Abstract
Background:
Out-of-hospital births have been increasing in the United States, although past studies have found wide variations between states. Our purpose was to examine trends in out-of-hospital births, the risk profile of these births, and state differences in women’s access to these births.
Methods:
National birth certificate data from 2004–2017 were analyzed. Newly available national data on method of payment for the delivery (private insurance, Medicaid, self-pay) were used to measure access to out-of-hospital birth options.
Results:
After a gradual decline from 1990–2004, the number of out-of-hospital births increased from 35,578 in 2004 to 62,228 in 2017. In 2017, 1 of every 62 births in the US was an out-of-hospital birth (1.61%). Home births increased by 77% from 2004–2017, while birth center births more than doubled. Out-of-hospital births were more common in the Pacific Northwest, and less common in the southeastern states such as Alabama, Louisiana, and Mississippi. Women with planned home and birth center births were less likely to have a number of population characteristics associated with poor pregnancy outcomes, including teen births, smoking during pregnancy, obesity, and preterm, low birthweight, and multiple births. More than 2/3 of planned home births were self-paid, compared to 1/3 of birth center and just 3% of hospital births, with large variations by state.
Conclusions:
Lack of insurance or Medicaid coverage is an important limiting factor for women desiring out-of-hospital birth in most states. Recent increases in out-of-hospital births despite important limiting factors highlights the strong motivation of some women to choose out-of-hospital birth.
Introduction
The rapid growth in home and birth center births in the United States since 2004 (1,2) has led to considerable research and discussion concerning place of birth (3–7). The slow adoption by states of the 2003 revised birth certificate has meant that a number of key variables, including planning status of home births, payer for the birth (private insurance, Medicaid or self-pay), and whether or not a woman received WIC benefits were not available nationally until 2016 (8). With the exception of California, which doesn’t report on planning status of home births (9), we now report nationally for the first time on these variables and their relationship to place of delivery. A recent move towards using the term “community birth” to denote planned home and birth center births is laudable (3,4,10); however, birth certificate data do not allow for accurate identification of community births in all states. Thus, the term “out-of-hospital” birth is used for this paper to promote uniformity in definitions between states, and to facilitate trend analysis (1,2); see Discussion section.
An important consideration for every woman in choosing a place of birth is whether insurance companies and/or Medicaid will cover the cost of the birth. In general, home and birth center births are about ½ to 1/3 the cost of hospital births (11–12). However, if a woman’s insurance company or Medicaid will not cover these births, then the cost is borne directly by the woman, which has the potential to make out-of-pocket payments for planned home or birth center births so costly as to be prohibitive. Thus, the new birth certificate data on method of payment for the delivery provides important information about access to out-of-hospital births.
The aims of the paper are to examine trends in out-of-hospital, home and birth center births and also variations in the incidence of these births by state. Since it is important to select low-risk women as candidates for out-of-hospital birth, we also examine differences by place of birth in population characteristics that may denote a higher risk of poor pregnancy outcome. Finally, we examine state differences in access to care for birth center and planned home births as represented by private insurance or Medicare coverage to pay for the cost of the delivery.
Methods
Data for 2017 and prior years are derived from birth certificates registered in State vital statistics offices, and then transmitted to the National Center for Health Statistics, where the data are made into publicly available national data files (8,9). For out-of-hospital births, information needed to complete the birth certificate is provided by the birth attendant (usually a midwife). For hospital births, the birth certificate is completed by the hospital birth registrar (13).
Two categories of midwife data were collected on the birth certificate: certified nurse-midwife (CNM)/certified midwife (CM), and non CNM/CM midwife. Non-CNM/CM midwife includes any other type of midwife besides CNM/CM, such as a certified professional midwife, licensed midwife, or direct-entry midwife (13).
Race and Hispanic origin are reported independently on the birth certificate and are obtained from the woman. Data for Hispanic women are not further classified by race because the overwhelming majority of these women are reported as white. Recent changes to race classification data allow for the reporting of single and multiple race data (8); however, to facilitate trend analysis, we continue to use the bridged race data which has been in use for trend analysis for the past decade (8). The obstetric estimate of gestation has been used as the national standard measure for gestational age since 2014 (14), and is used to measure gestational age for the percent preterm (<37 completed weeks of gestation) variable in this study.
Variables included in the study are generally well reported on birth certificates; missing values (<4% for all variables) were excluded before percentages were computed. Planning status of home birth was not reported for California (12% of US births), while breastfeeding initiation was not reported by California and Michigan (15 % of US births) (9). Percentages were computed per 100 birthing women (Table 1 and Figures 1 and 2), and also per 100 women in a specific group (Tables 2 and 3). Following National Center for Health Statistics guidelines, data were suppressed for states with fewer than 20 birth center births (9). All statements in the text were tested for statistical significance using a 2-proportion Z test, and all differences noted as higher or lower were statistically significant at the p<0.05 level.
Table 1.
Number and percentage of births by place of birth, United States and each State, 2017
| Total births, n | Total out of hospital+, n(%) | Birth center, n(%) | Home#, n(%) | Among home births, percent planned#~ | |
|---|---|---|---|---|---|
| United States | 3,855,500 | 62,228 (1.61) | 19,878( 0.52) | 38,343 ( 0.99) | 84.9 |
| Alabama | 58,941 | 256 (0.43) | * | 182 ( 0.31) | 46.5 |
| Alaska | 10,445 | 823 (7.88) | 589(5.64) | 206 (1.97) | 91.1 |
| Arizona | 81,872 | 1,399 (1.71) | 607 (0.74) | 706 (0.86) | 87.5 |
| Arkansas | 37,520 | 422 (1.12) | 87 (0.23) | 292 (0.78) | 87.2 |
| California | 471,658 | 5,398 (1.14) | 1,413 (0.30) | 3,520 (0.75) | ~ |
| Colorado | 64,382 | 1,679 (2.61) | 589 (0.91) | 1,040 (1.62) | 89.5 |
| Connecticut | 35,221 | 342 (0.97) | 104 (0.30) | 212 (0.60) | 79.3 |
| Delaware | 10,855 | 235 (2.16) | 140 (1.29) | 83 (0.76) | 75.6 |
| District of Columbia | 9,560 | 100 (1.05) | 24 (0.25) | 56 (0.59) | 69.6 |
| Florida | 223,630 | 4,043 (1.81) | 1,820 (0.81) | 2,020 (0.90) | 83.3 |
| Georgia | 129,243 | 1,182 (0.91) | 307 (0.24) | 822 (0.64) | 68.0 |
| Hawaii | 17,517 | 371 (2.12) | * | 318 (1.82) | 91.2 |
| Idaho | 22,181 | 837 (3.77) | 319 (1.44) | 504 (2.27) | 95.2 |
| Illinois | 149,390 | 921 (0.62) | * | 784 (0.52) | 73.8 |
| Indiana | 82,170 | 2,103 (2.56) | 732 (0.89) | 1,354 (1.65) | 92.8 |
| Iowa | 38,430 | 546 (1.42) | * | 489 (1.27) | 84.3 |
| Kansas | 36,519 | 713 (1.95) | 236 (0.65) | 449 (1.23) | 90.2 |
| Kentucky | 54,752 | 774 (1.41) | 27 (0.05) | 641 (1.17) | 88.6 |
| Louisiana | 61,018 | 283 (0.46) | 51 (0.08) | 173 (0.28) | 45.7 |
| Maine | 12,298 | 277 (2.25) | 20 (0.16) | 243 (1.98) | 92.9 |
| Maryland | 71,641 | 924 (1.29) | 326 (0.46) | 515 (0.72) | 67.2 |
| Massachusetts | 70,702 | 637 (0.90) | 192 (0.27) | 402 (0.57) | 58.0 |
| Michigan | 111,426 | 1,542 (1.38) | 117 (0.11) | 1,375 (1.23) | 87.0 |
| Minnesota | 68,595 | 1,551 (2.26) | 543 (0.79) | 972 (1.42) | 88.7 |
| Mississippi | 37,357 | 203 (0.54) | * | 179 (0.48) | 63.1 |
| Missouri | 73,034 | 1,722 (2.36) | 268 (0.37) | 1,164 (1.59) | 90.5 |
| Montana | 11,799 | 481 (4.08) | 158 (1.34) | 323 (2.74) | 95.5 |
| Nebraska | 25,821 | 135 (0.52) | 38 (0.15) | 90 (0.35) | 58.1 |
| Nevada | 35,756 | 512 (1.43) | * | 487 (1.36) | 82.7 |
| New Hampshire | 12,116 | 267 (2.20) | 121 (1.00) | 143 (1.18) | 83.0 |
| New Jersey | 101,250 | 514 (0.51) | * | 397 (0.39) | 50.5 |
| New Mexico | 23,767 | 518 (2.18) | 209 (0.88) | 283 (1.19) | 88.9 |
| New York | 229,737 | 3,203 (1.39) | 173 (0.08) | 2,339 (1.02) | 77.7 |
| North Carolina | 120,125 | 1,839 (1.53) | 1,173 (0.98) | 642 (0.53) | 68.6 |
| North Dakota | 10,737 | 135 (1.26) | * | 123 (1.15) | 85.4 |
| Ohio | 136,832 | 2,291 (1.67) | 716 (0.52) | 1,482 (1.08) | 82.2 |
| Oklahoma | 50,214 | 707 (1.41) | 112 (0.22) | 543 (1.08) | 88.3 |
| Oregon | 43,631 | 1,561 (3.58) | 613 (1.40) | 916 (2.10) | 92.6 |
| Pennsylvania | 137,745 | 4,865 (3.53) | 1,711 (1.24) | 2,611 (1.90) | 91.4 |
| Rhode Island | 10,638 | 54 (0.51) | * | 51 (0.48) | 72.5 |
| South Carolina | 57,029 | 964 (1.69) | 549 (0.96) | 406 (0.71) | 73.1 |
| South Dakota | 12,134 | 105 (0.87) | * | 99 (0.82) | 77.8 |
| Tennessee | 81,016 | 1,038 (1.28) | 214 (0.26) | 785 (0.97) | 89.4 |
| Texas | 382,050 | 5,562 (1.46) | 3,117 (0.82) | 2,378 (0.62) | 82.4 |
| Utah | 48,585 | 1,399 (2.88) | 388 (0.80) | 993 (2.04) | 95.0 |
| Vermont | 5,655 | 152 (2.69) | * | 145 (2.56) | 91.6 |
| Virginia | 100,391 | 1,241 (1.24) | 345 (0.34) | 878 (0.87) | 85.1 |
| Washington | 87,562 | 3,297 (3.77) | 1,351 (1.54) | 1,877 (2.14) | 92.0 |
| West Virginia | 18,675 | 181 (0.97) | 28 (0.15) | 125 (0.67) | 74.6 |
| Wisconsin | 64,975 | 1,755 (2.70) | 272 (0.42) | 1,366 (2.10) | 99.0 |
| Wyoming | 6,903 | 169 (2.45) | * | 160 (2.32) | 94.9 |
Category includes 3,273 “other”, 553 “clinic or doctor’s office”, and 181 “not stated” location.
Does not include planned home births that were transferred to hospitals.
Excludes data from California which did not report planning status of home birth.
Data were suppressed for 12 states that had <20 birth center births; see Methods section.
Source: Authors’ calculations based on 2017 birth certificate data.
Figure 1. Percentage of births occurring out of hospital: United States, 2004–2017.
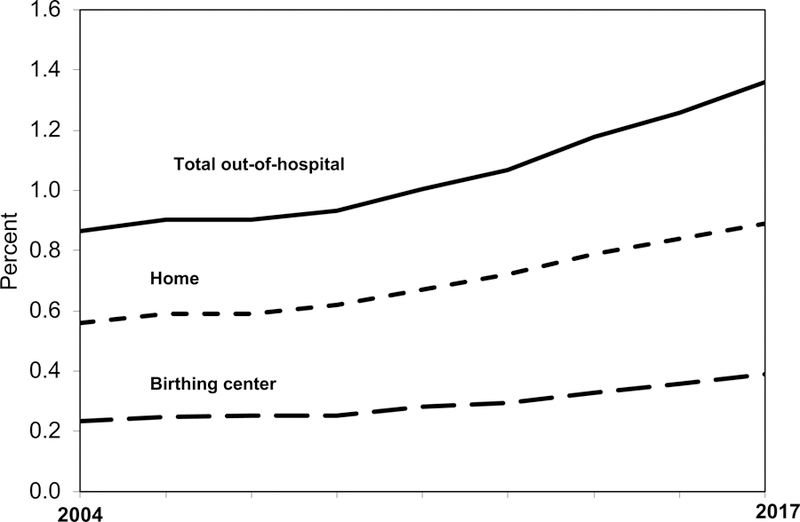
SOURCE: Birth certificate data from the National Vital Statistics System
NOTE: Out-of-hospital births include those occurring in a home, birthing center, clinic or doctor’s office, or other location.
Figure 2. Percentage of births occurring out of hospital by race and Hispanic origin of mother: United States, 2004–2017.
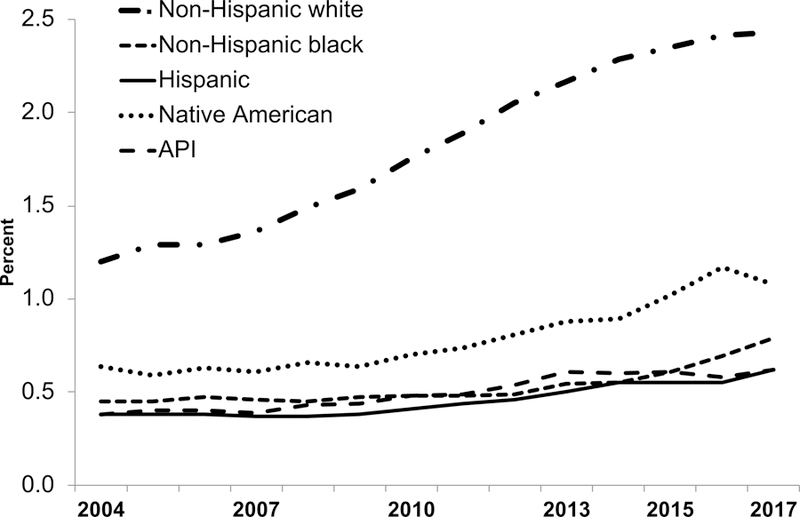
Notes:. API = Asian or Pacific Islander. Source: Birth certificate data from the National Vital Statistics System.
Table 2.
Percent of births with selected characteristics by place of birth, United States, 2017
| All births, n=3,855,500 |
Hospital, n=3,793,272 |
Out of hospital+, n=62,228 |
Birth center, n=19,878 |
Home #, n=38,343 |
Planned home * #, n=28,994 |
|
|---|---|---|---|---|---|---|
| Age of mother (years) | ||||||
| <20 | 5.1 | 5.2 | 1.4 | 0.9 | 1.4 | 0.7 |
| 20–34 | 77.3 | 77.3 | 77.1 | 81.0 | 74.9 | 75.8 |
| 35+ | 17.6 | 17.5 | 21.5 | 18.1 | 23.6 | 23.5 |
| Mother’s education - | ||||||
| Bachelor’s degree or | 32.3 | 32.2 | 38.6 | 47.8 | 35.6 | 36.3 |
| First live birth | 37.9 | 38.2 | 23.3 | 33.4 | 18.5 | 17.7 |
| Smoked during pregnancy | 6.9 | 7.0 | 3.0 | 1.1 | 3.3 | 0.9 |
| Pre-pregnancy Body Mass Index | ||||||
| Underweight (<18.5) | 3.4 | 3.4 | 4.3 | 3.9 | 4.4 | 4.2 |
| Normal weight (20.0–24. | 43.3 | 43.1 | 59.5 | 61.1 | 59.4 | 60.4 |
| Overweight (25.0–29.9) | 26.2 | 26.3 | 22.4 | 22.0 | 22.3 | 22.2 |
| Obese (30+) | 27.1 | 27.3 | 13.9 | 13.0 | 13.9 | 13.2 |
| Preterm birth | 11.6 | 11.8 | 4.5 | 1.5 | 5.2 | 2.1 |
| Low birthweight | 8.3 | 8.4 | 3.6 | 0.9 | 4.2 | 1.3 |
| Multiple birth | 3.4 | 3.5 | 0.7 | 0.2 | 1.0 | 0.7 |
| VBAC ^ | 2.0 | 2.0 | 3.4 | 1.7 | 4.1 | 4.2 |
| Trimester prenatal care began | ||||||
| 1st trimseter | 77.3 | 77.6 | 60.3 | 69.4 | 56.2 | 55.8 |
| 2nd trimester | 16.5 | 16.3 | 28.4 | 24.5 | 30.6 | 33.3 |
| Late or no prenatal care | 6.3 | 6.2 | 11.3 | 6.1 | 13.2 | 10.9 |
| Attendant at birth | ||||||
| Physician | 89.2 | 90.6 | 4.3 | 2.7 | 3.7 | 0.7 |
| CNM/CM | 9.1 | 8.7 | 34.1 | 56.6 | 24.4 | 29.4 |
| Other midwife | 0.8 | 0.1 | 41.2 | 36.7 | 45.6 | 50.7 |
| Other | 0.8 | 0.5 | 20.3 | 3.9 | 26.4 | 19.1 |
| Breastfeeding initiation~ | 82.2 | 82.0 | 93.5 | 97.8 | 92.3 | 97.5 |
| Receipt of WIC food | 38.1 | 38.5 | 11.9 | 10.2 | 11.4 | 6.9 |
| Method of payment for delivery | ||||||
| Medicaid | 43.0 | 43.4 | 17.5 | 17.9 | 15.4 | 8.6 |
| Private insurance | 49.1 | 49.4 | 29.6 | 47.5 | 20.6 | 19.0 |
| Self-pay | 4.1 | 3.4 | 48.9 | 32.2 | 59.4 | 67.9 |
| Other | 3.8 | 3.8 | 4.0 | 2.4 | 4.7 | 4.6 |
Category includes 3273 “other”, 553 “clinic or doctor’s office”, and 181 “unknown” location.
Does not include planned home births that were transferred to hospitals.
Excudes data from California which did not report planning status of home birth.
The percent of births for each place of birth that were vaginal births after cesarean.
Breastfeeding initiation was not reported for California and Michigan.
Source: Authors’ calculations based on 2017 birth certificate data.
Table 3.
Percentage of birth center and planned home births by method of payment for delivery, United States and each State, 2017
| Birth center births (n=19,878) |
Planned home births (n=28,994) ~# | |||||
|---|---|---|---|---|---|---|
| Medicaid | Private insurance | Self-pay | Medicaid | Private insurance | Self-pay | |
| United State | 17.9 | 47.5 | 32.2 | 8.6 | 19.0 | 67.9 |
| Alabama | * | * | * | 11.0 | 21.9 | 58.9 |
| Alaska | 30.8 | 54.2 | 6.8 | 29.4 | 38.5 | 14.7 |
| Arizona | 12.2 | 64.1 | 21.6 | 2.2 | 6.0 | 89.9 |
| Arkansas | 4.6 | 89.7 | 5.7 | 1.6 | 4.0 | 87.6 |
| California | 21.0 | 23.6 | 51.1 | ~ | ~ | ~ |
| Colorado | 14.1 | 76.8 | 7.5 | 7.1 | 15.3 | 71.0 |
| Connecticut | 23.1 | 73.1 | 3.8 | 18.9 | 40.9 | 36.6 |
| Delaware | 21.4 | 69.3 | 6.4 | 0 | 0 | 100.0 |
| District of Co | 37.5 | 50.0 | 4.2 | 2.6 | 76.9 | 20.5 |
| Florida | 37.2 | 46.3 | 16.1 | 30.4 | 36.5 | 31.5 |
| Georgia | 17.6 | 38.1 | 34.5 | 3.6 | 10.8 | 82.9 |
| Hawaii | * | * | * | 11.4 | 7.6 | 73.4 |
| Idaho | 24.1 | 30.4 | 42.0 | 16.4 | 14.1 | 53.2 |
| Illinois | * | * | * | 4.0 | 38.2 | 54.6 |
| Indiana | 0.0 | 13.8 | 85.8 | 0.5 | 4.2 | 93.9 |
| Iowa | * | * | * | 3.7 | 18.3 | 71.9 |
| Kansas | 19.1 | 59.6 | 16.6 | 0.5 | 17.2 | 79.9 |
| Kentucky | 37.0 | 55.6 | 7.4 | 1.1 | 2.1 | 79.2 |
| Louisiana | 74.5 | 13.7 | 9.8 | 2.5 | 7.6 | 79.7 |
| Maine | 0.0 | 21.4 | 78.6 | 7.6 | 7.6 | 83.9 |
| Maryland | 15.4 | 64.4 | 12.2 | 1.7 | 28.3 | 66.2 |
| Massachuse | 13.5 | 81.3 | 1.6 | 2.2 | 17.9 | 79.3 |
| Michigan | 3.4 | 68.1 | 27.6 | 2.6 | 32.8 | 62.1 |
| Minnesota | 11.0 | 85.3 | 1.7 | 9.8 | 21.1 | 65.6 |
| Mississippi | * | * | * | 0 | 4.4 | 94.7 |
| Missouri | 29.5 | 57.1 | 11.6 | 0.6 | 7.8 | 73.6 |
| Montana | 13.3 | 32.3 | 50.6 | 5.6 | 16.3 | 72.2 |
| Nebraska | 0.0 | 76.3 | 18.4 | 4.8 | 9.5 | 81.0 |
| Nevada | * | * | * | 0.5 | 15.4 | 82.5 |
| New Hamps | 24.0 | 63.6 | 11.6 | 19.0 | 36.2 | 40.5 |
| New Jersey | * | * | * | 2.5 | 51.0 | 43.5 |
| New Mexico | 33.0 | 57.9 | 5.3 | 45.6 | 16.1 | 35.1 |
| New York | 49.1 | 44.5 | 4.6 | 16.4 | 43.4 | 38.2 |
| North Caroli | 19.3 | 71.8 | 7.8 | 12.1 | 12.7 | 65.0 |
| North Dakot | * | * | * | 3.1 | 6.3 | 85.4 |
| Ohio | 0.3 | 1.8 | 97.9 | 1.6 | 2.8 | 91.8 |
| Oklahoma | 0.0 | 30.4 | 67.9 | 0.2 | 12.0 | 74.2 |
| Oregon | 21.3 | 62.0 | 14.9 | 15.9 | 33.4 | 49.9 |
| Pennsylvania | 7.3 | 41.0 | 51.3 | 0.6 | 4.2 | 93.4 |
| Rhode Island | * | * | * | 28.6 | 54.3 | 8.6 |
| South Caroli | 17.6 | 49.9 | 13.2 | 3.3 | 8.1 | 86.8 |
| South Dakota | * | * | * | 9.7 | 11.1 | 77.8 |
| Tennessee | 21.7 | 64.2 | 11.3 | 1.9 | 12.8 | 80.8 |
| Texas | 11.6 | 44.6 | 43.1 | 0.8 | 10.8 | 86.7 |
| Utah | 3.1 | 12.1 | 83.5 | 0.4 | 6.5 | 90.6 |
| Vermont | * | * | * | 38.5 | 43.1 | 18.5 |
| Virginia | 7.2 | 35.6 | 53.4 | 12.3 | 28.6 | 55.9 |
| Washington | 32.4 | 61.5 | 4.7 | 27.9 | 48.8 | 18.3 |
| West Virgini | 16.0 | 44.0 | 40.0 | 2.4 | 6.0 | 90.5 |
| Wisconsin | 18.0 | 39.0 | 41.5 | 7.8 | 5.4 | 77.8 |
| Wyoming | * | * | * | 13.5 | 23.6 | 59.5 |
Excludes data from California which did not report planning status of home birth.
Does not include planned home births that were transferred to hospitals.
Data were suppressed for 12 states that had <20 birth center births; see Methods section.
Source: Authors’ calculations based on 2017 birth certificate data.
NOTE: In 2017, 4.6% of planned home and 2.4% of birth center births were reported as
Results
In 2017, there were 62,228 out-of-hospital births in the United States, comprising 1.61% of US births. This included 38,343 home births, and 19,878 birth center births (Table 1). A small proportion of out-of-hospital births were listed as “other”(3,273), “clinic/doctor’s office” (553) or “unknown” (181) location. In 2017, the planning status of home birth was reported by all states except California. For the 49 reporting states and Washington DC, about 85% of home births were planned home births, and 15% were unplanned home births.
Trends
After a gradual decline from 1990–2004 (15), the percentage of out-of-hospital births increased by 85%, from 0.87% of births in 2004 to 1.61% of births in 2017 (Figure 1). Home births increased by 77%, from 0.56% of births in 2004 to 0.99% in 2017, while birth center births more than doubled, from 0.23% of births in 2004 to 0.52% in 2017.
Non-Hispanic white women had the highest percentage of out-of-hospital births, and also the largest percent increase from 2004–2017 (Figure 2). For non-Hispanic white women, the percent of out-of-hospital births more than doubled from 1.20 percent of total births in 2004 to 2.43 percent in 2017. In 2017, 1 out of every 41 United States births to a non-Hispanic white woman was an out-of-hospital birth. Out-of-hospital births also increased for all other race/ethnicity groups, albeit from a smaller base: by 76 percent for non-Hispanic black women, by 63 percent for Hispanic and Asian or Pacific Islander women, and by 69 percent for Native American women. The increase in home births among non-Hispanic white women accounted for 81 percent of the overall increase in home births between 2004 and 2017.
State Variations in Out-of-Hospital Births
These generally upwards trends concealed large differences in out-of-hospital birth rates by state and geographic region (Table 1). Several states in the Northwestern part of the country, as well as one Eastern state had out-of-hospital birth rates above 3%, including Alaska (7.88%), Montana (4.08%), Idaho (3.77%) Washington (3.77%), Oregon (3.58%) and Pennsylvania (3.53%). In contrast, several other states had out-of-hospital birth rates from 0.4–0.6%: Alabama, Louisiana, Mississippi, Nebraska, New Jersey, and Rhode Island.
Home births were most common in Montana (2.74%), Vermont (2.56%), Wyoming (2.32%), Idaho (2.27%), Washington (2.14%), Wisconsin (2.10%), Oregon (2.10%), and Utah (2.04%), while home births were least common (below 0.5%) in Alabama, Louisiana, Mississippi, Nebraska, New Jersey, and Rhode Island.
Birth centers are available in most, but not all states (16). Twelve states (Alabama, Hawaii, Illinois, Iowa, Mississippi, Nevada, New Jersey, North Dakota, Rhode Island, South Dakota, Vermont and Wyoming) had fewer than 20 birth center births in 2017, suggesting that birth centers were not an available option for women living in those states. Among states with at least 20 birth center births in 2017, Alaska had the highest percentage of births occurring in a birth center (5.64%), followed by Washington (1.54%), Idaho (1.44%), Oregon (1.40%), Montana (1.34%), Delaware (1.29%), Pennsylvania (1.24%) and New Hampshire (1.00%).
Population Characteristics
While it is no replacement for detailed medical information, the birth certificate data does contain limited information on population characteristics which may be associated with a higher or lower risk for poor pregnancy outcome (8, 17). For example, just 0.7% of planned home and 0.9% of birth center births were to teen mothers, compared to 5.2% of hospital births (Table 2). However, 23.5% of planned home births were to mothers aged 35 and over, compared to 18.1% of birth center births and 17.5% of hospital births. Regarding mother’s education, 36.3% of planned home and 47.8% of birth center births were to mothers with a bachelor’s degree or higher, compared to 32.2% of hospital births. Only 17.7% of planned home births were to mothers having their first live birth, compared to 33.4% of birth center and 38.2% of hospital births. Only 0.9% of women having a planned home and 1.1% of women having a birth center birth smoked during pregnancy, compared to 7.0% of women with a hospital birth.
When medical risk factors were examined, we found that mothers with planned home or birth center births were less likely than those with hospital births to have a pre-pregnancy body mass index of 30 or more (obesity). In 2017, 13.2% of women having planned home births and 13.0% of women having birth center births were obese, compared to 27.3% of hospital births.
Women with planned home or birth center births were also much less likely to have a preterm, low birthweight, or multiple birth. In 2017, 2.1% of planned home births and 1.5% of birth center births were preterm, compared to 11.8% of hospital births. About 1.3% of planned home births and 0.9% of birth center births were low birthweight, compared to 8.4% of hospital births. About 0.7% of planned home births were multiple births, compared to 0.2% of birth center and 3.5% of hospital births. About 4.2% of planned home births were vaginal births after cesarean (VBAC), compared to 1.7% of birth center, and 2.0% of hospital births, which may reflect restrictions on VBAC among U.S. hospitals (18).
Compared to women giving birth in a hospital, women with planned home and birth center births were less likely to enter prenatal care during the first trimester of pregnancy, perhaps reflecting delays in finding an appropriate provider and/or working out payment and insurance issues (see below). In 2017, 55.8% of women with planned home births and 69.4% of those with birth center births initiated prenatal care during the first trimester, compared to 77.6% of hospital births.
Attendant at birth, breastfeeding and receipt of WIC food
Nearly 1/3 (29.4%) of planned home births were attended by CNM/CM midwives, and another ½ (50.7%) by non CNM/CM midwives (Table 2). Only 0.7% of planned home births were delivered by physicians, while for 19.1% of these births, the birth attendant was marked as “other”, which may include, for example, a family member, emergency medical technician, or freebirther. For birth center births, 56.6% of births were delivered by CNM/CM midwives, 36.7% by non CNM/CM midwives, and only 2.7% by physicians. In contrast, 90.6% of hospital births were delivered by physicians, and just 8.7% by CNM/CM midwives.
Women with planned home and birth center births were much more likely to initiate breastfeeding than those with hospital births. In 2017, 97.5% of women with planned home births and 97.8% of women with birth center births initiated breastfeeding, compared to 82.0% of women with hospital births. Conversely, only 6.9% of women with planned home births and 10.2% of women with birth center births received WIC food during pregnancy, compared to 38.5% of women with hospital births.
State Variations in Birth Payments
In 2017, only 8.6% of planned home births were paid for by Medicaid, compared to 17.9% of birth center births and 43.4% of hospital births (Table 2). Similarly, only 19.0% of planned home births were paid for by private insurance, compared to 47.5% of birth center and 49.4% of hospital births. Instead, more than 2/3 (67.9%) of planned home births were paid out of pocket by the women themselves. This is compared to 32.2% of birth center, and just 3.4% of hospital births. A small percentage of births in each place of birth category were reported as “other” payment method.
However, there were large variations by state in these statistics. In fully 29 US states, more than 70% of planned home births were self-paid, indicating that most women were not able to access assistance in paying for their deliveries (table 3). In contrast, <20% of planned home births were self-paid in Alaska, Rhode Island, Vermont, and Washington.
In 44 states and Washington DC, fewer than 20% of planned home births were paid for by Medicaid, and the figure was <5% for 28 states and Washington DC. Medicaid was not a viable option to pay for the cost of planned home birth in the vast majority of states in 2017. In contrast, Medicaid paid for 45.6% of planned home births in New Mexico, 38.5% of births in Vermont, 30.4% in Florida, 29.4% in Alaska, 28.6% in Rhode Island, and 27.9% in Washington. In 33 states, fewer than 20% of planned home births were paid for by private insurance, indicating that private insurance was also not a viable option to cover the costs of planned home birth in most states. In contrast, >40% of planned home births were paid for by private insurance in 6 states and Washington DC (table 3).
When birth center births were examined, we found that about 1/3 were self-paid, compared to 2/3 of planned home births. Less than 10% of birth center births were self-paid In 13 states (Alaska, Arkansas, Colorado, Connecticut, Delaware, Kentucky, Louisiana, Massachusetts, Minnesota, New Mexico, New York, North Carolina, and Washington) and Washington DC. In contrast, more than 80% of birth center births were self-paid in Ohio (97.9%), Indiana (85.8%), and Utah (83.5%).
Discussion
While the total number of births in the U.S. has been slowly declining in recent years, the absolute number of planned home and birth center births has been increasing, resulting in 1.61% of all births now occurring outside the hospital. While data available from birth certificates is limited, we found that women with planned home and birth center births were less likely to have a number of population characteristics associated with poor pregnancy outcomes, including teen births, smoking during pregnancy, obesity, and preterm, low birthweight and multiple births, and were more likely to be highly educated than women with hospital births. The percent of women having first births was lower for planned home than for hospital births, which is encouraging given findings from England that home births had better outcomes among multiparous women (19). These findings taken together suggest that women with planned home and birth center births typically have the characteristics of what are generally seen as low risk births.
In contrast, women with planned home and birth center births were more likely to begin prenatal care after the first trimester of pregnancy, which may reflect delays in finding an appropriate provider and in working out payment and insurance issues. Also, a higher percentage of planned home than hospital births were to women aged 35 and over.
The proportion of births that were VBACs was notably higher among planned home than among hospital births. Many United States hospitals do not allow access to VBAC (18), and women denied a hospital VBAC may ultimately choose to have a VBAC in an out-of-hospital setting (20–23). Improving access to hospital VBACs could possibly reduce the demand for out-of-hospital VBACs.
We found strong regional patterns in out-of-hospital births, with these births being several times more likely in the Pacific Northwest states of Alaska, Idaho, Montana, Oregon, Washington and Wyoming than in southeastern states such as Alabama, Louisiana, and Mississippi. This pattern may be explained in part by wide variations by state in private insurance and Medicaid coverage for out-of-hospital births. Ultimately, 2/3 of planned home births and 1/3 of birth center births were self-paid by the mother, compared to only 3% of hospital births. This suggests that, despite successful pilot projects (24), most current payment mechanisms are not structured to support out-of-hospital birth options for a large proportion of women seeking them. This lack of access to payment options for out-of-hospital births may prevent many women from choosing these births. Substantial variations in state laws concerning the practice and licensing of non CNM/CM midwives may also contribute to state variations in out-of-hospital births (25). Further research is needed on the relationship between the policy environment and out-of-hospital birth incidence and outcomes.
Despite cautionary editorials in major medical journal highlighting dangers of out-of-hospital births in general and home births in particular (26–28) and the substantial out-of-pocket costs associated with these births, an increasing proportion of women are choosing to give birth outside the hospital. In one national survey, mothers who had recently given birth in a hospital were asked if they would consider giving birth at home or a birth center in the future birth and 64% expressed an interest in a birth center birth and 29% would consider a home birth. One-fourth of respondents said they would definitely want a birth center birth in the future(29).
The question that obviously arises from these data is what is happening in hospital births that leads to this small but potentially much larger group of women, many of whom have experienced a hospital birth, to seek to give birth elsewhere, even when that means bucking convention and paying more to do so. Advocates of hospital birth have primarily focused on the dangers they see in home births and restricting midwifery practices that support home birth (27), while at the same time erecting legal, financial and regulatory barriers for birth centers (30). Nonetheless, we have the highest proportion of out-of-hospital births in the thirty years such data have been collected. Women generally choose out-of-hospital birth because they feel that it is safer, with lower cesarean rates and fewer interventions; they also feel more empowered and in control of their experience (31–33). Perceived poor treatment that women received when they gave birth in a hospital is also a significant factor in the choice of out-of-hospital birth (31–33). For those interested in encouraging hospital birth, the best route to take would be to determine how to make hospital birth a more supportive, collaborative and empowering experience for mothers and families. At the same time, it is possible to make out-of-hospital birth safer through the establishment of collaborative agreements between hospitals and out-of-hospital birth providers. This could improve communications between birth providers, and smooth patient transfers when needed (34–35).
Strengths of the study include the comprehensiveness of birth certificate data which include information on the entire population of about 3.9 million United States births each year. Information for the data items used in the study is considered to be reasonably well reported (36,37). Limitations include the less than national coverage for some variables. For example, smoking during pregnancy is not reported by 2 states comprising 15% of US births (9). Also, it is impossible to ascertain the planning status of home birth for fully 12% of US births, since California does not report the planning status of home birth variable on the state’s birth certificate (9). Even for the other 49 states and Washington D.C. that do report the planning status of home birth, there is no way to identify planned home births that are transferred to the hospital during labor and delivery; these are recorded on the birth certificate simply as hospital births. Thus, the planned home birth category used in this study is an underestimate of the number of women who actually intended to deliver at home in the United States (38). The term community birth (including planned home and birth center births) is generally preferred for studies of this type as it describes what these births are, rather than defining them by what they are not, and also does not inadvertently imply that hospital birth is normative, and out-of-hospital birth is alternative or marginal (10). However, due to the limitations noted above, we have chosen to stay with the out-of-hospital birth terminology for this paper, to facilitate long-term trend analysis, and because of the current inability of birth certificate data to accurately identify community births in all states.
Conclusions
Our findings document the continued growth of out-of-hospital births in the United States - a phenomenon that challenges the dominant model of maternity care and, for some mothers, raises questions about the nature of that care. Instead of a system in which the dominant focus is on the potential risks of childbirth, society might be better served by a maternity care system in which mothers, wherever they give birth, feel empowered, engaged and safe. In such a system the emphasis is less on place of birth and much more on how best to serve the needs of mothers, infants and families.
Acknowledgements
We gratefully acknowledge support from the Eunice Kennedy Shriver National Center for Child Health and Human Development grant P2C-HD041041, Maryland Population Research Center, and the Maternal and Child Health Bureau grant R40MC29444 to Boston University School of Public Health.
Contributor Information
Marian MacDorman, Maryland Population Research Center, University of Maryland.
Eugene Declercq, Department of Community Health, Boston University School of Public Health.
References
- 1.MacDorman FM, Mathews TJ, Declercq E. Trends in out-of-hospital births, 1990–2012. NCHS Data Brief No. 144 Hyattsville, MD: National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 2.MacDorman MF, Declercq E. Trends and characteristics of United States out-of-hospital births 2004–2014: New information on risk status and access to care. Birth 2016;43(2):116–124. [DOI] [PubMed] [Google Scholar]
- 3.Bovbjerg ML, Cheyney M, Brown J, Cox KJ, Leeman L. Perspectives on risk: Assessment of risk profiles and outcomes among women planning community birth in the United States. Birth 2017. September; 44 (3) 209–221. [DOI] [PubMed] [Google Scholar]
- 4.Nethery E Gordon W Bovbjerg ML, Cheyney M. Rural community birth: Maternal and neonatal outcomes for planned community births among rural women in the United States, 2004–2009. Birth 2018. June; 45(2): 120–9. [DOI] [PubMed] [Google Scholar]
- 5.Cheyney M, Bovbjerg M, Everson C, Gordon W, Hannibal D, Vedam S. Outcomes of care for 16.924 planned home births in the United States: The Midwives Alliance of North America Statistics Project, 2004 to 2009. J Midwifery Womens Health 2014; 59(1): 17–27. [DOI] [PubMed] [Google Scholar]
- 6.Vedam S, Stoll K, MacDorman M, Declercq E, Cramer R, Cheyney M, Fisher T, Butt E, Yang YT, Powell Kennedy H. Mapping integration of midwives across the United States: Impact on access, equity, and outcomes. PLoS One 2018. February 21;13(2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vedam S, Leeman L, Cheyney M, Fisher TJ, Myers S, Low LK, Ruhl C. Transfer from planned home birth to hospital: improving interprofessional collaboration. J Midwifery Womens Health 2014; 59(6):624–34. [DOI] [PubMed] [Google Scholar]
- 8.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births, final data for 2016. National vital statistics reports, vol 67 no.1 2018 Available from: https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_01.pdf. Accessed September 15, 2018. [PubMed]
- 9.National Center for Health Statistics. User Guide to the 2017 Natality Public-Use File Available at: http://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/natality/UserGuide2017.pdf. Accessed September 15, 2018.
- 10.Cheyney M, Bovbjerg ML, Leeman L, Vedam S. What’s in a name? “out-of-hospital vs “community” birth. Journal of Midwifery and Women’s Health [In press]. [DOI] [PubMed] [Google Scholar]
- 11.American Association of Birth Centers. National Birth Center Study II Available at: https://www.birthcenters.org/page/NBCSII#about. Accessed September 15, 2018.
- 12.Health Management Associates. Midwifery Licensure and Discipline Program in Washington State: Economic Costs and Benefits Olympia, WA: Washington State Department of Health, 2007. [Google Scholar]
- 13.National Center for Health Statistics. Guide to completing the facility worksheet for the certificate of live birth and report of fetal death Hyattsville, MD: National Center for Health Statistics; 2016. Accessed September 15, 2018. Available at: https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. [Google Scholar]
- 14.Martin JA, Osterman MJK, Kirmeyer SE, Gregory ECW. Measuring gestational age in vital statistics data: Transitioning to the obstetric estimate. Naional Vital Statistics Reports, vol 64 no 5 Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 15.MacDorman MF, Menacker F, Declercq E. Trends and characteristics of home and other out-of-hospital births in the United States, 1990–2006. National vital statistics reports, vol 58 no 11 Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 16.American Association of Birth Centers. AABC Press Kit March 29, 2017. Available at: https://cdn.ymaws.com/www.birthcenters.org/resource/resmgr/About_AABC_-_Documents/aabc_press_kit.pdf . Accessed September 15, 2018.
- 17.Mathews TJ, MacDorman MF, Thoma ME. Infant mortality statistics from the 2013 linked birth/infant death data set. National vital statistics reports, vol 69 no. 7 Hyattsville, Maryland: National Center for Health Statistics; 2015. [Google Scholar]
- 18.Barger MK, Dunn JT, Bearman S, et al. A survey of access to trial of labor in California hospitals in 2012. BMC Pregnancy Childbirth 2013;3(13):83. doi: 10.1186/1471-2393-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birthplace in England Collaborative Group. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: The Birthplace in England national prospective cohort study. BMJ 2011;343:d7400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacDorman MF, Declercq E, Mathews TJ, Stotland N. Trends and characteristics of home vaginal birth after cesarean delivery in the United States and selected states. Obstet Gynecol 2012;119(4):737–744. [DOI] [PubMed] [Google Scholar]
- 21.Keedle H, Schmied V, Burns E, Dahlen HG. Women’s reasons for, and experiences of, choosing a homebirth following a caesarean section. BMC Pregnancy Childbirth 2015;15:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cox KJ, Bovbjerg ML, Cheyney M, Leeman LM. Planned home VBAC in the United States, 2004–2009: Outcomes, maternity care practices, and implications for shared decision-making. Birth 2015;42(4):299–308. [DOI] [PubMed] [Google Scholar]
- 23.Tilden EL, Cheyney M, Guise JM et al. Vaginal birth after cesarean: neonatal outcomes and United States birth setting. Am J Obstet Gynecol 2017. April;216(4):403.e1–403.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jolles DR, Langford R, Stapleton S, Cesario S, Koci A, Alliman J. Outcomes of childbearing Medicaid beneficiaries engaged in care at Strong Start birth center sites between 2012 and 2014. Birth 2017: 44(4); 298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang YT, Attanasio LB, Kozhimannil KB. State scope of practice laws, nurse-midwifery workforce, and childbirth procedures and outcomes. Womens Health Issues 2016(3);:262–7. [DOI] [PubMed] [Google Scholar]
- 26.Zafman KB, Stone JL, Factor SH. Trends in characteristics of women choosing contraindicated home births. J Perinat Med 2018; 46(6):573–7. [DOI] [PubMed] [Google Scholar]
- 27.Chervenak FA, , McCullough LB, Brent RL, Levene ML, Arabin B. Planned home birth: the professional responsibility response. Am J Obstet Gynecol 2013; 208(1):31–38. [DOI] [PubMed] [Google Scholar]
- 28.Cheyney M, Burcher P, Vedam S. A crusade against home birth. Birth 2014;41(1):1–4. [DOI] [PubMed] [Google Scholar]
- 29.Declercq ER, Sakala C, Corry MP, Applebaum S, Herrlich A. Listening to MothersSM III: New Mothers Speak Out New York: Childbirth Connection, June 2013. Available from: http://transform.childbirthconnection.org/wp-content/uploads/2013/06/LTM-III_NMSO.pdf . Accessed September 15, 2018. [Google Scholar]
- 30.American Association of Birth Centers. AABC tells the FTC about barriers to birth center care American Association of Birth Centers. 2014. Available at: https://www.birthcenters.org/news/news.asp?id=229190&hhSearchTerms=%22barriers%22. Accessed September 15, 2018.
- 31.Boucher D, Bennett D, McFarlin F, Freeze R. Staying home to give birth: why women in the United States choose home birth. J Midwifery Womens Health 2009;54(2):119–26. [DOI] [PubMed] [Google Scholar]
- 32.Bernhard C, Zielinski R, Ackerson K, English J. Home birth after hospital birth: Women’s choices and reflections. J Midwifery Womens Health 2014; 59(2): 160–6. [DOI] [PubMed] [Google Scholar]
- 33.Keedle H, Schmied V, Burns E, Cahlen HG. Women’s reasons for, and experiences of, choosing a homebirth following a caesarean section. BMC Pregnancy Childbirth 2015;15:206. doi: 10.1186/s12884-015-0639-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neilson D Making home birth safer in the United States through strategic collaboration: The Legacy Health System experience. Birth 2015;42(4):287–289. [DOI] [PubMed] [Google Scholar]
- 35.Home Birth Consensus Summit, Collaboration Task Force. Best Practice Guidelines: Transfer from Planned Home Birth to Hospital. Home Birth Consensus Summit, 2014 Available at: http://www.homebirthsummit.org/wp-content/uploads/2014/03/HomeBirthSummit_BestPracticeTransferGuidelines.pdf. Accessed September 15, 2018.
- 36.Martin JA, Wilson EC, Osterman MJK, Saadi EW, et al. Assessing the quality of medical and health data from the 2003 birth certificate revision: Results from two states. National Vital Statistics Reports, vol 62 no 2 Hyattsville, MD: National Center for Health Statistics, 2013. [PubMed] [Google Scholar]
- 37.Dietz P, Bombard J, Mulready-Ward C, Gauthier J, et al. Validation of selected items on the 2003 U.S. Standard Certificate of Live Birth: New York City and Vermont. Public Health Rep 2015;130:60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Declercq E, MacDorman MF, Menacker F, Stotland N. Characteristics of planned and unplanned home births in 19 states. Obstet Gynecol 2010; 116(1):93–9. [DOI] [PubMed] [Google Scholar]


