Abstract
Introduction:
Distal femoral shaft fractures are characterized by increasing incidence and complexity and are still considered a challenging problem (high morbidity and mortality). No consensus on best surgical option has been achieved.
Aim:
This study aims is to investigate radiographic, mineral bone densitometry and clinical outcomes of locking retrograde intramedullary (LRN) nailing and anatomical locking plate to surgically treat distal femoral shaft fractures in young adults based on the hypothesis that there is no statistical difference among the two surgical options in terms of results (radiographic, bone densitometry and outcomes assessment).
Methods:
Retrospective study: 30 patients divided into 2 groups (Group 1 LRN, Group 2 Nailing). Average age was 42.67±18.32 for Group 1 and 42.84 ±18.32 for Group 2 (range of age 18-65 for both groups). Gender Ratio (male: female) was 2.75 (11:4) for both Group 1 and 2. AO Classification, NUSS and RUSH score, VAS, Dexa scans, plain radiographs were used. Evaluation endpoint: 12 months after surgery (mean follow up 16.24).
Results:
No statistical difference in terms of surgery time, transfusions, wound healing. Similar results with regard to average time of bone healing, RUSH scores, VAS, regression between RUSH and VAS, average correlation clinical-radiographic results and patients outcomes. Only one patient of each group had reduction of mineral bone densitometry values.
Conclusion:
No statistical difference about the use of LNR or Nailing for treatment of distal femur shaft fractures in terms of radiographic, bone densitometry and outcomes has been found accordingly to our results. Good subjective and objective results are provided by both techniques. The choice among the two techniques must be based on surgeons’ experience, indications and subjective patients’ aspects. The absence of relevant similar data in the published literature does not allow definitive validation (or rejection) of our hypothesis. A more powered study with bigger cohort is needed for definitive validation.
Keywords: Distal Femoral Shaft Fractures, Locking Plate, Locking Retrograde Nail, Bone Healing, Radiographic Assessment
1. INTRODUCTION
Distal femoral fractures currently comprise about 4-6% of all femur fractures. The incidence and complexity of these types of injury are increasing due to the increasing rate of high-energy trauma, particularly in young patients. Low energy fractures (on native or prosthetic knee) of osteoporotic bones are instead more characteristic in the elderly population (1).
There are a number of reasons for which these fractures remain a challenging problem, involving mainly high rates of morbidity and mortality and challenging operative fixation of osteoporotic bones or periprosthetic fractures. Recognized treatment goals are to restore axial alignment, achieve anatomic reduction of the joint surface, and minimize joint stiffness by allowing early mobilization, all with minimal soft tissue disruption (2).
Studies have shown that internal fixation devices provide superior outcomes if compared to closed methods by providing good stability which consequently allows early mobilization and good functional outcomes (3, 4). In particular intramedullary nails and plates have been both successful strategies, with a reduction in surgical blood loss, operating time, and hospitalization compared to other methods. However consensus about the best management option remains controversial with results that significantly vary from one study to others (3, 4).
2. AIM
This study aims is to investigate radiographic, mineral bone densitometry and clinical outcomes of locking retrograde intramedullary (LRN) nailing and anatomical locking plate to surgically treat distal femoral shaft fractures in young adults based on the hypothesis that there is no statistical difference among the two surgical options in terms of results (radiographic, bone densitometry and outcomes assessment) (5-11).
3. METHODS
From January 2015 to January 2018, 72 patients with distal femoral shaft fractures were admitted and surgically treated at 2 trauma centers. From these 72 patients, we finally included 30 patients with femoral fracture of the distal third in our study (retrospective study). These 30 patients were further divided into 2 groups: LRN patients were treated with locking retrograde nail; Plate 2 patients were treated with plating.
Inclusion criteria: patients who sustained a distal third femoral fracture in the set-time frame admitted and treated at 2 trauma centers, pre-trauma conditions and absence of local or systemic disease able to affect the surgical treatment and his comorbidity and mortality, fitness to undergo surgery from the anaesthetic team, availability for 12 months postoperative clinical and radiological follow up.
Exclusion criteria: hematological or oncological patients, presence of acute or chronic infections; 3.2 type of fracture according to AO ( 12), age under 18 or over 65 for males, age over 50 for female or early menopause patients, bone metabolism disorders, rheumatological diseases, polytrauma, no previous injury on ipsilateral lower legs.
All fractures were classified according to the AO classification (12). Classifications for all patients are described in Table 1.
Table 1. Description of the populations.
| Description of population | LRN | Plate | P Value |
|---|---|---|---|
| Number of Patients | 15 | 15 | P>0.05 |
| Average age, years (standard deviation) | 42.67(±18.32) | 42.84(±18.32) | P>0.05 |
| Range of age. years | 18-65 | 18-65 | P>0.05 |
| Gender Ratio (male:female) | 2.75(11:4) | 2.75(11:4) | P>0.05 |
| Mechanism of injury | Fall From Height: 2(13.33%) | Fall From Height: 2(13.33%) | P>0.05 |
| Traffic Accident: 8(53.34%) | Traffic Accident: 8(53.34%) | P>0.05 | |
| Work Accident: 3(20%) | Work Accident: 3(20%) | P>0.05 | |
| Shooting: 2(13.33%) | Shooting: 2(13.33%) | P>0.05 | |
| Type of femoral shaft fractures according to AO | A1: 2(13.33%) | A1: 2(13.33%) | P>0.05 |
| A2:2(13.33%) | A2:2(13.33%) | P>0.05 | |
| A3:1(6.67%) | A3:1(6.67%) | P>0.05 | |
| B1:2(13.33.%) | B1:2(13.33.%) | P>0.05 | |
| B2:1(6.67%) | B2:1(6.67%) | P>0.05 | |
| B3:2(13.33%) | B3:2(13.33%) | P>0.05 | |
| C1:2(13.33%) | C1:2(13.33%) | P>0.05 | |
| C2:2(13.33%) | C2:2(13.33%) | P>0.05 | |
| C3:1(6.67%) | C3:1(6.67%) | P>0.05 | |
| Orthopedic device used in the surgery for the osteosynthesis of the femoral shaft fracture | Locked Retrograde Intramedullary Nail | Condylar Plat and screws | Not calculated |
| Work Occupation | Agricultural Industry: 3 (20%) | Agricultural Industry: 3 (20%) | P>0.05 |
| Industrial Sector: 9 (60%) | Industrial Sector: 9 (60%) | P>0.05 | |
| Tertiary Industry: 3 (60%) | Tertiary Industry: 3 (20%) | P>0.05 | |
| Injured lower Limb Side | Right: 6 (40%) | Right: 6 (40%) | Not calculated |
| Left: 9 (60%) | Left: 9 (60%) |
All patients were informed in a clear and comprehensive way of the type of treatment (See Operative Surgical Technique) and other possible surgical and conservative alternatives. Patients were treated according to the ethical standards of the Helsinki Declaration, and were invited to read, understand, and sign the informed consent form. Average age was 42.67±18.32 for Group 1 and 42.84 ±18.32 for Group 2 (range of age 18-65 for both groups). Gender Ratio (male: female) was 2.75 (11:4) for both Group 1 and 2. The other relevant demographic data and mechanisms of injury are described in Table 1.
We retrospectively used the Non-Union Scoring System (NUSS) (Table 1) (13) to study the bone healing on radiographs. The criteria to evaluate the patients groups bone healing were: Two readers utilized the RUSH (Radiographic Union Score for Hip) score provided by Chiavaras et al (14,15) and derived from the RUST (Radiographic Union Scale in Tibial Fractures) scoring system. RUSH provides four component scores: cortical bridging, cortical disappearance, trabecular consolidation, and trabecular disappearance. Each component can be scored from 1 to 3. Similarly, the two trabecular indices were scored from1 to 3, each based on consolidation for one of the indices, and fracture line disappearance for the other. The overall RUSH score therefore ranged from a minimum of 10 to a maximum of 30. Pain visual analogic score (VAS) was collected the same day when the X-rays were taken (16). We study the mineral bone densitometry of the top part of the femur using DEXA Scans (17). The femoral alignment was measured using plain radiographs and correlated with clinical outcomes.
The evaluation endpoint was set at 12 months after surgery.
Surgical technique for LRN: After having checked for associated fractures (e.g. fracture of the ipsilateral femoral neck), alignment, knee stability and limb length, patients were positioned supine on the radiolucent table. Routine prep and draping with a sterile bump under the knee. The anterior transtendinous approach to the knee was used with knee kept in about 30 degrees of flexion to avoid the action of the gastrocnemius in moving the distal fragment (incision from inferior pole of patella and tenotomy). Self-retainers, suction of synovial fluid and accurate haemostasis performed to improve visualization. A guidewire was then inserted at the level of the center of the intercondylar notch to the distal metaphysis under fluoroscopy check, followed by the reamer. These were then removed and replaced by a balltip guidewire in the femoral canal that was pushed into the distal aspect of the fracture. Pulling traction was then applied at 30 degree angle to achieve good fracture reduction. The guidewire subsequently was pushed past the fracture site and 3 cm past the lesser trochanter under fluoroscopy check. A ruler was used to decide the nail length and reaming of the canal was performed. A nail 1.5 below the size of the last used reamer was then inserted over the guidewire and pushed past the fracture site till fluoroscopy confirmation of good position. Distal interlocking screws (as indicated) were positioned (most distal first) using bicortical drilling and fluoroscopy. Same process for the proximal interlocking screws (most proximal first, 34 or 36 mm screws). Confirmation of final good metalwork position and no rotation of the distal femur were obtained with fluoroscopy (AP and lateral radiographs) with knee extended and 90 degree of bending. Good range of motion of both knee and hip, limb length and rotation were checked. Appropriate irrigation and haemostasis were assured throughout the entire procedure. Closure in layers (starting with patellar tendon and paratenon) was performed and surgical dressing applied.
Surgical technique for Plate: After having checked for associated fractures (e.g. fracture of the ipsilateral femoral neck), alignment, knee stability and limb length, patients were positioned supine on the radiolucent table. Routine prep and draping with a sterile bump under the knee. A midline approach with extended lateral parapatellar arthrotomy was used. This was followed by exposure of the femoral condyles and subluxation of the patella to achieve good fracture site exposure. Periosteal elevation of the capsule was performed assuring preservation of the lateral collateral ligament. Next step was the achievement of fracture reduction by the use of pointed reduction forceps under direct visualization and fluoroscopy check and the aid of K wires. A locking plate was then positioned submuscularly followed by fixation of the distal segment first, assuring that screw trajectory was parallel to the joint (position checked with fluoroscopy). Partially threaded or overdrilled fully threaded screws through the plate were used to provide interfragmentary compression. Two locking screws were used to ensure plate and alignment. Additional screws were then positioned appropriately. Fluoroscopy images were taken to ensure good metalwork position and absence of penetration through the intercondylar notch and check length, rotation and alignment. Flexion-extension reduction was achieved. Appropriate irrigation and haemostasis were assured throughout the entire procedure. Closure in layers was performed and surgical dressing applied.
Descriptive statistics were used to summarize the characteristics of the study group and subgroups, including means and standard deviations of all continuous variables. The t-test was used to compare continuous outcomes. The Chi-square test or Fisher’s exact test (in subgroups smaller than 10 patients) were used to compare categorical variables. The statistical significance was defined as P < 0.05. We used Pearson correlation coefficient (r) was used to compare the predictive score of outcomes and quality of life. Mean ages (and their range) of the patients were rounded at the closest year. The predictive score of outcomes and quality of life and their ranges were approximated at the first decimal while at the second decimal was approximated Pearson correlation coefficient (r).
4. RESULTS
The mean of follow-up was 16.24 (±0.44; range 12-24) months for LNR and 16.13 (±0.49; range 12-24) months for Plate, p>0.05. The surgery lasted an average of 52.8 (±15.6; range 25-76) minutes in LNR while 60.8 (±20.4; range 38 -83) minutes for Plate, p>0.05. The RBC IU of preoperative transfusions in our patients was on average 2.9 (±1.42; range 0-7) in LNR while 2.8 (±1.4; range 0-6) for Plate, p>0.05.
In both groups, patients demonstrated wound healing within 21 days. During the follow up we had no complications in both groups. The average time of bone healing was 142.4 (±15.7; 72 -168) days after the surgery in LNR while 143.6 (±14.4; 72 -168) days for Plate, p>0.05. At average day of the bone healing the RUSH was 26.8 (±2.4; range 24.1-30) point in LNR while 26.9 (±2.6; range 24.1-30) in Plate, p>0.05. At the average day of the bone healing the VAS was of 2.3 (±0.7; range 0-4) point in LNR while 2.2 (±0.8; range 0-4) in Plate, p>0.05. We found that at average day of bone healing the regression between RUSH and VAS scores showed a p value of 0.059 in LNR while p= 0.061 in Plate, p>0.05.
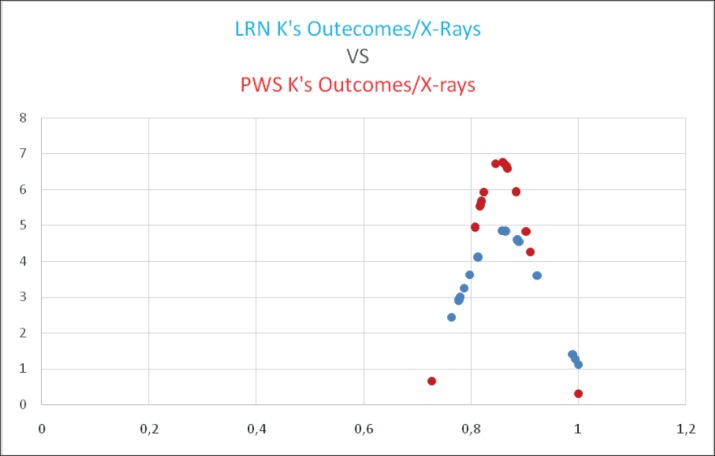
Two patients, one for each group had a reduction of mineral bone densitometry of proximal (from normal to ostheopenia) at the evaluation endpoints. The Average Correlation clinical-radiographic results and patients outcomes was high according to Cohen κ: 0.859457333±0.085103467 for LNR (Figure 1) while κ: 0.853606667±0,060782874 for Plate (Figure 1), p>0.05.
Figures 1. Comparison between the two Gaussian distributions at the12 months after the surgery, there was not a statistically differences p<0.05.
5. DISCUSSION
Fractures of the distal femur are relatively rare (0.4% of all fractures and 3% of femoral fractures and exhibit a bimodal distribution with a peak in frequency in young men and elderly women. A high energy trauma is frequently linked to young patients’ injury while a low energy trauma is related to older patients with osteoporotic bone. Conservative treatments are rarely used (reserved to bedridden patients or fractures with none or little displacement. A sufficient stabilization usually requires surgical management in order to withstand static and dynamic forces applied to the femur (18,19).
These fractures are serious with a high mortality rate in elderly populations which is comparable to that found in the proximal femur. Most frequent complications include infection and septic non-union, aseptic non-union, residual stiffness, secondary post-traumatic osteoarthritis, with initial chondral injury as well as incomplete reduction (20).
The main therapeutic principles of surgical management is to prioritize joint reconstruction if the fracture has an intra-articular extension. Exposure of epiphyseal fracture lines is obtained with the knee bent, especially with frontal lines. Stabilization on the frontal plane is usually not difficult, while sagittal plane stability with rotation of the condyles is much more difficult. The metaphyseal portion, in particular of the anterior cortex can serve as a reference point. The second step includes reducing the epiphysis on the metaphyso-diaphysis: this is performed with the leg in extension. In case of a comminute fracture, rotation and length should be carefully controlled (18).
Many surgical options are available for distal femur extra-articular fractures, including mini-invasive procedures. Open reduction and internal plate fixation is required if the fracture is intra-articular. The primary goal is thought to be a good restoration of the articular surface to the femoral shaft, maintenance of good stability and alignment, early mobilization and rehabilitation. The choice of the surgical technique takes into account patients’ functional goals, fracture characteristics, health comorbidities, bone quality, and risk of malunion and nonunion (2).
Among the many techniques, intramedullary nails and plates have been said to be successful strategies, able to guarantee good outcomes at a low complication rate compared to other surgical techniques. However consensus about the best management option remains controversial with results that significantly vary from one study to others. Particularly it remains unclear if one of the two techniques is able to provide better clinical and functional outcomes and/or lower complication/mortality rate (3, 4).
The traditional indications for retrograde nailing are the presence of an extra-articular fracture or a simple intra-articular fracture with little or no displacement; the traditional indications for locking compression plating are the presence of an extra-articular fractures, sagittal unicondylar fractures or supra- and intercondylar fractures (21).
Several biomechanical studies have shown that locking systems are better than classic internal fixation (DCP plate, retrograde nailing, blade plate) (22, 23, 24). In the best of our knowledge no studies have been performed to compare specifically retrograde intramedullary nailing to locking plates.
With regards to clinical results the scenario becomes much wider. Several studies have compared the different surgical techniques with ambiguous and controversial results. LCP was shown to cause a higher complication, surgical revision and non-union rates in some studies, while in other studies this technique seemed to guarantee union in all cases, good recovery of alignment and high quality function (25, 26). Retrograde intramedullary nailing was shown to provide better surgical revision and mal-union rates compared to other techniques (27). Other studies highlighted the absence of any statistical difference in in functional recovery between patients treated for single or multiple fractures. Comparisons in the literature between retrograde intramedullary nailing and blade plate by a mini-invasive approach have not shown any difference between intra-articular or extra-articular fractures (28). Moreover Markmiller et al. (29) did not report improved results for any particular implant for identical indications. In the scenario of uncertainty it seems that high quality results are more dependent upon the surgical technique and experience of the surgeon than the choice of implant (30).
A recent review highlighted the major limitations of the available evidence concerning current treatment interventions for fractures of the distal femur exist and that the currently available evidence is incomplete and insufficient to inform current clinical practice. They recommend the planning of a definitive, pragmatic, multicentre randomised controlled clinical trial comparing contemporary treatments such as locked plates and intramedullary nails (31).
We have not been able to carry on such a relevant study; however we are presenting a retrospective group control study (15 patients forming each of the 2 groups) including patients treated at 2 trauma centers and with which we present relative radiographic, bone densitometry and outcomes assessment.
We did not found any significant difference in terms of duration of surgery, despite the mean duration of LNR surgery exhibited a higher value (60.8 minutes against 52.8 minutes of nailing procedure). Neither we could find a statistically significant difference with regards to the RBC IU of preoperative transfusion. Despite the two different surgical approaches and size of the incisions, all patients of both groups had appropriate wound healing by 21 days post-op. These results highlighted the fact that the choice among the two studied procedure does not affect risks for the patients related to duration of surgery (e.g. blood loss, anaesthetic risks, tourniquet time),wound management and potential complications and management of blood loss. Other studies have hypothesised otherwise, with significant difference in terms of mean duration of surgery and intra-op blood loos discerned in favour of plating although complications rates were equivalent. Mean duration of union was not statistically different among the groups, but anyway longer for the plate group. Functional scores were comparable. The authors concluded however that surgical planning and expertise rather than the choice of implant are more crucial for optimal results, in keeping with our hypothesis (33).
Similar results were obtained with regards to bone healing timing. No statistical difference was noted among the groups, with average time of bone healing being of 142.4 days for LNR Group and 143.6 for Plating Group. Similarly RUSH scores were noted to be not very dissimilar (26.8 for LNR Group and 26.9 for Plating Group). These results supports the hypothesis that good fracture healing is achieved with both surgical techniques and that bony healing is not negatively affected by any of the two procedures. Therefore this aspect should not drive the surgeon to choose a technique instead of the other, but reasons for this choice must be solely connected to surgical indications and patients’ age, functional goals and comorbidities. Literature data supports that there is no evidence of any significant difference in any other outcomes at any time point and a definitive randomized trial could provide the lacking answers and validation of current results (33, 34).
Satisfactory results in both groups are also testified by the obtainment of similar VAS scores (questionnaire administered at the time of the xray taken to show level of fracture healing). Linking RUSH and VAS scores, we found that the regression between RUSH and VAS scores showed a p value of 0.059 in LNR while a value of p= 0.061 in Plate Group (at time of bone healing). More strength and significance to our results is given by Cohen K values for the average correlation of clinical-radiographic results and patients outcomes: k: 0.859457333±0.085103467 for LNR and κ: 0.853606667±0,060782874 for Plate. No significant difference in terms of bone densitometry where found in the two groups following evaluation of Dexa scans results. Only one patient of each group was found to have a reduction of mineral bone densitometry values.
In the best of our knowledge this is the first study that correlates the above results for patients with distal femur fracture treated with LNR or nailing. This does not allow us to compare our results with those obtained in other studies (particularly more power studies). However our study gives important information in a context of unclear and debated results and uncertainty and could be considered as a first step for further similar research with the aim to definitively validate our results and hypothesis. In fact it is very important for the surgeon to know implications and expected results of the two surgical options in order to take the best possible decision at the time of management decision. This implies that decision is taken accordingly to appropriate surgical indications and taking into account comorbidities and subjective aspects (such as pre-injury mobility status, goals, rehabilitation, etc…) as already supported in the literature (2, 33, 34).
6. CONCLUSION
Our hypothesis that there is no statistical difference about the use of LNR or Nailing for the treatment of distal femur shaft fractures in terms of radiographic, bone densitometry and outcomes is supported by our results. There is paucity of similar data in the published literature and this does not allow further comparison and/or validation/rejection of our hypothesis. Both procedures provide good subjective and objective results as low complication rates, good union timing and similar satisfactory experience for the patients have been recorded.
We advocate the need for a more powered study and bigger cohorts in order to definitively validate (or eventually reject) our hypothesis. More objective and/or subjective outcomes may be also studied in adjunct to the available ones in order to have a wider scenario and stronger results.
Author’s contribution:
GR, MB, GR, AC and LM gave substantial contributions to the conception and design of the study. VP, JCI, EDC, OB, GP and LM had substantial contribution in data acquisition, analysis, and interpretation of data for the work. GR, MB, GR, AC, VP, JCI, EDC, OB, GP and LM had a part in article preparing for drafting or revising it critically for important intellectual content, and gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms..
Conflict of interest:
There are no conflicts of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Khan AM, Tang QO, Spicer D. The Epidemiology of Adult Distal Femoral Shaft Fractures in a Central London Major Trauma Centre Over Five Years. Open Orthop J. 2017;11:1277–1291. doi: 10.2174/1874325001711011277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gangavalli AK, Nwachuku CO. Management of Distal Femur Fractures in Adults: An Overview of Options Orthop Clin North Am. 2016;47(1):85–96. doi: 10.1016/j.ocl.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Zhang F, Zhu L, Li Y, Chen A. Retrograde versus antegrade intramedullary nailing for femoral fractures: a meta-analysis of randomized controlled trials. Curr Med Res Opin. 2015;31(10):1897–1902. doi: 10.1185/03007995.2015.1078783. [DOI] [PubMed] [Google Scholar]
- 4.Li B, Gao P, Qiu G, Li T. Locked plate versus retrograde intramedullary nail for periprosthetic femur fractures above total knee arthroplasty: a meta-analysis. Int Orthop. 2016;40(8):1689–1695. doi: 10.1007/s00264-015-2962-9. [DOI] [PubMed] [Google Scholar]
- 5.Heiney JP, Battula S, O’Connor JA, Ebraheim N, Schoenfeld AJ, Vrabec G. Distal femoral fixation: a biomechanical comparison of retrograde nail, retrograde intramedullary nail, and prototype locking retrograde nail. Clin Biomech (Bristol, Avon) 2012;27(7):692–696. doi: 10.1016/j.clinbiomech.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Meneghini RM, Keyes BJ, Reddy KK, Maar DC. Modern retrograde intramedullary nails versus periarticular locked plates for supracondylar femur fractures after total knee arthroplasty. J Arthroplasty. 2014;29(7):1478–1481. doi: 10.1016/j.arth.2014.01.025. [DOI] [PubMed] [Google Scholar]
- 7.Kandemir U, Augat P, Konowalczyk S, Wipf F, von Oldenburg G, Schmidt U. Implant Material, Type of Fixation at the Shaft, and Position of Plate Modify Biomechanics of Distal Femur Plate Osteosynthesis. J Orthop Trauma. 2017;31(8):e241–e246. doi: 10.1097/BOT.0000000000000860. [DOI] [PubMed] [Google Scholar]
- 8.Strotman PK, Karunakar MA, Seymour R, Lack WD. Any Cortical Bridging Predicts Healing of Supracondylar Femur Fractures After Treatment With Locked Plating. J Orthop Trauma. 2017;31(10):538–544. doi: 10.1097/BOT.0000000000000887. [DOI] [PubMed] [Google Scholar]
- 9.Sheng W, Ji A, Chen C. Finite Element Analysis of Screw Layout of Locking Plate for Treating Femoral Shaft Fracture. Zhongguo Yi Liao Qi Xie Za Zhi. 2017;41(3):196–199. doi: 10.3969/j.issn.1671-7104.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Başcı O, Karakaşlı A, Kumtepe E, Güran O, Havıtçıoğlu H. Combination of anatomical locking plate and retrograde intramedullary nail in distal femoral fractures: comparison of mechanical stability. Eklem Hastalik Cerrahisi. 2015;26(1):21–26. doi: 10.5606/ehc.2015.06. [DOI] [PubMed] [Google Scholar]
- 11.Kiel J, Kaiser K. Source StatPearls (Internet). Treasure Island (FL) StatPearls Publishing; 2018-2018. Jun 11, Stress Reaction and Fractures. [PubMed] [Google Scholar]
- 12.Kim JW, Oh CW, Oh JK, Park KH, Kim HJ, Kim TS, Seo I, Park EK. Treatment of infra-isthmal femoral fracture with an intramedullary nail: Is retrograde nailing a better option than antegrade nailing? Arch Orthop Trauma Surg. 2018 May 24; doi: 10.1007/s00402-018-2961-6. [DOI] [PubMed] [Google Scholar]
- 13.Calori GM, Colombo M, Mazza EL, Mazzola S, Malagoli E, Marelli N, Corradi A. Validation of the Non-Union Scoring System in 300 long bone non-unions. Injury. 2014;45(Suppl 6):S93–7. doi: 10.1016/j.injury.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 14.Chiavaras MM, Bains S, Choudur H, Parasu N, Jacobson J, Ayeni O, Petrisor B, Chakravertty R, Sprague S, Bhandari M. The Radiographic Union Score for Hip (RUSH): the use of a checklist to evaluate hip fracture healing improves agreement between radiologists and orthopedic surgeons. Skeletal Radiol. 2013;42(8):1079–1088. doi: 10.1007/s00256-013-1605-8. [DOI] [PubMed] [Google Scholar]
- 15.Litrenta J, Tornetta P, Mehta S, et al. Determination of radiographic healing: an assessment of consistency using RUST and modified RUST in metadiaphyseal fractures. J Orthop Trauma. 2015;29(11):516–520. doi: 10.1097/BOT.0000000000000390. [DOI] [PubMed] [Google Scholar]
- 16.Maiettini D, Bisaccia M, Caraffa A, Rinonapoli G, Piscitelli L, Bisaccia O, Rollo G, Meccariello L, Ceccarini P, Rebonato A. Feasibility and Value of Radiographic Union Score Hip Fracture after Treatment with Intramedullary Nail of Stable Hip Fractures. Acta Inform Med. 2016;24(6):394–396. doi: 10.5455/aim.2016.24.394-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhuang H, Li Y, Lin J, Cai D, Cai S, Yan L, Yao X. Cortical thickness in the intertrochanteric region may be relevant to hip fracture type. BMC Musculoskelet Disord. 2017;18(1):305. doi: 10.1186/s12891-017-1669-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ehlinger M, Ducrot G, Adam P, Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res. 2013 May;99(3):353–360. doi: 10.1016/j.otsr.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 19.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006 Aug;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 20.Asencio G. Les fractures de l’extrémité inférieure du fémur. Table ronde de la Sofcot Rev Chir Orthop. 1988;75(Suppl. 1):168–183. [Google Scholar]
- 21.Von Keudell A1, Shoji K, Nasr M, Lucas R, Dolan R, Weaver MJ. J Treatment Options for Distal Femur Fractures. Orthop Trauma. 2016;30(Suppl 2):S25–27. doi: 10.1097/BOT.0000000000000621. [DOI] [PubMed] [Google Scholar]
- 22.Fulkerson E, Koval K, Preston CF, Iesaka K, Kummer FJ, Egol KA. Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plates. J Orthop Trauma. 2006;20(2):89–93. doi: 10.1097/01.bot.0000199119.38359.96. [DOI] [PubMed] [Google Scholar]
- 23.Zlowodzki M, Williamson S, Cole PA, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma. 2004;18:494–502. doi: 10.1097/00005131-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Zlowodzki M, Williamson S, Zardiackas L.D, Kregor P.J. Biomechanical evaluation of the less invasive stabilisation system and the 95-angled blade plate for the internal fixation of distal femur fracture in human cadaveric bones with high bone mineral density. J Orthop Trauma. 2004;60:836–840. doi: 10.1097/01.ta.0000208129.10022.f8. [DOI] [PubMed] [Google Scholar]
- 25.Vallier HA, Immler W. Comparison of the 95-degree angled blade plate and the locking condylar plate for the treatment of distal femoral fractures. J Orthop Trauma. 2012 Jun;26(6):327–332. doi: 10.1097/BOT.0b013e318234d460. [DOI] [PubMed] [Google Scholar]
- 26.Nayak RM, Koichade MR, Umre AN, Ingle MV. Minimally invasive plate osteosynthesis using a locking compression plate for distal femoral fractures. J Orthop Surg (Hong Kong) 2011;19(2):185–190. doi: 10.1177/230949901101900211. [DOI] [PubMed] [Google Scholar]
- 27.Thomson AB, Driver R, Kregor PJ, Obremskey WT. Long-term functional outcomes after intra-articular distal femur fractures: ORIF versus retrograde intramedullary nailing. Orthopedics. 2008 Aug;31(8):748–750. doi: 10.3928/01477447-20080801-33. [DOI] [PubMed] [Google Scholar]
- 28.Kavali C, Agus H, Turgut A. LISS: comparative study of multiply injured and isolated femoral fractures. J Orthop Sci. 2007;12:458–465. doi: 10.1007/s00776-007-1156-8. [DOI] [PubMed] [Google Scholar]
- 29.Markmiller M, Konrad G, Südkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res. 2004 Sep;(426):252–257. doi: 10.1097/01.blo.0000141935.86481.ba. [DOI] [PubMed] [Google Scholar]
- 30.Hierholzer C, von Rüden C, Pötzel T, Woltmann A, Bühren V. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: A retrospective analysis. Indian J Orthop. 2011 May;45(3):243–250. doi: 10.4103/0019-5413.80043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Griffin XL, Parsons N, Zbaeda MM, McArthur J. Cochrane Interventions for treating fractures of the distal femur in adults. Database Syst Rev. 2015;(8):CD010606. doi: 10.1002/14651858.CD010606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gill S, Mittal A, Raj M, Singh P, Singh J, Kumar S. Extra Articular Supracondylar Femur Fractures Managed with Locked Distal Femoral Plate or Supracondylar Nailing: A Comparative Outcome Study. J Clin Diagn Res. 2017;11(5):RC19–RC23. doi: 10.7860/JCDR/2017/25062.9936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoskins W, Sheehy R, Edwards ER, Hau RC, Bucknill A, Parsons N, Griffin XL. Nails or plates for fracture of the distal femur? data from the Victoria Orthopaedic Trauma Outcomes Registry. Bone Joint J. 2016;98-B(6):846–850. doi: 10.1302/0301-620X.98B6.36826. [DOI] [PubMed] [Google Scholar]


