Abstract
Introduction:
Malocclusion as an oral disorder can cause negative impact on individuals oral conditions, social interactions and self-esteem.
Aim:
The aim of this study was to compare oral health-related quality of life (OHQoL) of patients who had received fixed orthodontic treatment and patients who had not received fixed orthodontic treatment.
Materials and Methods:
Data were collected from 178 participants attended at professional dental office (mean age 22.71 years) in two groups (experimental and control). The experimental group comprised of 90 subjects who were in the retention phase, after their orthodontic treatment, and the control group comprised of 88 untreated subjects. Oral Health Impact Profile (OHIP-14) was used to assess the patients oral health related quality of life (OHQoL).
Results:
The control group had significantly higher OHIP-14 scores than experimental group (p < 0.001). Participants with treatment need reported a significantly greater negative impact on the overall OHRQoL score.
Conclusion:
Subjects with no history of orthodontic treatment had more negative oral health related quality (OHRQoL), than subjects who had completed orthodontic treatment. Dental malocclusion has significant negative impact on OHRQoL.
Keywords: Oral Health Impact Profile (OHIP), Oral health related quality of life (OHQoL), Orthodontic treatment
1. INTRODUCTION
Malocclusion as an oral disorder is highly prevalent and can unfavorably affect social, physical and psychological well-being of patients (1-3). Malocclusion can impair the quality of life in many people and affect various aspects of life, including function, appearance, and interpersonal relationships (4). Various types of orthodontic appliances are used to treat dental malocclusions, and need for orthodontic treatment in dental clinics is evaluated using certain measures, like index of orthodontic treatment need (IOTN), proposed by Brook and Shaw.(5) The Index of Orthodontic Treatment Need (IOTN) is a scoring system for malocclusion, which has been used extensively in the literature to evaluate actual and perceptive orthodontic treatment needs (6, 7). Traditionally, clinicians and researchers have been focused on the clinically based measures of outcome for orthodontic treatment, like IOTN index. But in recent years, researchers have been more oriented to patient based assessment of oral health status to better understand their needs and satisfaction with treatment (8, 9). Oral health-related quality of life is a concept that includes subjective evaluation of perceived physical, psychological , and social aspects of oral health. Oral Health Impact Profile (OHIP) questionnaire developed by Slade and Spencer in 1994 and short form OHIP-14 modified by Slade in 1997 has been found reliable and widely accepted for assessment of oral health-related quality of life in individuals with malocclusion (10). The original version of the OHIP scale includes 49 items that are divided into 7 domains. Because of the extensiveness of original form, shortened version of only 14 items of OHIP questionnaire was developed (11). The oral health-related quality of life (OHRQoL) provide an insight into how individual’s oral health status affects overall quality of life (QoL) (12-14). In spite of the fact that orthodontic treatment improves oral function, appearance and social well- being of the patients, some researchers didn’t find any significant relationship between orthodontic treatment of malocclusion and oral health related quality of life (15,16) Large number of the studies found a relationship between orthodontic treatment of malocclusion and OHQoL. Oliveira and Sheiham in their study concluded that oral-health quality of life of Brazilian adolescents was significantly improved after they completed orthodontic treatment compared to those who hadn’t received orthodontic treatment (17). Leao and Sheiham reported that young patients who had undergone orthodontic treatment had a better quality of life compared to those who had not undergone such a treatment (18). Zhang at al. concluded that orthodontic treatment significantly improved quality of life of their patients 6 months after orthodontic treatment (19).
2. AIM
The aim of this study was to compare oral health-related quality of life (OHQoL) of patients who had receive fixed orthodontic treatment and patients who had not received fixed orthodontic treatment
3. MATERIALS AND METHODS
Data were collected from 178 participants attended at professional dental office (mean age 22.71 years) in two groups (experimental and control). The experimental group comprised of 90 subjects who were in the retention phase, after their orthodontic treatment, and the control group comprised of 88 untreated subjects. The patients in experimental group were selected from the patients who were already referred to a private orthodontic clinic and had received fixed orthodontic treatment. The control group subjects were selected from patients who had been referred to the same private clinic and were candidates for orthodontic treatment. The patients with a history of maxillofacial surgeries, any systemic diseases or mental problems were excluded from the study. The selected subjects were informed about the study, and written informed consent was obtained from patients and parents of the participants. Oral Health Impact Profile (OHIP-14) was used to assess the patients oral health related quality of life (OHQoL). OHIP-14 consists of 14 questions, which measures the quality of life in seven fields of functional limitations, physical problems, mental and emotional problems, physical handicaps, mental and emotional handicaps, social handicaps and complete handicap. An OHIP- 14 (Oral Health Impact Profile-14) questionnaire was filled out for all the study parts in one session in the form of an interview. The subject’s answers were scored in the Lickert’s scale a “zero” for “never”, “1” for “seldom”, “2” for“ sometimes”, “3” for “mostly” and “4” for “almost always”. On the whole, a score ranging between “0” and “56” is calculated for each subject. Higher OHIP scores indicate worse and lower scores indicate better oral health-related quality of life for the subjects.
Patients treatment needs were categorized with Index of Treatment Need (IOTN).
Statistical analysis
The collected data was analyzed using IBM Statistics SPSS version 25.0. For comparing percentages of the IOTN Pearson’s Chi square test was used. For OHIP-14, the descriptive statistics; mean and standard deviation were calculated and Mann Whitney U test was used to compare ranks for OHIP-14 among the experimental and control group. The correlation between the OHIP-14 and the IOTN was measured using the Spearman’s rank correlation coefficients.
4. RESULTS
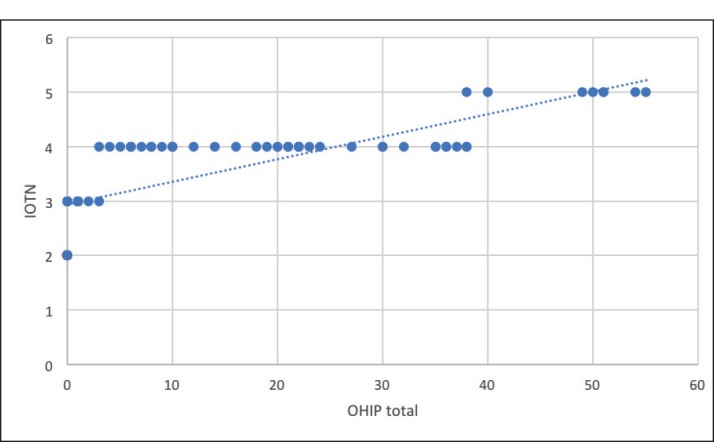
The comparison of the IOTN between the treated and non-treated subjects indicate that the majority of subjects in both groups had IOTN grade 4, followed in frequency by IOTN grade 2, and the least frequency of subjects in both groups with IOTN grade 5. (Table 1) Statistical analysis using chi-square test indicate that there is no statistically significant difference in IOTN among the observed groups (p>0.05) (Graph 1) Malocclusion significantly affected all domains of OHIP-14. The total OHIP-14 score was significantly lower (0.41 : 13.59) in the experimental group compared to control group. (Graph 2) Subjects in control group had significantly higher OHIP-14 mean rank scores than subjects who had completed orthodontic treatment, in experimental group. Comparison of mean ranks between the observed groups confirms the above mentioned statement with highly significant differences at all subscales of the OHIP-14 (app p<0.01). (Table2) Correlation analysis using the Spearman’s rank correlation coefficient indicate highly significant (p<0.05) correlation between the all sub domains and the total OHIP-14 and the IOTN score in both observed groups. (Table 3) Meaning that the IOTN truly reflect the QOL measured by the OHIP-14 questionnaire. In control group, it was observed that patients with high treatment need (grade 4 and 5) according to IOTN, had the highest OHIP-14 score. (Table 4), (Graph 3) Correlation analysis using the Spearman rank correlation coefficient indicate highly significant (p<0.05) correlation between the all sub domains and the total OHIP-14 and the IOTN score in control group. Meaning that the IOTN truly reflect the oral-health related quality of life measured by the OHIP-14 questionnaire for this group.
Table 1. Comparison of IOTN between the treated and non-treated subjects. χ2=0,611; p=0,894.
| IOTN – Index of treatment need * Group Crosstabulation | |||||
|---|---|---|---|---|---|
| Group | Total | ||||
| Experimental group | Control group | ||||
| IOTN – Index of treatment need | Grade 2–Little treatment need | Count | 12 | 11 | 23 |
| % | 13,3 | 12,5 | 12,9 | ||
| Grade 3–Moderate treatment need | Count | 25 | 29 | 54 | |
| % | 27,8 | 33,0 | 30,3 | ||
| Grade 4–Great treatment need | Count | 45 | 40 | 85 | |
| % | 50,0 | 45,5 | 47,8 | ||
| Grade 5–Very great treatment need | Count | 8 | 8 | 16 | |
| % | 8,9 | 9,1 | 9,0 | ||
| Total | Count | 90 | 88 | 178 | |
| % | 100,0 | 100,0 | 100,0 | ||
Figure 1. Comparison of IOTN between the experimental and control group.
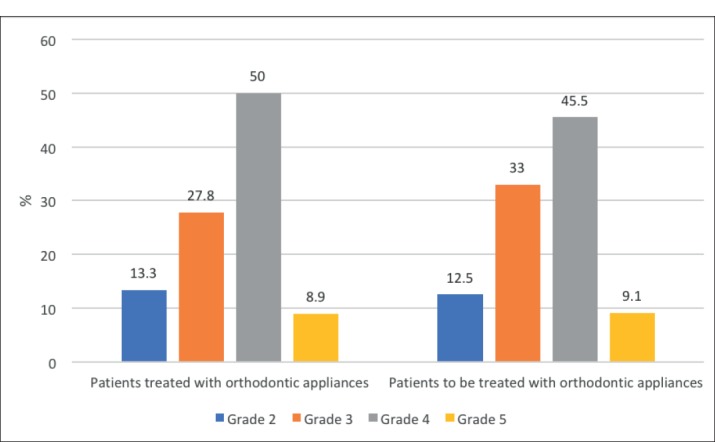
Figure 2. Comparison of OHIP-14 score between the subjects who received and who had not received treatment.
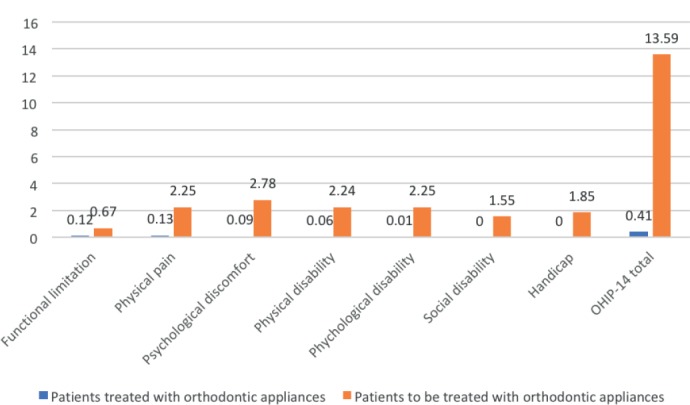
Table 2. Comparison of mean ranks between the observed groups.
| Ranks | |||||
|---|---|---|---|---|---|
| Group | N | Mean Rank | Sum of Ranks | p | |
| Functional limitation | Experimental group | 90 | 82,09 | 7388,50 | 0,002 |
| Control group | 88 | 97,07 | 8542,50 | ||
| Physical pain | Experimental group | 90 | 69,27 | 6234,50 | 0,0001 |
| Control group | 88 | 110,19 | 9696,50 | ||
| Psychological discomfort | Experimental group | 90 | 56,41 | 5077,00 | 0,0001 |
| Control group | 88 | 123,34 | 10854,00 | ||
| Physical disability | Experimental group | 90 | 67,43 | 6069,00 | 0,0001 |
| Control group | 88 | 112,07 | 9862,00 | ||
| Psychological disability | Experimental group | 90 | 66,27 | 5964,50 | 0,0001 |
| Control group | 88 | 113,26 | 9966,50 | ||
| Social disability | Experimental group | 90 | 72,50 | 6525,00 | 0,0001 |
| Control group | 88 | 106,89 | 9406,00 | ||
| Handicap | Experimental group | 90 | 64,50 | 5805,00 | 0,0001 |
| Control group | 88 | 115,07 | 10126,00 | ||
| OHIP-14 total | Experimental group | 90 | 57,83 | 5204,50 | 0,0001 |
| Control group | 88 | 121,89 | 10726,50 | ||
Table 3. Correlation analysis for both observed groups.
| Correlations | |||
|---|---|---|---|
| IOTN – Index of treatment need | |||
| Spearman’s rho | IOTN – Index of treatment need for both groups | Correlation Coefficient | 1,000 |
| Sig. (2-tailed) | . | ||
| N | 178 | ||
| Functional limitation | Correlation Coefficient | ,528** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| Physical pain | Correlation Coefficient | ,616** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| Psychological discomfort | Correlation Coefficient | ,436** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| Physical disability | Correlation Coefficient | ,548** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| Psychological disability | Correlation Coefficient | ,521** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| Social disability | Correlation Coefficient | ,446** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| Handicap | Correlation Coefficient | ,492** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| OHIP-14 total | Correlation Coefficient | ,507** | |
| Sig. (2-tailed) | ,000 | ||
| N | 178 | ||
| **. Correlation is significant at the 0.01 level (2-tailed). | |||
Table 4. Correlation analysis for the control group (non-treated subjects).
| Correlations | |||
|---|---|---|---|
| OHIP-14 total | |||
| Spearman’s rho | OHIP-14 total | Correlation Coefficient | 1,000 |
| Sig. (2-tailed) | . | ||
| N | 88 | ||
| IOTN – Index of treatment need for Control group | Correlation Coefficient | ,924** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| Functional limitation | Correlation Coefficient | ,755** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| Physical pain | Correlation Coefficient | ,947** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| Psychological discomfort | Correlation Coefficient | ,994** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| Physical disability | Correlation Coefficient | ,951** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| Phychological disability | Correlation Coefficient | ,954** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| Social disability | Correlation Coefficient | ,885** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| Handicap | Correlation Coefficient | ,963** | |
| Sig. (2-tailed) | ,000 | ||
| N | 88 | ||
| **. Correlation is significant at the 0.01 level (2-tailed). | |||
Figure 3. Correlation of IOTN and OHIP-14 results in control group.
5. DISCUSSION
In today’s practice, clinicians are those who place much more emphasis on patient-based evaluation of their oral health status. Clinical indicators such as Index of treatment need (IOTN) cannot describe the satisfaction of patients seeking treatment. Oral health-related quality of life (OHRQOL) is considered to be the best measurement for orthodontic treatment need and should be a part of the evaluation of oral health status in orthodontic patients (11, 12). High prevalence of malocclusion and dental deformities in population can have a negative impact on physical, social and psychological functioning of the individuals (2, 3). With treatment of malocclusion it is possible to improve function, facial appearance and dental aesthetics. Patient’s reported motivation to seek a treatment are commonly related to functional and aesthetic reasons, or to self esteem and self-confidence, although the percentages of patients reporting these motives have a great variation in different studies (20, 21, 22). The present study assessed the quality of life as related to the oral health (OHQoL), among the patients who had received and those who wished to receive fixed orthodontic treatment. In our study, it was found that patients who received orthodontic treatment had significantly improved oral health-related quality of life (OHRQoL). Our study was in consistence with study of Palomares et al. who found that adults who had completed orthodontic treatment and were in the retention phase of treatment, had better OHRQoL than non-treated subjects who were waiting for treatment (23). Chen et al. who followed 250 Chinese orthodontic patients showed that their OHQoL was better after they completed treatment than before or during orthodontic treatment.(24). Bernabe at al. in their study concluded that Brazilian adolescents who had undergone orthodontic treatment had less physical, psychological, and social complications associated with malocclusion in comparison with those who had no history of orthodontics (25). On the contrary, Taylor et al. in their investigation didn’t find any significant relationship between the orthodontic treatment and changes in the quality of life (15). A systematic review by Dimberg L et al. indicate that malocclusions basically have negative effects on OHRQoL, in the dimensions of emotional and social well being (26). In comprehensive systematic review and meta-analysis Andiappan M et al. reported that individuals who received treatment for malocclusion and individuals who didn’t have need for orthodontic treatment had significantly lower OHIP-14 scores, compared to those who needed orthodontic treatment (27). Also, previous studies reported that OHRQoL can be deteriorated, with the increase in severity of malocclusion (28, 29, 30). The greatest improvement of oral health quality of life (OHQoL) was observed in patients who needed treatment that combines orthodontics and orthognathic surgery (31, 32, 33). In our study, in control group (subjects waiting for orthodontic treatment) the highest score on the OHIP-14 scale, had the patients with high treatment need, according to IOTN. Majority of these patients comprised of those who needed combined orthodontic-surgical approach and of patients with signs and symptoms of TMD. The findings of this study agreed with previous studies reporting that malocclusion can cause pain indirectly, by leading to temporomandibular disorders (34, 35). In the study, high correlation between all domains and the total OHIP-14 and the IOTN score in both groups, showed that IOTN truly reflected the QoL measured by the OHIP-14 questionnaire. Although, all domains of OHRQoL were affected, the most significantly affected domains were psychological discomfort, psychological disability and physical pain. Similar to our study, Chen M et al. reported that malocclusion had a significantly negative impact on OHRQoL and that mostly affected domains were psychological discomfort and psychological disability (24). Previous studies also, indicate a strong association between malocclusion and psychological discomfort and disability (36, 37, 38). These findings support the assumption that with correction of orofacial deformities and improvement of patient’s oral function and aesthetics, we consequently exert positive effect on patient’s psychological and social well-being. Correction of dental malocclusion improves oral health-related quality of life in general. This study has shown that subjects who were waiting for orthodontic treatment had more negative OHRQoL of life, than subjects who received orthodontic treatment. Based on study results, it can be concluded that an OHRQoL is very useful tool for assessment of orthodontic treatment needs and consequent improvement of quality of life.
Limitations: One of the limitations was that were no pretreatment assessment of OHRQoL of treated patients and also the study should be done on overall population, so we can exclude possible bias. Also, sample size was limited, and in future individuals with larger sample are needed to undeceive the correlation between malocclusion and treatment needs.
6. CONCLUSION
Malocclusion has a significant negative impact on OHRQoL and its domains. Subjects with no history of orthodontic treatment had significantly worse OHIP-14 score, than subjects who had completed orthodontic treatment. There was significant association between mean overall OHIP-14 score and high orthodontic treatment need (Grade 4 and 5) in non-treated group.
Author’s contribution:
Each author gave substantial contribution to the conception or design of the work and in the acquisition, analysis and interpretation of data for the work. Each author had role in drafting the work and revising it critically for important intellectual content. Each author gave final approval of the version to be published and they agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial support and sponsorship:
None.
Conflicts of interest:
There are no conflicts of interest.
REFERENCES
- 1.Liu Z, McGrath C, Hägg U. The impact of malocclusion/orthodontic treatment need on the quality of life. A systematic review. Angle Orthod. 2009;79(3):585–591. doi: 10.2319/042108-224.1. [DOI] [PubMed] [Google Scholar]
- 2.Rusanen J, Lahti S, Tolvanen M, Pirttiniemi P. Quality of life in patients with severe malocclusion before treatment. Eur J Orthod. 2010;32:43–48. doi: 10.1093/ejo/cjp065. [DOI] [PubMed] [Google Scholar]
- 3.Silvola AS, Rusanen J, Tolvanen M, Pirttiniemi P, Lahti S. Occlusal characteristics and quality of life before and after treatment of severe malocclusion. Eur J Orthod. 2012;34:704–709. doi: 10.1093/ejo/cjr085. [DOI] [PubMed] [Google Scholar]
- 4.Locker D. Concept of oral health, disease and the quality of life. In: Slade GD, editor. Measuring oral health and quality of life. Chapel Hill: University of North Carolina; p. 1997. [Google Scholar]
- 5.Brook PH, Shaw WC. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11(3):309–20. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 6.Perillo L, Masucci C, Ferro F, Apicella D, Baccetti T. Prevalence of orthodontic treatment need in southern Italian schoolchildren. Eur J Orthod. 2010;32(1):49–53. doi: 10.1093/ejo/cjp050. [DOI] [PubMed] [Google Scholar]
- 7.Jamilian A, Darnahal A, Damani E, Talaeipour M, Kamali Z. Prevalence of orthodontic treatment need and occlusal traits in school children. Int Scholar Res Not 2014. 2014:5. doi: 10.1155/2014/349793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGrath C, Bedi R. The value and use of ‘‘quality of life’’ measures in the primary dental care setting. Prim Dent Care. 1999;6:53–57. [PubMed] [Google Scholar]
- 9.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. Journal of Orthodontics. 2001;28:152–158. doi: 10.1093/ortho/28.2.152. [DOI] [PubMed] [Google Scholar]
- 10.Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 11.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 12.Ravaghi V, Farrahi-Avval N, Locker D, Underwood M. Validation of the persian short version of the oral health impact profile (OHIP-14) Oral Health Prev Dent. 2010;8(3):229–235. [PubMed] [Google Scholar]
- 13.Chen M, Wang DW, Wu LP. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in chinese patients. Angle Orthod. 2010;80:49–53. doi: 10.2319/010509-9.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bramanti E, Matacena G, Cecchetti F, Arcuri C, Cicciù M. Oral health-related quality of life in partially edentulous patients before and after implant therapy: a 2-year longitudinal study. Oral Implantol (Rome) 2013;6(2):37–42. [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor KR, Kiyak A, Huang GJ, Greenlee GM, Jolley CJ, King GJ. Effects of Malocclusion and its treatment on the quality of life of adolescents. Am J Orthod Dentofacial Orthop. 2009;136(3):382–392. doi: 10.1016/j.ajodo.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 16.Tsakos G. Combining normative and psychosocial perception for assessing orthodontic treatment needs. J Dent Educ. 2008 Aug;72(8):876–885. [PubMed] [Google Scholar]
- 17.de Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004 Mar;31(1):20–27. doi: 10.1179/146531204225011364. [DOI] [PubMed] [Google Scholar]
- 18.Leao A, Sheiham A. The development of a socio-dental measure of dental impacts on daily living. Community Dent Health. 1996 Mar;13(1):22–26. [PubMed] [Google Scholar]
- 19.Zhang M, McGrath C, Hagg U. Patients expectations and experiences of fixed orthodontic appliances therapy. Impact on quality of life. Angle Orthod. 2007 Mar;77(2):318–322. doi: 10.2319/0003-3219(2007)077[0318:PEAEOF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Bailey LJ, Haltiwanger LH, Blakey GH, Proffit WR. Who seeks surgical orthodontic treatment: a current review . International Journal of Adult Orthodontics and Orthognathic Surgery. 2001;16:280–292. [PubMed] [Google Scholar]
- 21.Siow KK, Ong ST, Lian CB, Ngeow WC. Satisfaction of orthognathic surgical patients in a Malaysian population. Journal of Oral Science. 2002;44:165–171. doi: 10.2334/josnusd.44.165. [DOI] [PubMed] [Google Scholar]
- 22.Pahkala RH, Kellokoski JK. Surgical-orthodontic treatment and patients functional and psychological well-being . American Journal of Orthodontics and Dentofacial Orthopedics. 2007;132:158–164. doi: 10.1016/j.ajodo.2005.09.033. [DOI] [PubMed] [Google Scholar]
- 23.Palomares NB, Celeste RK, Oliveira BH, Miguel JA. How does orthodontic treatment affect young adults’ oral healthrelated quality of life? Am J Orthod Dentofacial Orthop. 2012;141:751–758. doi: 10.1016/j.ajodo.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 24.Chen M, Feng ZC, Liu X, Li ZM, Cai B, Wang DW. Impact of malocclusion on oral health–related quality of life in young adults. The Angle Orthodontist. 2015;85:986–991. doi: 10.2319/101714-743.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernabé E, Sheiham A, Tsakos G, Messias de Oliveira C. The impact of orthodontic treatment on the quality of life in adolescents: A case-control study. Eur J Orthod. 2008;30:515–520. doi: 10.1093/ejo/cjn026. [DOI] [PubMed] [Google Scholar]
- 26.Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod. 2015;37:238–247. doi: 10.1093/ejo/cju046. [DOI] [PubMed] [Google Scholar]
- 27.Andiappan M, Gao W, Bernabe E, Kandala NB, Donaldson AN. Malocclusion, orthodontic treatment, and Oral Health Impact Profile (OHIP-14): Systematic review and meta-analysis. Angle Orthod. 2015;85:493, 500. doi: 10.2319/051414-348.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Y, Hagg U, Rabie AB. Severity of dentofacial deformity, the motivations and the outcome of surgery in skeletal Class III patients. Chin Med J (Engl) 2002;115:1031–1034. [PubMed] [Google Scholar]
- 29.Choi SH, Kim JS, Cha JY, Hwang CJ. Effect of malocclusion severity on oral health-related quality of life and food intake ability in a Korean population. Am J Orthod Dentofacial Orthop. 2016;149:384–390. doi: 10.1016/j.ajodo.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 30.Simões RC, Goettems ML, Schuch HS, Torriani DD, Demarco FF. Impact of malocclusion on oral health-related quality of life of 8-12 years old schoolchildren in Southern Brazil. Braz Dent J. 2017;28:105–112. doi: 10.1590/0103-6440201701278. [DOI] [PubMed] [Google Scholar]
- 31.Hatch JP, Rugh JD, Clark GM, Keeling SD, Tiner BD, Bays RA. Health-related quality of life following orthognathic surgery. International Journal of Adult Orthodontics and Orthognathic Surgery. 1998;13:67–77. [PubMed] [Google Scholar]
- 32.Motegi E, Hatch JP, Rugh JD, Yamaguchi H. Health-related quality of life and psychosocial function 5 years after orthognathic surgery. American Journal of rthodontics and Dentofacial Orthopedics. 2003;124:138–143. doi: 10.1016/s0889-5406(03)00391-3. [DOI] [PubMed] [Google Scholar]
- 33.Lee S, McGrath C, Samman N. Impact of orthognathic surgery on quality of life. Journal of Oral and Maxillofacial Surgery. 2008;66:1194–1199. doi: 10.1016/j.joms.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Koroluk LD, Tulloch JF, Phillips C. Incisor trauma and early treatment for Class II. Division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2003;123:117–125. doi: 10.1067/mod.2003.86. [DOI] [PubMed] [Google Scholar]
- 35.Shulman JD, Peterson J. The association between incisor trauma and occlusal characteristics in individuals 8-50 years of age. Dent Traumatol. 2004;20:67–74. doi: 10.1111/j.1600-4469.2004.00234.x. [DOI] [PubMed] [Google Scholar]
- 36.Silvola AS, Varimo M, Tolvanen M, Rusanen J, Lahti S, Pirttiniemi P. Dental esthetics and quality of life in adults with severe malocclusion before and after treatment. Angle Orthod. 2014;84:594–599. doi: 10.2319/060213-417.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feu D, de Oliveira BH, de Oliveira AM, Kiyak HA, Miguel JA. Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop. 2010;138:152–159. doi: 10.1016/j.ajodo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 38.Feu D, Miguel JA, Celeste RK, Oliveira BH. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013;83:892–898. doi: 10.2319/100412-781.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


