Abstract
Introduction:
To the best of our knowledge, this is the first study about malignant eyelid tumors in the region of Tuzla, Bosnia and Herzegovina, and it shows similar results comparing with other countries (the annual incidence of eyelid tumors in Tuzla region is about 3.73/100 000 population). Malignant eyelid tumors are relatively uncommon, but potentially fatal disease. However, if detected early and treated adequately, the prognosis is generally excellent.
Aim:
The aim of this study was the clinical and microscopical analysis of malignant eyelid tumors in treated patients, the presentation of surgical treatment and reconstructive methods of eyelid tumors.
Methods:
This retrospective study included 60 patients surgically treated at the University Clinical Center Tuzla from January 2012 to December 2016, who were initially diagnosed with malignant eyelid tumors in accordance to the final results obtained by histological examination of excised lesions.
Results:
In the group of malignant tumors, the most common tumors were BCC (85%), which were predominantly found on the lower eyelids (92.16%) and showed female predominance (51.06%). SCC was the second most common eyelid malignancy (15%) and showed a predilection for the lower eyelid involvement and male predominance (55.56%). Tumors up to 2 cm in diameter (clinical stage T1) were found in 78.33% of cases, 95.74% of which with radical excision, while 4.26% with non-radical excision.
Conclusion:
Treatment by complete excision with histological confirmation of tumor clearance is recommended. Perineural spread is an adverse prognostic sign, which may require postoperative radiotherapy. Orbital invasion is a rare complication but, if recognized early, it can be treated effectively with exenteration. Because presentation varies and histological examination is required for accurate diagnosis, any suspicious lesion occurring on the eyelids should be excised or biopsied. All patients with malignant tumors should be advised of the risk of recurrent or new tumors and encouraged to attend lifelong follow up.
Keywords: Malignant Eyelid tumors, histological confirmation, clearance, tumor excision
1. INTRODUCTION
Basal cell carcinoma (BCC) is generally a slow-growing tumor for which metastases is rare, occurring in only 0.5 percent or less of cases (1). Despite the fact that this malignancy is rarely fatal, BCC can be highly destructive and disfiguring to local tissues when presentation is delayed or treatment is inadequate. Clinically, BCCs usually appear as flesh or pink colored pearly papules and occur on the head or neck in 85 percent of cases, 20% of which occur on the eyelids (2). Tumor typically occurs at the age of 60-80. Although metastasis is rare, BCC of the eyelids has a high risk of recurrence. BCC is usually not fatal, but if it is not diagnosed for a long time, the function and the appearance of the eyelid will be destroyed (3). BCC treatment involves surgical modalities such as electrodessication and curettage (EDC), excision, cryosurgery, and Mohs micrographic surgery. Such methods are typically reserved for localized BCC and offer high 5-year cure rates in generally over 95 percent of cases (4–5).
Squamous cell carcinoma (SCC) is an invasive epithelial malignancy showing keratinocytic differentiation. It is the second most common malignant neoplasm of the eyelids (6), comprising 5-10% of all eyelid malignancies. The incidence for eyelid SCC has been reported to be between 0.09 and 2.42 of cases per 100 000 population (7). Intrinsic risk factors include albinism, pre-existing chronic skin lesions and genetic skin disorders such as xeroderma pigmentosum and epidermodysplasia verruciformis. Eyelid SCC is a relatively uncommon, but potentially fatal disease. It is responsible for considerable morbidity; however, if detected early and treated adequately, the prognosis is generally excellent and death and disability can be reduced. The clinical presentation varies and histological examination is required for accurate diagnosis. Because of the significant morbidity of these lesions and in order to better define the clinical features and treatment outcomes and to make management recommendations, we conducted a review of all malignant eyelid tumors treated over a five-year period.
2. AIM
The aim of this study was the clinical and microscopical analysis of malignant eyelid tumors in treated patients, the presentation of surgical treatment and reconstructive methods of eyelid tumors.
3. METHODS
This retrospective study included 60 patients surgically treated at the University Clinical Center Tuzla from January 2012 to December 2016, who were initially diagnosed with malignant eyelid tumors in accordance to the final results obtained by histological examination of excised lesions. The most common eyelid malignancy was BCC, followed by SCC. It is a retrospective study during which patient’s medical history was used for acquiring general data, as well as data on clinical findings, diagnostic procedures and surgical treatment. Following variables were analyzed: general patient data, age, gender; clinical findings: characteristics of suspected lesion (anatomical localization and size), and radical excision of tumor. Proper diagnosis was based on adequate biopsy and pathohistological verification of tumor. All the necessary macro and micro analyses of surgically obtained samples were done at the Pathology polyclinic for laboratory diagnostics of University Clinical Center in Tuzla. All the tissue specimens were formaldehyde fixed and paraffin wax embedded. Histological cuts were stained with hematoxilineosin. Immunohistochemical staining was performed on 5 μm tissue sections that were placed on organosilane pretreated glass slides. We used descriptive statistics to calculate the arithmetic means, absolute and relative frequencies, and incidence. Ethical approval for the study was obtained from the Ethics Committee at University Clinical Center Tuzla, Bosnia and Herzegovina.
4. RESULTS
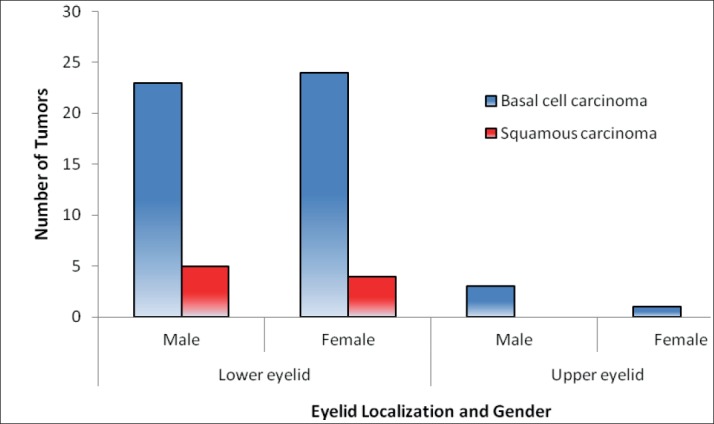
Patient ages ranged from 45 to 90 years, with a mean age of 67,57 years. Patients were male 31 and 29 were female. The demographic data of malignant eyelid tumors are summarized in Table 1. In the group of malignant tumors, the most common tumors were BCC (85%), which were predominantly found on the lower eyelids (92.16%) and showed female predominance (51.06%). SCC was the second most common eyelid malignancy (15%) and showed a predilection for the lower eyelid involvement and male predominance (55.56%) (Graph 1). Tumors up to 2 cm in diameter (clinical stage T1) were found in 78.33% of cases, 95.74% of which with radical excision, while 4.26% with non-radical excision.
Graph 1. Distributions of malignant eyelid tumors in Tuzla region from 2012 to 2016.
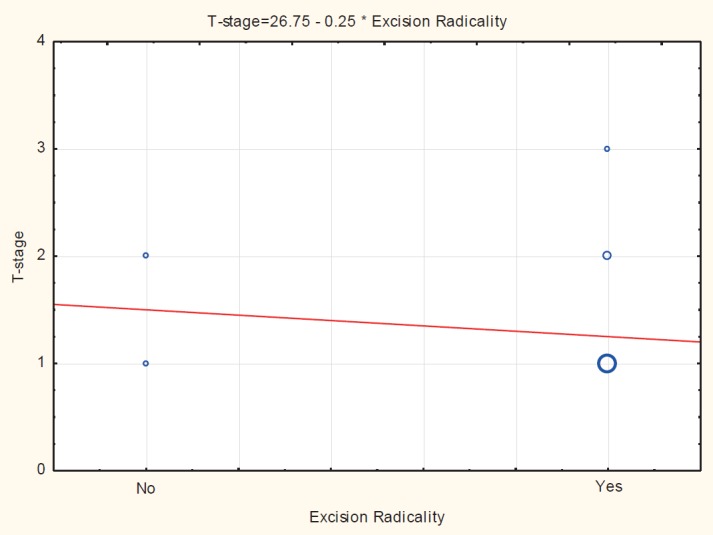
Tumors from 2 to 5 cm (clinical stage T2), found in 21.66% of cases (Graph 2), present very large tumors, the excision of which necessarily involves large tissue defects. Radicality of excision was poor in 16.67% cases.
Graph 2. Correlation between size of tumors and excision radicality.
5. DISCUSSION
Eyelid skin is not only the thinnest skin of the body but also among the most common sunlight-exposed areas of skins. Apart from subcutaneous fat layer, eyelid contains all other skin structures that can be the origin of various malignant tumors. Eyelid tumors could be cosmetically disturbing to patients as well as diagnostically difficult for family physicians, dermatologists, and ophthalmologists (8-11). Approximately 5% to 10% of all skin cancers occur in the eyelid. Incidence studies indicate that BCC is the most frequent malignant eyelid tumor, followed by SCC, sebaceous gland carcinoma, and malignant melanoma. Many therapeutic methods have been suggested to combat the morbidity and mortality associated with these lesions (7).
A largest reported study in Europe for the frequencies of eyelid tumors was published in Switzerland (8) with a total of 5504 cases. In this study, the most common eyelid malignancy was BCC (80.95%), followed by SCC (14.29%). In the research conducted by Huang and al. (12) the most common tumors were BCC (57.8%), which were predominantly found on the lower eyelids (78.3%) and in male patients (68.7%), SCC was the third most common eyelid malignancy (10.1%) and showed a male predominance (69.6%). According to histological analysis of the examined samples in our study, the highest number of tumors was BCC (85%), which were predominantly found on the lower eyelids (92.16%) and showed female predominance (51.06%). SCC was the second most common eyelid malignancy (15%) and showed a predilection for the lower eyelid involvement and male predominance (55.56%). Malignant lid tumors tended to locate in the lower eyelid, which could be attributed to most BCC with a predilection for the lower eyelid.
Eyelid reconstruction should be carefully considered as both function and aesthetic outcomes are important after clear excision of tumors. Exenteration is considered in the case of extensive orbital invasion or high-risk aggressive tumors in order to reduce the rate of recurrence. Eyelid tumors are common in clinical practice. Postoperative defects are often complex to treat, as the reconstruction must be functionally satisfying and aesthetically flawless. During clinical examination of a patient, one should clarify whether it is an inflammatory process or malignant tumor, as in certain cases clinical features are very similar.
Previously described eyelid tumors are very common in practice. They are predominantly present in patients who were exposed to long-term ultraviolet radiation. From the aspect of reconstruction, the resulting defect on one of the mentioned regions after the tumor excision often presents a complex problem. If the resection of all eyelid structures has been performed, it is necessary to reconstruct the same ad integrum. Smaller defects are reconstructed by skin grafts from adequate donor place, while larger defects are reconstructed by local flaps (Figures 1-4). It should especially be pointed out that the radicality of excision during the operative procedure itself should be pathohistological verified, just before the immediate reconstruction. Having in mind the specificity of the region, its deeper structure, it is clear that each mistake in the procedure as well as the tumors in advanced stadium can have very bad consequences for the health of the patient. The highest number of diagnosed skin tumors in both genders was in clinical stage I (78.33%), and clinical stage II (21.66%), which is in accordance to data obtained during a study that was done in Turky, where 78% of skin tumors was verified in clinical stage I, with maximal diameter measuring 20 mm (13). Tumors with sizes 2-5cm in diameter (T2) are large tumors where excision almost always results in large tissue defects. Radicality of excision was poor in 16.67% cases, which is high percentage. Bearing in mind the specificity of this region, poor excision should be treated, as recurrences in this region have a high risk of eye loss. Analyzing the radicality of excision in each T stadium we can see that in this region excision was radical in 93.33% of cases, while it was non-radical in 6.67% of cases. Many different studies throughout the world also present similar results. In the research conducted by Zielinski and al. (14) histopathological verification of tumor margins revealed incomplete excision in 14.7% patients, and study of Huang and al. (12) 9.7% patients was required advanced orbital exenteration or enucleation.
Figure 1. BCC of upper and lower eyelid.

Figure 3 and 4. Radically excised BCC with reconstructive procedure planned.

We believe that this result emerges from the fact that patients usually come for medical help too late and when the disease has already advanced. When it comes to large tumors with infiltration of deeper structures and organs, excision is better as those cases involve large mutilant surgeries in which eye as an organ is not spared but rather removed. Therefore, orbital exenteration or hemifacialectomy with or without resection of the bone part is done. The integrity of the eyelids is important for protecting and preserving the function of the globe. The distance of the tumor from the eyelid margin and the diameter of the tumor are important to estimate the prognosis and choose the best surgical technique.
When the tumor affects the margin of the eyelid, reconstruction with a flap based on the tumor size in the eyelid is necessary to preserve eyelid function and aesthetics. The aim of surgery is to excise the entire tumor (margins >3 mm outside the tumor) and reestablish eyelid functionality and aesthetics. The United Kingdom (UK) National Multidisciplinary Guidelines recommend that non-infiltrative BCCs <2 cm should be excised with a margin of 4–5 mm. Smaller margins (2–3 mm) may be taken in case of limited reconstructive options (15). The involvement of the eyelid margin makes surgical reconstruction more difficult. The smaller the size of the tumor, the simpler the reconstruction, and better functional and aesthetic results are obtained (16).
6. CONCLUSION
To the best of our knowledge, this is the first study about malignant eyelid tumors in the region of Tuzla, Bosnia and Herzegovina, and it shows similar results comparing with other countries (the annual incidence of eyelid tumors in Tuzla region is about 3.73/100 000 population). Malignant eyelid tumors are relatively uncommon, but potentially fatal disease. However, if detected early and treated adequately, the prognosis is generally excellent. Treatment by complete excision with histological confirmation of tumor clearance is recommended. Perineural spread is an adverse prognostic sign, which may require postoperative radiotherapy. Orbital invasion is a rare complication but, if recognized early, it can be treated effectively with exenteration. Because presentation varies and histological examination is required for accurate diagnosis, any suspicious lesion occurring on the eyelids should be excised or biopsied. All patients with malignant tumors should be advised of the risk of recurrent or new tumors and encouraged to attend lifelong follow up. Prevention remains of prime importance in minimizing the morbidity and mortality of these lesions.
Figure 2. Postoperative result.

Author’s contribution:
M.B, E.I, A.N.V gave a substantial contribution to the conception and design of the work. M.B, A.R gave a substantial contribution of data. A.M, M.H, M.S, gave a substantial contribution to the acquisition, analysis, or interpretation of data for the work. M.B, E.I, A.N.V, M.B, A.R had a part in article preparing for drafting or revising it critically for important intellectual content. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms..
Conflicts of interest:
There are no conflicts of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Lo JS, Snow SN, Reizner GT. Metastatic basal cell carcinoma: report of twelve cases with a review of the literature. J Am Acad Dermatol. 1991;24(5):715–719. doi: 10.1016/0190-9622(91)70108-e. [DOI] [PubMed] [Google Scholar]
- 2.Kyrgidis A, Vahtsevanos K, Tzellos TG. Clinical, histological and demographic predictors for recurrence and second primary tumours of head and neck basal cell carcinoma. A 1062 patient-cohort study from a tertiary cancer referral hospital. Euro J Dermatol. 2010;20(3):276–282. doi: 10.1684/ejd.2010.0903. [DOI] [PubMed] [Google Scholar]
- 3.Sun MT, Wu A, Huilgol SC, Selva D. Accuracy of biopsy in subtyping periocular basal cell carcinoma. Ophthal Plast Reconstr Surg. 2015;31(6):449–451. doi: 10.1097/IOP.0000000000000372. [DOI] [PubMed] [Google Scholar]
- 4.Chren MM, Linos E, Torres JS. Tumor recurrence 5 years after treatment of cutaneous basal cell carcinoma and squamous cell carcinoma. J Invest Dermatol. 2013;133(5):1188–1196. doi: 10.1038/jid.2012.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silverman MK, Kopf AW, Bart RS. Recurrence rates of treated basal cell carcinomas. Part 3: Surgical excision. J Dermatol Surg Oncol. 1992;18(6):471–476. doi: 10.1111/j.1524-4725.1992.tb03307.x. [DOI] [PubMed] [Google Scholar]
- 6.Reifler DM, Hornblass A. Squamous cell carcinoma of the eyelid. Surv Ophthalmol. 1986;30:349–365. doi: 10.1016/0039-6257(86)90089-5. [DOI] [PubMed] [Google Scholar]
- 7.Cook BE, Bartley GB. Epidemiologic characteristics and clinical course of patients with malignant eyelid tumours in an incidence cohort in Olmsted County, Minnesota. Ophthalmology. 1999;106:746–750. doi: 10.1016/S0161-6420(99)90161-6. [DOI] [PubMed] [Google Scholar]
- 8.Deprez M, Uffer S. Clinicopathological features of eyelid skin tumors. A retrospective study of 5504 cases and review of literature. The American Journal of Dermatopathology. 2009;31(3):256–262. doi: 10.1097/DAD.0b013e3181961861. [DOI] [PubMed] [Google Scholar]
- 9.Sotiropoulos G, Gartzios C, Raggos V, et al. Eyelid tumors at the university eye clinic of Ioannina, Greece: a 30-year retrospective study. Middle East African Journal of Ophthalmology. 2015;22(2):230–232. doi: 10.4103/0974-9233.151881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gundogan FC, Yolcu U, Tas A, et al. Eyelid tumors: clinical data from an eye center in Ankara, Turkey. Asian Pacific Journal of Cancer Prevention. 2015;16(16):4265–4269. doi: 10.7314/apjcp.2015.16.10.4265. [DOI] [PubMed] [Google Scholar]
- 11.Ho M, Liu DTL, Chong KKL, Ng HK, Lam DSC. Eyelid tumours and pseudotumours in Hong Kong: a ten-year experience. Hong Kong Medical Journal. 2013;19(2):150–155. [PubMed] [Google Scholar]
- 12.Huang YY, Liang WY, Tsai CC, Kao CS, et al. Comparison of the Clinical Characteristics and Outcome of Benign and Malignant Eyelid Tumors: An Analysis of 4521 Eyelid Tumors in a Tertiary Medical Center. BioMed Research International. 2015;8:160–165. doi: 10.1155/2015/453091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ceylan C, Ozturk G, Alper S. Non-Melanoma skin cancers between the years of 1990 and 1999 in Izmir, Turkey: demographic and clinico-pathological characteristics. J Dermatol. 2003;30(2):23–131. doi: 10.1111/j.1346-8138.2003.tb00359.x. [DOI] [PubMed] [Google Scholar]
- 14.Zielinski T, Pisera P, Siewiera I, Sporni S, Iljin A. Surgical treatment of malignant eyelid tumors. Pol Merkur Lekarski. 2013;34(202):214–218. [PubMed] [Google Scholar]
- 15.Newlands C, Currie R, Memon A, Whitaker S, Woolford T. Non-melanoma skin cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130(2):125–132. doi: 10.1017/S0022215116000554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pfeiffer MJ, Pfeiffer N, Valor C. Estudio descriptivo sobre el carcinoma basocelular en el párpado. Descriptive study on basal cell eyelid carcinoma. Arch Soc Esp Oftalmol. 2015;90(9):426–431. doi: 10.1016/j.oftal.2014.12.001. [DOI] [PubMed] [Google Scholar]


