Abstract
Background:
Little is known about the natural history of a surgically treated symptomatic lateral discoid meniscus. The goals of this study were to describe the rate and factors associated with recurrent lateral meniscal tears and progression to symptomatic lateral compartment osteoarthritis (OA) in patients surgically treated for a symptomatic lateral discoid meniscus.
Hypothesis:
Patients with surgically treated lateral discoid meniscus have a high incidence of meniscal retear and progression to lateral compartment OA.
Study Design:
Case series; Level of evidence, 4.
Methods:
A large geographic database was reviewed to identify and confirm patients presenting with symptomatic lateral discoid meniscus between 1998 and 2015. Charts were reviewed to document treatment and outcomes at a minimum clinical follow-up of 2 years.
Results:
A total of 59 patients (27 females, 32 males) with a mean age of 25.7 years (range, 4.0-66.0 years) underwent surgical management of a discoid lateral meniscus and were evaluated for a mean of 5.6 years (range, 2.0-23.7 years). Of these, 48 (82%) patients underwent partial lateral meniscectomy, with 24 patients undergoing concurrent saucerization. Eleven (18%) underwent meniscal repair. Tear-free survival following surgery was 41% at 8 years. Progression to symptomatic lateral compartment OA was 50% at 8 years. Young age (hazard ratio, 0.96; 95% CI, 0.93-0.99; P = .01) and open growth plates (hazard ratio, 3.19; 95% CI, 1.15-8.88; P = .03) were associated with increased incidence of postoperative retear. Older age at diagnosis and body mass index ≥30 kg/m2 were associated with increased risk of progression to lateral compartment OA on final radiographs.
Conclusion:
Patients with a surgically treated lateral discoid meniscal tear had a high rate of recurrent meniscal tear (59% at 8 years). Approximately 50% of surgically treated patients developed symptomatic lateral compartment OA at 8 years from diagnosis.
Keywords: lateral discoid meniscus, surgical treatment, meniscal retear, osteoarthritis
Discoid meniscus is a hypertrophic discoid-shaped meniscus that can lead to pain, effusions, and mechanical symptoms often referred to as “snapping knee syndrome.”9,10,12,13,16 A recent series of patients with symptomatic lateral discoid meniscus reported a high rate of associated meniscal tears (72%) and surgical treatment (86%).19 These observations are consistent with prior reports noting a significantly higher rate of meniscal tears in this patient population.11,18
There is a general consensus on surgical management for symptomatic lateral discoid meniscus or unstable lateral discoid meniscal tears to relieve symptoms and possibly prevent early lateral compartment wear.8,10,26 This is especially important considering that the incidence of symptomatic lateral discoid meniscus has been noted to be highest among young, active adolescents.19 For this reason, most authors favor meniscal preservation with repair or partial meniscectomy over total meniscectomy.10,12,23,26 Yet, little is understood about outcomes of discoid meniscal lesions, and choice of treatment remains highly debated.
Recent studies have shown that, aside from its abnormal morphology and/or absent peripheral attachments, a discoid meniscus contains a decreased number and more heterogeneous arrangement of collagen fibers as compared with a normal meniscus.1,7 This abnormal composition of discoid meniscal tissue is theorized to result in poor vascularity and altered stability that may further contribute to tear vulnerability and poor healing potential. These factors raise concern about an increased retear rate in this cohort following surgical treatment.21
The purpose of this study was to (1) describe the rate and factors associated with recurrent lateral discoid meniscal tears after surgical treatment and (2) evaluate the rate of progression and factors associated with symptomatic lateral compartment osteoarthritis (OA) in patients with surgically treated lateral discoid meniscus at a minimum clinical follow-up of 2 years.
Methods
We conducted a search of all cases of symptomatic lateral discoid meniscus in Olmsted County, Minnesota, between January 1, 1998, and June 30, 2015. Patients were identified through the Rochester Epidemiology Project, a database compiling complete medical records for all residents of Olmsted County. This database has been described in detail and allows for the capture of all medical records and procedures for patients within this geographically defined community.17,24 We identified patients using the International Classification of Diseases, Ninth Revision, diagnosis code for lateral discoid meniscus (717.5). Individual chart review of medical records was performed to confirm discoid meniscus diagnosis and gather relevant data related to the initial symptoms/injury, treatment, and outcomes. This study was approved by the institutional review board at the supporting institution.
Inclusion criteria consisted of (1) patients 4 years of age and older who were surgically treated for a symptomatic lateral discoid meniscus and (2) a 2-year minimum clinical follow-up. Patients were considered to have a symptomatic lateral discoid meniscus if they reported knee pain or mechanical symptoms (painful popping, snapping, or decreased knee extension) or had a meniscal injury in the setting of a lateral discoid meniscus detected on magnetic resonance imaging (MRI) or at the time of diagnostic arthroscopy. A diagnosis of lateral discoid meniscus was made if the MRI showed continuity between the anterior and posterior horns of the lateral meniscus in ≥3 consecutive slices in the sagittal plane and/or if the ratio of the minimal meniscal width to maximal tibial width was >20% in the coronal plane.20,26 A diagnosis of lateral discoid meniscus was made during diagnostic arthroscopy if the meniscus exhibited a hypertrophic semilunar or discoid shape partially covering (Watanabe type I) or completely covering (Watanabe type II) the lateral tibial plateau and/or if there was presence of a hypermobile meniscus resulting from deficient posterior tibial attachments (Watanabe type III or Wrisberg variant).25 Systematic probing of the discoid meniscus was employed to assess for peripheral instability. Evidence of hypermobility or peripheral detachment and its location were documented. Surgically treated patients were evaluated by either a pediatric or an adult board-certified orthopaedic surgeon.
All patients had pre- and postoperative routine weightbearing anteroposterior, lateral, and patellar radiographs. Rosenberg and hip-to-ankle views were obtained at the discretion of the treating orthopaedic surgeon. All patients were seen for routine postoperative follow-up. Length of postoperative follow-up was established at the discretion of the treating surgeon. Final follow-up was considered to be the last evaluation by a board-certified orthopaedic surgeon. Exclusion criteria consisted of (1) patients initially thought to have a lateral discoid meniscus on MRI but later found to have normal meniscus at the time of diagnostic arthroscopy and (2) patients with a symptomatic lateral discoid meniscus treated nonoperatively.
Included patients were then divided according to the type of surgical intervention: partial meniscectomy (including saucerization) or meniscal repair (including saucerization). Removal of intact meniscal tissue for the sole purpose of reshaping was classified as saucerization. Debridement of an unstable portion of the meniscus with or without shaping of the remaining meniscus (saucerization) was classified as partial meniscectomy. Patients sustaining a recurrent meniscal tear following surgical intervention were identified if a new meniscal tear was diagnosed on repeat MRI postoperatively or at the time of subsequent diagnostic arthroscopy. Progression to lateral compartment OA was assessed, defined as symptomatic knee pain and a Kellgren-Lawrence grade of ≥2 on final postoperative radiographs as compared with preoperative films.
Statistical Analysis
Descriptive statistics were used to present demographic data with means, standard deviations, and percentages, as appropriate for categorical variables. The Fisher exact test was used for comparing proportions, while Mann-Whitney U testing was used for nominal values, such as age, to provide robust nonparametric testing. Kaplan-Meier models were used to assess the incidence of retear after operative management, all-cause reoperation, and progression to lateral compartment OA. Cox proportional hazards regression was performed to determine risk factors for symptomatic knee pain at the time of final follow-up. P values <.05 were considered significant. Analyses were conducted in R (v 3.4.1; R Core Team).
Results
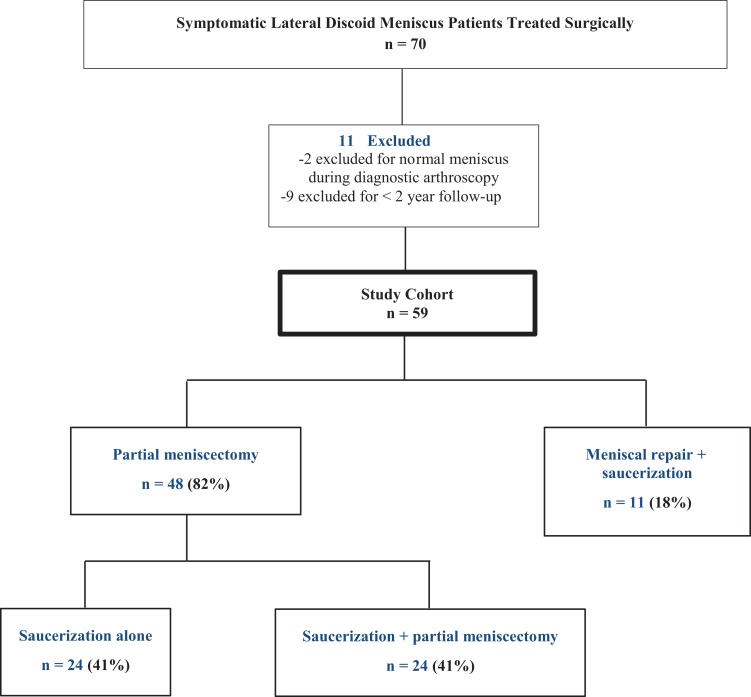
We identified 70 patients surgically treated for a symptomatic lateral discoid meniscus diagnosed on MRI or at the time of diagnostic arthroscopy. Of these, 59 patients met inclusion criteria, with 9 patients excluded for less than 2 years of follow-up and 2 patients excluded after diagnostic arthroscopy failed to demonstrate a discoid meniscus initially diagnosed on MRI. Patients had a mean age of 25.7 years (median, 17; interquartile range, 15-36; range, 4-66 years), with a unimodal age distribution skewed toward younger patients. Patients were evaluated for a mean of 5.6 years (range, 2.0-23.7 years). There were 27 females (46%) and 32 males (54%). Seven patients (12%) had bilateral symptomatic discoid menisci (Table 1). Treated patients were either first evaluated at a tertiary sports specialty center or seen elsewhere and referred to a single tertiary sports specialty center for definitive treatment. Pediatric patients (age ≤16 years) were primarily treated by a pediatric orthopaedic surgeon, and adult patients (age ≥17 years) were primarily treated by an adult sports surgeon. None of the included patients had undergone prior surgical treatment in the affected knee.
TABLE 1.
Study Demographics for the Patients With Discoid Meniscus (N = 59)
| Demographic | Mean ± SD or n (%) |
|---|---|
| Age at diagnosis, y | 25.7 ± 16.4 |
| Physeal status | |
| Closed | 43 (73) |
| Open | 16 (17) |
| Sex | |
| Male | 32 (54) |
| Female | 27 (46) |
| Laterality | |
| Right | 25 (42) |
| Left | 27 (46) |
| Bilateral | 7 (12) |
| Body mass index, kg/m2 | 28.0 ± 6.1 |
| Smoking status | |
| Nonsmoker | 34 (58) |
| Previous smoker | 14 (24) |
| Current smoker | 11 (18) |
| Surgical treatment | |
| Direct repair | 11 (18) |
| Saucerization + partial meniscectomy | 24 (41) |
| Saucerization alone | 24 (41) |
Of the 59 patients included, 50 (85%) had an associated lateral meniscal tear at presentation confirmed with MRI or at the time of diagnostic arthroscopy. Forty-eight (82%) patients underwent partial lateral meniscectomy, with 24 (41%) undergoing concurrent saucerization. An additional 11 patients (18%) underwent meniscal repair and saucerization (Figure 1).
Figure 1.
Flowchart of the study cohort and distribution of patients according to the type of procedure.
Intraoperatively, 15 (25%) patients had an incomplete discoid (type I); 38 (65%) had a complete discoid (type II); and 6 (10%) demonstrated posterior rim hypermobility owing to deficient posterior attachments (type III) (Table 2). Of the 59 patients, 12 (20%) were observed to have peripheral instability, of which 6 (50%) had posterior third instability, 4 (33%) had anterior third instability, and 2 (17%) had middle third instability (Table 2).
TABLE 2.
Morphologic Characteristics of Discoid Lateral Meniscus (N = 59)
| Characteristic | n (%) |
|---|---|
| Discoid type | |
| Type I | 15 (25) |
| Type II | 38 (65) |
| Type III | 6 (10) |
| Peripheral instability | |
| Anterior | 4 (33) |
| Middle | 2 (17) |
| Posterior | 6 (50) |
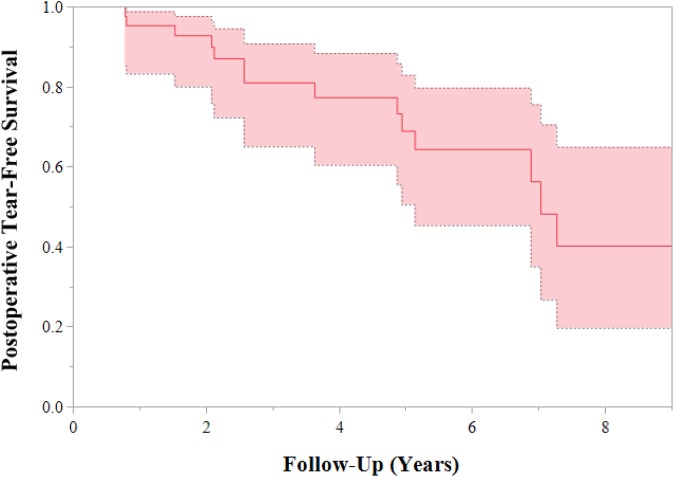
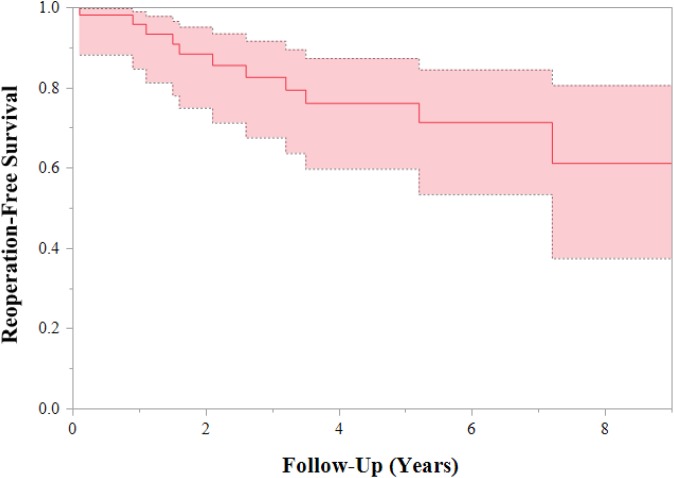
At final follow-up, 14 of the 50 patients (28%) initially diagnosed with a lateral meniscal tear were found to have a postoperative retear on repeat MRI or subsequent diagnostic arthroscopy. Of these, 4 patients had been treated with meniscal repair, and 10 had been treated with partial lateral meniscectomy. Following index surgery, tear-free survival was 93% at 2 years, 71% at 5 years, and 41% at 8 years (Figure 2), and reoperation-free survival was 89% at 2 years, 76% at 5 years, and 61% at 8 years (Figure 3). Young age (hazard ratio [HR], 0.96; P = .01) and open growth plates (HR, 3.19; P = .03) were associated with increased incidence of postoperative retear (Table 3), with a 4% decrease in risk of retear for every year increase in age at diagnosis. No association was found between sex (female: HR, 2.14; 95% CI, 0.71-6.45; P = .18), body mass index (BMI; HR, 1.02; 95% CI, 0.26-3.90; P = .98), or smoking (HR, 0.89; P = .85) and postoperative retear (Table 3). When treatment choice and hazard of postoperative retear or reoperation were evaluated, the type of operative intervention performed was found to have no significant effect on outcome, with meniscectomy and saucerization performing similarly to meniscal repair (P = .18 in both cases). Secondary surgery included 4 repeat partial lateral meniscectomies, 3 total knee arthroplasties, 1 eight-Plate (Orthofix) application for guided growth in the setting of valgus malalignment, 1 lateral meniscal re-repair, 1 lateral meniscal transplant, 1 loose body removal, 1 lateral femoral condyle osteochondral autograft transplantation surgery, 1 osteochondral defect retrograde drilling, and 1 lateral unicompartmental knee arthroplasty.
Figure 2.
Survival free of retear after index procedure. Shading indicates 95% CI.
Figure 3.
Survival free of reoperation after index procedure. Shading indicates 95% CI.
TABLE 3.
Risk Factors for Postoperative Meniscal Reteara
| Variable | HR (95% CI) | P |
|---|---|---|
| Age (per year increase) | 0.96 (0.93-0.99) | .01 |
| Growth plate status | ||
| Closed | Reference | |
| Open | 3.19 (1.15-8.88) | .03 |
| Sex | ||
| Male | Reference | |
| Female | 2.14 (0.71-6.45) | .18 |
| Body mass index | ||
| <30 | Reference | |
| ≥30 | 1.02 (0.26-3.90) | .98 |
| Smoking status | ||
| Nonsmoker | Reference | |
| Previous smoker | 1.64 (0.53-5.09) | .39 |
| Current smoker | 0.89 (0.27-2.92) | .85 |
| Surgical treatment | ||
| Direct repair | Reference | |
| Partial meniscectomy | 0.30 (0.05-1.72) | .18 |
| Saucerization | 0.51 (0.19-1.37) | .18 |
aBold indicates statistical significance (P < .05). HR, hazard ratio.
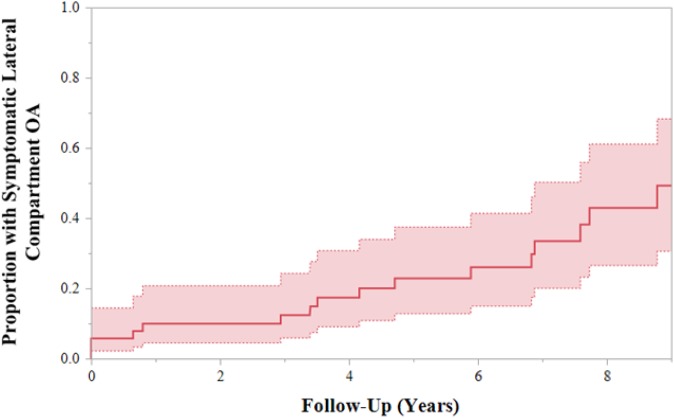
Overall progression to symptomatic lateral compartment OA was 10% at 2 years, 24% at 5 years, and 50% at 8 years (Figure 4). Of the 18 patients who developed symptomatic lateral compartment OA, 11 (61%) had a Kellgren-Lawrence grade of ≥2 on their last radiographic follow-up. Type of operative intervention performed (partial meniscectomy, saucerization, or direct repair) was found to have no significant effect on progression to lateral compartment OA (reference, P = .28, and P = .50, respectively). Risk for lateral compartment OA on final radiographs was noted to increase by 2% (P = .046) for every additional year in age at diagnosis. An increased risk for progression to symptomatic lateral compartment OA was observed in patients with a BMI ≥30 (P < .01). No association was found between growth plate status, sex, or smoking and risk for progression to symptomatic lateral compartment OA (Table 4).
Figure 4.
Cumulative incidence of progression to lateral compartment osteoarthritis (OA). Shading indicates 95% CI.
TABLE 4.
Risk Factors for Progression to Lateral Compartment Osteoarthritisa
| Variable | HR (95% CI) | P |
|---|---|---|
| Age (per year increase) | 1.02 (1.00-1.05) | .046 |
| Growth plate status | ||
| Closed | Reference | |
| Open | 0.58 (0.20-1.70) | .23 |
| Sex | ||
| Male | Reference | |
| Female | 0.92 (0.36-2.35) | .86 |
| Body mass index | ||
| <30 | Reference | |
| ≥30 | 3.75 (1.43-9.84) | <.01 |
| Smoking status | ||
| Nonsmoker | Reference | |
| Previous smoker | 0.75 (0.26-2.20) | .60 |
| Current smoker | 1.01 (0.29-3.49) | .99 |
aBold indicates statistical significance (P < .05). HR, hazard ratio.
Discussion
The natural history and long-term outcome of surgically treated symptomatic lateral discoid meniscus and associated meniscal tears in young patients remain unclear. Clinical concerns include meniscal retear and progression to OA. The purpose of this study was to describe the rate and factors associated with recurrent lateral discoid meniscal tears after surgical treatment and to evaluate the rate of progression and factors associated with symptomatic lateral compartment OA at a minimum clinical follow-up of 2 years.
Patients with a symptomatic lateral discoid meniscus in this cohort had a high rate of meniscal retears (59% at 8 years) following meniscal repair or partial meniscectomy. These subsequent tears contributed to the high reoperation rate (39% at 8 years). Need for reoperation was determined by the treating surgeon according to the tear type, location, and presence of mechanical symptoms. Young age and open growth plates were risk factors for postoperative retear. We inferred that young, active patients may be at higher risk for injury to an already susceptible meniscus, as young age and open growth plate status are considered surrogates for an increased activity level. Nevertheless, these observations require further investigation outside the scope of this study, such as a direct comparison with the retear rates of patients with nondiscoid meniscus. No association was observed between sex, BMI, or smoking and risk of postoperative retear. The postoperative retear rate observed in this cohort is higher than the contemporary failure rates between 10% and 16% reported for all-inside and inside-out meniscal repairs.5 The failure rate noted for lateral discoid meniscal tears following repair or partial meniscectomy in this population more closely matched failure rates reported for revision meniscal repairs.14
The inferior quality of discoid meniscal tissue is suspected to be responsible for this increased risk of failure. Cadaveric studies on the discoid meniscus have proposed a biomechanical explanation for these inferior properties. A study analyzing the ultrastructural content of the discoid meniscus with transmission electron microscopy demonstrated an abnormally low number and more heterogeneous arrangement of collagen fibers in discoid menisci.1 The authors suggested that this abnormal composition leads to poor vascularity and stability and affects the structure’s overall healing potential. Yet, a more recent study quantifying the degree of heterogeneity of discoid meniscal collagen ultrastructure proposed that the observed disarray of collagen fibers is associated with secondary degeneration and may be an acquired, rather than an intrinsic, property of discoid menisci.3 Whether intrinsic or acquired, these studies highlight the inferior quality of discoid meniscal tissue, which could explain its propensity for degeneration and tear.
In this cohort, the choice of surgical treatment did not affect outcome, with a similar risk for postoperative retear and reoperation following meniscal repair or partial meniscectomy. Despite these observations, most authors would agree that meniscal preservation with repair or partial meniscectomy is preferred over total meniscectomy given the load-sharing role of the meniscus, young age of patients with discoid meniscus, and desire to minimize early postmeniscectomy OA.10,12,26 A 2017 systematic review evaluating surgical outcomes in patients with discoid meniscus strongly supported saucerization over total meniscectomy.23
Yet, available evidence reviewed in this study failed to demonstrate improved results with meniscal repair. The heterogeneity of discoid meniscal tears, as well as numerous other confounding variables, limited our ability to comment on the role of discoid meniscal repair. This is especially true given that discoid meniscal tears are often horizontal cleavage or complex degenerative tears and are thus not amenable to repair.6,22 Prior studies have suggested that tear patterns could be associated with different discoid types; thus, meniscal repair may be more feasible in certain patients and not others.2 Additionally, ultrastructural analysis has shown that the degree of collagen fiber disarray observed in the discoid meniscus may vary depending on its location.4 In this analysis, the peripheral portion of the discoid meniscus was found to be more robust and organized than the thinner and loosely irregular central portion. This confers the improved ability of the peripheral portion to resist hoop stresses. Thus, efforts at preserving this portion of the discoid meniscus may be critical in preserving function.
Choice of treatment for discoid meniscal tears remains a highly debated topic, and treatment ultimately depends on individual cases and surgeons’ preferences. The lateral discoid meniscal tears that underwent repair in our cohort were likely more severe tears, tears with associated peripheral instability, and tears that were amenable to repair. Meniscal tears not amenable to repair, which underwent partial meniscectomy, were treated with the goal of preserving as much meniscal tissue as possible.
At final follow-up, patients demonstrated a high rate of progression to early symptomatic lateral compartment OA (50% at 8 years), with a majority of patients (61%) demonstrating a lateral compartment Kellgren-Lawrence grade of ≥2. Our observations are consistent with recently reported data on OA progression in patients with symptomatic lateral discoid meniscus who underwent partial meniscectomy.15 Those authors reported radiographic progression to lateral compartment OA in 69% of the knees, with >30% of patients noting unfavorable clinical outcomes at 10-year follow-up. These observations validate the concern that patients with lateral discoid meniscus have a propensity to develop early lateral compartment wear.
In the current study, the risk of progression to lateral compartment OA after surgical treatment was associated with older age at diagnosis of lateral discoid meniscus and with obesity (BMI ≥30). No association was found between sex, smoking status, or type of surgical intervention and risk of progression to OA. It remains unclear whether the observed lateral compartment degenerative changes can be attributed solely to the effects of partial meniscectomy or if the discoid meniscus confers less protection of joint surfaces than the normal meniscus, given its observed inferior biomechanical properties and/or lack of peripheral attachments. For instance, peripheral instability did not significantly predict arthritis at last follow-up. Moreover, the high rate of associated meniscal tears observed in patients with discoid meniscus raises the question of whether degenerative joint changes result from cartilage lesions at the time of meniscal tear. A 2014 study investigating the relationship between discoid meniscal tears and traumatic cartilage lesions found that 27% of patients with a discoid meniscal tear had a concomitant cartilage lesion at the time of diagnosis.6 These were often located in the lateral tibial plateau and predominantly affected female patients with elevated BMI who presented with symptoms lasting more than 6 months. It is likely that the etiology behind early lateral compartment OA in patients with symptomatic lateral discoid meniscus cannot be explained by a single variable but is rather multifactorial.
To our knowledge, this is the first study to present data on outcomes of symptomatic lateral discoid meniscus using a geographically defined population. The unique medical records linkage system provided by the Rochester Epidemiology Project allows almost complete ascertainment of all cases of symptomatic lateral discoid meniscus treated in Olmsted County during the study period. Nevertheless, this retrospective study has several important limitations. As patients were not prospectively assessed with standardized follow-up visits and radiographs, there may be a bias toward capturing patients who experienced poor outcomes. This study may also be underpowered to detect differences in outcomes among the different treatment groups. Additionally, given the heterogeneity of this patient population, it is difficult to ascertain the effect of confounding variables in the observed outcomes. Moreover, values reported for this cohort are largely based on MRI and radiographic data, and for this reason, our observations may not necessarily correlate with patient-reported clinical outcomes.
Although the Rochester Epidemiology Project allows almost complete ascertainment of identifying all clinically recognized symptomatic discoid meniscus diagnoses within a well-defined population, the database may not capture patients who sought medical treatment outside Olmsted County and those patients who were misdiagnosed. Moreover, the database is composed of mostly white patients, and, as such, observations from this cohort may not be generalizable to other, more ethnically diverse geographic regions. Additional limitations to our study include the inconsistent availability of preoperative alignment films, the variability in imaging methodology, and the inability to reliably report the type of meniscal tear, the percentage of meniscus remaining after partial meniscectomy, or the presence of concomitant cartilage injuries. Therefore, we were unable to assess the risk of retear and progression to symptomatic lateral compartment OA based on preoperative alignment, type of meniscal tear, or concomitant cartilage injuries at the time of presentation.
Conclusion
Patients who underwent surgical management with either partial meniscectomy or meniscal repair demonstrated a high rate of recurrent meniscal tear. Younger age and open growth plates were associated with an increased risk of retear. Approximately 50% of patients developed symptomatic lateral compartment OA at 8 years from initial presentation, with almost two-thirds of the patients having a Kellgren-Lawrence grade of ≥2 at final radiographic follow-up. Risk factors for OA progression were older patient age and BMI ≥30 at the time of presentation. As such, we recommend close postoperative follow-up of young, skeletally immature patients following surgical meniscal repair and counseling of older patients with higher BMI regarding risk factors for discoid meniscus–associated OA.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: O.D.S. has received hospitality payments from Zimmer Biomet. M.H. has received hospitality payments from DePuy Synthes. C.L.C. has received educational support from Stryker, Zimmer Biomet, and Arthrex. D.L.D. has received research support from Arthrex and is a member of the NBA/GE Strategic Advisory Board. D.L.D.’s spouse has stock/stock options in and receives royalties from Tenex Health and Sonex Health. B.A.L. receives royalties from Arthrex; is a consultant for Arthrex, ConMed Linvatec, and Smith & Nephew; receives research support from Arthrex, Biomet, Smith & Nephew, and Stryker. M.J.S. receives royalties from Arthrex, is a consultant for Arthrex, and receives research support from Stryker. A.J.K. receives research support from Aesculap/B. Braun, Arthrex, the Arthritis Foundation, Ceterix, Histogenics, the Musculoskeletal Transplantation Foundation, and Depuy Orthopaedics; receives royalties from Arthrex; and is a consultant for Arthrex, JRF Ortho, and Vericel. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Mayo Clinic Institutional Review Board (ID: 16-007076).
References
- 1. Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL. Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med. 2007;35(3):475–478. [DOI] [PubMed] [Google Scholar]
- 2. Bin SI, Kim JC, Kim JM, Park SS, Han YK. Correlation between type of discoid lateral menisci and tear pattern. Knee Surg Sports Traumatol Arthrosc. 2002;10(4):218–222. [DOI] [PubMed] [Google Scholar]
- 3. Choi YH, Seo YJ, Ha JM, Jung KH, Kim J, Song SY. Collagenous ultrastructure of the discoid meniscus: a transmission electron microscopy study. Am J Sports Med. 2017;45(3):598–603. [DOI] [PubMed] [Google Scholar]
- 4. Cui JH, Min BH. Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy. 2007;23(6):635–641. [DOI] [PubMed] [Google Scholar]
- 5. Fillingham YA, Riboh JC, Erickson BJ, Bach BR, Jr, Yanke AB. Inside-out versus all-inside repair of isolated meniscal tears: an updated systematic review. Am J Sports Med. 2017;45(1):234–242. [DOI] [PubMed] [Google Scholar]
- 6. Fu D, Guo L, Yang L, Chen G, Duan X. Discoid lateral meniscus tears and concomitant articular cartilage lesions in the knee. Arthroscopy. 2014;30(3):311–318. [DOI] [PubMed] [Google Scholar]
- 7. Furumatsu T, Maehara A, Okazaki Y, Ozaki T. Intercondylar and central regions of complete discoid lateral meniscus have different cell and matrix organizations. J Orthop Sci. 2018;23(5):811–818. [DOI] [PubMed] [Google Scholar]
- 8. Good CR, Green DW, Griffith MH, Valen AW, Widmann RF, Rodeo SA. Arthroscopic treatment of symptomatic discoid meniscus in children: classification, technique, and results. Arthroscopy. 2007;23(2):157–163. [DOI] [PubMed] [Google Scholar]
- 9. Jeannopoulos CL. Observations on discoid menisci. J Bone Joint Surg Am. 1950;32(3):649–652. [PubMed] [Google Scholar]
- 10. Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthop Surg. 1996;4(4):191–200. [DOI] [PubMed] [Google Scholar]
- 11. Kim JH, Bin SI, Lee BS, Kim JM, Kim NK, Lee CR. Does discoid lateral meniscus have inborn peripheral rim instability? Comparison between intact discoid lateral meniscus and normal lateral meniscus. Arch Orthop Trauma Surg. 2018;138(12):1725–1730. [DOI] [PubMed] [Google Scholar]
- 12. Kramer DE, Micheli LJ. Meniscal tears and discoid meniscus in children: diagnosis and treatment. J Am Acad Orthop Surg. 2009;17(11):698–707. [DOI] [PubMed] [Google Scholar]
- 13. Kroiss F. Die Verletzungen der Kniegelenkoszwischenknorpel und ihrer Verbindungen. Beitr Klin Chir. 1910;66:598–801. [Google Scholar]
- 14. Krych AJ, Reardon P, Sousa P, Levy BA, Dahm DL, Stuart MJ. Clinical outcomes after revision meniscus repair. Arthroscopy. 2016;32(9):1831–1837. [DOI] [PubMed] [Google Scholar]
- 15. Lee CR, Bin SI, Kim JM, Lee BS, Kim NK. Arthroscopic partial meniscectomy in young patients with symptomatic discoid lateral meniscus: an average 10-year follow-up study. Arch Orthop Trauma Surg. 2018;138(3):369–376. [DOI] [PubMed] [Google Scholar]
- 16. Nathan PA, Cole SC. Discoid meniscus: a clinical and pathologic study. Clin Orthop Relat Res. 1969;64:107–113. [PubMed] [Google Scholar]
- 17. Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rohren EM, Kosarek FJ, Helms CA. Discoid lateral meniscus and the frequency of meniscal tears. Skeletal Radiol. 2001;30(6):316–320. [DOI] [PubMed] [Google Scholar]
- 19. Sabbag OD, Hevesi M, Sanders TL, et al. Incidence and treatment trends of symptomatic discoid lateral menisci: an 18-year population-based study. Orthop J Sports Med. 2018;6(9):2325967118797886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Samoto N, Kozuma M, Tokuhisa T, Kobayashi K. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging. 2002;20(1):59–64. [DOI] [PubMed] [Google Scholar]
- 21. Shieh AK, Edmonds EW, Pennock AT. Revision meniscal surgery in children and adolescents: risk factors and mechanisms for failure and subsequent management. Am J Sports Med. 2016;44(4):838–843. [DOI] [PubMed] [Google Scholar]
- 22. Smillie IS. The congenital discoid meniscus. J Bone Joint Surg Br. 1948;30:671–682. [PubMed] [Google Scholar]
- 23. Smuin DM, Swenson RD, Dhawan A. Saucerization versus complete resection of a symptomatic discoid lateral meniscus at short- and long-term follow-up: a systematic review. Arthroscopy. 2017;33(9):1733–1742. [DOI] [PubMed] [Google Scholar]
- 24. St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Watanabe M, Takeda S, Ikeuchi H. Atlas of Arthroscopy. Tokyo, Japan: Igaku-Shoin; 1978. [Google Scholar]
- 26. Yaniv M, Blumberg N. The discoid meniscus. J Child Orthop. 2007;1(2):89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]