Abstract
Aim:
To evaluate safety and efficacy of Laser in situ Keratomileusis (LASIK) procedure for the correction of high hypermetropia.
Methods:
Retrospective study of 160 patients (266 eyes) who underwent LASIK procedure for the correction of hypermetropia between +3.00 and +7.00 diopters(D) and cylinder up to 2.00D from January 2013 and August 2015. All ablations were performed with Wavelight Allegretto Eye-Q400Hzexcimer laser (Alcon, Forth Worth, TX, USA) with aberration free module and were centered on a corneal vertex. All flaps were made with Moria M2 (Moria, Antony, France) mechanical microkeratome (90μm head). Preoperative and postoperative uncorrected and corrected distant visual acuity (UDVA, CDVA), spherical equivalent (SE) and a berrometry for 5mm pupil were measured. Measurements were taken at 1 week, 1,3,6 and 12 months after the surgery. Wilcoxon Signed Ranks Test was used for statistical analysis.
Results:
Postoperative UDVA was lower than preoperative CDVA at 1 week(p=0.001), at 1 month there was no difference (p=0.099), and at 3,6 and 12 months UDVA was better (p<0.0001). Preoperative SE was 4.69±1.20D (+3.75 to +7.50D). At 1 week SE was 0.03±0.67D (-0.50 to +0.63D), while at 1 year regressed to 0.58±0.56D (+0.25 to +0.88D). Sphere shifted from negative values targeted in treatment planning to compensate for regression to positive values. There was significant difference in SE at every time point (p<0.0005). There was a significant increase in coma (p<0.0001), trefoil (p<0.0001, p=0.0006) and spherical aberration (p=0.022, p=0.0052) at 1 week and 1 month postoperatively, without change throughout the rest of follow up.
Conclusion:
LASIK for high hypermetropia showed satisfactory results in postoperative refraction with reasonable regression without significant loss of lines of visual acuity. However, more test are necessary to asses optical quality.
Keywords: LASIK, Hypermetropia, refractive surgery
1. INTRODUCTION
Refractive surgery for hyperopia has been a challenge for surgeons in last few decades (1, 2). Hyperopia contributes to around 1/3 of all of refractive anomalies (3), but still the focus of corneal refractive surgery has centered primarily on myopia. Many studies have reported high level of safety and efficacy of Laser in situ Keratomileusis (LASIK) in correction of low hyperopia(up to 4 D) (1-2, 4-5).
The complications that have been limiting hyperopic LASIK in high hyperopia include decentration and regression, poor qualityof vision related to the induction of a significant high level of higher-order aberrations which can affect the predictability, safety, and efficacy of the treatment (6-8).
However, advances in eye trackers and ablation profiles have led to improvement in results of LASIK even for high hyperopia (4-5, 9-12).
2. AIM
The purpose of this study is to evaluate safety and efficacy of LASIK procedure in high hyperopia.
3. METHODS
The study included 160 patients (266 eyes) that underwent LASIK procedure for hypermetropia correction. The range of diopters was between +3.00 and +7.0 diopters(D) and cylinder up to 2.00 D.
Preoperative examinations
All patients underwent a complete preoperative ophthalmological examination. Inclusion criteria were: stable refraction, hypermetropia between +3.00 and +7.00 D, astigmatism ≤2.00 D. Ocular criteria were those normally adopted in refractive surgery. Exclusion criteria were unstable hyperopia, age younger than 18 years, active corneal disease, lens opacities, irregular cornea on corneal topography, previous ocular surgery, history of ocular trauma, uveitis, anterior or posterior synechiae, glaucoma, and ocular hypertension. Patients with amblyopia and a potential CDVA of less than 0.2 were also excluded.
Surgical procedure and postoperative care
Prior to the surgery, two drops of topical anesthetic (Novesine, OmniVision GmbH, Puchheim, Germany) were instilled at 2- minute intervals, and the eye was cleaned with 2.5 % povidone iodine. A corneal flap was made using Moria M2 mechanical microkeratome with 90 μm head (Moria, Antony, France). Wavelight Allegretto Eye-Q 400Hz (Alcon, Forth Worth, TX, USA) was used for the excimer laser treatment. The optical zone was fixed at 6.5 mm as recommended by the manufacturer, and the wave front optimized program was used. The Aberration FreeTM program was applied in all cases.
For all patients, the programmed treatment consisted of cycloplegic spherical correction with manifest astigmatic power and axis.“Wellington nomogram“ provided by the company was used for spherical correction.
The flap was lifted and excimer laser ablation was delivered to the stroma. Patients were instructed to concentrate on the fixation light throughout the ablation. When the ablation was completed, the flap was repositioned after the interface was irrigated with balanced salt solution, removing any debris. Postoperative therapy included combination of topical antibiotic and steroid drops (Tobradex, Alcon, Forth Worth, TX, USA) 4 times daily for 2 weeks, and artificial tears (Blink, Abbott Medical Optics, Santa Ana, CA, USA) 6-8 times daily for at least 1 month.
Postoperative evaluation
All patients were examined at 1 week, 1, 3, 6 and 12 months after the surgery. Results 1 year after the surgery were analyzed in this study. At each visit UDVA, CDVA and SE were measured. Slit-lamp examination, tonometry, and corneal topography was also performed.
Statistical calculation was performed with SPSS for Windows (19.0, SPSS Inc, Chicago, Illinois, SAD) and Microsoft Excel (11.0, Microsoft Corporation, Redmond, WA, SAD). The comparison between the preoperative and postoperative periods was performed with the Wilcoxon signed rank test. Value of p<0.05 was considered statistically significant.
4. RESULTS
The study has been conducted from January 2013 and August 2015. Out of 160 patients (266 eyes) 93 were males (58%) and 67 were females (42%). Average age was 42±11.3 years (range: 21 - 66 years).
CDVA preoperatively was 0.77±0.24 (range: 0.6-0.9). Postoperative UDVA was lower than preoperative CDVA at 1 week (p=0.001), at 1 month there was no difference (p=0.099), but at 3,6 and 12 months UDVA was significantly better compared to preoperative CDVA (p<0.0001).
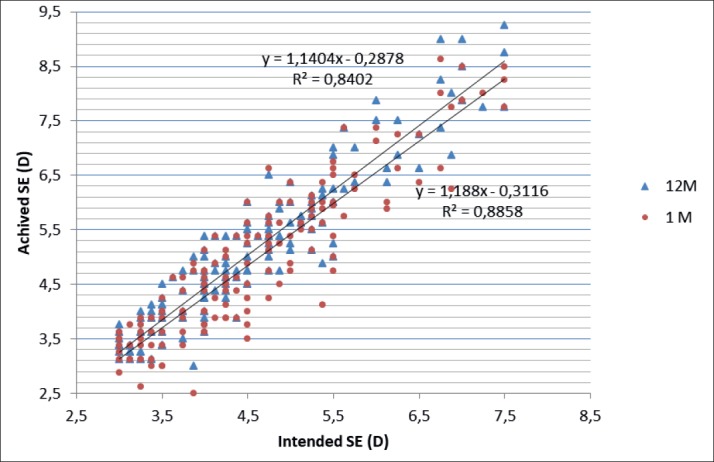
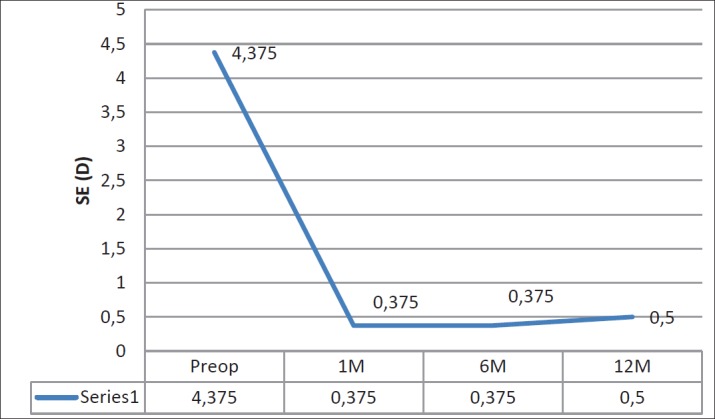
Preoperative SE was 4.69±1.2D (range +3.75 to +7.50 D). At 1 week SE was 0.03±0.67D (range -0.50 to + 0.63D), while at 1 year regressed to 0.58±0.56D (range +0.25 to +0.88D), as shown in Graph 1. Sphere shifted from negative values targeted in treatment planning to compensate for regression to positive values. There was significant difference in SE at every time point (p<0.0005). There was a strong correlation between the attempted and achieved corrections (R2 Z 0.65). (Graph 2).
Graph 1. Scattergram comparing achieved spherical equivalent refraction 12 months postoperatively (Y axis) and attempted spherical equivalent refraction (X axis). SE – spehical equivalent, D- diopter, M – month.
Graph 2. Spherical equivalent preoperatively and in follow up period. SE – spehical equivalent, D- diopter, M – month.
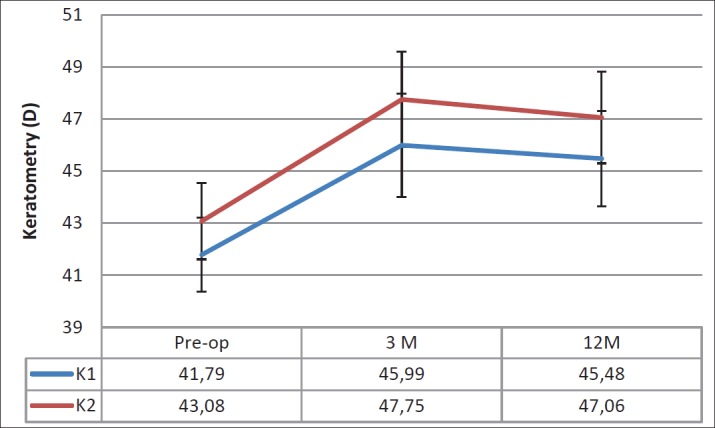
There was no statistically significant difference in postoperative values of keratometry and pachymetry during follow up period. In Graph 3 keratometry changes are presents.
Graph 3. Changes in keratometry in follow up period D-diopter, M-months, K – keratometry.
There was a significant increase in coma (p<0.0001), trefoil (p<0.0001,p=0.0006) and spherical aberration (p=0.022,p=0.0052) at 1 week and 1 month postoperatively, without change throughout the rest of follow up.
In our study efficacy index (defined as UDVA at 12 month postoperatively / CDVA preoperatively) 1.037. Safety index (defined as CDVA at 12 months / CDVA preoperatively) 1.054.
5. DISCUSSION
For few decades there have been many attempts to correct hyperopia, but were not effective or safe enough (9, 13). Recent literature on the other hand shows that it is possible to achieve±0.50D one year after LASIK in hyperopic patients, which is also demonstrated in our study (14). Result of our study do differ somewhat from current literature. Residual SE in our study was as high as +0.40 D. Kanellopulus et al. report residual myopia of -0.39±0.30D after two years, and Gil-Cazora et al. hyperopia of +0.72±0.80D in first months after the surgery (15, 16). In our study there was small myopic shift (p<0.001) in first postoperative visits, but this slight over correction was transitory. This can also be consistent with the natural progression of hyperopia in population (17). Desai et al. reported modest regression of refractive effect even after 5 years of followup (+0.40 ± 0.79 D) (18). Other older publications stated that under correction was expected in patients with SE +5.00 D. Those results were guidelines for better planning, so this over correction in first postoperative period was expected and planned (19).
Complications in this study were loss of 2 lines in twoeyes (0.74%), loss of 1 line in one eye (0.37%), diffuse lamellar keratitis (DLK) in three eyes (1.13%), prolonged dry eye in nine patients (18 eyes) (6.7%) even after 3 months postoperatively. Loss of lines varies between studies (18, 19), older studies state that the higher hyperopia and the smaller optical zone, loss of lines and less efficient results are expected (7). Later, surgical safety was defined as loss of 2 or more lines of CDVA at 6 months between 1 and 5% (21). Our study is within these margins.
There was a significant increase in coma (p<0.0001), trefoil (p<0.0001, p=0.0006) and spherical aberration (p=0.022, p=0.0052) at 1 week and 1 month postoperatively, without change throughout the rest of follow up.
Increase in coma and spherical aberration was statistically significant, similar results have been reported by other authors (22). Induction of HOAs in our patients can have correlation to loss of lines in the study, but there was not statistically significant connection. Further, more HOA oriented studies, are needed to include more factors into study.
Enhancement was performed in 15 eyes (5.6%), compared to 29.4% reported by Jorge L et al (23). We believe that our low percent of enhancement is due to newer eye tracking systems, balanced nomograms and higher repletion rate of laser and the use of optimized aberration-free ablation profiles. Also, we have rigorous inclusion criteria in terms of full cyclopegia and long preoperative preparation with the patient.
Safety index is somewhat higher compared to Jorge (index 0.94), in our study index was 1.054. Efficacy index on the other hand was extremely better (index 1.037), than in other studies: (ranging from 0.6115 to 0.9) (24). Our results were morecomparable to Simon et al. report ofsafety index 1.03 and efficacy index 1.40 (25).
We plan to report the outcomes over a longer period, because some studies found average increase in hyperopia +0,54 over 5 years postoperatively, which is more than expected physiologically and can be indicator of destabilization of cornea after LASIK (20).
6. CONCLUSION
LASIK for high hyperopia showed satisfactory results in postoperative refraction with reasonable regression without loss of lines of visual acuity, however more test are necessary to asses optical quality.
Author’s contribution:
A.P, M.A.P, N.Ž and S.G gave substantial contributions to the conception or design of the work in acquisition, analysis, or interpretation of data for the work. A.B and A.P had a part in article preparing for drafting or revising it critically for important intellectual content, and A.B and M.B gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms.
Conflicts of interest:
There are no conflicts of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Suarez E, Torres F, Duplessie M. LASIK for correction of hyperopia and hyperopia with astigmatism. Int ophthalmol Clin. 1996;36(4):65–72. doi: 10.1097/00004397-199603640-00010. [DOI] [PubMed] [Google Scholar]
- 2.Ditzen K, Huschka H, Pieger S. Laser in situ keratomileusis for hyperopia. J Cataract refract surg. 1998;24(1):42–47. doi: 10.1016/s0886-3350(98)80073-4. [DOI] [PubMed] [Google Scholar]
- 3.Hashmani S, Hashmani N, Haroon H, et al. Visual and refractive outcomes of Topography-guided laser-assisted In situ Keratomileusis in Virgin eyes. Cureus. 2018;10(1):e2131. doi: 10.7759/cureus.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spadea l, Sabetti l, D’alessandri l, Balestrazzi E. Photorefractive keratectomy and lasIK for the correction of hyperopia:2-year follow-up. J refract surg. 2006;22:131–136. doi: 10.3928/1081-597X-20060201-09. [DOI] [PubMed] [Google Scholar]
- 5.Alio J, Galal A, Ayala MJ, Artola A. Hyperopic LASIK with Esiris/Schwind technology. J Refract Surg. 2006;22(8):772–781. doi: 10.3928/1081-597X-20061001-07. [DOI] [PubMed] [Google Scholar]
- 6.Argento CJ, Cosentino MJ. Comparison of optical zones in hyperopic laser in situ keratomileusis: 5.9 mm versus smaller optical zones. J Cataract Refract Surg. 2000;26(8):1137–1146. doi: 10.1016/s0886-3350(99)00356-9. [DOI] [PubMed] [Google Scholar]
- 7.EL-Helw M, Emarah A. Predictability and stability of refraction with increasing optical zone diameter in hyperopic LASIK. Clin Ophthalmol. 2010;4(1):455–845. doi: 10.2147/opth.s11007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davidorf JM, Eghbali F, Onclinx T, Maloney RK. Effect of varying the optical zone diameter on the results of hyperopic laser in situ keratomileusis. Ophthalmology. 2001;108(7):1261–1265. doi: 10.1016/s0161-6420(01)00588-7. [DOI] [PubMed] [Google Scholar]
- 9.Lee EJ, Lim DH, You JY, Chung TY, Chung ES. Clinical Outcome of Retreatment after Refractive Surgery. J Korean Ophthalmol Soc. 2015;56(2):180–189. [Google Scholar]
- 10.Jacobs JM, Sanderson MC, Spivack LD, Wright JR, Roberts AD, Taravella MJ. Hyperopic laser in situ keratomileusis to treatovercorrected myopic LASIK. J Cataract Refract Surg. 2001;27:389–395. doi: 10.1016/j.jcrs.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Mimouni M, Flores V, Sela T, Munzer G, Kaiserman I. Risk Factors for Re-treatment following Hyperopic LASIK. Journal of refractive surgery. 2018;34(5):316–320. doi: 10.3928/1081597X-20180228-02. [DOI] [PubMed] [Google Scholar]
- 12.Peng YM, Hannan S, Teenan D, Schallhorn S J, Schallhorn JM. Monovision lasik in emmetropic presbyopic patients. Clin Ophthalmology. 2018;12:1665–1671. doi: 10.2147/OPTH.S170759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waring GO, III, Fant B, Stevens G, Phillips S, Fischer J, Tanchel N, Schanzer C, Narvaez J, Chayet A. Laser in situ keratomileusis for spherical hyperopia and hyperopic astigmatism using the NIDEK EC-5000 excimer laser. J Refract Surg. 2008;24(2):123–136. doi: 10.3928/1081597X-20080201-02. [DOI] [PubMed] [Google Scholar]
- 14.Reinstein DZ, Carp GI, Archer TJ, Buick T, Gobbe M, Rowe EL, Jukic M, Brandon E, Moore J, Moore T. LASIK for the Correction of High Hyperopic Astigmatism With Epithelial Thickness Monitoring. J Refract Surg. 2017;33(5):314–321. doi: 10.3928/1081597X-20170111-04. [DOI] [PubMed] [Google Scholar]
- 15.Kanellopoulos AJ. Topography-guided hyperopic and hyperopic astigmatism femtosecond laser-assisted LASIK: long-term experience with the 400 Hz eye-Q excimer platform. Clin Ophthalmol. 2012;6(1):895–901. doi: 10.2147/OPTH.S23573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gil-Cazorla R, Teus MA, de Benito-Llopis L, Mikropoulos DG. Femtosecond laser vs mechanical microkeratome for hyperopic laser in situ keratomileusis. Am J Ophthalmol. 2011;152(1):16–21. doi: 10.1016/j.ajo.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Guzowski M, Wang JJ, Rochtchina E, et al. Five-year refractive changes in an older population; the Blue Mountains Eye Study. Ophthalmology. 2003;110(7):1364–1370. doi: 10.1016/S0161-6420(03)00465-2. [DOI] [PubMed] [Google Scholar]
- 18.Lee KE, Klein BE, Klein R. Changes in refractive error over a 5-year interval in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1999;40(8):1645–164. [PubMed] [Google Scholar]
- 18.Rajen U, Desai, ATul Jain MD, Edward E, Manche MD. Long-term follow-up of hyperopic laser in situ keratomileusis correction using the Star S2 excimer laser. J Cataract Refract Surg. 2008;34(2):232–237. doi: 10.1016/j.jcrs.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 19.Esquenazi S. Five-year follow-up of laser in situ keratomileusis for hyperopia using the Technolas Keracor 117C excimer laser. J Refract Surg. 2004;20:356–363. doi: 10.3928/1081-597X-20040701-09. Ophthalmology. 2004; 111: 1604-1617. [DOI] [PubMed] [Google Scholar]
- 20.Quito CF, Agahan AL, Evangelista RP. Long-Term Followup of Laser In Situ Keratomileusis for Hyperopia Using a 213 nm Wavelength Solid-State Laser. ISRN Ophthalmol. 2013;2013:276984. doi: 10.1155/2013/276984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chamon W, Allemann N, Alio JL, Azar DT. Management of Complications in Refractive Surgery. Berlin, Germany: Springer-Verlag; 2008. Refractive surgery outcomes and frequency of complications; pp. 1–8. [Google Scholar]
- 22.Nancy J, Keir OD, Trefford Simpson, Natalie Hutchings, Lyndon Jones, Desmond Fonn, Moptom J. Outcomes of wavefront-guided laser in situ keratomileusis for hyperopia Cataract Refract Surg. 2011;37:886–893. doi: 10.1016/j.jcrs.2010.12.039. [DOI] [PubMed] [Google Scholar]
- 23.Alió, Jorge L, El-Aswad A, Vega-Estrada A, Javaloy J. Laser in situ keratomileusis for high hyperopia (>5.0 diopters) using optimized aspheric profiles: Efficacy and safety. J Cataract Refract Surg. 2013;39(4):519–527. doi: 10.1016/j.jcrs.2012.10.045. [DOI] [PubMed] [Google Scholar]
- 24.Llovet F, Galal A, Benitez-del-Castillo J-M, Ortega J, Martin C, Baviera J. One-year results of excimer laser in situ keratomileusis for hyperopia. J Cataract Refract Surg. 2009;35:1156–1165. doi: 10.1016/j.jcrs.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 25.Bababeygy SR, Zoumalan IC, Chien YF, Manche EE. Wavefront-guided laser in situ keratomileusis retreatment for consecutive hyperopia and compound hyperopic astigmatism. J Cataract Refract Surg. 2008;34(8):1260–1266. doi: 10.1016/j.jcrs.2008.04.026. [DOI] [PubMed] [Google Scholar]


