Abstract
Because human patients with monkeypox virus (MPXV) infection report painful symptoms, it is reasonable to assume that animals infected with MPXV experience some degree of pain. Understanding whether and how analgesics affect MPXV disease progression is crucial when planning in vivo challenge experiments. In the current study, we challenged prairie dogs with a low dose (4 × 103 pfu) of MPXV and treated with meloxicam (NSAID) or buprenorphine (opioid); control animals did not receive analgesia or received analgesia without MPXV challenge. Subsets of animals from each group were serially euthanized during the course of the study. Disease progression and viral kinetics were similar between groups, but MXPV-infected, meloxicam-treated animals showed increasing trends of morbidity and mortality compared with other groups. Differences between no-analgesia MPXV-infected control animals and MPXV-infected animals treated with buprenorphine were minimal. The findings in the current study allow more informed decisions concerning the use of analgesics during experimental MPXV challenge studies, thereby improving animal welfare. In light of these findings, we have modified our pain scale for this animal model to include the use of buprenorphine for pain relief when warranted after MPXV challenge.
Abbreviations: dpi, days postinfection; MPXV, monkeypox virus
Since the eradication of smallpox (caused by Variola virus), the closely related Monkeypox virus (MXPV) has become the most important human health threat within the genus Orthopoxvirus. As evidenced by the 2003 United States outbreak, as well as sporadic outbreaks of MPXV within central Africa, there is a continued need to study this zoonotic virus.10,23,24 In addition, MPXV provides a surrogate for the study of related orthopoxviruses including Variola virus. Such research is critical in the event of a reemergence (whether due to natural circumstances or a biothreat event, such as synthetic reconstruction). Previous studies of the prairie dog MPXV model showed that after intranasal or scarification challenge with a reasonable viral dose (approximately 104 to 105 pfu), animals developed a disease that closely resembled human monkeypox infection including a protracted incubation period before the development of generalized lesions.11 In addition, these studies have shown that the prairie dog model is valuable for comparison of disease attributable to the 2 MPXV clades (West African and Congo Basin), primarily by demonstrating differences in mortality and morbidity.11,12,13
Human patients with MXPV infection report painful symptoms during the course of disease including headache, sore throat, back pain, and mouth sores.9 Therefore, it is likely that animals infected with MXPV experience some degree of pain, especially during robust infections. Despite this, analgesics are often withheld during challenge studies due to concerns that the viral disease course might be altered. Indeed, our studies previously did not use analgesics during MPXV challenge prairie dog studies due to this concern. NSAID, including salicylates and glucocorticoids are commonly prescribed to alleviate pain in both humans and animals. Meloxicam is an NSAID typically used in veterinary medicine and inhibits both COX1 and COX2. Although important in clinical settings, NSAID have been shown to inhibit the nuclear factor NFкB, which is the primary regulator of inflammation and plays a key role in regulating the immune response, including to viral infection.17 Orthopoxviruses have been shown to encode multiple proteins that act in various ways to inhibit NFкB activity.21,26 The ability of Orthopoxviruses to modulate NFкB activation likely plays an important role in the ability of these viruses to cause disease, therefore the utilization of substances that inhibit NFкB activation (such as NSAID) could potentially change the viral lifecycle and resulting disease progression/presentation during challenge studies.7
Opioids, such as buprenorphine, are other common drugs used to alleviate pain. These drugs have been shown to have multiple adverse effects that may exacerbate morbidity during viral infections. For example, MPXV infection can cause respiratory distress in prairie dogs which could be confused with the respiratory depression that has been reported with opioid analgesics.20 In addition, opioid analgesics in rats have been shown to cause temperature deregulation which could negatively affect the ability of infected animals to recover after anesthesia and could alter behavior and eating habits.2 Lastly, MPXV tropism in the liver is extensive and has been shown to alter liver enzymes of infected prairie dogs. This impact could be exacerbated by opioid use as these drugs are primarily metabolized in the liver.6
Within this study, we sought to determine 1) whether the use of either meloxicam or buprenorphine within the prairie dog resulted in adverse events (assessed through weights, clinical observation and blood chemistries) and 2) whether the use of either meloxicam or buprenorphine in conjunction with MPXV infection resulted in increased pathogenesis (assessed through body weight, clinical observation, blood chemistries, immune response, viral load and pathology). Our hypothesis was that the use of either analgesic would result in increased morbidity and mortality during in vivo MPXV challenge studies. Because buprenorphine did not, in fact, increase morbidity and mortality, we have modified our pain scale, which now includes the use of buprenorphine for pain relief within prairie dogs, thereby improving animal welfare during MPXV challenge studies with this animal model.
Materials and Methods
Animals.
Wild-caught, juvenile black-tailed prairie dogs (Cynomys ludovicianus) were obtained from Texas. At the time of infection, animals were approximately 8 mo old and had been prescreened by a veterinarian, determined to be in good health status, and found negative for the presence of antiorthopoxvirus antibodies. A sterile passive integrated transponder tag was injected subcutaneously at the base of the neck for animal identification. The average starting weight for animals was 446 g (range, 360 to 620 g). During experimental infections animals were housed individually in large HEPA-filtered ventilated cages rack system within a BSL3E animal room. The study was performed according to the IACUC guidelines of the Centers for Disease Control under an approved protocol (2367HUTPRAC). In addition to prairie dog chow (Brisky, Franklinville, NY, or Exotic Nutrition, Newport News, VA) and hay, animals were provided with monkey biscuits, mixed nuts, and approved fruit and vegetables for added dietary enrichment and assessment of appetence.
Analgesics.
Because animals used during MXPV challenge studies do not typically need pain relief until several days after infection, administration of analgesics began at 3 d postinfection (dpi). Animals that were given meloxicam on 3 through 21 dpi, or until the animal's predetermined day of euthanasia. Meloxicam administration stopped 2 d earlier than buprenorphine (dosed day 3 to 23) due to an injection site reaction in some of these animals. We were careful to deliver future injections well away from any lesions observed.
Meloxicam (4 mg/kg) was given to animals by subcutaneous injection once daily. This dosage was based on standard treatment regimens of meloxicam in rats and mice.16 The volume of drug administered was based on the weight of each animal, and the total volume administered at each treatment was 0.5 to 1.5 mL.
Buprenorphine (0.1 mg/kg) was given by subcutaneous injection every 12 h. This dosage was based on studies with buprenorphine in rats and mice.16 The volume of drug administered was based on the weight of each animal, and the total volume administered at each treatment was between 0.5 to 1.5 mL.
Animal groups.
Forty-one prairie dogs were divided into 5 experimental groups (plus 2 control animals that received PBS). The 4 groups that were treated with an analgesic contained a total of 18 males and 18 females, which were distributed among the groups. On day 0, animals (n = 27) were challenged intranasally with WA MPXV (4 × 103 pfu in 10 µL). This dosage was based on previous studies, using a dose that resulted in 100% morbidity with minimal mortality in the prairie dog MPXV model.12 Among the challenged animals, 5 received no analgesic treatment (to serve as positive controls); 11 were treated once daily with meloxicam and 11 were treated twice daily with buprenorphine. Fourteen animals were uninfected but treated with appropriate analgesic (meloxicam (n = 7) or buprenorphine (n = 7)) for comparison of blood chemistry values, clinical signs, and pathologic findings in tissues collected during necropsy. On sampling days (see later section), the animals received the appropriate drug once while anesthetized; for buprenorphine, the 2nd dose was administered without anesthesia and while the prairie dog was held at the scruff of the neck while using bite-proof gloves. This procedure was due to the belief that anesthetizing prairie dogs twice daily is not beneficial to the animals’ health and may negatively affect disease progression. For anesthesia, inhalational isoflurane was used to induce the animals directly within their cages; nose cones were then used to maintain anesthesia during procedures. On nonsampling days and if not scheduled for euthanasia, prairie dogs receiving analgesic treatment were appropriately dosed daily with meloxicam and every 12 h with buprenorphine (either under anesthesia or while scruffed, being consistent throughout the study).
On sampling days 4, 6, 9, and 12 dpi, subsets of prairie dogs from each group (n = 1 or 2) were euthanized while under anesthesia; these time points were selected according to earlier studies using this model.13 Animals that were not euthanized were anesthetized, weighed, checked for MPXV lesions (and other signs of morbidity), and had blood and oral swabs collected. Animals not euthanized by day 12 were sampled on day 17, as described earlier. A pain scoring system was previously established13 for the MPXV challenge prairie dog model and was used during the current study to guide enhanced care and monitoring of the animals and provided guidance regarding when to administer subcutaneous fluids or euthanize an animal. All animals that survived infection were euthanized 24 d after inoculation. After death or euthanasia, all prairie dogs underwent a complete necropsy, as described later.
Virus.
The WA MPXV strain used to challenge prairie dogs, MPXV-USA-2003-044, was isolated during the 2003 United States outbreak.19,23 The virus has been fully sequenced and underwent 2 passages in African green monkey kidney cells (BSC40 line) prior to seed pool production; sucrose-cushion semipurified preparations of virus were used for animal challenges.
Animal inoculation.
Inoculation doses (4 × 103 pfu) were calculated according to the morbidity and mortality rates that we observed in our previous studies with this animal model. Briefly, a challenge dose of 6 × 103 pfu WA MPXV resulted in disease morbidity, including skin lesions and viral shedding identified in oral cavity samples, in 100% of animals with 25% mortality.12 Because our goal was to achieve morbidity with limited mortality so that differences in the clinical signs of animals treated with or without analgesic might be observed, we challenged prairie dogs with a slightly lower dose in the current study than used previously. The viral strain stock was diluted in PBS. Inocula titers were reconfirmed through standard plaque assays (described later). Prairie dogs were inoculated intranasally while they were under general anesthesia using 1% to 5% isoflurane administered through a vaporizer (VetEquip, Livermore, CA); the total inoculation volume was 10 µL (5 µL in each nostril). In addition, the 14 animals that served as treatment-only controls were mock-infected by using PBS.
Observations and sampling.
Throughout the 24-dpi study period, individual animals were observed for signs of morbidity (inappetence, decreased activity, recumbence with reluctance to move, etc.) and clinical lesions, including skin rash. On scheduled euthanasia days (4, 6, 9, and 12 dpi) and at 17 dpi, oral swabs, blood, weights, and lesion counts were collected from all animals while under general anesthesia (as described earlier) before subsets of anesthetized animals were euthanized by intracardiac administration of sodium pentobarbital (100 mg/kg). For those animals euthanized, blood and tissue samples were also collected. For nonterminal collection, blood was collected from the saphenous vein according to IACUC-approved protocol. Strict euthanasia criteria were applied throughout the study as follows: no response to touch, loss of 25% or more of the starting body weight, or accrual of a total score of 10 on the following scale (decreased activity, 2 points; lethargy, unsteady gait, or inappetence, 3 points; labored breathing and/or recumbence, 5 points).
Necropsy and tissue specimen collection.
Euthanasia of all animals was performed according to IACUC standards in a BSL3 laboratory and by using BSL3 PPE. Complete necropsies were performed after euthanasia with duplicate sets of tissues taken. Instruments were cleaned and decontaminated with 5% Microchem (Westborough, MA), 70% ethanol, and sterile water between collections of each tissue. One set of tissues was frozen at –70◦C prior to further processing. The other tissue set, including the head, was placed into 10% buffered formalin solution for histologic evaluation. Oral and ocular swabs were collected by using sterile individual Dacron swabs and stored frozen without diluent. Serum was separated from whole blood and processed for serology and clinical chemistry. Tissues and swabs were subsequently processed and further prepared for DNA analysis and virus isolation.
Sample preparation for PCR and viral growth.
Sample processing was performed under BSL2 conditions with BSL3 work practices. The BioRobot EZ1 Workstation (Qiagen, Hilden, Germany) was used for genomic DNA extraction from all blood, swab, and tissue samples. Samples were incubated at 56 °C for 1 h to inactivate viable virus particles prior to DNA extraction. For whole blood samples, 100 µL was used for DNA extraction, and the remaining blood was used for tissue culture propagation. For each swab collected, 400 µL of PBS was added, and Swab Extraction Tube Systems (SETS, Roche, Basel, Switzerland) protocol was used to recover a sample from the swab. DNA was extracted from 100 µL of the swab lysate. The remaining swab eluate was used for virus isolation. For tissue preparation, tissue samples were weighed, and 1-mL aliquots of PBS containing SPEX beads (SPEX SamplePrep, Metuchen, NJ) were prepared. The PBS–bead aliquot was then poured into a tube containing the individual tissue sample. The GenoGrinder 2000 (SPEX SamplePrep) was used following the manufacturer's instructions to create a tissue homogenate; 100 µL of the homogenate was used for extraction of DNA. The remaining homogenate was used for virus isolation.
Real-time PCR analysis.
Samples were evaluated through real-time PCR analysis using forward and reverse primers and probes complimentary to the conserved nonvariola orthopoxvirus E9L (DNA polymerase) gene.18 Purified MPXV DNA (10 fg to 1 ng) was used as standard controls to allow quantification of viral DNA. MPXV-positive samples produced Ct values (in duplicate) of 37 or lower; weakly positive samples yielded Ct values of 38 or 39 (in duplicate).
Virus-tissue infectivity.
All samples were stored at –70◦C until virus isolation. Previous analyses demonstrated that real-time PCR analysis of MPXV DNA detects trace amounts of MPXV DNA.10 Therefore, specimens were first tested for the presence of orthopoxvirus DNA by PCR analysis and, when positive, were subsequently evaluated for viable virus through tissue culture propagation. Each swab or tissue sample was titrated in duplicate by using 10-fold dilutions of swab eluate or tissue slurry on BSC40 cell monolayers, incubated at 35.5 °C and 6% CO2 for 72 h, and subsequently stained with crystal violet stain containing formalin to visualize plaques. Titers were expressed as pfu per milliliter of blood or swab eluate or pfu per gram of tissue.
Serologic analysis.
A modified ELISA was used for analysis of anti orthopoxvirus immunoglobulins in separated serum, as previously described in detail.11,14
High-content screening–green fluorescent protein neutralization assay.
Beginning on day 9 pi, serum samples were further tested in the high content screening–green fluorescent protein neutralization assay as described previously.15 In brief, serum samples were serially diluted from 1:40 to 1:1280 and neutralizing antibody titers against Vaccinia virus-labeled green fluorescent protein were measured. This assay detects the percentage of responder cells (which produce green fluorescent protein; this value is then normalized to control wells to produce the relative percentage of responders). The reported values are titers for 50% relative responders, which are equivalent to the serum dilution that neutralizes 50% of viral infection (ID50) in a traditional plaque reduction neutralization titer assay. The ID50 was calculated by using a modified variable slope sigmoidal equation (Hill equation, Levenberg Marquardt algorithm) and Prism 5.0 (GraphPad Software, La Jolla, CA), with goodness of fit to this sigmoidal curve (represented by R2; all R2 values considered positive were above 0.9000) calculated by the least-squares method.
Blood chemistry values.
Serum was separated out from whole blood, transferred to a clean tube and stored at –20 °C prior to analysis. The Piccolo blood chemistry analyzer (Abaxis, Union City, CA) was used to determine the following blood chemistry parameters: sodium, globulins, potassium, glucose, calcium, BUN, creatinine, ALP, ALT, amylase, phosphorus, total bilirubin, albumin, and total protein.
Histopathologic evaluation.
After euthanasia, a necropsy was performed, and tissues were collected as described earlier. Tissues were fixed in 10% neutral-buffered formalin for at least 48 h and then transferred to 70% ethanol for routine processing to create paraffin blocks, which were subsequently sectioned at 3 μm. Animal heads were decalcified by using standard techniques. Slides were stained with hematoxylin and eosin for histopathologic evaluation.
Statistical analyses.
Because data were not normally distributed, nonparametric statistical analyses were used. The Wilcoxon rank-sum test was used to compare the percentage change in blood chemistry parameters from day 0 to day 9 for each group of animals. A P value of 0.05 or less was considered statistically significant. Data analysis was performed by using SAS version 9.3 (SAS Institute, Cary, NC)
Results
Clinical observations.
Meloxicam-treated, MPXV-uninfected control prairie dogs tolerated the NSAID analgesic with minimal clinical signs (Table 1). Animals in this treatment group lost less than 5% of body weight, and appetence and activity remained constant throughout the study. The only side effect due to the daily subcutaneous injection was the formation of a single abscess each on the dorsum of 3 animals beginning on day 9, 16, or 21 (Table 1). The average clinical score for this group of animals was 0.4 (range, 0 to 1; Table 1). Necropsy findings for this group revealed no abnormalities, with the exception that 1 of the 3 animals euthanized at 24 dpi (PD12057) had an enlarged liver with a prominent reticular pattern.
Table 1.
Clinical and laboratory findings in prairie dogs
| Euthanasia day (dpi) | Animal | Maximal weight loss (%) | Clinical signs | Maximal clinical score | Injection site lesion (day of onset [dpi]) | Gross pathology | Maximal no. of lesions observed | OPXV antibodies detected | Neutralizing antibodies detected | Viral DNA in tissue (no. positive / no. tested) | Viable virus in tissue (no. positive / no. tested) | Highest viral load, site | |
| Meloxicam only | |||||||||||||
| 4 | PD12019 | 0 | NO | 0 | NO | NO | NA | NA | NA | NA | NA | NA | |
| 6 | PD12017 | 4.1 | NO | 0 | NO | NO | NA | NA | NA | NA | NA | NA | |
| 9 | PD12021 | 1.7 | NO | 0 | NO | NO | NA | NA | NA | NA | NA | NA | |
| 12 | PD12006 | 0 | Lesion on dorsum due to meloxicam injection | 1 | Yes (9) | NO | NA | NA | NA | NA | NA | NA | |
| 24 | PD12029 | 2.7 | NO | 0 | NO | NO | NA | NA | NA | NA | NA | NA | |
| PD12036 | 1.1 | Lesion on dorsum due to meloxicam injection | 1 | Yes (21) | NO | NA | NA | NA | NA | NA | NA | ||
| PD12057 | 0 | Lesion on dorsum due to meloxicam injection | 1 | Yes (16) | Liver enlarged, pale, with prominent reticular pattern | NA | NA | NA | NA | NA | NA | ||
| Buprenorphine only | |||||||||||||
| 4 | PD12056 | 0.6 | NO | 0 | NO | NO | NA | NA | NA | NA | NA | NA | |
| 6 | PD12001 | 7.9 | NO | 0 | NO | Slightly friable. Liver, bloody at cut surface | NA | NA | NA | NA | NA | NA | |
| 9 | PD12072 | 4.2 | NO | 0 | NO | NO | NA | NA | NA | NA | NA | NA | |
| 12 | PD12045 | 4.2 | NO | 0 | NO | NO | NA | NA | NA | NA | NA | NA | |
| 24 | PD12055 | 0 | NO | 0 | NO | Liver light brown with nutmeg appearance; very friable | NA | NA | NA | NA | NA | NA | |
| 24 | PD12071 | 2.4 | NO | 0 | NO | Liver slightly pliable; bleeding on surface | NA | NA | NA | NA | NA | NA | |
| 24 | PD12046 | 3.8 | NO | 0 | NO | Surface of liver adjacent to diaphragm had multiple white spots | NA | NA | NA | NA | NA | NA | |
| MPXV only | |||||||||||||
| 4 | PD12028 | 3.3 | NO | 0 | NA | NO | 0 | Negative | NE | 4/12 | 0/12 | NE | |
| 6 | PD12058 | 2.4 | NO | 0 | NA | NO | 0 | Negative | NE | 10/11 | 8/11 | 6.0×105, spleen | |
| 9 | PD12014 | 4.2 | RD, ruffled fur | 3 | NA | Mild lymph-adenopathy; gallbladder moderately enlarged; spleen moderately enlarged with a finely nodular appearance of small white lesions; mesenteric lymph node slightly enlarged; small intestine thin- walled with yellow, mucoid substance | 0 | Negative | Negative | 12/12 | 11/12 | 1.7×108, spleen | |
| 12 | PD12011 | 1.7 | Nasal discharge | 2 | NA | NO | 2 | Positive | Positive | 11/11 | 8/11 | 1.9×107, nasal | |
| 24 | PD12034 | 13.7 | RD, nasal discharge, ruffled fur | 6 | NA | Liver firm and pale brown, with rounded edges | 13 | Positive | Positive | 12/12 | 1/12 | 3.4×104, nasal | |
| MPXV + meloxicam | |||||||||||||
| 4 | PD12027 | 0 | NO | 0 | NO | NO | 0 | NE | NE | 5/12 | 0/12 | NA | |
| 4 | PD12004 | 4.8 | NO | 0 | NO | NO | 0 | NE | NE | 5/12 | 0/12 | NA | |
| 4 | PD12112ᵻ | 1.1 | NO | 0 | NO | Mild lymph-adenopathy | 0 | NE | NE | 5/12 | 1/12 | 2.8×102, lymph node | |
| 6 | PD12077 | 8.5 | NO | 1 | NO | NO | 0 | Negative | NE | 11/12 | 3/12 | 2.2×104, spleen | |
| 9 | PD12037 | 9.5 | Ruffled fur, mild abdominal bloat | 5 | NO | Spleen faintly mottled, possible early internal lesions; possible mild mesenteric lymph node enlargement; all lung lobes with dark mottling | 1 | Negative | Positive | 11/12 | 9/12 | 1.7×107, tongue | |
| 9 | PD12038 | 6.9 | NO | 1 | NO | Mild lymph-adenopathy | 1 | Negative | Negative | 10/11 | 8/11 | 5.8x106, nasal | |
| 12 or 18a | PD12024 | 0 | NO | 0 | NO | NO | 0 | Negative | Negative | 0/12 | NE | NE | |
| 12 or 18 | PD12078 | 10.3 | Bloated, ruffled fur, bloody nose, urine- matted fur | 10 | NO | Mild lymph-adenopathy; few scattered small white nodules on liver; gall-bladder slightly enlarged; colon moderately gas-filled. Linear blood clot in trachea, lungs hemorrhagic and mottled. | 2 | Negative | Positive | 12/12 | 9/12 | 5.1×107, tongue | |
| 12 or 18 | PD12114ᵻ | 28.4 | RD, de-hydration, bloating, nasal discharge, bloody nose, lethargic | 10 | NO | Mesenteric area covered with yellowish fluid, friable spleen and abdominal fat, hepato-megaly and friable liver, intestinal adhesions | 18 | Positive | Positive | 12/13 | 10/13 | 3.1×106, nasal | |
| 24 | PD12096 | 2.2 | Lesion on dorsum due to meloxicam injection, RD | 4 | Yes (14) | NO | 8 | Positive | Positive | 10/12 | 1/12 | 4.6.0×102, nasal | |
| 24 | PD12059 | 6.1 | Bloating, nasal discharge, RD, de-hydration | 8 | Yes (15) | NO | 1 | Positive | Positive | 11/12 | 0/12 | NE | |
| MPV + buprenorphine | |||||||||||||
| 4 | PD12002 | 9.2 | NO | 0 | NO | NO | 0 | Negative | NE | 4/12 | 0/12 | NE | |
| 4 | PD12064 | 6.0 | NO | 1 | NO | NO | 0 | Negative | NE | 4/12 | 0/12 | NE | |
| 6 | PD12092 | 2.7 | NO | 0 | NO | NO | 0 | Negative | NE | 10/12 | 6/12 | 2.0×106, tongue | |
| 6 | PD12025 | 7.7 | NO | 1 | NO | NO | 0 | Negative | NE | 11/12 | 1/12 | 6.2×102, nasal | |
| 9 | PD12115 | 3.9 | NO | 0 | NO | NO | 0 | Negative | Positive | 10/12 | 5/12 | 6.8×105, small intestine | |
| 9 | PD12085 | 8.1 | NO | 1 | NO | NO | 0 | Negative | Negative | 9/12 | 2/12 | 2.9×105, spleen | |
| 12 | PD12049 | 19.1 | RD, nasal discharge | 8 | NO | Lymph-adenopathy, left kidney possibly dilated | 3 | Positive | Positive | 10/11 | 8/11 | 1.9×108, nasal | |
| 12 | PD12119 | 18.4 | RD, nasal discharge, facial edema, ruffled fur | 9 | NO | Lymph-adenopathy, lungs had foamy liquid on cut surface, right lung dark and brown on dorsal surface, liver friable and pale, gas and liquid in jejunum | 0 | Positive | Positive | 12/12 | 3/12 | 8.5×105, nasal | |
| 24 | PD12091 | 4.6 | RD | 4 | NO | Liver has nutmeg appearance, areas of discoloration and hepato-megaly; spleen congested | 6 | Positive | Positive | 3/12 | 0/12 | NE | |
| 24b | PD12079 | 3.2 | NO | 0 | NO | NO | NO | Negative | Negative | 0/12 | NE | NE | |
| 24b | PD12105 | 3.2 | NO | 0 | NO | NO | NO | Negative | Negative | 0/12 | NE | NE | |
NA, not applicable; NE, not examined; NO, nothing observed; RD, respiratory depression during anesthesia
Premature death
Infection unsuccessful
Similarly to meloxicam control animals, the buprenorphine-treated, MPXV-uninfected control animals appeared to tolerate the opioid with no clinical signs; animals in this treatment group lost less than 8% of body weight, and appetence and activity remained constant throughout the study (Table 1). No respiratory depression or other clinical signs were observed. Clinical scores for all of these animals remained at 0 for the study duration (Table 1). At necropsy, the livers of 4 of the 7 animals were friable or discolored (or both).
MPXV-challenged no-analgesia control animals had a disease presentation similar to that previously characterized in this model.11-13 Prairie dogs euthanized at 4 and 6 dpi did not show clinical signs of disease (Table 1). The animal euthanized at 9 dpi (PD12014) presented with ruffled fur and displayed respiratory depression during anesthesia. The clinical scores for these animals ranged from 0 to 6, with an average of 2.2 (Table 1). On necropsy, numerous gross lesions attributable to MPXV infection were observed (Table 1). The 2 remaining MPXV control animals presented with cutaneous MPXV rash at 11 dpi (PD12011) and 14 dpi (PD12034). Because we used a low-dose challenge of the less virulent West African MPXV clade, numbers of cutaneous pox lesions were minimal (Table 1). As planned, PD12011 was euthanized at 12 dpi; with the exception of cutaneous pox lesions and nasal discharge, no other clinical signs or gross lesions were seen. In addition, PD12034 was euthanized at 24 dpi, after recovering from MPXV challenge. During the infection, in addition to cutaneous lesions, PD12034 showed respiratory depression under anesthesia, nasal discharge, ruffled fur, inappetence, and 13.7% loss of body weight.
Clinical findings in animals challenged with MPXV and treated with meloxicam are summarized in Table 1; clinical scores were highest for this group of animals (mean, 3.5; range, 0 to 10). In addition, PD12112 unexpectedly died during anesthesia on day 4, after 1 d of meloxicam treatment. During necropsy, this animal was noted to have mild lymphadenopathy (a known clinical sign of MPXV infection).9 The 2 animals in this group that were euthanized as scheduled at 9 dpi had numerous clinical signs attributed to viral infection (Table 1). At 12 dpi, PD12078 was euthanized as planned. Although this animal had developed only 2 MXPV lesions (in the buccal mucosa), it had more severe clinical signs than the MXPV control animals, including bloody nose, gastrointestinal bloat, and matted or ruffled fur. Inappetence was noted during the course of infection, and 10.3% weight loss occurred prior to euthanasia. Gross necropsy findings also were extensive in this animal (Table 1). Although PD12114 was scheduled for euthanasia at 24 dpi, this animal instead was euthanized at 18 dpi due to extreme weight loss (28.4%) and measures of morbidity. This animal first developed cutaneous lesions at 12 dpi and had a total of 18 pox lesions at the time of euthanasia. Clinical signs included respiratory depression under anesthesia, dehydration, gastrointestinal bloat, nasal discharge or blood, and lethargy. In addition, numerous gross lesions were seen during necropsy (Table 1). Similar to the meloxicam treatment controls, the 2 animals in this group that were euthanized at 24 dpi (PD12096 and PD 12059) had subcutaneous abscesses on the dorsum due to daily analgesic administration. At the time of necropsy, there were no other abnormal findings.
Clinical findings in animals challenged with MPXV and treated with buprenorphine beginning on day are summarized in Table 1; the clinical score average for this group (2.7 with a range of 0 to 9) were similar to the average clinical score of the MPXV control group (2.2). Until day 12 pi, no animals in this group had clinical signs of infection. Only 2 animals in the MPXV challenged/ buprenorphine treated group developed cutaneous lesions. Animals PD12049 and PD12119 were euthanized at 12 dpi and had moderate weight loss during the course of infection (19.1% and 18.4%, respectively). Both of these animals had respiratory depression under anesthesia, nasal discharge, and, for PD12119, facial edema and ruffled fur. Several gross lesions were seen during necropsy of these 2 animals (Table 1). The prairie dog PD12091 was euthanized at 24 dpi, having developed only 6 cutaneous MPXV lesions, minimal weight loss (4.6%), and respiratory depression during the study. Gross lesions in the liver and spleen were seen during necropsy.
Blood chemistry results.
Although significant differences emerged in some of the blood chemistry values (ALP, ALT, BUN, globulins, potassium, sodium, and phosphorus) when comparing between 0 and 9 dpi (Table 2), none of the conditions (meloxicam, buprenorphine, MPXV) exerted a significant effect when compared with PBS (PBS only; Table 2). Although too few data were available at study end to statistically compare the mean percentage change at 24 dpi, trends were observed. Uninfected animals treated with meloxicam had decreased albumin and increased BUN compared with PBS animals, and buprenorphine-treated animals had increased ALT values compared with PBS animals (data not shown).
Table 2.
Statistical comparison (Wilcoxon rank-sum test) of the percentage change in blood chemistry values from 0 to 9 dpi Only blood chemistries with statistical findings are shown.
| MPXV + meloxicam | MPXV + buprenorphine | MPXV only | Meloxicam only | Buprenorphine only | ||
| ALP | ||||||
| MPXV + meloxicam | — | |||||
| MPXV + buprenorphine | 0.19 | — | ||||
| MPXV only | 0.79 | 0.11 | — | |||
| Meloxicam only | 0.73 | 0.03 | 0.63 | — | ||
| Buprenorphine only | 0.06 | 0.41 | 0.04 | 0.02 | — | |
| PBS only | 0.57 | 0.80 | 0.40 | 0.27 | 0.19 | |
| ALT | ||||||
| MPXV + meloxicam | — | |||||
| MPXV + buprenorphine | 0.91 | — | ||||
| MPXV only | 1 | 0.86 | — | |||
| Meloxicam only | 0.19 | 0.74 | 0.23 | — | ||
| Buprenorphine only | 0.03 | 0.29 | 0.04 | 0.73 | — | |
| PBS only | 0.38 | 0.80 | 0.40 | 0.80 | 0.38 | |
| BUN | ||||||
| MPXV + meloxicam | — | |||||
| MPXV + buprenorphine | 0.91 | — | ||||
| MPXV only | 0.04 | 0.06 | — | |||
| Meloxicam only | 0.08 | 0.11 | 0.06 | — | ||
| Buprenorphine only | 0.15 | 0.02 | 0.04 | 0.91 | — | |
| PBS only | 0.10 | 0.13 | 0.20 | 0.13 | 0.1 | |
| Globulins | ||||||
| MPXV + meloxicam | — | |||||
| MPXV + buprenorphine | 1 | — | ||||
| MPXV only | 0.54 | 0.63 | — | |||
| Meloxicam only | 0.02 | 0.03 | 0.06 | — | ||
| Buprenorphine only | 0.38 | 0.41 | 0.25 | 1 | — | |
| PBS only | 0.81 | 1 | 1 | 0.20 | 0.38 | |
| Potassium | ||||||
| MPXV + meloxicam | — | |||||
| MPXV + buprenorphine | 0.19 | — | ||||
| MPXV only | 0.25 | 0.11 | — | |||
| Meloxicam only | 1 | 0.49 | 1 | — | ||
| Buprenorphine only | 0.42 | 0.78 | 0.04 | 0.56 | — | |
| PBS only | 0.86 | 0.53 | 0.80 | 0.80 | 0.57 | |
| Phosphorous | ||||||
| MPXV + meloxicam | — | |||||
| MPXV + buprenorphine | 0.19 | — | ||||
| MPXV only | 1 | 0.40 | — | |||
| Meloxicam only | 0.19 | 0.03 | 0.40 | — | ||
| Buprenorphine only | 1 | 0.41 | 0.79 | 0.19 | — | |
| PBS only | 0.57 | 0.13 | 0.40 | 0.80 | 0.57 | |
| Sodium | ||||||
| MPXV + meloxicam | — | |||||
| MPXV + buprenorphine | 0.91 | — | ||||
| MPXV only | 0.57 | 0.63 | — | |||
| Meloxicam only | 0.56 | 0.69 | 1 | — | ||
| Buprenorphine only | 0.42 | 0.41 | 0.04 | 0.06 | — | |
| PBS only | 0.57 | 1 | 0.80 | 0.53 | 1 | |
Significant differences (P ≤ 0.05) are bolded.
Antibody response.
Serum from challenged animals was tested by ELISA for antiorthopoxvirus antibody titers; beginning at 9 dpi, serum samples were further tested for neutralization titers. Prairie dogs within the 3 groups mounted an ELISA-measurable immune response at 9 to 12 dpi, similar to our other studies with this animal model.13 In previous studies with MPXV in prairie dogs, cutaneous lesions and increased antibody titers (measured by ELISA) consistently occurred simultaneously. However, in the current study, one MPXV–buprenorphine animal (PD12091) and 2 MPXV–meloxicam animals (PD12078, PD12096) developed pox lesions on day 12 but were negative by ELISA, although they did have neutralizing titers at this time point (data not shown) as measured by the neutralization assay. The ELISA and neutralization values at 12 and 17 dpi were similar between MPXV control animals and those challenged and treated with either meloxicam or buprenorphine (Table 3).
Table 3.
Comparison of ELISA and viral neutralization titers in prairie dog serum
| MPXV only | MPXV + meloxicam | MPXV + buprenorphine | |
| ELISA results | |||
| 12 dpi | 0.38 (average; n = 2) | 0.19 (average; n = 3) | 0.09 (average; n = 3) |
| 17 dpi | 0.64 (n = 1) | 0.68 (average; n = 3) | 0.68 (n = 1) |
| Neutralization titers (50% RPR) | |||
| 12 dpi | 199 (average; n = 2) | 284 (average n = 3) | 291 (average; n = 3) |
| 17 dpi | 93 (n = 1) | 349 (average; n = 3) | 280 (n = 1) |
ELISA values are given as the optical density minus the cut-off value; neutralization titers are given as the 50% relative percentage of responders (RPR; responder cells produce green fluorescent protein) titers.
Kinetics of viral spread.
In MPXV-challenged control animals, viral DNA was first detected at 4 dpi in the blood, lungs, stomach, and liver (Table 4). Viable virus was present from the majority of samples collected from this group of animals beginning at 6 dpi. By day 24, only the nasal cavity had viable virus remaining, but viral DNA was still detectable in all tissues collected, except blood. When we looked at the peak viral load for the MPXV control animals (each tissue throughout the study), we saw a range of 1 × 102 pfu (blood) to 2 × 108 pfu (spleen) at 9 dpi.
Table 4.
Incidental pathology findings in prairie dogs
| Euthanasia day (dpi) | Animal | Incidental findings | ||
| Meloxicam only | ||||
| 4 | PD12019 | NE | ||
| 6 | PD12017 | NE | ||
| 9 | PD12021 | Diffuse glycogen vacuolation within hepatocytes (cause unknown). | ||
| 12 | PD12006 | Multifocal moderate lymphoplasmacytic infiltrates were present within the lamina propria and submucosa. This lesion was similar to those seen in dogs and humans as a result of Helicobacter infections of the stomach. This lesion could also represent a residual inflammatory reaction to gastric parasitic (helminth) infections. Submucosal lymphoplasmacytic and histiocytic inflammatory foci in the gastric mucosa. | ||
| 24 | PD12029 | A slight increase in the numbers of lymphocytes and plasma cells within the lamina propria of the duodenum was present. Moreover, the glycogen vacuolation within the liver section from this animal was diffuse and marked. In addition, there was slight growth of yeast (Candida spp.) in the esophageal mucosa. | ||
| 24 | PD12036 | Submucosal lymphoplasmacytic and histiocytic inflammatory foci in the stomach mucosa. Glycogen vacuolation in the liver section was diffuse and moderate. Focal, moderate bronchus- associated lymphoid tissue hyperplasia was seen within the lung. A single submucosal lymphocytic inflammatory focus was seen in the submucosa of the esophagus. | ||
| 24 | PD12057 | Sub-mucosal lymphoplasmacytic and histiocytic inflammatory foci in the stomach mucosa. Animal 12057 had diffuse and moderate glycogen vacuolation of the hepatocytes. Additionally, in the liver, multifocal mild portal infiltrates of lymphoid cells were observed and the Kupffer cells were prominent. | ||
| Buprenorphine only | ||||
| 4 | PD12056 | NE | ||
| 6 | PD12001 | NE | ||
| 9 | PD12072 | In the stomach of this animal, two small lymphoid nodules were observed in the mucosa. Similar to the meloxicam treated-animals, glycogen vacuolation was observed (for this animal it was moderate and mostly periportal to midzonal within the hepatic lobules). In the lungs, occasional small granulomas were seen with histiocytes and neutrophils within). Most likely, these granulomas formed as a reaction to either inhaled foreign bodies or to migrating parasites. Nevertheless, neither foreign bodies nor parasites were found within these granulomas. The esophagus had small bacterial colonies within the cornified layer without an inflammatory reaction. A bilateral impaction of feed material in the root of the molars, with neutrophilic inflammation and bone remodeling unilaterally was seen. | ||
| 12 | PD12045 | The hepatocytes within all zones of the hepatic lobules had mild and diffuse glycogen vacuolation. Multifocal, mild, superficial esophagitis with multifocal erosions were observed. Inflammatory infiltrate consisted of numerous neutrophils, either singly or in small clusters, were present in the superficial layers of the esophageal epithelium. In these areas where neutrophils are the esophageal epithelium is extensively vacuolated and/or focally eroded. Small numbers of bacteria are seen attached to the epithelial surface throughout. | ||
| 24 | PD12055 | Periportal and moderate hepatocytic vacuolation were present. Bacteria were observed on the mucosal surface of the esophagus. | ||
| 24 | PD12071 | Mild, focal periportal mixed (lymphoplasmacytic, histiocytic, and neutrophilic) inflammatory infiltrate as well as focal hepatic necrosis with associated, mostly neutrophilic inflammatory infiltrate were observed. The kidney of this animal had focal mild interstitial nephritis. Bronchus-associated lymphoid tissue was prominent in the lung section. | ||
| 24 | PD12046 | Stomach had a single prominent sub-mucosal lymphoid nodule. Hepatocytic glycogen vacuolation was moderate and diffuse. In the kidney, there was a focus of interstitial nephritis with associated tubular degeneration and regeneration. The esophagus had scattered, small mixed inflammatory infiltrate consisting of lymphoplasmacytes and histiocytes, and similar nodules were seen in the submucosa (probably due to prior trauma). This animal also had unilateral impacted food material within a root of a molar tooth. | ||
| MPXV only | ||||
| 4 | PD12028 | NE | ||
| 6 | PD12058 | NE | ||
| 9 | PD12014 | Lymphoid nodule in the submucosa of the stomach. | ||
| 12 | PD12011 | Lymphoplasmacytic inflammatory infiltrates were seen in the mucosa and submucosa of the stomach. The duodenum had mildly increased numbers of lymphocytes and plasma cells in the lamina propria. Scattered bacterial colonies in the cornified layer of the esophagus (without any inflammatory reaction). There was diffuse and mild hepatocytic glycogen vacuolation throughout the liver. | ||
| 24 | PD12034 | The liver had multifocal lymphoplasmacytic infiltrates in scattered portal triads. The heart had a focal myocardial necrosis and associated mixed (neutrophilic, histiocytic, and lymphocytic) inflammatory infiltrate. The kidney had focal subcapsular mixed inflammatory infiltrate primarily lymphoplasmacytic with lesser number of neutrophils. A focal collection of alveolar macrophages were observed within the lung. There was diffuse and mild hepatocytic glycogen vacuolation throughout the liver. | ||
| MPXV + meloxicam | ||||
| 4 | PD12027 | NE | ||
| 4 | PD12004 | NE | ||
| 4a | PD12112 | NE | ||
| 6 | PD12077 | NE | ||
| 9 | PD12037 | NO | ||
| 9 | PD12038 | NO | ||
| 12b | PD12024 | NO | ||
| 12 | PD12078 | A submucosal lymphoid follicle with focal and mild inflammation in the muscle coat was observed in the stomach; infiltrate was perivascular lymphoplasmacytic and histiocytic. The kidney displayed mild chronic interstitial nephritis (most likely pre-existing ascending inflammation not related to NSAID treatment or viral infection). | ||
| 18a | PD12114 | NO | ||
| 24 | PD12096 | NO | ||
| 24 | PD12059 | NO | ||
| MPXV + buprenorphine | ||||
| 4 | PD12002 | NE | ||
| 4 | PD12064 | NE | ||
| 6 | PD12092 | NE | ||
| 6 | PD12025 | NE | ||
| 9 | PD12115 | NO | ||
| 9 | PD12085 | NO | ||
| 12 | PD12049 | NO | ||
| 12 | PD12119 | The kidney had multifocal, chronic interstitial nephritis with radiating bands of fibrosis (residual scar from prior interstitial nephritis). | ||
| 24 | PD12091 | NO | ||
NE, not examined; NO, no incidental findings observed
Died prematurely
Unsuccessfully infected
The findings above are believed to be incidental and unrelated to either MPXV infection or analgesia.
Compared with other groups, viral DNA was detectable in more tissues at 4 dpi in the MXPV-challenged animals treated with meloxicam (Table 4). In addition on day 4, PD12112 in this group unexpectedly died while under anesthesia and presented with lymphadenopathy, with viable virus detected in the salivary gland and submandibular lymph node. This presentation was earlier than in our MPXV-positive controls and in a previous serial euthanasia study with WA MPXV.11 For other animals, tissues were all positive for virus beginning at 6 or 9 dpi, except for blood (viremia from this group was not evaluated). By day 24, similar to the MPXV control animals, only the nasal cavity was still positive for viable virus, but viral DNA remained in all tissues except the blood. The lowest peak viral load was from the brain (1 × 102 pfu at 18 dpi) of the MPXV– meloxicam animals, and the tongue had the highest viral load in this group of animals (5 × 107 pfu at 12 dpi).
Tissues were all positive for virus beginning at 6, 9, or 12 dpi, except for blood (viremia from this group was not detected) and stomach of MXPV–buprenorphine animals (Table 4). In this group, no viable virus was present in any tissue at 24 dpi, although viral DNA was still detected in several tissues. The tissue with the lowest peak viral load in this group was the skin lesion at 12 dpi (8 × 102 pfu), and the highest peak viral load was seen in the nasal cavity at 12 dpi (2 × 108 pfu).
Pathology findings.
Previously, we described the pathogenesis of MPXV in the prairie dog model13 between 2 and 24 dpi, in which pathologic changes due to viral infection were first observed primarily at 9 dpi. In light of these results, we performed histologic evaluations on animals euthanized between 9 and 24 dpi in the current study to look for pathologic changes after consecutive days of NSAID or opioid treatment. Only animals with pathologic findings (due to intranasal MPXV challenge or analgesic use) are described. Incidental findings (those unassociated with either MPXV infection or analgesic treatment) are listed in Table 5.
Table 5.
Kinetics of MPXV viral spread in prairie dogs challenged with MPXV and treated or not treated with analgesic
| WA MPXV only | WA MPXV + meloxicam | WA MPXV + buprenorphine | |||||||||
| Viral DNA present at dpi | Viable virus present at dpi | Peak viral load (no. of pfu/g; at dpi) | Viral DNA present at dpi | Viable virus present at dpi | Peak viral load (no. of pfu/g; at dpi) | Viral DNA present at dpi | Viable virus present at dpi | Peak viral load value (pfu/g; day) | |||
| Oral swab | 6–17 | 6–17 | 2 × 106; 9 | 4–24 | 6–21 | 5 × 107; 12 | 6–24 | 6–12 | 3 × 105; 12 | ||
| Blood | 4–17 | 9 | 1 × 102; 9 | 6–17/18 | ND | ND | 4–17 | ND | ND | ||
| Nasal cavity | 6–24 | 6–24 | 5 × 107; 9 | 4–24 | 9–24 | 6 × 106; 9 | 6–12 | 6–12 | 2 × 108; 12 | ||
| Salivary gland and | 6–24 | 6–12 | 3 × 107; 9 | 4–24 | 4–18 | 2 × 105; 9 | 4–12 | 6–12 | 1 × 105; 12 | ||
| submandibular lymph node | |||||||||||
| Spleen | 6–24 | 6–12 | 2 × 108; 9 | 4–24 | 6–9 | 9 × 106; 9 | 4–24 | 6–12 | 3 × 105; 6 | ||
| Tongue | 6–24 | 6–12 | 9 × 106; 9 | 6–24 | 6–18 | 5 × 107; 12 | 6–24 | 6–12 | 3 × 106; 12 | ||
| Lung | 4–24 | 6–9 | 5 × 104; 9 | 6–24 | 9–18 | 6 × 105; 9 | 6–12 | 9–12 | 4 × 104; 12 | ||
| Liver | 4–24 | 6–12 | 7 × 106; 9 | 4–24 | 9–12 | 6 × 104; 9 | 4–12 | 12 | 2 × 104; 12 | ||
| Small Intestine | 6–24 | 6–12 | 2 × 104; 9 | 4–24 | 9–18 | 5 × 105; 12 | 6–12 | 6–9 | 7 × 105; 9 | ||
| Mesenteric lymph node | 6–24 | 6–12 | 3 × 106; 9 | 4–24 | 6–12 | 7 × 103; 9 | 4–12 | 6–12 | 5 × 104; 6 | ||
| Belly skin or lesion | 9–24 | 12 | 1 × 106; 12 | 6–24 | 9–18 | 2 × 107; 18 | 12–24 | 12 | 8 × 102; 12 | ||
| Stomach | 4–24 | 9–12 | 5 × 103; 9 | 4–24 | 9–18 | 2 × 105; 9 | 4–24 | ND | ND | ||
| Brain | 6–24 | 9 | 2 × 102; 9 | 9–24 | 9–18 | 1 × 102; 18 | 6–12 | 12 | 7 × 103; 12 | ||
ND, no positive samples detected
Detection of MPXV DNA and viable viral particles is shown as the range of days after infection on which PCR tests and viral culture assays, respectively, were positive. The day on which peak viral load was detected is shown after the titer.
Meloxicam-treated, uninfected controls.
PD12006 had an injection-site reaction due to daily subcutaneous administration of meloxicam. The epidermis had a locally extensive subcorneal pustule, and the dermis contained a perivascular to interstitial, mostly neutrophilic inflammatory infiltrate. Degeneration, necrosis, mild neutrophilic and histiocytic inflammation and regeneration were present in the underlying cutaneous muscle. The surrounding soft tissues were normal. In addition, 2 of the 3 animals euthanized after 24 d of meloxicam treatment (PD12036 and PD12057) had similar injection site abscesses.
Buprenorphine-treated, uninfected controls.
Buprenorphine control animals had various, minimal, and nonsignificant histologic lesions. None of these lesions were compatible with or attributable to the treatment with buprenorphine.
MPXV-challenged control animals.
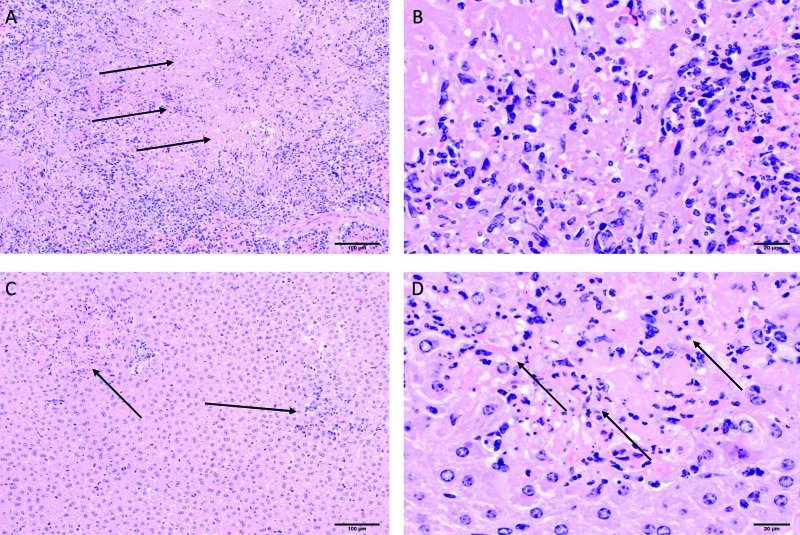
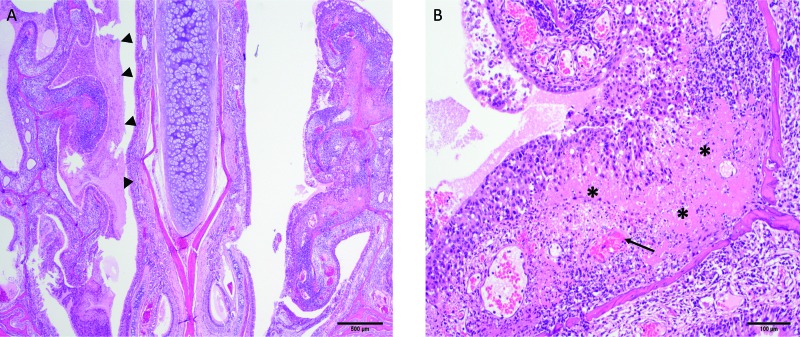
The MPXV-challenged animal that was euthanized at 9 dpi (PD12014) exhibited histologic lesions attributable to MPXV infection. Unilateral moderate neutrophilic rhinitis was observed in this animal. In addition, the submandibular lymph nodes had multifocal necrosis as did the spleen, which had multifocal, widespread necrosis both in the white and red pulp (affecting primarily red pulp; Figure 1 A and B). The liver had minimal, multifocal hepatic necrosis with associated, mostly neutrophilic inflammatory infiltrate (Figure 1 C and D). In addition, PD12011 was euthanized at 12 dpi and had several histologic lesions, including bilateral, severe, necrotizing to purulent rhinitis, and osteolysis in the nasal turbinates. In addition, there was necrosis of the nasal-associated lymphoid tissue and adjacent soft tissues (Figure 2 A and B). The submandibular lymph node and mesenteric lymph node displayed prominent germinal centers in the lymphoid follicles. In the liver, infrequent, small neutrophilic inflammatory foci were observed, and the Kupffer and endothelial cells were prominent. The trachea had focal, mild infiltrate (lymphocytes, plasma cells, and lesser numbers of histiocytes) in the submucosa. PD12034 was euthanized at 24 dpi and had minimal histologic lesions, comprising residual mild, diffuse lymphoplasmacytic bilateral rhinitis with mucosal and necrosis of nasal-associated lymphoid tissue.
Figure 1.
Representative histopathologic images of a prairie dog (PD12014) challenged with MPXV. (A and B) Spleen had multifocal, widespread necrosis (arrows). (C and D) Minimal, multifocal hepatic necrosis is evident. Hematoxylin and eosin stain; magnification: 10× (A and C), 40× (B and D).
Figure 2.
Representative images of a prairie dog (PD12011) challenged with MPXV. (A) Necrotic debris (arrowheads) covers the nasal mucosa. Magnification, 2×. (B) Nasal cavity also shows widespread necrosis (asterisks) and vasculitis (arrow). Magnification, 10×. Hematoxylin and eosin stain.
Meloxicam-treated, MPXV-challenged animals.
Animals challenged with MPXV and treated with meloxicam for 9 d before euthanasia (PD12037 and PD12038) exhibited histologic lesions characteristic of poxviral infection, similar to those seen in the MPXV-positive control animal. PD12037 had neutrophilia in the capillaries within the nasal mucosa, with neutrophils traversing the nasal mucosa. In addition, PD12038 had several lesions characteristic of MPXV infection, primarily bilateral neutrophilic and necrotizing rhinitis as well as necrosis of nasal-associated lymphoid tissue. Histologic lesions for PD12078, euthanized at 12 dpi included bilateral neutrophilic rhinitis with necrosis of the nasal-associated lymphoid tissue. The mesenteric lymph node displayed lymphadenitis characterized by infiltration with macrophages and some neutrophils. Multiple minute foci of hepatic necrosis with associated inflammatory infiltrates (mostly neutrophils) were observed in the liver, as were prominent and hypertrophied Kupffer and endothelial cells. PD12114 was euthanized at 18 dpi due to meeting morbidity endpoint criteria. Examination of the submandibular lymph node revealed acute multifocal necrosis. The liver displayed prominent Kupffer cells throughout. Sinusoids had moderately increased numbers of neutrophils (sinus neutrophilia). The skin from the injection site of this animal had necrotizing myositis and cellulitis (reaction to injection). Two animals (PD12096 and PD12059) were challenged with MPXV, treated with meloxicam for 21 d, and euthanized at 24 dpi; PD12096 had minimal histologic lesions, whereas PD2059 had necrotizing and neutrophilic rhinitis. The mesenteric lymph node had focal, mild necrotizing lymphadenitis.
Buprenorphine-treated MPXV-challenged animals.
Two animals (PD12115 and PD12085) that were challenged with MPXV and treated with the opioid buprenorphine were euthanized at 9 dpi; PD12115 had histologic lesions characteristic of poxviral infection, including minimal multifocal neutrophilic infiltrate observed in the nasal cavity. Animals (PD12049 and PD12119) were challenged with MPXV and treated with buprenorphine for 12 d before euthanasia. PD12049 had bilateral moderate purulent rhinitis, with osteolysis and necrosis of nasal-associated lymphoid tissue. Multiple minute foci of hepatocellular necrosis were observed in the liver, as well as moderately prominent Kupffer and endothelial cells. In addition, the skin of this animal had a focal subcorneal neutrophilic pox pustule that extended into the superficial dermis. PD12119 had severe bilateral neutrophilic and necrotizing rhinitis, necrosis of the nasal-associated lymphoid tissue with intralesional bacterial cocci, and unilateral dental pulp necrosis. The submandibular lymph node had necrosis with scattered Langhans-type giant cells. In the liver, Kupffer's cells were prominent, and moderate sinusoidal neutrophilia was. The animal euthanized at day 24 in this group (PD12091) had minimal histologic lesions.
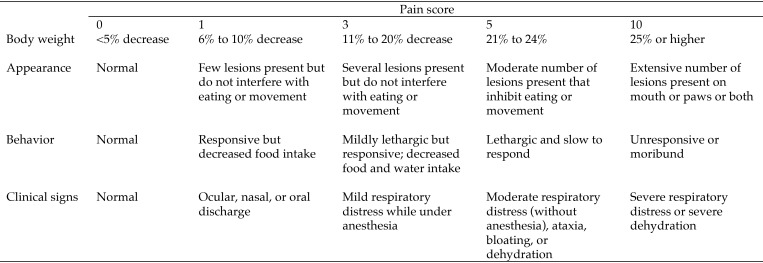
Amendment of pain score for prairie dog MPXV challenge studies.
During previous MPXV challenge studies using this nonstandard laboratory model, we sought to develop a pain scale specific for the disease progression in prairie dogs. Given the findings from this animal study, in which the use of buprenorphine did not increase any clinical or molecular signs in animals challenged with MPXV, we were able to refine the pain scale and incorporate buprenorphine for the alleviation of pain (Figure 3). This new pain scale, which increases animal welfare through the use of analgesic during MPXV challenge studies, is now incorporated in all prairie dog studies within our branch.
Figure 3.
Scale developed to assess pain in prairie dogs infected with MPXV, including incorporation of buprenorphine for alleviation of pain. During pain assessment, a score is given for each category; these scores are summed for determination of pain. Each pain scale has a corresponding action plan; italics indicate modifications reflecting the results of the current study. Specifically, for a total score of 1 to 3 or a score of <1 in a category, offer additional approved palatable treats to encourage eating. For a total score of 4 to 6, perform a complete physical assessment (including anesthetization for determination of weight) at least every 48 to 72 hours, offer additional approved palatable treats to encourage eating, administer subcutaneous or oral fluids when dehydration is observed, and administer buprenorphine as instructed by attending veterinarian or primary investigator in light of clinical signs (for a total time of no more than 7 study days). For a total score of 7 to 9, increase the frequency of observation to at least twice daily, with one of these observations a complete physical assessment, (including anesthetization for determination of weight), notify the attending veterinarian, administer buprenorphine as instructed by attending veterinarian or primary investigator in light of clinical signs (for a total time of no more than 7 study days), offer additional approved palatable treats to encourage eating, and administer subcutaneous or oral fluids when dehydration is observed or consider euthanasia. When the total score is 10 or greater, euthanize animal.
Discussion
Overall prairie dogs tolerated both buprenorphine and meloxicam for this extended period very well, providing valuable information that both analgesics can be safely used within this nonstandard laboratory animal species during routine laboratory husbandry. Respiratory depression has been associated with the use of opioids20 and gastritis with NSAID; on the basis of animal observation, weight monitoring, and necropsy observations, neither of these side effects occurred in treated prairie dogs. With the exception of lesions on the dorsum due to meloxicam injections, no other adverse clinical signs were observed in either meloxicam- or buprenorphine-treated, uninfected control animals. Histologic evaluation of meloxicam controls revealed various incidental findings. One animal in the meloxicam control group that was euthanized on day 24 had an enlarged liver, and on histologic evaluation, multifocal mild portal infiltrates of lymphoid cells were observed in the liver as were prominent Kupffer cells. Prominent Kupffer cells has been attributed to NSAID toxicity in rats.1 Similarly, the buprenorphine-treated controls had numerous incidental findings. Of note, 2 of the buprenorphine treatment animals euthanized at 24 dpi had mild interstitial nephritis; in addition, one of these had tubular degeneration and regeneration. Liver and kidney toxicity due to the use of morphine and tramadol (opioids) has been seen.3 However, buprenorphine is primarily excreted through the liver, and therefore kidney toxicity is not a known side effect during treatment; consequently, these findings were likely incidental and specific to these 2 animals. Because these are outbred animals, observing some abnormalities during histologic examination is not unexpected.
MPXV-challenged control animals had a typical disease progression associated with a low-dose challenge of WA MPXV as we have previously described.12 Although clinical signs and cutaneous MPXV lesions were minimal, the tissue tropism of the virus was extensive, with viable virus detected in all tested tissues and viral loads reaching as high as 2 × 108 pfu per gram of tissue. The MPXV-challenged, meloxicam-treated animals had a similar disease progression as MPXV control animals; however we noted subtle increases in disease severity. For example, within the MPXV-challenged, meloxicam-treated group, there were 2 unexpected deaths; the animal that died at 4 dpi had viable virus and lymphadenopathy at time of death. On the basis of our previous studies in this animal model, we would not expect these findings until 6 to 9 dpi.13 The other unexpected death in the MPXV–meloxicam group was an animal that had to be euthanized at 18 dpi due to weight loss and pronounced morbidity. In addition, some animals in this group showed more severe clinical signs (gastrointestinal bloat, bloody nose, dehydration, and lethargy), resulting in the highest clinical score average, compared with the MPXV controls.
Those animals challenged with MXPV and treated with buprenorphine for the course of the study had a similar disease progression as MPXV-challenged control animals. In the MPXV–buprenorphine animals, no clinical signs were observed until 12 dpi, only 2 animals developed cutaneous MPXV lesions, and lesion number was minimal on those 2 animals. There were no unexpected deaths in the MPXV–buprenorphine group, and the tissue tropism and peak viral load (Table 4) were similar to those in MXPV control animals. The variability seen in the quantity of virus per gram of tissues between animals and groups is very similar to a previous MPXV challenge study with prairie dogs.13 Histologic examination of animals in the 3 MPXV-challenged groups revealed pathologic lesions attributable to viral infection. However, there was no indication that treatment with either meloxicam or buprenorphine exacerbated the virus-attributed lesions. In addition, when we compared antibody response, ELISA and neutralization results were similar between the 3 groups of animals at both 12 and 17 dpi, suggesting that the use of either analgesic did not have an effect on the immune response.
The study had several limitations, primarily that the numbers in each study group were low. Because prairie dogs are relatively large laboratory animals that have to be caged individually and because we are limited by the amount of cage space available within our BSL3 animal laboratories, we are restricted to using smaller groups of animals. In addition, we limit the number of animals to more safely execute these BSL3 studies. Furthermore, we had 3 animals that were challenged unsuccessfully, thereby further decreasing our animal numbers (Figure 1d/1e). There are several possible explanations for why these animals were not infected after experimental inoculation. Although the animals are completely anesthetized during inoculation, it is possible that the virus was not efficiently delivered during intranasal challenge. We have previously seen a steep-dose response in this animal model, in which 6 × 103 pfu of each MPXV clade resulted in overt MPXV disease in all 4 animals.12 However, in the same study, a dose of 6 × 102 pfu (approximately 1 log lower) resulted in only one of the 4 challenged animals becoming infected. If the intended inoculation was efficiently given, another possibility is that this animal's innate immune system was able to effectively clear the virus before the adaptive immune system became involved, as differences in disease response and progression can occur in wild, outbred animals. Another study limitation to consider is that we used only the WA MPXV clade. A worthwhile future study would be to use the Congo Basin (CB) MPXV clade, which may have some differences in the manner in which it circumvents the host's immune response as compared with WA MPXV. Although we did not use nociception tests to assess pain relief, both analgesics have been well characterized as providing pain relief within multiple animal species.4,8,22,28,29 However, conflicting results for pain relief attributed to meloxicam have been reported,4,25 thereby giving more support for the use of buprenorphine in prairie dogs.
In the current study, we used a low-dose challenge of WA MPXV and treated groups of animals with either meloxicam or buprenorphine. If either of these analgesics caused an increase in viral pathogenesis, we expected to see stark differences in our MPXV-challenged, analgesic-treated animals compared with the MPXV-positive untreated animals (that is, earlier and increased cutaneous lesion development; increased morbidity and mortality; and increased viral loads within tissues). Objective measures of disease progression (that is viral load and tissues infected) were similar despite analgesic treatment or lack thereof. Although these objective signs were similar between the groups, there was an increasing trend of morbidity and mortality in the MXPV-infected, meloxicam-treated animals. Given these observations, as well as the development of a dorsal abscess in the meloxicam-treated animals and potential blood chemistry changes at 24 dpi in both challenge groups (decreased albumin and increased BUN in meloxicam treated and increased ALT values in the buprenorphine treated animals (compared with PBS controls)), we do not be recommend administering either of these analgesics (especially at the high dose used) for an extended period during a viral infection, as done in the current study (18 d for meloxicam and 20 d for buprenorphine). Evidence disfavoring the use of meloxicam during MPXV infection was stronger (particularly given that 2 animals in this group died during the study) than for buprenorphine. After we completed this study, a report describing the pharmacokinetics of meloxicam in black-tailed prairie dogs was published, and results suggested that a 1.0-mg/kg subcutaneous dose of meloxicam administered every 24 h might be excessive, in light of high absorption in and slow elimination from plasma.30 Because we lacked this information at the inception of our study, we based the dosing (4 mg/kg) on meloxicam use in mice (typically administered at 1 to 5 mg/kg).16 If a lower dosage of meloxicam had been used, we may not have seen the injection site reactions that occurred in 4 of the 18 animals or some of the differences in pathogenicity mentioned earlier.
The differences that we observed when comparing buprenorphine-treated MPXV-infected animals with MPXV controls were so subtle that use of buprenorphine should be considered when clinical scores indicate pain during future MPXV challenge studies involving prairie dogs. Further evidence to support use of this analgesic is given in other studies with rats, which demonstrated that buprenorphine treatment does not result in immunosuppressive activity compared with other opiods.27 A recent study looking at the pharmacokinetic profiles of meloxicam and sustained-release buprenorphine within prairie dogs suggest that sustained-release buprenorphine maintained likely therapeutic plasma levels (0.001 μg/mL) beyond 72 h.5 The benefits of using this sustained-release analgesic include decreasing the stress of the animals while on protocol (less handling, because pain is alleviated for as long as 72 h) as well as increasing the safety of personnel (again, less handling of infected animals). Therefore, we conclude that the use of buprenorphine for short-term pain relief (that is, less than 7 d) would likely result in few or no differences in pathogenicity. In light of these results we have modified our pain scale for prairie dog MPXV studies to include the use of buprenorphine (Figure 3), thereby greatly improving animal welfare during future challenge studies.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. The authors declare no competing financial interests. We thank Ashley Kondas for reviewing the manuscript.
References
- 1.Abatan MO, Lateef I, Taiwo VO. 2006. Toxic effects of nonsteroidal antiinflammatory agents in rats. Afr J Biomed Res 9:219–223. [Google Scholar]
- 2.Adler MW, Geller EB, Rosow CE, Cochin J.1988. The opioid system and temperature regulation. 10.1146/annurev.pa.28.040188.002241 [DOI] [PubMed] [Google Scholar]
- 3.Atici S, Cinel I, Cinel L, Doruk N, Eskandari G, Oral U. 2005. Liver and kidney toxicity in chronic use of opioids: an experimental long-term treatment model. J Biosci 30:245–252. 10.1007/BF02703705 [DOI] [PubMed] [Google Scholar]
- 4.Bianchi M, Panerai AE. 2002. Effects of lornoxicam, piroxicam, and meloxicam in a model of thermal hindpaw hyperalgesia induced by formalin injection in rat tail. Pharmacol Res 45:101–105. 10.1006/phrs.2001.0921. [DOI] [PubMed] [Google Scholar]
- 5.Cary CD, Lukovsky-Akhsanov NL, Gallardo-Romero NF, Tansey CM, Ostergaard SD, Taylor WD, Jr, Morgan CN, Powell N, Lathrop GW, Hutson CL. 2017. Pharmacokinetic profiles of meloxicam and sustained-release buprenorphine in prairie dogs (Cynomys ludovicianus). J Am Assoc Lab Anim Sci 56:160–165. [PMC free article] [PubMed] [Google Scholar]
- 6.Chang Y, Moody DE. 2009. Glucuronidation of buprenorphine and norbuprenorphine by human liver microsomes and UDP-glucuronosyltransferases. Drug Metab Lett 3:101–107. 10.2174/187231209788654117. [DOI] [PubMed] [Google Scholar]
- 7.D'Acquisto F, May MJ, Ghosh S. 2002. Inhibition of nuclear factor κB (NFκB): an emerging theme in antiinflammatory therapies. Mol Interv 2:22–35. 10.1124/mi.2.1.22. [DOI] [PubMed] [Google Scholar]
- 8.Foley PL, Liang H, Crichlow AR. 2011. Evaluation of a sustained-release formulation of buprenorphine for analgesia in rats. J Am Assoc Lab Anim Sci 50:198–204. [PMC free article] [PubMed] [Google Scholar]
- 9.Huhn GD, Bauer AM, Yorita K, Graham MB, Sejvar J, Likos A, Damon IK, Reynolds MG, Kuehnert MJ. 2005. Clinical characteristics of human monkeypox and risk factors for severe disease. Clin Infect Dis 41:1742–1751. 10.1086/498115. [DOI] [PubMed] [Google Scholar]
- 10.Hutson CL, Lee KN, Abel J, Carroll DS, Montgomery JM, Olson VA, Li Y, Davidson W, Hughes C, Dillon M, Spurlock P, Kazmierczak JJ, Austin C, Miser L, Sorhage FE, Howell J, Davis JP, Reynolds MG, Braden Z, Karem KL, Damon IK, Regnery RL. 2007. Monkeypox zoonotic associations: insights from laboratory evaluation of animals associated with the multistate US outbreak. Am J Trop Med Hyg 76:757–768. 10.4269/ajtmh.2007.76.757. [DOI] [PubMed] [Google Scholar]
- 11.Hutson CL, Olson VA, Carroll DS, Abel JA, Hughes CM, Braden ZH, Weiss S, Self J, Osorio JE, Hudson PN, Dillon M, Karem KL, Damon IK, Regnery RL. 2009. A prairie dog animal model of systemic orthopoxvirus disease using West African and Congo Basin strains of monkeypox virus. J Gen Virol 90:323–333. 10.1099/vir.0.005108-0. [DOI] [PubMed] [Google Scholar]
- 12.Hutson CL, Carroll DS, Self J, Weiss S, Hughes CM, Braden Z, Olson VA, Smith SK, Karem KL, Regnery RL, Damon IK. 2010. Dosage comparison of Congo Basin and West African strains of monkeypox virus using a prairie dog animal model of systemic orthopoxvirus disease. Virology 402:72–82. 10.1016/j.virol.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hutson CL, Carroll DS, Gallardo-Romero N, Drew C, Zaki SR, Nagy T, Hughes C, Olson VA, Sanders J, Patel N, Smith SK, Keckler MS, Karem K, Damon IK. 2015. Comparison of monkeypox virus clade kinetics and pathology within the prairie dog animal model using a serial sacrifice study design. BioMed Res Int 2015:1.–. 10.1155/2015/965710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karem KL, Reynolds M, Braden Z, Lou G, Bernard N, Patton J, Damon IK. 2005. Characterization of acute-phase humoral immunity to monkeypox: use of immunoglobulin M enzyme-linked immunosorbent assay for detection of monkeypox infection during the 2003 North American outbreak. Clin Diagn Lab Immunol 12:867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keckler MS, Carroll DS, Gallardo-Romero NF, Lash RR, Salzer JS, Weiss SL, Patel N, Clemmons CJ, Smith SK, Hutson CL, Karem KL, Damon IK. 2011. Establishment of the black-tailed prairie dog (Cynomys ludovicianus) as a novel animal model for comparing smallpox vaccines administered preexposure in both high–and low-dose monkeypox virus challenges. J Virol 85:7683–7698. 10.1128/JVI.02174-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kendall LV, Hansen RJ, Dorsey K, Kang S, Lunghofer PJ, Gustafson DL. 2014. Pharmacokinetics of sustained-release analgesics in mice. J Am Assoc Lab Anim Sci 53:478–484. [PMC free article] [PubMed] [Google Scholar]
- 17.Kopp E, Ghosh S. 1994. Inhibition of NFκB by sodium salicylate and aspirin. Science 265:956–959. 10.1126/science.8052854. [DOI] [PubMed] [Google Scholar]
- 18.Li Y, Olson VA, Laue T, Laker MT, Damon IK. 2006. Detection of monkeypox virus with real-time PCR assays. J Clin Virol 36:194–203. 10.1016/j.jcv.2006.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Likos AM, Sammons SA, Olson VA, Frace AM, Li Y, Olsen-Rasmussen M, Davidson W, Galloway R, Khristova ML, Reynolds MG, Zhao H, Carroll DS, Curns A, Formenty P, Esposito JJ, Regnery RL, Damon IK. 2005. A tale of 2 clades: monkeypox viruses. J Gen Virol 86:2661–2672. 10.1099/vir.0.81215-0. [DOI] [PubMed] [Google Scholar]
- 20.Montandon G, Ren J, Victoria NC, Liu H, Wickman K, Greer JJ, Horner RL. 2016. G-protein–gated inwardly rectifying potassium channels modulate respiratory depression by opioids. Anesthesiology 124:641–650. 10.1097/ALN.0000000000000984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moss B, Shisler JL. 2001. Immunology 101 at poxvirus U: immune evasion genes. Semin Immunol 13:59–66. 10.1006/smim.2000.0296 [DOI] [PubMed] [Google Scholar]
- 22.Pieper K, Schuster T, Levionnois O, Matis U, Bergadano A. 2011. Antinociceptive efficacy and plasma concentrations of transdermal buprenorphine in dogs. Vet J 187:335–341. 10.1016/j.tvjl.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 23.Reed KD, Melski JW, Graham MB, Regnery RL, Sotir MJ, Wegner MV, Kazmierczak JJ, Stratman EJ, Li Y, Fairley JA, Swain GR, Olson VA, Sargent EK, Kehl SC, Frace MA, Kline R, Foldy SL, Davis JP, Damon IK. 2004. The detection of monkeypox in humans in the western hemisphere. N Engl J Med 350:342–350. 10.1056/NEJMoa032299. [DOI] [PubMed] [Google Scholar]
- 24.Rimoin AW, Kisalu N, Kebela-Ilunga B, Mukaba T, Wright LL, Formenty P, Wolfe ND, Shongo RL, Tshioko F, Okitolonda E, Muyembe JJ, Ryder RW, Meyer H. 2007. Endemic human monkeypox, Democratic Republic of Congo, 2001 to 2004. Emerg Infect Dis 13:934–937. 10.3201/eid1306.061540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santos AR, Vedana EM, De Freitas GA. 1998. Antinociceptive effect of meloxicam, in. neurogenic and inflammatory nociceptive models in mice. Inflamm Res 47:302–307. 10.1007/s000110050333. [DOI] [PubMed] [Google Scholar]
- 26.Seet BT, Johnston JB, Brunetti CR, Barrett JW, Everett H, Cameron C, Sypula J, Nazarian SH, Lucas A, McFadden G. 2003. Poxviruses and immune evasion.Annu Rev Immunol 21:377–423.doi: 10.1146/annurev.immunol.21.120601.141049 [DOI] [PubMed] [Google Scholar]
- 27.Sacerdote P. 2006. Opioids and the immune system. Palliat Med 20 Suppl 1:s9–s15. [PubMed] [Google Scholar]
- 28.Waite ME, Tomkovich A, Quinn TL, Schumann AP, Dewberry LS, Totsch SK, Sorge RE. 2015. Efficacy of common analgesics for postsurgical pain in rats. J Am Assoc Lab Anim Sci 54:420–425. [PMC free article] [PubMed] [Google Scholar]
- 29.Wen ZH, Tang CC, Chang YC, Huang SY, Chen CH, Wu SC, Hsieh SP, Hsieh CS, Wang KY, Lin SY, Lee HL, Lee CH, Kuo HC, Chen WF, Jean YH. 2013 Intraarticular injection. of the selective cyclooxygenase-2 inhibitor meloxicam (Mobic) reduces. experimental osteoarthritis and nociception in rats. Osteoarthritis Cartilage 21:1976–1986. 10.1016/j.joca.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 30.Wright TL, Eshar D, McCullough C, Warner M, Kukanich B. 2017. Pharmacokinetics of. single-dose subcutaneous meloxicam injections in black-tailed prairie dogs. (Cynomys ludovicianus). J Am Assoc Lab Anim Sci 56:539–543. [PMC free article] [PubMed] [Google Scholar]