Abstract
Purpose:
To determine if surface treatment and cement selection for traditional 3 mol% yttria partially stabilized zirconia (3Y-PSZ), “translucent” 5 mol% yttria-stabilized zirconia (5Y-Z), or lithium disilicate crowns affected their fracture load.
Materials and Methods:
Crowns with 0.8 mm uniform thickness (96, n = 8/group) were milled of 3Y-PSZ (Lava Plus), 5Y-Z (Lava Esthetic), or lithium disilicate (e.max CAD) and sintered/crystallized. Half the crowns were either particle-abraded with 30 μm alumina (zirconias) or etched with 5% hydrofluoric acid (lithium disilicate), and the other half received no surface treatment. Half the crowns from each group were luted with resin-modified glass ionomer (RMGI, RelyX Luting Plus) and half were luted with a resin cement (RelyX Unicem 2) to resin composite dies. Crowns were load cycled (100,000 cycles, 100 N force, 24°C water) and then loaded with a steel indenter until failure. A 3-way ANOVA examined the effect of material, cement, and surface treatment. Post-hoc comparisons were performed with Tukey-Kramer tests.
Results:
Fracture load was signficiantly different for materials and cements (P < 0.001) but not surface treatments (P = 0.770). All lithium disilicate crowns luted with RMGI failed in fatigue loading cycling. 3Y-PSZ and 5Y-Z crowns luted with resin showed a higher fracture load compared with RMGI (P<0.001). With resin cement, there was no signficant difference in fracture load between 5Y-Z and lithium disiliciate (P = 1) whereas 3Y-PSZ had a higher fracture load (P<0.001).
Conclusions:
Cement type affected fracture load of crowns but surface treatment did not. The 0.8 mm uniform thick crowns tested benefited from using resin cement regardless of type of ceramic material. Crowns fabricated from 5Y-Z may be particle-abraded if luted with resin cement.
Keywords: Cementation, resin cements
A practice-based research study conducted in 2015 reported that 32% of surveyed dentists would generally choose a monolithic zirconia restoration for a single-unit posterior crown, and 21% would choose lithium disilicate glass ceramics.1 At the time the survey was administered, the predominant zirconia used for monolithic crowns was 3 mol% yttria partially-stabilized zirconia (3Y-PSZ); 3Y-PSZ meets ISO 6872:2015 Type II Class 5 flexural strength requirements and is about twice as strong but half as translucent as lithium disilicate, which meets the Class 3 requirements.2,3 Therefore, the clinician has the option of prescribing a high-strength, opaque zirconia crown or a more translucent lithium disilicate crown, which requires bonding or increased restorative space to achieve sufficient strength. Five mol% yttria-stabilized zirconia (5Y-Z) is a newer form of zirconia, which has been marketed as “translucent” or “anterior” zirconia and meets ISO 6872:2015 Type II, Class 4 flexural strength requirements.4 This form of zirconia is intermediate in strength and translucency to 3Y-PSZ and lithium disilicate.2,3 As this formulation of zirconia is available from many manufacturers, scientific evidence is needed to develop recommended protocols for the cementation of 5Y-Z crowns.
Another recent practice-based research study conducted in 2016 to 2017 discovered that 71% of lithium disilicate crowns were luted with resin cement, whereas only 30% of zirconia crowns were luted with resin cement.5 Clinicians may choose to use resin cements with lithium disilicate crowns due to several studies showing that glass-based crowns luted with resin cement demonstrated a higher strength than those luted with resin-modified glass ionomer (RMGI) cement.6,7 The increase in strength achieved with resin cement is credited to either the ability to bond with tooth to prevent crack propagation in the ceramic or the better mechanical properties of the resin cement.8 On the other hand, many clinicians lute zirconia crowns with RMGI cement, and several studies have reported that the strength of 3Y-PSZ is not affected by luting with a RMGI cement even at a 0.5 mm thickness.9,10 As 5Y-Z is intermediate in strength to lithium disilicate and 3Y-PSZ, the clinician is left with the challenging decision to choose which type of cement is more appropriate. To further complicate the clinical situation, many clinicians may be unaware of what type zirconia they are using and default to the use of RMGI cement. Therefore, a primary aim of this study is to compare the strength of 3Y-PSZ, 5Y-Z, and lithium disilicate crowns after fatigue load cycling when used with resin or RMGI cement.
Several systematic reviews have reported the efficacy of bonding to zirconia by performing alumina particle abrasion followed by a primer containing the molecule 10-methacryloyloxydecyl dihydrogen phosphate (MDP).11–14 Unlike particle abrasion of glass-ceramic materials, particle abrasion of 3Y-PSZ zirconia does not weaken the material in static strength testing.15,16 Three mol% yttria partially-stabilized zirconia undergoes transformation toughening in which local transformation of tetragonal zirconia to monoclinic zirconia can impede propagation of an advancing crack. A recent study of 5Y-Z, however, reported that alumina particle abrasion reduced its flexural strength by 26 to 64%.17 The high concentration of cubic phase likely limits this material from undergoing transformation toughening. Many dental laboratories and clinicians particle abrade the intaglio surface of 5Y-Z crowns to improve their retention; however, the effect of this particle abrasion on the fracture load of crowns after fatigue testing has not been measured when luted with resin or RMGI cement.
The aim of this paper was to examine the crown fracture load of 3Y-PSZ, 5Y-Z, and lithium disilicate after fatigue testing with different luting protocols. The null hypotheses were that there would be no differences between the 3 restorative materials (3Y-PSZ, 5Y-Z, lithium disilicate) and that there would be no effect of cement (RMGI or resin cement) or surface treatment (alumina particle abrasion or hydrofluoric acid etching).
MATERIALS AND METHODS
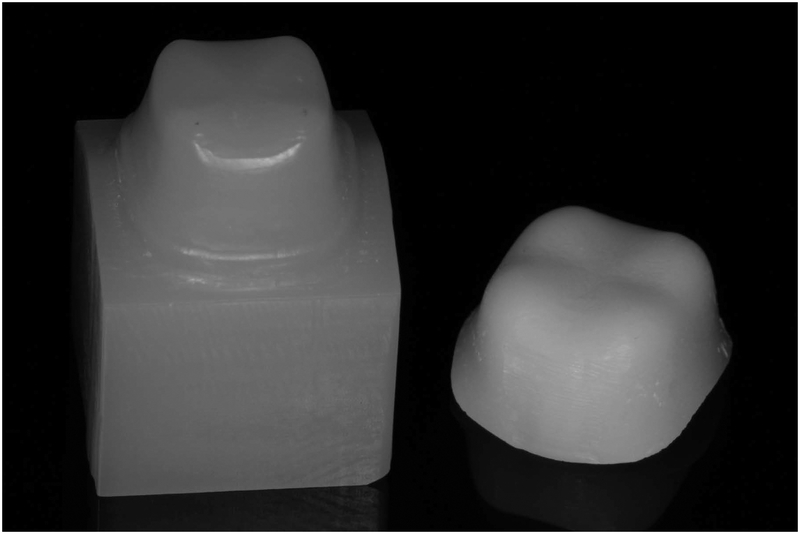
Standardized crown preparations were designed with AutoCAD software with a 0.8 mm shoulder margin and 1 mm incisal-cervical marginal curvature. Tooth dies were milled out of a resin composite (Crystal Ultra; Digital Dental, Scottsdale, AZ) that has a similar modulus as dentin (modulus = 10 GPa) using a 5-axis mill (CORiTEC 450i; imes-icore, Eiterfeld, Germany) (Fig 1). After fabrication, a representative tooth die was scanned with a laboratory scanner (d800; 3Shape, Copenhagen, Denmark) and used to digitally design a stylized crown using 3shape software. The crown was designed by selecting an even 0.8 mm thickness for all walls of the crown. An.stl file of the stylized crown was saved.
Figure 1:
Resin composite tooth die (left) and stylized crown (right).
The crown materials tested in this study included a 3Y-PSZ (Lava Plus; 3M ESPE, St. Paul, MN), a 5Y-Z (Lava Esthetic; 3M ESPE), and a lithium disilicate material (IPS e.max CAD LT; Ivoclar Vivadent, Schaan, Lichtenstein). The 3Y-PSZ and the 5Y-Z were dry milled (DWX-51D; Roland, Hamamatsu, Japan). The crowns were then sintered in a furnace (Austromat basic; DEKEMA, Freilassing, Germany) following the manufacturer’s recommended sintering cycle (Fig 1). The lithium disilicate crowns were milled in a PlanMill 40 (Planmeca, Helsinki, Finland). They were crystallized in a Programat CS furnace (Ivoclar Vivadent) using the manufacturer’s recommended standard crystallization cycle.
Tooth dies and crowns were randomly divided into 4 groups (n = 8) for each material. In the first group, the 3Y-PSZ and 5Y-Z crowns were alumina particle abraded prior to luting. Particle abrasion was performed with 30 μm alumina (white aluminum oxide grit #280 mesh; Kramer Industries, Piscataway, NJ) at 0.02 MPa pressure for 10 seconds at a distance of 10 mm. The lithium disilicate crowns were etched with 5% hydrofluoric acid (etching gel; Ivoclar Vivadent) for 20 seconds, rinsed with water for 20 seconds, and then coated with silane (RelyX Ceramic Primer; 3M ESPE). The crowns were then luted to the tooth dies with a self-adhesive resin cement (RelyX Unicem; 3M ESPE) and allowed to self-cure for 6 minutes with 200 g of applied weight.
The crowns in the second group were treated identically to the crowns in the first group except that a RMGI cement (RelyX Luting Plus; 3M ESPE) was used and allowed to self-cure for 6 minutes with 200 g of applied weight. The crowns in the third group did not receive any surface treatment after crystallization or sintering and were luted to the tooth dies with a self-adhesive resin cement (RelyX Unicem) and allowed to self-cure for 6 minutes with 200 g of applied weight. The crowns in the fourth group were treated identically to the crowns in the third group, except that a RMGI cement (RelyX Luting Plus) was used and allowed to self-cure for 6 minutes with 200 g of applied weight. All groups were luted at ambient temperature and humidity.
The crowns were load cycled for 100,000 cycles at 1 Hz with 100 N force in a custom fatiguing device. Specimens were loaded against a stainless steel ball (diameter = 8 mm) that made contact with the stylized crowns on each of the 4 cusps. Fatigue testing was performed in 24°C water. At the completion of the test, the crowns were examined to determine if any catastrophic failures occurred. The crowns that survived fatigue load cycling were then loaded to failure in compression in a universal testing machine (Model 4411; Instron, Norwood, MA). The load was applied with a stainless steel indenter (diameter = 12 mm) with a 1 mm/min compressive loading rate. A 1.5 mm rubber sheet was placed between the indenter and the crown to distribute the load and simulate a food bolus. During compressive load testing, the applied load was monitored for events of sudden decrease in load. At these events, the load was removed, and the crowns were inspected for visual signs of fracture. The highest load prior to fracture was recorded.
Representative crowns were viewed with scanning electron microscopy (SEM, Quanta FEG 650; FEI, Hillsboro, OR). The intaglio surface of an as-milled and alumina particle abraded 5Y-Z crown were examined. One surface-treated 5Y-Z and lithium disilicate crown were bonded to a tooth die, sectioned, and viewed in cross-section.
Descriptive statistics (mean ± SD and 95% confidence interval) were used to summarize the fracture load of the crowns from a combination of different materials, cements, and surface treatment. A 3-way ANOVA was used to examine the effects of materials, cements, surface treatments, and all possible interactions between the factors on the fracture load of the crowns. The post-hoc tests for the pairwise differences were conducted using Tukey-Kramer procedure. Normality assumption of the data was verified using a histogram and a Normal Q-Q plot prior to analysis. Lithium disilicate crowns luted with RMGI were excluded from the analysis due to 100% pre-test failure. A P-value < 0.05 was considered statistically significant in two-tailed statistical tests. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC). The box and whisker plot was created using Tableau v.2018.2 (Tableau, Seattle, WA)
RESULTS
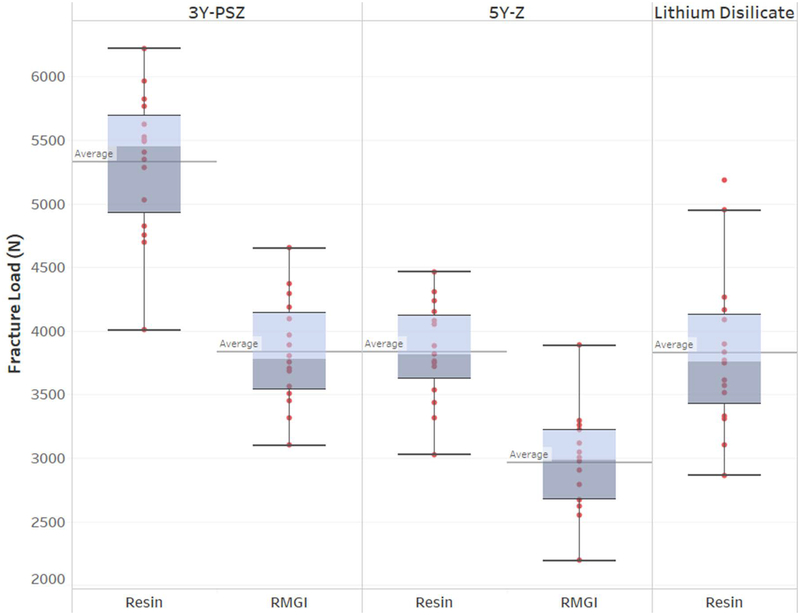
All lithium disilicate crowns luted with RMGI cement and 2 of the particle abraded 5Y-Z crowns luted with RMGI cement failed in fatigue load cycling. The descriptive statistics for materials by different cements and surface treatment are presented in Table 1. The fracture load was signficiantly different depending on the types of crown material and cement used (P < 0.001) but not for surface treatment (P = 0.770) (Table 2). Significant interaction between material and cement was observed (P = 0.013), suggesting crown fracture load was affected by types of materials and cements (Table 2). Specifically, 3Y-PSZ and 5Y-Z crowns luted with resin showed a higher fracture load compared with crowns luted with RMGI (P<0.001) (Table 3, Fig 2). With the use of a resin cement, the comparisons between materials revealed that there was no signficant difference in frature load between 5Y-Z and lithium disiliciate (P = 1) whereas 3Y-PSZ had a higher fracture load compared to both 5Y-Z and lithium disiliciate (P < 0.001). With the use of a RMGI cement, 3Y-PSZ had a higher fracture load than 5Y-Z (P < 0.001). The interactions between material and surface treatment, cement and surface treatment, and the 3-way interaction were not significant. These indicate that the crown fracture load was not a function of the different surface treatments studied.
Table 1.
Descriptive statistics for fracture load (N) by materials, cements, and surface treatments
| Surface treatment | No surface treatment | |||||||
|---|---|---|---|---|---|---|---|---|
| Resin | 95% C.I. | RMGI | 95% C.I. | Resin | 95% C.I. | RMGI | 95% C.I. | |
| 3Y-PSZ | 5383.6 ±713.0 | (4787.5, 5979.7) | 3865.7 ±363.7 | (3561.6, 4169.7) | 5272.3 ±383.3 | (4951.9, 5592.7) | 3801.4 ±480.6 | (3399.7, 4203.2) |
| 5Y-Z | 3647.7 ±396.4 | (3316.3, 3979.1) | 3007.4 ±320.9 | (2670.7, 3344.1) | 4008.0 ±287.2 | (3767.9, 4248.1) | 2937.2 ±479.4 | (2536.5, 3338) |
| Lithium Disilicate | 3768.5 ±286.9 | (3528.6, 4008.3) | NA | NA | 3883.1 ±847.4 | (3174.6, 4591.6) | NA | NA |
Table 2.
Result of three-way ANOVA
| Source of variation | DF | F | p |
|---|---|---|---|
| Material types | 2 | 56.44 | <0.0001 |
| Cement types | 1 | 87.21 | <0.0001 |
| Surface treatment | 1 | 0.09 | 0.770 |
| Material types*Cement types | 1 | 6.45 | 0.013 |
| Material types*Surface treatment | 2 | 0.43 | 0.650 |
| Cement types*Surface treatment | 1 | 0.58 | 0.450 |
| Material types*Cement types*Surface Treatment | 1 | 0.9 | 0.350 |
Table 3.
Result of Tukey-Kramer post-hoc tests
| Material x Cement | ||||
|---|---|---|---|---|
| i | J | Mean difference (i - j) | 95% C.I. | p |
| 3Y-PSZ + RMGI | 3Y + PSZ Resin | −1494.38 | (−1982.92, −1005.84) | <0.001 |
| 3Y-PSZ + RMGI | Lithium Disilicate + Resin | 7.76 | (−480.78, 496.3) | 1 |
| 3Y-PSZ + Resin | Lithium Disilicate + Resin | 1502.14 | (1013.6, 1990.68) | <0.001 |
| 5Y-Z + RMGI | 5Y-Z + Resin | −855.52 | (−1364.01, −347.03) | 0.001 |
| 5Y-Z + RMGI | 3Y-PSZ + RMGI | −861.23 | (−1369.72, −352.74) | 0.001 |
| 5Y-Z + RMGI | 3Y-PSZ + Resin | −2355.61 | (−2864.1, −1847.12) | <0.001 |
| 5Y-Z + RMGI | Lithium Disilicate + Resin | −853.48 | (−1361.97, −344.99) | 0.010 |
| 5Y-Z + Resin | 3Y-PSZ + RMGI | −5.71 | (−494.25, 482.83) | 1 |
| 5Y-Z + Resin | 3Y-PSZ + Resin | −1500.09 | (−1988.63, −1011.55) | <0.001 |
| 5Y-Z + Resin | Lithium Disilicate + Resin | 2.05 | (−486.49, 490.59) | 1 |
Figure 2:
Box and whisker plot showing the fracture load (N) of crowns from different materials and cements. The horizontal reference line denotes the mean; the line inside the box depicts the median; the upper and lower hinges represent 25th and 75th percentile, respectively.
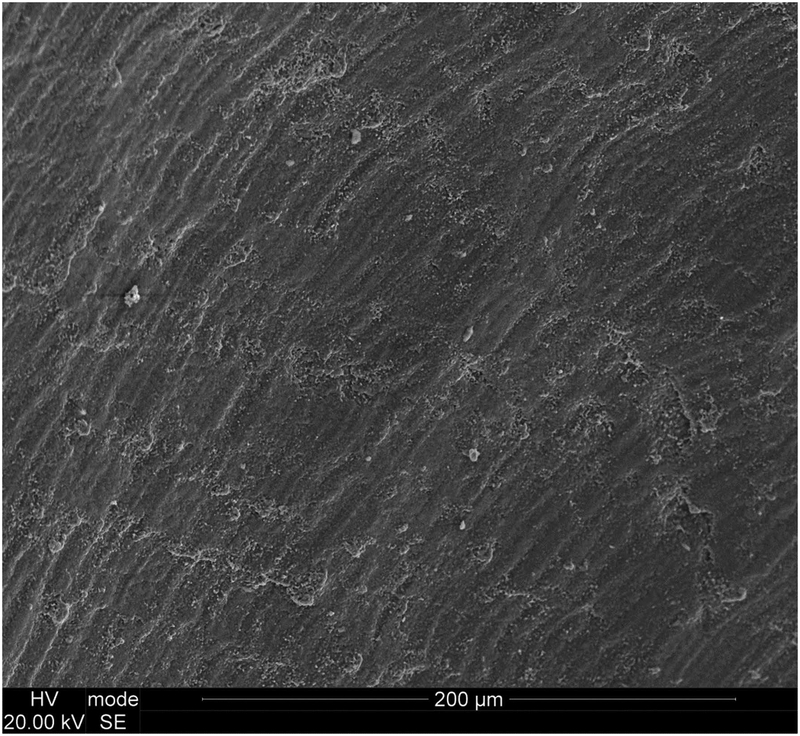
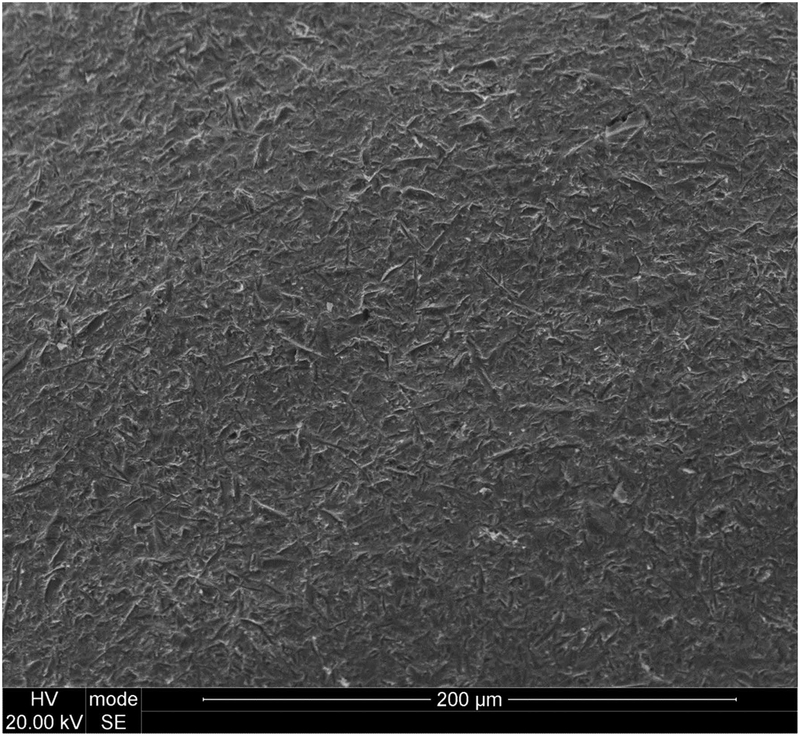
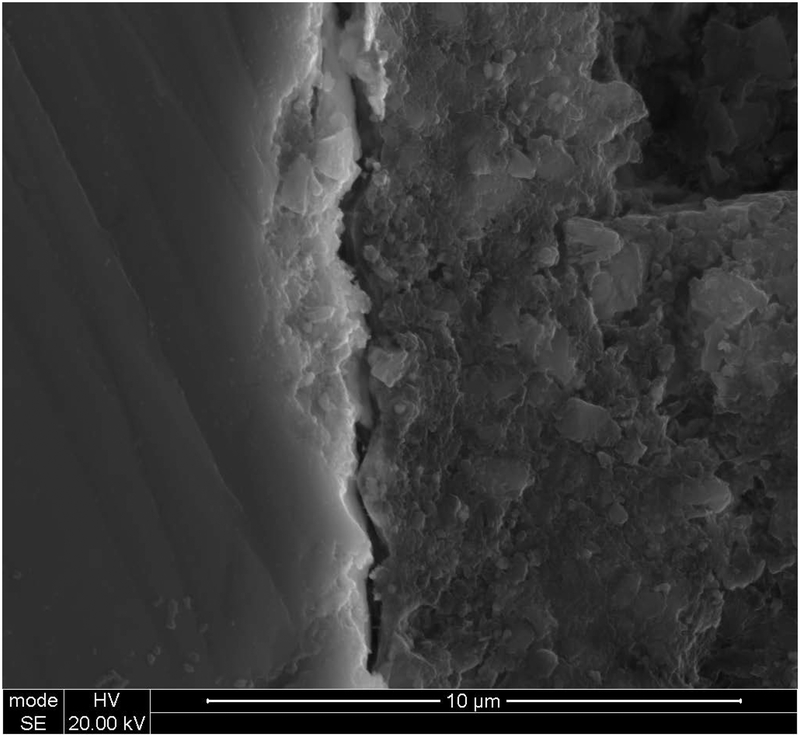
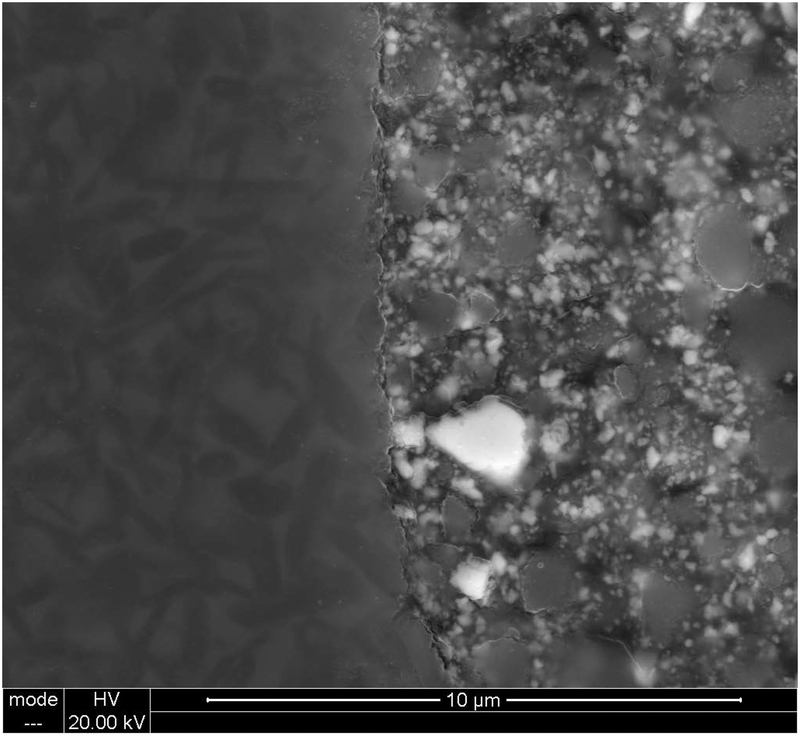
Observation of the intaglio surface of the 5Y-Z crowns showed that the as-milled surface demonstrated striations from milling (Fig 3). The particle-abraded surface shows surface pitting (on the scale of 1 to 5 μm) that overlays the the milling striations (Fig 4). The cross-section of the 5Y-Z crown and resin cement shows close adaptation and surface features on the scale of 1 to 5 μm (Fig 5). The cross-section of lithium disilicate crown and resin cement shows surface features with a finer texture (Fig 6).
Figure 3:
Intaglio surface of as-milled 5Y-Z crown.
Figure 4:
Intaglio surface of alumina particle abraded 5Y-Z crown.
Figure 5:
Cross-section of interface between alumina-particle abraded 5Y-Z crown (left) and resin cement (right).
Figure 6:
Cross-section of interface between hydrofluoric acid etched lithium disilicate crown (left) and resin cement (right).
DISCUSSION
The purpose of this study was to determine if the type of ceramic material used to fabricate a crown or the method used to lute the crown would affect its fracture load after fatiguing. Based on the results, the only null hypothesis accepted was that the surface treatment of the intaglio of the crown (particle abrasion or hydrofluoric acid etching) did not affect its fracture load. Both the ceramic material and the type of cement significantly affected crown fracture load.
The use of alumina particle-abrasion did not significantly affect the fracture load of 5Y-Z crowns unlike previous results of flexural strength testing, which showed a reduction in strength of 5Y-Z.17 There are several differences in testing methodologies between crown fracture testing and flexural strength testing that may account for these differences. First, specimens used for 3-point bend, 4-point bend, and biaxial flexural strength testing are polished to a flat surface ending with 15 to 20 μm grit diamond polishing media.3 On the other hand, the intaglio surface of the crowns produced in this study have been left as-milled in order to best represent the clinical situation. Although the use of particle abrasion will add additional defects to the surface of a milled crown (Fig 4), the as-milled surface already contains surface irregularity (Fig 3). Therefore, particle abrasion of a pristine, polished flexural strength specimen will be more likely to produce strength-reducing surface flaws than particle abrasion of the already roughened as-milled surface of a crown.
Another difference in methodologies is that crown fracture testing uses a layer of cement and a supporting tooth die, whereas the surface placed in tension during flexural strength testing is unsupported. The cross-section of the interface between resin cement and the particle-abraded zirconia shows there was close adaptation of the cement with the zirconia, on scale similar to the 1 to 5 μm size of the pits produced from particle abrasion (Fig 5). The adaptation may be assumed because of the matching surface profile of the zirconia and cement layers despite the visual separation likely caused by specimen preparation. By filling in the irregularities produced from particle abrasion and bonding the 5Y-Z to the supporting tooth die, the cement may help transfer stresses to the supporting die and prevent cracks from spreading through the crown. As the methodology used in this study more closely simulates the clinical situation than flexural strength testing, the results of this study justify alumina particle abrasion of 5Y-Z.
The observation that 3Y-PSZ crowns were not affected by particle abrasion also contradicts a previous study that showed the same material increased in flexural strength following particle abrasion.18 The increase in flexural strength recorded when 3Y-PSZ is particle-abraded with 30 or 50 μm alumina has been credited to surface tetragonal to monoclinic phase transformation causing compression in the surface layer.18 Mechanical fatigue, similar to the type performed in the current study, however, has been shown to negate any positive influence on strength caused by particle abrasion.19
It was not surprising that lithium disilicate was not weakened by 20 seconds of 5% hydrofluoric acid etching, as this surface treatment also does not weaken flexural strength specimens.20 Hydrofluoric acid etching lithium disilicate provides fine surface texture that allows close adaptation interpenetration of the resin cement (Fig 6); therefore, it may also play a role in reinforcing the strength of lithium disilicate in crown fracture testing as forces can be easily transferred to the supporting die. A previous study showed that etching with 3% or 5% hydrofluoric acid improved the cyclic load-to-failure of lithium disilicate crowns;21 however, this result was not observed in the current study. Due to the advantages in bond strength observed with etching hydrofluoric acid, clinicians should continue to follow manufacturers’ recommendations for etching lithium disilicate restorations when adhesively bonding.
The higher fracture load of 3Y-PSZ crowns than lithium disilicate crowns (with resin cement) and 5Y-Z crowns (with both cements) was expected due to the differences in strength of these materials. The similar crown fracture load of lithium disilicate and 5Y-Z crowns with resin cement may seem unexpected based on previous reports of 34% higher flexural strength of a 5Y-Z than lithium disilicate.2 Another study also reported that the the fracture load of lithium disilicate bonded to a dentin substitute achieved a higher load than 5Y-Z, despite the higher biaxial flexural strength of the 5Y-Z material than lithium disilicate.22 In that study, the higher load capacity of lithium disilicate when luted to a dentin substitute was credited to the better match in elastic modulus between the lithium disilicate (95 GPa) and the resin cement (7.9 GPa)/resin tooth die (18.6 GPa) than that of 5Y-Z (210 GPa). When a low modulus foundation (i.e., dentin) supports a higher modulus crown, flexure of the ceramic crown may occur with occlusal loading. Therefore, despite its lower strength, a lithium disilicate crown luted to dentin with resin cement may show similar fracture capacity as a 5Y-Z crown luted to dentin with resin cement.
In this study, all lithium disilicate crowns luted with RMGI cement failed in fatigue; however, the 0.8 mm occlusal thickness was below the 1.5 mm thickness recommended for RMGI cement or 1 mm thickness recommended for resin cement. This thickness was used to standardize the specimens and represent a worst-case scenario. The survival of the lithium disilicate crowns at this thickness when luted with a resin cement is evidence that adhesively bonding this material improves its fracture capacity. Despite these results, clinicians and technicians should continue to adhere to the manufacturer’s recommended minimum material thickness.
All materials showed improved fracture performance when luted with a resin cement as compared to a RMGI cement. This improvement may be credited to the ability of the resin cement to form a strong bond between the dentin substitute and the crown, and in turn preventing the growth of cracks within the crown. Additionally, resin cements have a higher modulus and strength than RMGI cements, allowing for a better foundation.23
An important clinical consideration is the acceptability of luting 5Y-Z crowns with RMGI cement. Without particle abrasion, all 5Y-Z crowns luted with RMGI survived fatigue testing but recorded a lower fracture load than 5Y-Z or lithium disilicate crowns luted with a resin cement. With particle abrasion, 2 of the 8 5Y-Z crowns luted with RMGI failed in fatigue, but those that survived recorded the same fracture load as the crowns without particle abrasion. The manufacturer of this 5Y-Z recommends a minimum thickness of 0.8 mm, particle abrasion with 30 μm alumina, and luting the crown with the same resin cement used in this study. If the clinician were to disregard the manufacturer’s recommendations and use an RMGI cement with 5Y-Z, a decreased strength performance would be expected and particle abrasion should not be used. Five mol% yttria-stabilized zirconia and lithium disilicate performed similarly when used with resin cement; however, the 5Y-Z performed better than the lithium disilicate crowns when used with RMGI cement. A clinical advantage based on this observation is that 5Y-Z crowns may be less likely to fracture during the try-in and adjustment procedure, as they survived fatigue testing without adhesive bonding.
There are several limitations in this study. Ideally, the crowns would have been luted to natural tooth dies; however, the choice was made to use a dentin substitute in order to limit experimental variability. Longer aging and fatigue cycling may have also been helpful to better predict the performance of the crowns. These results are specific to the materials tested in this study, and differences in composition of other brands of material may have significant effects on the conclusions of this study.
Future studies may examine the effects of surface treatment and cement on the fatigue life of ceramic crowns. Additionally, various thicknesses of ceramics may be examined to determine when the difference in fracture load between crowns luted with RMGI and resin cement is negligible. Finally, other types of abrasives and air pressures may be examined to determine if there is an improved method to create surface texture on 5Y-Z without affecting strength.
CONCLUSIONS
All-ceramic crowns (3Y-PSZ, 5Y-Z, lithium disilicate) at a 0.8 mm thickness benefited from the use of resin cement. Based on this study, the 5Y-Z crown material could be alumina particle-abraded prior luting with with resin cement. The 5Y-Z and lithium disilicate crowns luted with resin cement achieved similar fracture loads. Luting of 5Y-Z crowns with RMGI should only be performed with caution at 0.8 mm thickness and if attempted, should not be alumina particle-abraded prior to luting.
Acknowledgements
This work was partially supported by a grant from 3M. A pilot study was supported by a grant from the American Academy of Esthetic Dentistry. The statistical analysis was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (award number UL1TR001417). The authors thank the University of Alabama at Birmingham scanning electron microscopy laboratory for assistance with microscopy, and James Omar Bradley from the UAB dental laboratory and Borris Simmons from Vulcan Dental Laboratory for their assistance with fabricating the crowns.
This work was partially based on a research grant sponsored by 3M ESPE, St. Paul, MN
Footnotes
Conflict of interest declaration: Dr. Burgess and Dr. Lawson, through UAB, have/have had contracts and research grants with 3M and Ivoclar Vivadent. Dr. Burgess has honoraria paid by 3M, and Dr. Lawson has honoraria paid by Ivoclar Vivadent. Geoffrey Morris is a former employee of 3M. All other authors are free of conflicts of interest for this work.
This data was previously presented at the 2018 annual session of the AADR in Ft. Lauderdale FL (March 21–24 2018).
REFERENCES
- 1.Makhija SK, Lawson NC, Gilbert GH, et al. : Dentist material selection for single-unit crowns: Findings from the National Dental Practice-Based Research Network. J Dent 2016;55:40–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwon SJ, Lawson NC, McLaren EE, et al. : Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent 2018;120:132–137 [DOI] [PubMed] [Google Scholar]
- 3.Zhang Y, Lawn BR: Novel zirconia materials in dentistry. J Dent Res 2018;97:140–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawson NC, Litaker MS, Ferracane JL, et al. : Choice of cement for single-unit crowns: Findings from the National Dental Practice-Based Research Network. J Am Dent Assoc 2019; doi: 10.1016/j.adaj.2019.01.021. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heintze SD, Cavalleri A, Zellweger G, et al. : Fracture frequency of all-ceramic crowns during dynamic loading in a chewing simulator using different loading and luting protocols. Dent Mater 2008;24:1352–1361 [DOI] [PubMed] [Google Scholar]
- 6.Borges GA, Caldas D, Taskonak B, et al. : Fracture loads of all-ceramic crowns under wet and dry fatigue conditions. J Prosthodont 2009;18:649–655 [DOI] [PubMed] [Google Scholar]
- 7.Burke FJ: The effect of variations in bonding procedure on fracture resistance of dentin-bonded all-ceramic crowns. Quintessence Int 1995;26:293–300 [PubMed] [Google Scholar]
- 8.Zesewitz TF, Knauber AW, Nothdurft FP: Fracture resistance of a selection of full-contour all-ceramic crowns: an in vitro study. Int J Prosthodont 2014;27:264–266 [DOI] [PubMed] [Google Scholar]
- 9.Nakamura K, Mouhat M, Nergård JM, et al. : Effect of cements on fracture resistance of monolithic zirconia crowns. Acta Biomater Odontol Scand 2016;2:12–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inokoshi M, De Munck J, Minakuchi S, et al. : Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res 2014;93:329–34 [DOI] [PubMed] [Google Scholar]
- 11.Thammajaruk P, Inokoshi M, Chong S, et al. : Bonding of composite cements to zirconia: A systematic review and meta-analysis of in vitro studies. J Mech Behav Biomed Mater 2018;80:258–268 [DOI] [PubMed] [Google Scholar]
- 12.Tzanakakis EG, Tzoutzas IG, Koidis PT: Is there a potential for durable adhesion to zirconia restorations? A systematic review. J Prosthet Dent 2016;115:9–19 [DOI] [PubMed] [Google Scholar]
- 13.Sailer I, Makarov NA, Thoma DS, et al. : All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater 2015;31:603–623 [DOI] [PubMed] [Google Scholar]
- 14.Ozcan M, Melo RM, Souza RO, et al. : Effect of air-particle abrasion protocols on the biaxial flexural strength, surface characteristics and phase transformation of zirconia after cyclic loading. J Mech Behav Biomed Mater 2013;20:19–28 [DOI] [PubMed] [Google Scholar]
- 15.Passos SP, Linke B, Major PW, et al. : The effect of air-abrasion and heat treatment on the fracture behavior of Y-TZP. Dent Mater 2015;31:1011–21 [DOI] [PubMed] [Google Scholar]
- 16.McLaren EA, Lawson N, Choi J, et al. : New high-translucent cubic-phase-containing zirconia: Clinical and laboratory considerations and the effect of air abrasion on strength. Compend Contin Educ Dent 2017;38:e13–e16 [PubMed] [Google Scholar]
- 17.International Organization for Standardization. ISO 6872:2015 Dental ceramic International Organization for Standardization, Geneva: (2015). https://www.iso.org/standard/59936.html. Accesssed 5/18/19 [Google Scholar]
- 18.Garcia Fonseca R, de Oliveira Abi-Rached F, dos Santos Nunes Reis JM, et al. : Effect of particle size on the flexural strength and phase transformation of an airborne-particle abraded yttria-stabilized tetragonal zirconia polycrystal ceramic. J Prosthet Dent 2013;110:510–514 [DOI] [PubMed] [Google Scholar]
- 19.Aboushelib MN, Wang H, Kleverlaan CJ, et al. : Fatigue behavior of zirconia under different loading conditions. Dent Mater 2016;32:915–920 [DOI] [PubMed] [Google Scholar]
- 20.Menees TS, Lawson NC, Beck PR, et al. : Influence of particle abrasion or hydrofluoric acid etching on lithium disilicate flexural strength. J Prosthet Dent 2014;112:1164–1170 [DOI] [PubMed] [Google Scholar]
- 21.Prochnow C, Pereira GKR, Venturini AB, et al. : How does hydrofluoric acid etching affect the cyclic load-to-failure of lithium disilicate restorations? J Mech Behav Biomed Mater 2018;87:306–311 [DOI] [PubMed] [Google Scholar]
- 22.Yan J, Kaizer MR, Zhang Y: Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater 2018;88:170–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saskalauskaite E, Tam LE, McComb: Flexural strength, elastic modulus, and pH profile of self-etch resin luting cements. J Prosthodont 2008;17:262–268 [DOI] [PubMed] [Google Scholar]