Abstract
Introduction:
Hydrocephalus (HCP) remains one of the commonest pathologies treated in developing countries. Endoscopic third ventriculostomy (ETV) has become the alternative to shunt-divergen procedures in the treatment of many pathologies of the cerebral fluid in the brain. Age has been considered a limitation to perform the procedure, we started to perform ETV In younger patients earlier than many other units. Objectives: In this study, we demonstrate the overall efficacy of ETV in infants younger than 1-year of age and to subsequently report the outcome of this procedure.
Methods:
From 2000 till 2016 we have performed a total of 386 cases of ETV of all ages. 71-cases were infants (below 1-year of age). Our study was undertaken to evaluate these cases. Patients were divided into two subgroups according to the cause of hydrocephalus; obstructive HCP, communicating HCP.
Results:
Mean time for follow up was 52 months. Mean age at surgery was 137days (7- 351days). The population included 31-females and 40-males, while10 infants were premature. Success rates were; 91.6%, 63.6% correspond to each sub-group with an overall success rate of 73.24%.
Conclusion:
ETV in infants is feasible, technically more demanding. Success rate justifies the procedure to be performed in such age group of patients. ETV can be used, attentively, in cases of hydrocephalus associated with MMC, morbidity and mortality does not differ from the general population.
Keywords: ETV, endoscopic fenestration in infant, infants, hydrocephalus
1. INTRODUCTION
Developing countries are facing the greatest burden of pediatric hydrocephalus, there are inadequate data to determine the incidence and prevalence of hydrocephalus(1-10). This liability is related to more health challenges, etiology assumed to correspond to high birth rates, maternal and perinatal risk factors, malnutrition education gaps, also greater risk of untreated neonatal or even prenatal infections and neural tube defects (11-18).
Hydrocephalus (Primary and secondary) remains one of the commonest and devastating pediatric neurosurgical pathologies. The incidence of congenital hydrocephalus has been estimated to be 0.2- 0.8/1000 live births (3). Unique challenges affecting the treatment of hydrocephalus in the developing world include a dominance of post-infectious hydrocephalus, limited resources, and restricted access to neurosurgical care (1).
Even though the insertion of ventriculoperitoneal (VP) shunts has been the pillar of hydrocephalus treatment, VP shunt insertion is associated with high complication and failure rates. On the other hand, over the last few years, endoscopic third ventriculostomy (ETV) has come into picture (7, 19-21). Indications for performing ETV are based on radiological findings that demonstrate a non-communicating type hydrocephalus. Patients with hydrocephalus from aqueductal stenosis are, in general, excellent candidates for ETV. Although controversial, patients less than 6 months of age have not shown uniformly good results with ETV, and most authors do not advocate the procedure in this group (5).
2. AIM
In this study, we demonstrate the overall efficacy of ETV in infants younger than 1 year of age and to subsequently report the outcome of this procedure.3
3. METHODS
A retrospective cohort study was carried out in one of the referral neurosurgical hospitals, the King Hussein Medical Center. The appraised data included socio-demographics of patients, clinical investigations, etiology of hydrocephalus, and postoperative complications. The study includes all consecutive patients who were admitted to our hospital with a diagnosis of hydrocephalus between January 2000, and January 2016. Patients were divided into three subgroups according to the cause of hydrocephalus; obstructive HCP, communicating HCP.
All patients who were older than 1-year, of age or had surgical shunt procedures before the study period started were excluded. Patient charts were revised thoroughly and cases with missing information also were excluded. Postoperative Follow-Up of the patients scheduled at the outpatient clinic 2-weeks after the procedure, 3-months, 6-months and yearly. Monitoring of vital signs, head circumference (HC) measurements, and neurologic examination. After 4-6 weeks interval post-operatively, a radiological evaluation conducted. Postoperative complications observed.
Surgical details
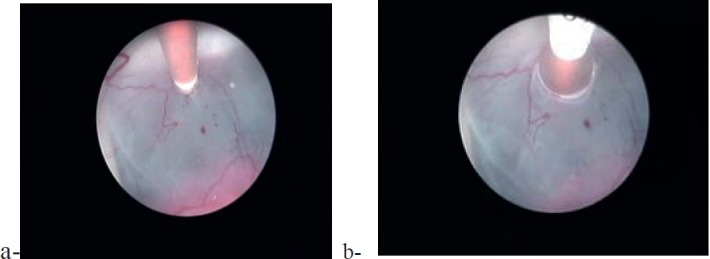
The patient is positioned supine with the head slightly flexed. A coronal burr hole is performed with the optimal entry position at 3 cm lateral to the midline and 1 cm anterior to the coronal suture (Figure 1). The rigid endoscope is advanced into the lateral ventricle. Under direct vision, the endoscope is passed through the foramen of Monro into the third ventricle - the foramen of Monro can be identified by the thalamostriate vein and choroid plexus (Figure 2). The third ventricle is inspected prior to perforation of the floor. The ventriculostomy is placed just posterior to the infundibular recess of the pituitary stalk, anterior to the mammillary bodies. Perforation is either blunt, using the endoscope, or with an instrument followed by balloon catheter dilatation (Figure 3). Entry into the pre-pontine cistern is performed with caution so as to avoid injury to the basilar apex and perforating vessels. Hemostasis with irrigation is achieved until a clear operative field is visualized.
Figure 1. Pre-operative views showing: the skin marking and entry point.
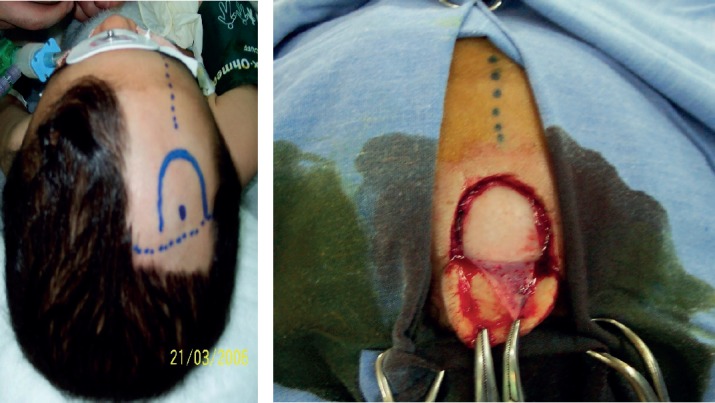
Figure 2. Intraoperative view showing the foramen of Monro, which identified by the thalamostriate vein and choroid plexus.
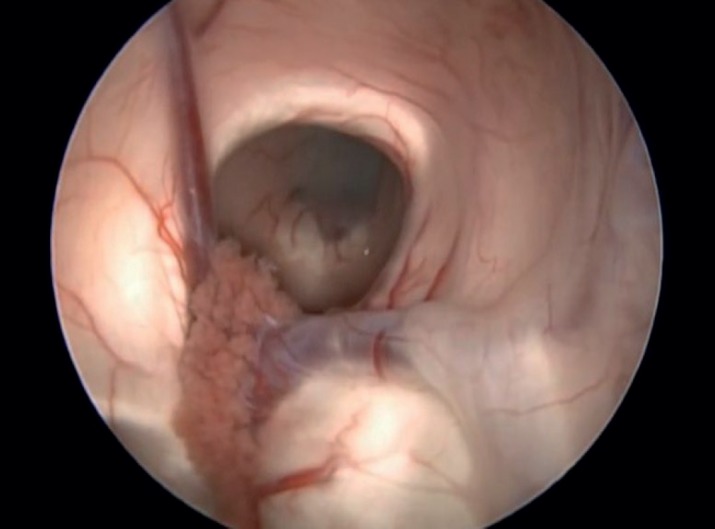
Figure 3. Intraoperative view showing: a) the blunt perforation of the floor of the third ventricle, b) the balloon dilatation.
4. RESULTS
Endoscopic third ventriculostomy was performed in the 386 patients overall in our center in all ages, 71-patients were less than 1-year old. There were no technical difficulties in the procedure even in the cases associated with anatomical distortion of the floor of the third ventricle due to the associated congenital anomalies.
Based on the preoperative radiological imaging, 42-patients (59.15%) diagnosed to have non-communicating (obstructive) hydrocephalus and 29-patients (40.84%) had communicating hydrocephalus, however, in 14-cases HCP associated with MMC.
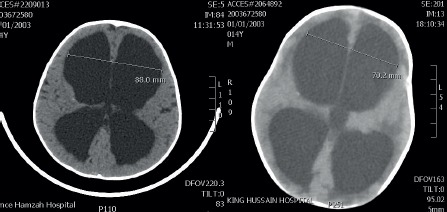
The signs and symptoms of increased intracranial pressure resolved after ETV in all patients. The immediate post-operative period showed complications related to CSF pressure; CSF leak in 3-cases treated with head elevation and pressure dressing, CSF collection in the wound area in 4-cases resolved with a pressure dressing. Four patients developed fever and meningeal irritation signs and symptoms after 3-days from ETV, the external ventricular drain was inserted and antibiotics started for one week. The patient improved, drain removed, patients maintained on antibiotics for another week with no sequels. The initial clinical success rate of one clinical parameter was 84.50% and decreased slightly to 73.24% during long-term follow-up. The size of ventricles showed a reduction in 53-cases (Figure 4). ETV proved successful in the immediate and mid-term control of hydrocephalus.
Figure 4. a) preoperative CT scan, b) postoperative CT scan showing the reduction in ventricular system.
On Long-term follow-up, 19-patients developed symptomatic hydrocephalus which was treated with a Ventriculo-peritoneal shunt, 8 patients had hydrocephalus associated with MMC. There was no deaths nor permanent morbidity related to the procedure.
5. DISCUSSION
Hydrocephalus, a potentially lethal condition, imposes urgent surgical treatment. The routine placement of shunts significantly reduces the overall morbidity and mortality rates (18). Currently, treatment has undergone several paradigm shifts during the past decades. The advantages of improved visualization and minimally invasive neuroendoscopy are precious enhancements to modern neurosurgical conditions’ management. Therefore, neuro-endoscopic procedures have proven to be a reliable and safe alternative to open procedures (9, 13, 16).
The revival of neuroendoscopy can be traced to advancement in optics and computer technology (16).
ETV creates a communication between the ventricular system and subarachnoid spaces at the level of the floor of the third ventricle. The procedure has been shown to offer an acceptable, low-cost, and valid alternative to placement of a permanent shunt in children with obstructive hydrocephalus in developing countries, as well as cases in which hydrocephalus develops following aqua-ductal stenosis. This policy had to surpass a myriad of obstacles which interface the successful set up of neuro-endoscopy service including: steep learning curve, demanding logistic support (12, 14. 22-26).
There are numerous studies now confirming the high success rate and low complication rate of ETV. It is now considered a safe and effective treatment for obstructive hydrocephalus in selected patients (4, 8.11).
Indications for performing ETV are based on computed tomography or magnetic resonance imaging (MRI) findings that demonstrate a non-communicating type hydrocephalus with obstruction at the level of, or distal to, the third ventricle (12-14), 18, 26).
In this analysis diverse causes identified for the cerebrospinal fluid (CSF) pathways occlusion, including: intraventricular hemorrhage 22-patients (30.98%), inflammatory processes in the CSF system 14 patients (19.71%), congenital malformations 29-patients (40.84%), and brain tumors 4 patients (5.63%), Others were 2.81%.
Although controversial, patients less than 6 months of age have not shown uniformly good results with ETV, and most authors do not advocate the procedure in this group. Rationalization due to; immaturity of the CSF re-adsorption pathways, obstruction of the subarachnoid spaces and low intracranial pressure are the main causes of endoscopy failures (5, 12, 15, 17).
An evolving role for endoscopic third ventriculostomy (ETV) in MMC has provoked much debate, due to anatomical variants described. This study shown 14 cases of infants with MMC variants associated with hydrocephalus. All patients demonstrated clinical improvement (in acute/subacute cases) or stabilization (in chronic cases). Eight patients requiring a second surgery. ETV can be used, albeit cautiously, in cases of hydrocephalus associated with MMC. However, the frequency with which anatomical variation is encountered and the difficulty of the assessment of success make the procedure more challenging than usual (20).
Success of ETV has been determined in many publications as; avoiding a shunt in a patient who would otherwise require one. Most authors would classify ETV as successful if a patient later shows clinical evidence of normal intracranial pressure (ICP) and structural evidence of stable or decreased ventricular size (2, 5, 6, 15, 24).
In our current study, we have found a more positive response with ETV for relieving the increased intracranial pressure, the initial overall success rate was 84.50%, principally in the group of patients with non-communicating hydrocephalus. ETV has numerous potential benefits over the standard shunt procedure, which possesses its own set of inherent risks and complications.
Postoperative complications of endoscopic interventions, including both wound complications (CSF leak, meningitis, subdural or subcutaneous accumulation of CSF) and neurological complications (seizures, Injury to the fornix, intraventricular hemorrhage, basilar artery injury, cardiac arrhythmias or respiratory arrest and failed ETV) were observed only in single cases and were transient 4, 5, 19, 27-29). Our study reported the following immediate post-operative complications related to CSF pressure; CSF collection in the wound area in 4 cases resolved with a pressure dressing; in 3 patients CSF leakage developed through the burr hole incision site; treated with a pressure dressing. Four patients with myelomeningocele developed fever and meningeal irritation signs and symptoms after 3-days from ETV, the external ventricular drain was inserted and antibiotics started for one week. The patient improved, drain removed, patients maintained on antibiotics for another week with no sequels. In general, these complications occurred in 15.49% of cases. There was no mortality directly associated with the surgery.
Our work supports the trend adopting the ETV for the management of all cases of symptomatic hydrocephalus in infants and in accordance with the work other authors adopting the same policy concluded (16, 22, 23, 25).
6. CONCLUSION
Neuroendoscopy is a rapidly evolving field combines a high efficacy and a minimal risk of injury, which adheres to the principles of minimally invasive surgery that can be performed on an emergency basis. Despite myriad obstacles which interface the successful set up of neuroendoscopy service, the indications for this technique of neuroendoscopy are swiftly expanding.
ETV in infants is feasible, technically more demanding, success rate justifies the procedure to be performed in such age-group of patients. ETV Eliminates reliance on mechanical shunts with all their limitations, and returns CSF dynamics to essentially normal physiological status in patients with obstructive hydrocephalus. ETV can be used, albeit cautiously, in selected cases of hydrocephalus associated with MMC. Morbidity and mortality do not differ from the general population.
Author’s contribution:
Each author gave substantial contributions to the conception or design of the work in acquisition, analysis, or interpretation of data for the work. Each author had a part in article preparing for drafting or revising it critically for important intellectual content, and each author gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms.
Conflict of interest:
There are no conflicts of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Agrawal A, Sampley S. Spinal dysraphism: A challenge continued to be faced by neurosurgeons in developing countries. Asian journal of neurosurgery. 2014;9(2):68–71. doi: 10.4103/1793-5482.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Algin O, Ucar M, Ozmen E, et al. Assessment of third ventriculostomy patency with the 3D-SPACE technique: a preliminary multicenter research study. J Neurosurg. 2015;122:1347–1355. doi: 10.3171/2014.10.JNS14298. [DOI] [PubMed] [Google Scholar]
- 3.Chi JH, Fullerton HJ, Gupta N. Time trends and demographics of deaths from congenital hydrocephalus in children in the United States: National Center for Health Statistics data, 1979 to 1998. J Neurosurg. 2005;103(2 suppl):113–118. doi: 10.3171/ped.2005.103.2.0113. [DOI] [PubMed] [Google Scholar]
- 4.Cinalli G. Alternatives to shunting. Childs Nerv Syst. 1999;15:718–731. doi: 10.1007/s003810050461. [DOI] [PubMed] [Google Scholar]
- 5.Cinalli G, Saint-Rose C, Chumas P, et al. Failure of third ventriculostomy in the treatment of aqueductal stenosis in children. J Neurosurg. 1999;90:448–544. doi: 10.3171/jns.1999.90.3.0448. [DOI] [PubMed] [Google Scholar]
- 6.Deopujari CE, Karmarkar VS, Shaikh ST. Endoscopic Third Ventriculostomy: Success and Failure. Journal of Korean Neurosurgical Society. 2017;60(3):306–314. doi: 10.3340/jkns.2017.0202.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enger PO, Svendsen F, Wester K. CSF shunt infections in children: experiences from a population-based study. Acta Neurochir (Wien) 2003;145:243–248. doi: 10.1007/s00701-002-1068-5. [DOI] [PubMed] [Google Scholar]
- 8.Fiorillo A, Maggi G, Martone A, et al. Shunt-related abdominal metastases in an infant with medulloblastoma: long-term remission by systemic chemotherapy and surgery. J Neurooncol. 2001;52:273–276. doi: 10.1023/a:1010687121450. [DOI] [PubMed] [Google Scholar]
- 9.Furlanetti LL, Santos MV, De Oliveira RS. The success of endoscopic third ventriculostomy in children: analysis of prognostic factors. Pediatr Neurosurg. 2013;48:352–359. doi: 10.1159/000353619. [DOI] [PubMed] [Google Scholar]
- 10.Griffith HB. Technique of fontanelle and persutural ventriculoscopy and endoscopic ventricular surgery in infants. Childs Brain. 1975;1:359–363. doi: 10.1159/000119587. [DOI] [PubMed] [Google Scholar]
- 11.Hoffman HJ, Hendrick EB. Metastasis via ventriculoperitoneal shunt in patients with medulloblastoma. J Neurosurg. Humphreys RP. 1976;44:462–466. doi: 10.3171/jns.1976.44.5.0562. [DOI] [PubMed] [Google Scholar]
- 12.Hopf N, Grunert P, Fries G, et al. Endoscopic third ventriculostomy: Outcome analysis of 100 consecutive procedures. Neurosurgery. 1999;44:795–804. doi: 10.1097/00006123-199904000-00062. [DOI] [PubMed] [Google Scholar]
- 13.Husain M, Jha D, DK V, et al. Neuro-endoscopic surgery - experience and outcome analysis of 102 consecutive procedures in a busy neurosurgical centre of India. Acta Neurochir. (Wien) 2003;145:369–375. doi: 10.1007/s00701-003-0033-2. [DOI] [PubMed] [Google Scholar]
- 14.Jiménez-León JC, Jiménez CS, Betancourt YM. Neuroendoscopy. Its usefulness in the hydrocephalus management of children in developing countries. Medicina (B Aires) 2007;67(6 Pt 1):665–673. [PubMed] [Google Scholar]
- 15.Kulkarni AV, Sgouros S, Constantini S. International Infant Hydrocephalus Study: initial results of a prospective, multicenter comparison of endoscopic third ventriculostomy (ETV) and shunt for infant hydrocephalus. Child’s nervous system : ChNS: official journal of the International Society for Pediatric Neurosurgery. 2016;32(6):1039–1048. doi: 10.1007/s00381-016-3095-1. [DOI] [PubMed] [Google Scholar]
- 16.Lam S, Harris D, Rocque B, et al. Pediatric endoscopic third ventriculostomy: a population-based study. J Neurosurg Pediatr. 2014;14:455–464. doi: 10.3171/2014.8.PEDS13680. [DOI] [PubMed] [Google Scholar]
- 17.Massimi L, Di Rocco C. Surgical treatment of posthemorrhagic infantile hydrocephalus. Minerva pediatrica. 2013;65(4):417–425. [PubMed] [Google Scholar]
- 18.Muir RT, Wang S, Warf BC. Global surgery for pediatric hydrocephalus in the developing world: a review of the history, challenges, and future directions. Neurosurgical focus. 2016;41(5):E11. doi: 10.3171/2016.7.FOCUS16273. [DOI] [PubMed] [Google Scholar]
- 19.Muszynski CA, Laurent JP, Cheek WR. Effect of ventricular drainage and dural closure on cerebro-spinal fluid leaks after posterior fossa tumor surgery. Pediatr Neurosurg. 1994;21:227–231. doi: 10.1159/000120840. [DOI] [PubMed] [Google Scholar]
- 20.Perez da Rosa S, Millward CP, Chiappa V, et al. Endoscopic Third Ventriculostomy in Children with Myelomeningocele: A Case Series. Pediatric neurosurgery. 2015;50(3):113–118. doi: 10.1159/000381747. [DOI] [PubMed] [Google Scholar]
- 21.Pirotte BJ, Lubansu A, Bruneau M, et al. Sterile surgical technique for shunt placement reduces the shunt infection rate in children: preliminary analysis of a prospective protocol in 115 consecutive procedures. Childs Nerv Syst. 2007;23:1251–1261. doi: 10.1007/s00381-007-0415-5. [DOI] [PubMed] [Google Scholar]
- 22.Raouf A, Zidan I, Mohamed E. Endoscopic third ventriculostomy for post-inflammatory hydrocephalus in pediatric patients: is it worth a try? Neurosurgical review. 2015;38(1):149–155. doi: 10.1007/s10143-014-0582-2. discussion 55. [DOI] [PubMed] [Google Scholar]
- 23.Sainte-Rose C, Cinalli G, Roux FE, et al. Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg. 2001;95:791–797. doi: 10.3171/jns.2001.95.5.0791. [DOI] [PubMed] [Google Scholar]
- 24.Schmitt PJ, Jane JA., Jr A. lesson in history: the evolution of endoscopic third ventriculostomy. Neurosurg Focus. 2012;33(E11) doi: 10.3171/2012.6.FOCUS12136. [DOI] [PubMed] [Google Scholar]
- 25.Valenzuela S, Trellez A. Pediatric neuroendoscopy in Chile. Analysis of the first 100 cases. Childs Nerv Syst. 1999;15:457–460. doi: 10.1007/s003810050439. [DOI] [PubMed] [Google Scholar]
- 26.Warf BC, Tracy S, Mugamba J. Long-term outcome for endoscopic third ventriculostomy alone or in combination with choroid plexus cauterization or congenital aqueductal stenosis in African infants. J Neurosurg Pediatr. 2012;10:108–111. doi: 10.3171/2012.4.PEDS1253. [DOI] [PubMed] [Google Scholar]
- 27.Yadav Y, Parihar V, Kher Y. Complication avoidance and its management in endoscopic neurosurgery. Neurology India. 2013;61(3):217–325. doi: 10.4103/0028-3886.115051. [DOI] [PubMed] [Google Scholar]
- 28.Yadav YR, Parihar V, Pande S, et al. Endoscopic third ventriculostomy. Journal of neurosciences in rural practice. 2012;3(2):163–173. doi: 10.4103/0976-3147.98222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yadav YR, Shenoy R, Mukerji G, et al. Water jet dissection technique for endoscopic third ventriculostomy minimises the risk of bleeding and neurological complications in obstructive hydrocephalus with a thick and opaque third ventricle floor. minimally invasive neurosurgery : min. 2010;53(4):155–158. doi: 10.1055/s-0030-1263107. [DOI] [PubMed] [Google Scholar]


