s quality of life. Males are less likely to suffer from depression than females. Psychosocial factors were reviewed to have a significant role in perpetuating and precipitating depressive illness; traumatic/stressful life events being the most prevalent factor followed by low socioeconomic status, financial issues, social failure, and serious or chronic illness. Our review lays the foundation for policymakers, clinicians, and researchers to develop effective strategies for managing depression. Clinical interventions that target disordered eating, ways to cope in a more social setting, interpersonal effectiveness, body image dissatisfaction, and experience of stigma, may be useful in treating and preventing depression, given that they appear to be consistent risk factors. Further research is needed to identify effective strategies for treating and preventing depression among the elderly population.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
References
- 1.Fekadu N, Shibeshi W, Engidawork E. Major depressive disorder: pathophysiology and clinical management. J Depress Anxiety 2017;6(1):255-257 . 10.4172/2167-1044.1000255 [DOI] [Google Scholar]
- 2.WHO. (2017). Global Health Estimates; Depression and other common mental disorders. [cited 2018 January 25]. Available from: http://apps.who.int/iris/bitstream/10665/254610/1/WHO-MSD-MER-2017.2-eng.pdf.
- 3.Eloul L, Ambusaidi A, Al-Adawi S. Silent epidemic of depression in women in the Middle East and North Africa region: emerging tribulation or fallacy? Sultan Qaboos Univ Med J 2009. Apr;9(1):5-15. [PMC free article] [PubMed] [Google Scholar]
- 4.Ghubash R, Hamdi E, Bebbington P. The Dubai Community Psychiatric Survey: acculturation and the prevalence of psychiatric disorder. Psychol Med 1994. Feb;24(1):121-131. 10.1017/S0033291700026891 [DOI] [PubMed] [Google Scholar]
- 5.Afifi M, Al Riyami A, Morsi M, Al Kharusil H. Depressive symptoms among high school adolescents in Oman. East Mediterr Health J 2006;12(Suppl 2):S126-S137. [PubMed] [Google Scholar]
- 6.Okasha A, Kamel M, Sadek A, Lotaif ZB. Psychiatric morbidity among university students in Egypt. Br J Psychiatry 1977. Aug;131:149-154. 10.1192/bjp.131.2.149 [DOI] [PubMed] [Google Scholar]
- 7.Kilzieh N, Rastam S, Maziak W, Ward KD. Comorbidity of depression with chronic diseases: a population-based study in Aleppo, Syria. Int J Psychiatry Med 2008;38(2):169-184. 10.2190/PM.38.2.d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Strategy for mental health and substance abuse in the Eastern Mediterranean Region 2012–2016.
- 9.Al-Busaidi Z, Bhargava K, Al-Ismaily A, Al-Lawati H, Al-Kindi R, Al-Shafaee M, et al. Prevalence of depressive symptoms among university students in Oman. Oman Med J 2011. Jul;26(4):235-239. 10.5001/omj.2011.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khalil AH, Rabie MA, Abd-El-Aziz MF, Abdou TA, El-Rasheed AH, Sabry WM. Clinical characteristics of depression among adolescent females: a cross-sectional study. Child Adolesc Psychiatry Ment Health 2010. Oct;4:26. 10.1186/1753-2000-4-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Afifi M, Al Riyami A, Morsi M, Al Kharusil H. Depressive symptoms among high school adolescents in Oman. East Mediterr Health J 2006;12(Suppl 2):S126-S137. [PubMed] [Google Scholar]
- 12.Asal AR, Abdel-Fattah MM. Prevalence, symptomatology, and risk factors for depression among high school students in Saudi Arabia. Neurosciences (Riyadh) 2007. Jan;12(1):8-16. [PubMed] [Google Scholar]
- 13.Levine DS, Sripada RK, Ganoczy D, Walters H, Gorman LA, Valenstein M. Poorer physical health is associated with greater mental health service utilization in a sample of depressed US Army National Guard soldiers. Mil Med 2016. Aug;181(8):803-810. 10.7205/MILMED-D-15-00287 [DOI] [PubMed] [Google Scholar]
- 14.GBD. GBD Profile: United Arab Emirates, 2010. [cited 2018 January 25]. Available from: http://www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_united_arab_emirates.pdf.
- 15.Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health 2013;34:119-138. 10.1146/annurev-publhealth-031912-114409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zivin K, Wharton T, Rostant O. The economic, public health, and caregiver burden of late-life depression. Psychiatr Clin North Am 2013. Dec;36(4):631-649. 10.1016/j.psc.2013.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weyerer S, Eifflaender-Gorfer S, Köhler L, Jessen F, Maier W, Fuchs A, et al. German AgeCoDe Study group (German Study on Ageing, Cognition and Dementia in Primary Care Patients) Prevalence and risk factors for depression in non-demented primary care attenders aged 75 years and older. J Affect Disord 2008. Dec;111(2-3):153-163. 10.1016/j.jad.2008.02.008 [DOI] [PubMed] [Google Scholar]
- 18.Chang-Quan H, Zheng-Rong W, Yong-Hong L, Yi-Zhou X, Qing-Xiu L. Education and risk for late life depression: a meta-analysis of published literature. Int J Psychiatry Med 2010;40(1):109-124. 10.2190/PM.40.1.i [DOI] [PubMed] [Google Scholar]
- 19.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol 2009;5:363-389. 10.1146/annurev.clinpsy.032408.153621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009 Aug;151(4):264-269, W64. [DOI] [PubMed]
- 21.Hamdan A, Hawamdeh S, Hussein A. The prevalence and correlates of depressive symptoms among Arab women in a primary health care setting. Int J Psychiatry Med 2008;38(4):453-467. 10.2190/PM.38.4.e [DOI] [PubMed] [Google Scholar]
- 22.Ahmed I, Banu H, Al-Fageer R, Al-Suwaidi R. Cognitive emotions: depression and anxiety in medical students and staff. J Crit Care 2009. Sep;24(3):e1-e7. 10.1016/j.jcrc.2009.06.003 [DOI] [PubMed] [Google Scholar]
- 23.Al-Maskari F, Shah SM, Al-Sharhan R, Al-Haj E, Al-Kaabi K, Khonji D, et al. Prevalence of depression and suicidal behaviors among male migrant workers in United Arab Emirates. J Immigr Minor Health 2011. Dec;13(6):1027-1032. 10.1007/s10903-011-9470-9 [DOI] [PubMed] [Google Scholar]
- 24.Sulaiman N, Hamdan A, Tamim H, Mahmood DA, Young D. The prevalence and correlates of depression and anxiety in a sample of diabetic patients in Sharjah, United Arab Emirates. BMC Fam Pract 2010. Oct;11(1):80. 10.1186/1471-2296-11-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghubach R, El-Rufaie O, Zoubeidi T, Sabri S, Yousif S, Moselhy HF. Subjective life satisfaction and mental disorders among older adults in UAE in general population. Int J Geriatr Psychiatry 2010. May;25(5):458-465. 10.1002/gps.2360 [DOI] [PubMed] [Google Scholar]
- 26.Mellal AA, Albluwe T, Al-Ashkar DA. The prevalence of depressive symptoms and its socioeconomic determinants among university students in al Ain, UAE. Int J Pharm Pharm Sci 2014. Jan;6(5):309-312. [Google Scholar]
- 27.Alsaadi T, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, Nasreddine W, et al. Depression and anxiety among patients with epilepsy and multiple sclerosis: UAE comparative study. Behav Neurol 2015;2015:196373. 10.1155/2015/196373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alsaadi T, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, Almaskari B, et al. Prevalence of depression and anxiety among patients with epilepsy attending the epilepsy clinic at Sheikh Khalifa Medical City, UAE: A cross-sectional study. Epilepsy Behav 2015 Nov;52(Pt A):194-199. [DOI] [PubMed]
- 29.Hawamdeh S, Almakhzoomy I, Hayajneh Y. Screening and correlates of depression and HbA1 C in United Arab Emirates (UAE) women with diabetes. Perspect Psychiatr Care 2013. Oct;49(4):262-268. [DOI] [PubMed] [Google Scholar]
- 30.Schulte SJ, Thomas J. Relationship between eating pathology, body dissatisfaction and depressive symptoms among male and female adolescents in the United Arab Emirates. Eat Behav 2013. Apr;14(2):157-160. 10.1016/j.eatbeh.2013.01.015 [DOI] [PubMed] [Google Scholar]
- 31.Alsaadi T, Kassie S, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, et al. Potential factors impacting health-related quality of life among patients with epilepsy: Results from the United Arab Emirates. Seizure 2017. Dec;53:13-17. 10.1016/j.seizure.2017.10.017 [DOI] [PubMed] [Google Scholar]
- 32.Gariballa S, Alessa A. Association between muscle function, cognitive state, depression symptoms and quality of life of older people: evidence from clinical practice. Aging Clin Exp Res 2018. Apr;30(4):351-357. 10.1007/s40520-017-0775-y [DOI] [PubMed] [Google Scholar]
- 33.Thomas J, Anouti FA, Hasani SA, Abdel-Wareth L, Haq A. Sunshine, sadness and seasonality: 25-hydroxyvitamin d, and depressive symptoms in the United Arab Emirates (UAE). Int J Ment Health Promot 2011. Dec;13(1):23-26 . 10.1080/14623730.2011.9715647 [DOI] [Google Scholar]
- 34.Thomas J, Al-Anouti F. Sun exposure and behavioral activation for hypovitaminosis D and depression: A controlled pilot study. Community Ment Health J 2018. Aug;54(6):860-865. 10.1007/s10597-017-0209-5 [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention (CDC) Current depression among adults---United States, 2006 and 2008. MMWR Morb Mortal Wkly Rep 2010. Oct;59(38):1229-1235. [PubMed] [Google Scholar]
- 36.Aalto-Setälä T, Marttunen M, Tuulio-Henriksson A, Poikolainen K, Lönnqvist J. One-month prevalence of depression and other DSM-IV disorders among young adults. Psychol Med 2001. Jul;31(5):791-801. 10.1017/S0033291701004081 [DOI] [PubMed] [Google Scholar]
- 37.Daradkeh TK, Ghubash R, Abou-Saleh MT. Al Ain community survey of psychiatric morbidity II. Sex differences in the prevalence of depressive disorders. J Affect Disord 2002. Nov;72(2):167-176. 10.1016/S0165-0327(01)00452-9 [DOI] [PubMed] [Google Scholar]
- 38.Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci 2015. Jul;40(4):219-221. 10.1503/jpn.150205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li L, Wang HM, Ye XJ, Jiang MM, Lou QY, Hesketh T. The mental health status of Chinese rural-urban migrant workers : comparison with permanent urban and rural dwellers. Soc Psychiatry Psychiatr Epidemiol 2007. Sep;42(9):716-722. 10.1007/s00127-007-0221-0 [DOI] [PubMed] [Google Scholar]
- 40.Chou KL. Pre-migration planning and depression among new migrants to Hong Kong: the moderating role of social support. J Affect Disord 2009. Apr;114(1-3):85-93. 10.1016/j.jad.2008.06.005 [DOI] [PubMed] [Google Scholar]
- 41.Qiu P, Caine E, Yang Y, Chen Q, Li J, Ma X. Depression and associated factors in internal migrant workers in China. J Affect Disord 2011. Nov;134(1-3):198-207. 10.1016/j.jad.2011.05.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jhee JH, Kim H, Park S, Yun HR, Jung SY, Kee YK, et al. Vitamin D deficiency is significantly associated with depression in patients with chronic kidney disease. PLoS One 2017. Feb;12(2):e0171009. 10.1371/journal.pone.0171009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gulf News. Dubai launches mental health strategy. 2019. [cited 2019 May 9]. Available from: https://gulfnews.com/uae/health/dubai-launches-mental-health-strategy-1.2207626.
- 44.Sayed MA. Mental health services in the United Arab Emirates: Challenges and opportunities. Int J Emerg Ment Health Hum Resilience. 2015;17(3):661-663 . 10.4172/1522-4821.1000263 [DOI] [Google Scholar]


