Abstract
Positive memory encoding and retrieval deficits have an empirical relation with several post-trauma outcomes. Drawing from the Contractor et al. model, we examined relations between positive memory characteristics and post-trauma mental health indicators. A trauma-exposed community sample of 203 participants (Mage = 35.40 years; 61.10% female) was recruited via Amazon’s Mechanical Turk. Participants completed measures of posttraumatic stress disorder (PTSD; PTSD Checklist for DSM-5), depression (Patient Health Questionnaire-9), posttraumatic cognitions (Posttraumatic Cognitions Inventory), affect (Positive and Negative Affect Schedule), count/number of recalled specific positive memories (Autobiographical Memory Test) and accessibility of a specific positive memory (i.e. subjective ease of recalling details of a memory; Memory Experiences Questionnaire-Short Form). Linear regression results indicated that PTSD intrusion severity, PTSD negative alterations in cognitions and mood (NACM) severity, PTSD alterations in arousal and reactivity (AAR) severity, self-blame, and positive affect significantly and negatively predicted the count of specific positive memories. Further, PTSD NACM severity, PTSD AAR severity, negative cognitions about the self, and negative affect significantly and negatively predicted accessibility of a specific positive memory. Thus, count/accessibility of specific positive memories was associated with several post-trauma mental health indicators; this highlights the relevance and potential impact of integrating positive memories into trauma treatment.
Keywords: PTSD, depression, affect, cognitions, positive memories
Introduction
Deficits in the encoding, consolidation, and/or retrieval of positive memories play a role in the symptomatology of posttraumatic stress disorder (PTSD; Brewin and Holmes, 2003; McNally, Lasko, Macklin, & Pitman, 1995; Schönfeld and Ehlers, 2017). However, most current trauma research and clinical work primarily targets traumatic memories (Bernsten and Rubin, 2007; Schnurr, 2017). To incorporate a unique and primary focus on positive memories into the current trauma paradigm, Contractor et al. (2018) proposed a conceptual model outlining hypothesized mechanisms underlying the effects of positive memory processing on post-trauma outcomes with a focus on PTSD severity. Drawing from this model, we empirically examined the relation of the count of specific positive memories and accessibility of a specific positive memory (i.e. subjective ease of recalling a positive memory; Sutin and Robins, 2007) to post-trauma mental health indicators related to PTSD.
Positive Memories and PTSD
Positive memory processes and characteristics may contribute to the etiology and maintenance of PTSD severity (Contractor, Brown, et al., 2018). For example, evidence indicates that fewer positive memories pre-trauma was associated with greater PTSD severity post-trauma, both among pregnant women hospitalized with anticipated late-pregnancy and delivery complications (Hauer, Wessel, Engelhard, Peeters, & Dalgleish, 2009) and male fire-fighters (Bryant, Sutherland, & Guthrie, 2007). Further, trauma-exposed individuals with PTSD symptoms report difficulties in autobiographical memory specificity (de Decker, Hermans, Raes, & Eelen, 2003; Hayes, VanElzakker, & Shin, 2012; Ono, Devilly, & Shum, 2016), wherein they have greater difficulties recalling specific positive memories compared to individuals without PTSD (McNally, et al., 1995; McNally, Litz, Prassas, Shin, & Weathers, 1994). Indeed, a review of trauma studies indicated overgenerality (i.e., non-specificity) of memories for both positive and negative cues among trauma-exposed individuals (Williams et al., 2007). Attentional biases towards negative information (Aupperle, Melrose, Stein, & Paulus, 2012; Fani et al., 2012), rumination on negative memories cued by trauma reminders (Ehlers and Clark, 2000), and numbing/emotion dysregulation symptoms (Litz, Orsillo, Kaloupek, & Weathers, 2000; Weiss, Dixon-Gordon, Peasant, & Sullivan, 2018) experienced by trauma-exposed individuals may contribute to difficulties in recalling specific positive memories. In line with these findings, interventions increasing specific (positive) memory recall have been found to be effective for emotional disorders (Barry, Sze, & Raes, 2019), including for PTSD severity (Callahan, Maxwell, & Janis, 2019; Moradi et al., 2014). Thus, memory-based interventions show promise in addressing PTSD symptoms (Hitchcock, Werner-Seidler, Blackwell, & Dalgleish, 2017). In fact, increasing specific positive memory recall may serve as a resilience factor when coping with stressors (Askelund, Schweizer, Goodyer, & van Harmelen, 2019). Overall, evidence indicates that positive memory recall may inversely relate to PTSD severity.
Positive Memories and Depression
Trauma-exposed individuals may experience depression comorbid with PTSD (Bonde et al., 2016; Contractor, Roley-Roberts, Lagdon, & Armour, 2017; Rytwinski, Scur, Feeny, & Youngstrom, 2013). Given that both PTSD and depression have common underlying mechanisms (Post, Feeny, Zoellner, & Connell, 2016), some positive-memory processes and effects may be shared across the two constructs. Indeed, evidence indicates that individuals with depressed mood report difficulty recalling (specific) positive memories (Clark and Teasdale, 1982; Williams, et al., 2007), are more likely to recall unpleasant and unhappy events (Snyder and White, 1982), and rate positive memories as less vivid (Werner-Seidler and Moulds, 2011), than individuals without depressed mood; this, in turn, may maintain a chronic negative mood (Matt, Vázquez, & Campbell, 1992). Potential contributing factors outlined in the extant research include an over-focus on negative cognitions and stimuli (Beck, 1976; Murphy et al., 1999), reduced positive outcome expectancies (Clark and Teasdale, 1982), deficits in processing positive content (Joormann and Siemer, 2004; Werner-Seidler and Moulds, 2011), overgeneralized memory biases (Brittlebank, Scott, Williams, & Ferrier, 1993), and mood repair difficulties integral to depression (Gross and Muñoz, 1995; Tomarkenand and Keener, 1998).
Following from this, increasing specific positive memory recall has been shown to relate to beneficial outcomes for individuals with depression. For example, targeting positive memory recall caused reductions in sad mood among individuals meeting criteria for at least two major depressive episodes (Foland-Ross, Cooney, Joormann, Henry, & Gotlib, 2014) and mood improvements among individuals with major depressive disorder (Werner-Seidler, Tan, & Dalgleish, 2017). Extending from this, interventions focused on increasing retrieval of specific memories have caused reductions in depression severity among trauma-exposed adolescents (Neshat-Doost et al., 2013); training focused on increasing access to specific positive memories has repaired induced negative mood among individuals with depression (Arditte Hall, De Raedt, Timpano, & Joormann, 2018); and interventions focused on using positive stories to strengthen a positive self-image have improved self-esteem among individuals with depression (Korrelboom, Maarsingh, & Huijbrechts, 2012). Overall, evidence supports an inverse relation between positive memory recall and depression severity among trauma-exposed individuals.
Positive Memories and Affect
Trauma-exposed individuals, especially those with PTSD, report dysregulation for negative and positive affect (Keane, Fairbank, Caddell, Zimering, & Bender, 1985; Litz, et al., 2000; Weiss, et al., 2018). Positive memory recall may aid emotion regulation processes by downregulating negative affect and upregulating positive affect (Quoidbach, Mikolajczak, & Gross, 2015; Rusting and DeHart, 2000) among trauma-exposed individuals. Indeed, experimental evidence supports a negative relation between positive memories and negative affect, and a positive relation between positive memories and positive affect (Joormann, Siemer, & Gotlib, 2007; Josephson, 1996; Rusting and DeHart, 2000). To elaborate, an experiment by Josephson (1996) demonstrated that after a sad mood induction, participants who followed a negative memory with a positive one reported a more positive mood than participants who recalled two consecutive negative memories. Another study by Rusting and DeHart (2000) using four distinct samples indicated that after inducing a negative mood, engaging in positive reappraisal enhanced retrieval of more positive memories, and focusing on negative events enhanced retrieval of more negative memories. Related to interventions, procedures focused on enhancing recall of specific positive memories have found to increase positive emotions and reduce negative emotions among individuals with PTSD (Panagioti, Gooding, & Tarrier, 2012). Overall, evidence supports that positive memory recall may relate to enhanced positive affect and reduced negative affect among trauma-exposed individuals.
Positive Memories and Cognitions
Trauma-exposed individuals have predominantly negative self, other/world, and future schemas (Foa and Kozak, 1986; Janoff-Bulman, 1992), which creates difficulties in therapeutically disputing trauma-related maladaptive cognitions (McNally, et al., 1994). Positive memory recall may enhance adaptive cognitions; enhanced positive affect following positive memory retrieval may activate positive interpretations of events and pleasant thoughts/memories (mood-congruency effect; Blaney, 1986; Rusting and DeHart, 2000; Rusting and Larsen, 1998) and increase positive content in thoughts (broaden-and-build theory; Fredrickson, 2001). Further, greater positive memory specificity may reduce cognitive (primarily negative self-cognitions) vulnerability to depression over time among individuals with stressful life experiences (Askelund, et al., 2019), suggesting that engaging with positive memories particularly impacts negative beliefs about self. Overall, supporting evidence indicates that positive memory recall may beneficially impact schemas and self-image among trauma-exposed individuals.
Current Study
Despite the aforementioned findings, little research has examined relations between positive memory recall and a broad range of post-trauma mental health indicators including PTSD, depression, affect, and cognitions. Additionally, when PTSD has been researched in relation to positive memories, the heterogeneity in its symptom clusters has rarely been considered; evidence suggests variable relations between the different PTSD symptom clusters and psychopathology (Armour, Contractor, Palmieri, & Elhai, 2014; Contractor, Armour, Forbes, & Elhai, 2016; Contractor et al., 2014; Contractor, Greene, Dolan, & Elhai, 2018). Lastly, investigators have rarely examined objective and subjective facets of positive memory recall in the same study. Notably, factors such as emotional status have been found to differentially impact subjective memory ratings and objective memory performance (Smith, Petersen, Ivnik, Malec, & Tangalos, 1996), highlighting the importance of examining multiple facets of autobiographical memory recall.
Addressing these limitations and drawing from the Contractor et al. (2018) model, we examined the relation between positive memory characteristics (count of specific positive memories and accessibility of a specific positive memory) and several theoretically relevant post-trauma mental health indicators (PTSD subscale severity [intrusions, avoidance of trauma reminders, negative alterations in cognitions and mood, alterations in arousal and reactivity]; depression severity; positive and negative affect; and post-trauma cognitions). Further, we examined objectively assessed (i.e., count of specific positive memories measured via a performance-based task of the Autobiographical Memory Test; Williams and Broadbent, 1996) and subjectively reported (i.e., ease of accessing a specific positive memory measured via a self-report measure of the Memory Experiences Questionnaire-Short Form; Luchetti and Sutin, 2016) facets of positive memory recall (Holland and Kensinger, 2010). Notably, these two positive memory characteristics are related; greater accessibility of a specific positive memory may enhance one’s ability to recall more specific positive memories consistent with mood-congruent memory recall (Bower, 1981) as discussed by Clark and Collins (1993).
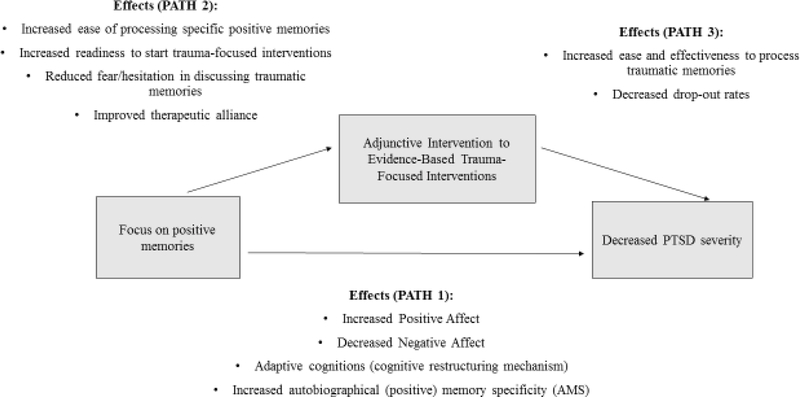
Given that the conceptual relations of the Contractor et al. (2018) model (see Figure 1) have not been empirically examined in prior studies, the primary aim of the current study was to establish whether the hypothesized relations were present within this sample. Specifically, we hypothesized that a significant negative relation between specific positive memory recall count/accessibility with PTSD symptom cluster severity (McNally, et al., 1994; Moradi, et al., 2014), depression severity (Clark and Teasdale, 1982; Snyder and White, 1982), maladaptive post-trauma cognitions (Blaney, 1986; Fredrickson, 2001; Rusting and Larsen, 1998), and negative affect (Joormann, et al., 2007; Josephson, 1996; Rusting and DeHart, 2000) would have greater difficulties recalling specific positive memories (count/accessibility). Further, we hypothesized a significant positive relation between specific positive memory recall count/accessibility with positive affect (Joormann, et al., 2007; Josephson, 1996; Rusting and DeHart, 2000).
Figure 1.
Contractor et al. (2018) Conceptual Model outlining Proposed Effects of Targeting Positive Memories on Post-trauma Outcomes
Methods
Procedure and Participants
The study was approved by the University of North Texas Institutional Review Board. The current study was part of a larger study conducted via Amazon’s Mechanical Turk (MTurk) online recruitment platform; it was described as a 60-minute study examining relations between the recall of positive memories, positive memory processes, and emotional distress indicators among individuals experiencing stressful life events. The inclusionary criteria included being >/=18 years, having a working knowledge of English, endorsing a stressful life experience, and no current or previous diagnosis of sleep apnea. Sleep apnea, which includes brief awakenings during sleep, is related to lower quality sleep (Ho and Brass, 2011), influences sleep disturbances (American Psychiatric Association, 2013), and interferes with memory consolidation (Kloepfer et al., 2009). All such factors may adversely influence one’s ability to accurately report on other sleep indicators (e.g., sleep quality and quantity) as well as on symptomatology; information on these variables were collected as part of the larger study to examine the relation between PTSD severity, self-reported sleep indicators, and memory functioning. Eligible participants who provided informed consent and completed the entire survey without failing validity checks received $1.50 as compensation, consistent with recommended (Barger, Benrend, Sharek, & Sinar, 2011; Schmidt, 2015) and implemented compensation practices (e.g., Contractor, Frankfurt, Weiss, & Elhai, 2017; Seligowski and Orcutt, 2016; van Stolk-Cooke et al., 2018). Additionally, compensation rates have not been found to negatively influence data quality (Buhrmester, Kwang, & Gosling, 2011).
Exclusions, Missing Data, and Sample Characteristics
A total of 695 participants attempted the survey; 299 duplicate responses were excluded based on multiple attempts (remainder n = 466). We excluded 89 participants for not meeting study inclusionary criteria (remainder n = 377); 138 participants for failing validity checks inserted to ensure attention and comprehension (reminder n = 239; Meade and Craig, 2012; Oppenheimer, Meyvis, & Davidenko, 2009; Thomas and Clifford, 2017); one participant for not endorsing any traumatic event on the Life Events Checklist for DSM-5 (reminder n = 238; LEC-5; Weathers et al., 2013); 32 participants for not following instructions on the Memory Experiences Questionnaire-Short Form (reminder n = 206; MEQ-SF; Luchetti and Sutin, 2016); and three individuals with > 30% missing data on any variable of interest (reminder n = 203). The final sample of 203 participants averaged 35.40 years of age (SD = 11.52); 124 were female (61.10%). Eighty-five (41.90%) participants had probable PTSD based on the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013) cut-off score > 31 (Blevins, Weathers, Davis, Witte, & Domino, 2015; Bovin et al., 2016; Wortmann et al., 2016). Detailed information on demographics and psychopathology variables is provided in Table 1.
Table 1.
Demographic and psychopathology variables-related information (n=203)
| Variable | Mean (SD) | Range |
|---|---|---|
| Age | 35.40 (11.52) | 19–72 |
| Years of schooling | 15.36 (2.38) | 6–27 |
| Count of specific positive memories | 6.88 (2.48) | 0–10 |
| Accessibility of a specific positive memory | 4.38 (.86) | 1–5 |
| PTSD intrusion severity | 7.33 (5.34) | 0–20 |
| PTSD avoidance severity | 7.03 (3.19) | 2–14 |
| PTSD NACM severity | 8.98 (7.29) | 0–26 |
| PTSD AAR severity | 7.54 (6.11) | 0–24 |
| Negative cognitions about self | 2.76 (1.40) | 1–6 |
| Negative cognitions about the world | 4.19 (1.55) | 1–7 |
| Self-blame | 2.62 (1.51) | 1–6 |
| Positive affect | 31.86 (9.23) | 10–50 |
| Negative affect | 18.44 (8.82) | 10–46 |
| Depression severity | 7.00 (6.84) | 0–27 |
| n (%) | ||
| Gender | ||
| Male | 77 (37.90%) | |
| Female | 124 (61.10%) | |
| Transgender | 1 (.50%) | |
| Gender Queer | 1 (.50%) | |
| Agender | 0 (0%) | |
| Other | 0 (0%) | |
| Employment Status | ||
| Part time | 31 (15.30%) | |
| Full time | 143 (70.40%) | |
| Retired | 4 (2.00%) | |
| Unemployed | 20 (9.90%) | |
| Unemployed Student | 5 (2.50%) | |
| Relationship Status | ||
| Single | 63 (31.00%) | |
| Living with significant other | 36 (17.70%) | |
| Married | 83 (40.90%) | |
| Divorced | 18 (8.90%) | |
| Separated | 2 (1.10%) | |
| Widowed | 1 (.50%) | |
| Ethnicity | ||
| Hispanic or Latino | 17 (8.40%) | |
| Not Hispanic or Latino | 183 (90.10%) | |
| Unknown | 3 (1.50%) | |
| Racial Status (could endorse more than one category) | ||
| Caucasian or White | 168 (82.80%) | |
| African American or Black | 27 (13.30%) | |
| Asian | 8 (3.90%) | |
| American Indian or Alaskan Native | 7 (3.40%) | |
| Native Hawaiian/other Pacific Islander | 1 (.50%) | |
| Unknown | 1 (.50%) | |
| Income | ||
| Less than $15,000 | 15 (7.40%) | |
| $15,000 – $24,999 | 26 (12.80%) | |
| $25,000 – $34,999 | 18 (8.90%) | |
| $35,000 – $49,999 | 42 (20.70%) | |
| $50,000 – $64,999 | 42 (20.70%) | |
| $65,000 – $79,999 | 24 (11.80%) | |
| $80,000 and higher | 36 (17.70%) | |
| Treatment for Mental Health/Emotional Problem (could endorse more than one category) | ||
| Currently in therapy | 28 (13.80%) | |
| Been in therapy in the past | 88 (43.30%) | |
| Currently taking medications for mental health/emotional problem | 44 (21.70%) | |
| Have taken medications in the past for mental health/emotional problem | 59 (29.10%) | |
| Never received treatment (therapy/medications) for mental health/ emotional problem | 78 (38.40%) | |
| Worst Traumatic Event endorsed on the LEC-5 | ||
| Natural disaster | 26 (12.80%) | |
| Fire or explosion | 5 (2.50%) | |
| Transportation accident | 32 (15.80%) | |
| Serious accident at work/home/during recreational activity | 9 (4.40%) | |
| Exposure to a toxic substance | 0 (0%) | |
| Physical assault | 16 (7.90%) | |
| Assault with a weapon | 7 (3.40%) | |
| Sexual assault | 34 (16.70%) | |
| Other unwanted/uncomfortable sexual experience | 8 (3.90%) | |
| Combat or exposure to war | 1 (.50%) | |
| Forced captivity | 0 (0%) | |
| Life-threatening illness | 11 (5.40%) | |
| Severe human suffering | 3 (1.50%) | |
| Sudden, violent death | 15 (7.40%) | |
| Sudden, accidental death | 15 (7.40%) | |
| Serious injury/harm/death you caused to someone else | 4 (2.20%) | |
| None of these events happened to me | 17 (8.04%) | |
Note. LEC-5 = Life Events Checklist for DSM-5. PTSD = posttraumatic stress disorder. NACM = negative alternations in cognitions and mood. AAR = alterations in arousal and reactivity. Valid percentages were used to account for missing data.
Measures (in order of their presentation)
Demographic information.
We obtained information on age, gender, income, educational level, racial and ethnic status, relationship status, and mental health treatment.
Life Events Checklist for DSM-5 (LEC-5; Weathers, et al., 2013).
The LEC-5 is a 17-item self-report measure evaluating lifetime traumatic events. The 18th item assessed the most distressing of the endorsed traumatic events (subsequent PTSD measure was completed in reference to this distressing trauma). Participants indicated their exposure to each event on a 6-point nominal scale: happened to me, witnessed it, learned about it, part of my job, not sure, and does not apply. For the current study, positive endorsement of a traumatic event equated endorsing either of the first four response options for either of the first 16 LEC-5 items consistent with the DSM-5 Criterion A for PTSD (American Psychiatric Association, 2013).
PTSD Checklist for DSM-5 (PCL-5; Weathers, et al., 2013).
The PCL-5 is a 20-item self-report measure assessing past-month PTSD symptom severity. Response options range from 0 (not at all) to 4 (extremely). The four subscales include intrusions, avoidance, negative alterations in cognitions and mood (NACM), and alterations in arousal and reactivity (AAR). The PCL-5 has excellent psychometric properties (Blevins, et al., 2015; Bovin, et al., 2016; Wortmann, et al., 2016). In the current study, the Cronbach’s α for the intrusions, avoidance, NACM, and AAR subscales was .90, .87, .89, and .87, respectively.
Posttraumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo, 1999).
The PTCI is a 36-item self-report measure that assesses thoughts related to an experienced trauma. Response options range from 1 (totally disagree) to 7 (totally agree). The measure yields 3 subscales: Negative Cognitions about the Self (assessing feelings of unworthiness and incompetence), Negative Cognitions about the World (assessing the view that the world is dangerous), and Self-Blame (assessing blame of oneself for causing or failing to prevent a trauma). The PTCI has demonstrated adequate psychometric properties (Beck et al., 2004). In the current study, Cronbach’s α was .96, .91, and .85 for the subscales of Negative Cognitions about the Self, Negative Cognitions about the World, and Self-Blame respectively.
Autobiographical Memory Test (AMT; Williams and Broadbent, 1996).
The AMT was used to examine the count of specific positive memories participants were able to recall. Participants were presented with 10 positively valenced cue words: friendly, happy, honest, kind, humorous, cheer, pleased, relieved, lively, and glorious (Kleim and Ehlers, 2008; McNally, et al., 1995). Each cue word was followed by a prompt to recall a specific and meaningful memory of an event related to the cue word within 60 seconds, and participants subsequently typed the description of the recalled memory (Williams and Broadbent, 1996). Instructions for the AMT task were adapted from previous autobiographical memory studies (Henderson, Hargreaves, Gregory, & Williams, 2002; Williams et al., 1996; Zinbarg, Rekart, & Mineka, 2006). Based on recommended coding procedures (Griffith et al., 2009; Sutherland and Bryant, 2008b), AMT responses were coded as specific (i.e., memories of events that occurred within one day in a particular place), extended (i.e., memories of events which lasted longer than one day), categoric (i.e., memories that were summations of multiple repeated events), semantic associate (i.e., information that was not a personal memory), omission (i.e., did not recall the memory within 60 seconds or indicated inability to recall a memory), or non-positive (i.e., recalled a negative memory). For non-positive memories, we adapted coding criteria from the Coding and Assessment System for Narratives of Trauma (CASNOT); a response was coded as non-positive if the emotional tone and/or valence of the response was coded as predominantly negative (i.e., ratings of 3–4 on a scale from 0 [completely positive] to 4 [completely negative]; Fernández-Lansac and Crespo, 2017). Total number of responses coded as specific represented the count of specific positive memories variable in the current study (Sutherland and Bryant, 2008b). Interrater reliability for coding AMT responses as “specific” versus “overgeneral” (i.e., categoric or extended) for all cue words ranged from substantial to almost perfect (kappa range = .63 - .92; Landis and Koch, 1977).
Memory Experiences Questionnaire–Short Form (MEQ-SF; Luchetti and Sutin, 2016).
The MEQ-SF is a 31-item self-report measure comprising of 10 subscales examining 10 phenomenological characteristics of a described specific positive memory on a 5-point rating scale from 1 (strongly disagree) to 5 (strongly agree). Among the 10 phenomenological domains, the current study used the accessibility subscale scores (higher scores indicated greater accessibility and thus ease of recall of a specific positive memory). Items included in this subscale were as follows: “This memory was easy for me to recall;” “It was difficult for me to think of this memory;” and “I had to think for a while before I could recall this event.” Participants were asked to recall and write two paragraphs about one specific, positive memory using instructions adapted from existing studies (Boyacioglu and Akfirat, 2015; Janssen, Hearne, & Takarangi, 2015; Sutin and Robins, 2007; Wing, Schutte, & Byrne, 2006), and then completed the MEQ-SF. To ensure that the MEQ-SF memory responses were positively valenced, the memories were coded using CASNOT dimensions of emotional tone and emotional valence as described above (Fernández-Lansac and Crespo, 2017). The MEQ-SF has demonstrated adequate psychometric properties (Luchetti and Sutin, 2016); Cronbach’s α was .83 for the accessibility subscale in the current study. Interrater reliability for coding MEQ-SF responses as positive versus non-positive was substantial (kappa = .66; Landis and Koch, 1977).
Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988).
The PANAS is a self-report measure consisting of two, 10-item subscales assessing positive and negative affect. Participants rated the degree to which they experienced positive or negative affect over the past week on a 5-point Likert scale ranging from 1 (very slightly or not at all) to 5 (extremely). The PANAS demonstrates adequate psychometric properties (Crawford and Henry, 2004). In the current study, Cronbach’s α for the PANAS negative and positive scales were .91 and .94, respectively.
The Patient Health Questionnaire-9 (PHQ-9; Kroenke and Spitzer, 2002).
The PHQ-9 is a 9-item self-report measure assessing depression symptom severity within the past 2 weeks. Response options range from 0 (not at all) to 3 (nearly every day). The PHQ-9 has excellent psychometric properties (Kroenke and Spitzer, 2002; Kroenke, Spitzer, & Williams, 2001). In the current study, the Cronbach’s α for the total scale was .92.
Statistical Analyses
First, we examined normality (skewness < 2; kurtosis < 7; Curran, West, & Finch, 1996); the assumption of normality was not violated for the primary variables of the current study. Next, based on bivariate correlation results, post-trauma mental health indicators found to significantly correlate with the positive memory variables (p < .05) were entered as independent variables in subsequent linear regression analyses, in order to examine hypothesized relations in the Contractor et al. (2018) model conceptual model.
Following from this, we conducted nine linear regressions. We utilized linear regressions, rather than multiple regressions for two reasons. First, this study aimed to examine relations between positive memory variables and distinct post-trauma mental health constructs (PTSD subscale severity, depression severity, types of post-trauma cognitions, and affect) without adjusting for their influence on each other within the same model. When multiple variables are included in a multiple regression model, model effects can become inflated and/or dependent on which variables (of an infinite number of variables) are included in the model (Simmons, Nelson, & Simonsohn, 2011). As many of these variables are related, we wanted to understand each specific relationship, rather than the relationships in concert with other variables we could include in the analyses. Second, the study aims were consistent with the distinctiveness of these post-trauma mental health constructs in the Contractor et al. (2018) conceptual model, which has not been examined empirically. For the dependent variable of count of specific positive memories, we examined associations with five independent variables of PTSD intrusion severity, PTSD NACM severity, PTSD AAR severity, self-blame, and positive affect. For the dependent variable of accessibility of a specific positive memory, we examined associations with four independent variables of PTSD NACM severity, PTSD AAR severity, negative cognitions about self, and negative affect. Effect sizes were interpreted using standardized beta (β) estimates. Additionally, the Benjamini and Hochberg (B-H; 1995) method was used to control for the false discovery rate.
Results
Participants recalled an average of 6.88 (SD = 2.48) specific positive memories, and the average accessibility rating of a specific positive memory was 4.38 (SD = .86). See Table 2 for bivariate correlation results. Count of specific positive memories was significantly, negatively correlated with PTSD intrusion severity, PTSD NACM severity, PTSD AAR severity, self-blame, and positive affect. Accessibility of a specific positive memory was significantly, negatively correlated with PTSD NACM severity, PTSD AAR severity, negative cognitions about the self, and negative affect. The significance of the results of each regression analysis was determined based on the B-H critical value of .05 (Table 3).
Table 2.
Pearson’s Correlations between PTSD Severity, Negative Cognitions, Affect, Depression Severity, and Memory Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Count of specific positive memories | - | |||||||||||
| 2. Accessibility of a specific positive memory | .25*** | - | ||||||||||
| 3. Intrusion severity | −.16* | −.09 | - | |||||||||
| 4. Avoidance severity | −.02 | −.08 | .39*** | - | ||||||||
| 5. NACM severity | −.14* | −.17* | .75*** | .58*** | - | |||||||
| 6. AAR severity | −.19** | −.21** | .75*** | .49*** | .83*** | - | ||||||
| 7. Negative cognitions about the self | −.07 | −.21** | .54*** | .74*** | .73*** | .64*** | - | |||||
| 8. Negative cognitions about the world | .07 | .05 | .34*** | .78*** | .48*** | .43*** | .59*** | - | ||||
| 9. Self-blame | −.16* | −.14 | .39*** | .47*** | .50*** | .43*** | .66*** | .38*** | - | |||
| 10. Positive affect | −.24** | .07 | −.01 | −.25*** | −.18* | −.08 | −.33*** | −.13 | −.10 | - | ||
| 11. Negative affect | −.11 | −.20** | .46*** | .42*** | .60*** | .60*** | .66*** | .35*** | .41*** | −.34*** | - | |
| 12. Depression severity | .01 | −.13 | .50*** | .51*** | .69*** | .67*** | .72*** | .45*** | .40*** | −.35*** | .68*** | - |
Note.
p < .05
p < .01
p < .001
PTSD = posttraumatic stress disorder; NACM = negative alternations in cognitions and mood; AAR = alterations in arousal and reactivity.
Table 3.
Regression Results of the Relation between PTSD Severity, Negative Cognitions, Affect, and Memory Variables
| B | SE | β | t | R2 | F | |
|---|---|---|---|---|---|---|
| DV = Count of specific positive memories (n = 203) | ||||||
| Intrusion severity | −.07 | .03 | −.16 | −2.29p=.023* | .03 | 5.25 p=.023* |
| NACM severity | −.05 | .02 | −.14 | −1.99 p=.048* | .02 | 3.97p=.048* |
| AAR severity | −.08 | .03 | −.19 | −2.74 p=.007** | .04 | 7.53 p=.007** |
| Self-blame | −.27 | .11 | −.16 | −2.35 p=.020* | .03 | 5.53 p=.020* |
| Positive affect | −.06 | .02 | −.24 | −3.47 p=.001** | .06 | 12.04 p=.001** |
| DV = Accessibility of a specific positive memory (n = 200) | ||||||
| NACM severity | −.02 | .01 | −.17 | −2.49 p=.014* | .03 | 6.19 p=.014* |
| AAR severity | −.03 | .01 | −.21 | −3.06 p=.003** | .05 | 9.37 p=.003** |
| Negative cognitions about the self | −.13 | .04 | −.21 | −3.00 p=.003** | .04 | 8.99 p=.003** |
| Negative affect | −.02 | .01 | −.20 | −2.91 p=.004** | .04 | 8.47 p=.004** |
Note.
p < .05
p < .01
boldface indicates statistical significance compared to the Benjamini–Hochberg (B-H) critical value of .05. PTSD = posttraumatic stress disorder; DV = dependent variable; NACM = negative alternations in cognitions and mood; AAR = alterations in arousal and reactivity.
Count of specific positive memories
Results of linear regressions indicated that count of specific positive memories (i.e., number of specific positive memories recalled) was significantly and negatively associated with PTSD intrusion severity (R2 = .03; F[1, 201] = 5.25, p = .023), PTSD NACM severity (R2 = .02; F[1, 201] = 3.97, p = .048), PTSD AAR severity (R2 = .04; F[1, 201] = 7.53, p = .007), self-blame (R2 = .03; F[1, 201]= 5.53, p = .020), and positive affect (R2 = .06; F[1, 201]= 12.04, p = .001). Specifically, participants with greater PTSD intrusion severity (β = −.16, t = 2.29), PTSD NACM severity (β = −.14, t = 1.99), PTSD AAR severity (β = −.19, t = 2.74), self-blame (β = −.16, t = 2.35), and positive affect (β = −.24, t = 3.47) recalled fewer specific positive memories.
Accessibility of a specific positive memory
Results of linear regressions indicated that reported accessibility of a specific positive memory (i.e., self-reported ease of recalling details of a specific positive memory) was significantly and negatively associated with PTSD NACM severity (R2 = .03; F[1, 200] = 6.19, p = .014), PTSD AAR severity (R2 = .05; F[1, 200] = 9.37, p = .003), negative cognitions about the self (R2 = .04; F[1, 200] = 8.99, p = .003), and negative affect (R2 = .04; F[1, 200] = 8.47, p = .004). Specifically, participants with greater PTSD NACM severity (β = −.17, t = 2.49), PTSD AAR severity (β = −.21, t = 3.06), negative cognitions about the self (β = −.21, t = 3.00), and negative affect (β = −.20, t = 2.91) reported less accessibility of a specific positive memory.
Discussion
Drawing from the Contractor et al. (2018) conceptual model, the current study is the first to examine the relations between objective (i.e., count of specific positive memories) and subjective (i.e., reported accessibility of a specific positive memory) memory facets with a broad range of post-trauma mental health indicators. Broadly, within the current study, trauma-exposed individuals with more severe symptomatology demonstrated deficits in positive memory-related processes, consistent with past research and theory (e.g., Joormann, et al., 2007; Josephson, 1996; McNally, et al., 1994; Moradi, et al., 2014; Schönfeld and Ehlers, 2017). Specifically, participants with greater PTSD intrusion severity, PTSD NACM severity, PTSD AAR severity, self-blame, and positive affect recalled fewer specific positive memories. Further, participants with greater PTSD NACM severity, PTSD AAR severity, negative cognitions about the self, and negative affect reported greater difficulties accessing details of a specific positive memory. Across analyses, PTSD AAR symptoms, PTSD NACM symptoms, self-related post-trauma cognitions, and positive/negative affect were most consistently associated with positive memory processes. Results are important from an intervention perspective as they as they highlight difficulties with positive memory recall, which could be an intervention target.
Associations between Positive Memory Processes and Post-trauma Mental Health Indicators
There are a couple of possible factors explaining the associations between PTSD AAR severity and positive memory processes. First, neuroimaging results demonstrate that individuals with PTSD, who have higher hyperarousal symptoms, have lower hippocampal activity, which leads to poorer trauma-related memory encoding (Hayes et al., 2011). It is possible that chronic PTSD-related hyperarousal symptoms impair memory encoding and retrieval more broadly, including for positive memories. Indeed, chronic hyperarousal is associated with elevated glucocorticoid secretion, which negatively impacts the hippocampus (Kim and Diamond, 2002), thus negatively impacting memory-related processes over time. Second, PTSD AAR symptoms may diminish cognitive capacity for the retrieval of count/details of specific (positive) memories (Harvey, Bryant, & Dang, 1998). Thus, PTSD AAR symptoms, in particular, may increase difficulties accessing multiple specific positive memories, as well as the details of those memories. In regards to PTSD NACM severity, by virtue of the inherent greater negative affect and reduced positive affect associated with these symptoms (American Psychiatric Association, 2013), these symptoms may trigger more negative versus positive memories (associative network theory; Bower, 1981). Relatedly, the content of maladaptive cognitions associated with PTSD NACM symptoms may impede individuals’ capacities to retrieve numerous and detailed specific positive memories, because of an over-focus on negative aspects of experiences. Future work is necessary to better understanding these findings.
Although less robust than the findings for PTSD AAR severity and NACM severity, PTSD intrusions were negatively associated with the count of specific positive memories. Trauma-exposed individuals may block out traumatic memories to avoid aversive physiological/psychological distress and intrusive thoughts/flashbacks (PTSD intrusions symptoms; Dalgleish, Rolfe, Golden, Dunn, & Barnard, 2008; Hermans, Defranc, Raes, Williams, & Eelen, 2005; Moradi et al., 2008). Perhaps, some trauma-exposed individuals may simultaneously block out positive memories along with intrusive traumatic memories because they experience any intense emotion consequent to memory retrieval – regardless of its valence – as aversive (Weiss, et al., 2018). Separately, previous research suggests PTSD intrusion symptoms lead to depleted working memory capacity, which then limits memory retrieval (Kuyken and Brewin, 1995) and contributes to over-general memory retrieval (Brewin, Reynolds, & Tata, 1999). In this manner, increased PTSD intrusion severity may impact one’s capacity to retrieve specific positive memories. Taken together, these factors help to explain why PTSD-related intrusions were associated with recalling fewer specific positive memories.
Existing research and theory help to explain why affect (negative or positive) was consistently associated with both positive memory processes. Consistent with the mood-congruency hypothesis (Ingram, 1984; Teasdale, 1988), the presence of negative affect contributes to increased recall of negative memories, particularly among individuals with a ruminative style (McFarland and Buehler, 1998), making it potentially more difficult to retrieve specific positive memories. Following from this, higher levels of baseline negative affect (perhaps related to the experience of traumatic events and PTSD symptoms) may have negatively impacted participants’ ability to recall details of a specific positive memory with ease in the current study. Referencing positive affect, contrary to study hypotheses, participants with greater positive affect recalled fewer specific positive memories. Given that this was a cross-sectional study, regression results reference strength of predictive relations rather than direction or causality. Perhaps, the recall of positive memories is experienced as aversive (i.e., increased negative affect and/or lower positive affect) for some trauma-exposed participants due to difficulties regulating positive affect (Weiss, et al., 2018; Weiss, Nelson, Contractor, & Sullivan, in press), which may explain the negative association between positive affect and count of specific positive memories. Future research can empirically examine positive emotion regulation abilities as well as factors such as engaging in experiential processing (awareness of sensory and bodily experiences) that may mediate the relation between positive affect and positive memory processes (Gadeikis, Bos, Schweizer, Murphy, & Dunn, 2017).
In terms of post-trauma cognitions, self-blame was associated with fewer recalled specific positive memories, whereas negative cognitions about the self were associated with less accessibility of a specific positive memory. Trauma-exposed individuals have a negative biases for their self-schemas/concepts (Janoff-Bulman, 1992; Ono, et al., 2016), which may be amplified when asked to recall positive autobiographical memories that inherently are memories about the self (Conway and Pleydell-Pearce, 2000). To elaborate, trauma-exposed individuals may become more aware of the discrepancy between currently experienced negative self-concept and positive self-concept experienced during the recalled positive event (Agar, Kennedy, & King, 2006; O’Donnell, Elliott, Wolfgang, & Creamer, 2007), and may engage in further negative rumination about self (as seen with individuals reporting high levels of dysphoric mood; Hetherington and Moulds, 2015; Joormann and Siemer, 2004). This discrepancy may account for greater retrieval of traumatic (versus positive) memories in response to positive cues (Sutherland and Bryant, 2008a). Future research is necessary to better understand these findings, while accounting for the potentially moderating impact of co-occurring depressive disorders, processing mode of the memories (abstract/analytical versus concrete), and rumination based on existing research (Hetherington and Moulds, 2015; Joormann and Siemer, 2004).
Variability in Findings across Constructs
What is less clear is why some PTSD symptom clusters and associated constructs were correlated with the count of specific positive memories, but not accessibility of a specific memory, or vice versa, as well as why PTSD avoidance severity, negative cognitions about the world, and depression severity were not significantly correlated with either positive memory process. Such findings are inconsistent with existing literature (e.g., Blaney, 1986; Brittlebank, et al., 1993; D. M. Clark and Teasdale, 1982; Werner-Seidler and Moulds, 2011). A number of factors may help explain these differences, including (1) our examination of distinct PTSD symptom clusters, (2) our inclusion of both objective (i.e., count of specific positive memories recalled) and subjective (i.e., self-reported ease of accessing a specific positive memory) facets of positive memory processes, and (3) particular sample characteristics impacting obtained results. These factors are explored more in depth below.
First, most relevant prior work has examined overall PTSD symptom severity (i.e., total PTSD severity score; e.g., Bryant, et al., 2007; de Decker, et al., 2003; McNally, et al., 1994), rather than the distinct PTSD symptom clusters (i.e., AAR, NAMC, intrusions, and avoidance). Existing research indicates that the distinct PTSD symptoms clusters are differentially associated with various clinical correlates (Contractor, et al., 2016; Contractor, et al., 2014; Contractor, Weiss, Dolan, & Mota, in press; Silverstein, Dieujuste, Kramer, Lee, & Weathers, 2017); for example, PTSD NACM and AAR symptoms have been found to strongly relate with non-somatic depression compared to other PTSD symptom clusters (Contractor, Greene, et al., 2018) and PTSD externalizing behavior symptoms (part of the PTSD AAR symptom cluster) have been found to strongly associate with reckless/self-destructive behaviors compared to other PTSD symptom clusters (Contractor, et al., in press). Thus, examining the relation of these individual PTSD symptom clusters with distinct positive memory processes is informative and adds to the Contractor et al. (2018) conceptual model. In the context of the current study, it is not particularly surprising that some/all PTSD symptom clusters would differentially relate to particular positive memory processes; specifically, all PTSD symptom clusters (except avoidance) were associated with difficulties with positive memory processes. Future research would benefit from further examining why particular PTSD symptom clusters are associated with particular positive memory processes.
Second, results may be partially attributed to unique differences across the two examined positive memory processes. Indeed, the count of specific positive memories is an objective measure (count data) drawn from a performance-based task, whereas the ease of accessing a specific positive memory is a self-reported subjective measure of participants’ perceptions of their ability to recall details of a specific positive memory with ease. Given that these two measures capture different facets of positive memory processes and that emotional status differentially impacts performance across these facets (Smith, et al., 1996), it is not surprising that outcomes for each positive memory facet in the current study differs. Further research is needed to better understand underlying mechanisms that link some post-trauma facets to count of specific positive memories and other post-trauma facets to accessibility of a specific positive memory. Further, intervention development work will benefit from considering the distinct aspects of positive memory recall. For example, when considering how intentionally recalling and processing specific positive memories might impact post-trauma symptomatology over time, it is important to understand how these symptoms impact individuals’ abilities to recall any specific positive memory (count), as well as individuals’ perceived difficulties in accessing details of these positive memories (accessibility), in order to guide intervention development efforts. Third, study results may be partly attributed to the unique sample-related characteristics. For instance, individuals with a PTSD diagnosis seeking clinical care may be more strongly impacted by avoidance symptoms in positive memory retrieval tasks, as compared to our convenience-based community sample. Further replications and extensions of this work are necessary to better understand how these, and other aspects of positive memories, relate to PTSD and associated constructs.
Limitations and Future Directions
Some limitations need to be considered when interpreting our findings. First, we utilized self-report assessments; future research would benefit from using clinician-administered measures of the assessed constructs, such as the Clinician Administered PTSD Scale (Weathers et al., 2017). However, clinician-administered and self-report measures of PTSD are highly correlated (Monson et al., 2008), making the PCL-5 more practical to administer within the current study. Second, this was a convenience-based community sample with women overrepresented and minorities underrepresented. It will be necessary to determine whether these results generalize to more diverse clinical samples with more severe symptomatology. Importantly, this sample did experience substantial psychopathology, for which they had sought treatment (i.e., 62% had received mental health treatment) and had clinically significant PTSD symptoms (i.e., 42% of sample). Relatedly, given this level of symptomatology, we acknowledge potential ethical concerns involved with having participants identify traumas/symptoms (we only asked them to identify if and which traumatic event was experienced rather than to describe the traumatic event) and suicidal ideation in an online survey (Chandler and Shapiro, 2016). We had limited control over intervening in the event of participant distress given the anonymous nature of the online surveys; we, thus, provided several national mental health resources in the informed consent (e.g., telephone and website information for National Suicide Prevention Lifeline, National Sexual Assault Hotline, Veterans Crisis Line, Samaritans state-wide helpline), ensured IRB approval prior to conducting the study, and emphasized that participants could stop study participation at any time. Importantly, research has shown that inquiring about suicidal ideation does not induce/increase suicidal ideation (Dazzi, Gribble, Wessely, & Fear, 2014; Mathias et al., 2012).
Third, we acknowledge that in-person studies are ideal given better ability to intervene in the event of participant distress, better ability to assess comprehension and provide clarification, and ability to provide practice tests for performance-based tasks. This being said, it is worth noting that MTurk is widely used in trauma studies, and captures individuals with PTSD symptoms in a cost- and time-effective manner, with PTSD prevalence rates similar to those found in epidemiological studies (van Stolk-Cooke, et al., 2018). Moreover, MTurk and other online-recruitment platforms have been widely used in research which has included questions on suicidal ideation/thoughts (Contractor and Weiss, 2019; Shapiro, Chandler, & Mueller, 2013), and participants have reported comfort in disclosing mental health information with MTurk (Shapiro, et al., 2013). Fourth, although, we examined overall comprehension of the survey using validity checks, and provided detailed examples of what would (versus not) constitute a specific memory in response to two hypothetical cue words as part of the AMT instructions, we did not explicitly examine comprehension of the AMT task by providing practice items (Griffith, et al., 2009) given the online format of this task (Henderson, et al., 2002; Zinbarg, et al., 2006). Hence, it is possible some participants had difficulties comprehending the AMT, especially those experiencing greater psychological distress and/or PTSD severity, which can impede cognitive abilities (Vasterling, Brailey, Constans, & Sutker, 1998; Wilson et al., 2005). Additionally, we are unsure if eliciting positive (versus traumatic) memories on the AMT could have contributed to participant distress. Hence, future research would benefit from replicating this preliminary study by concurrently assessing comprehension and subsequent distress levels experienced by participants as they complete the tasks (including AMT). Finally, given that this is a relatively new area of inquiry, there may be other positive memory processes (e.g., vividness) impacted by PTSD and depressive symptom severity that would benefit from empirical examination.
Despite these limitations, this is the first study, to our knowledge, to delineate the specific relations of particular PTSD symptom clusters and associated post-trauma symptomatology with two distinct positive memory processes drawing from the Contractor et al. (2018) conceptual model. This work provides the impetus to further examine how positive memory processes are impacted among trauma-exposed populations and to utilize this information to inform intervention development efforts. Specifically, when providing therapeutic treatment to trauma-exposed individuals, practice recalling specific positive memories and/or their details may contribute to improving PTSD severity and cognitions about self while reducing negative affect (Contractor, Banducci, Jin, Keegan, & Weiss, in Review; Ono, et al., 2016). Future research can empirically examine these questions within the context of a clinical trial, as well as explore the contribution of positive memory recall deficits in particular to the onset/maintenance of post-trauma clinical symptoms.
Acknowledgments
We thank Ms. Stephanie Caldas who helped with the coding of memory data.
The research described here was supported, in part, by the National Institute on Drug Abuse under Grant Number K23DA039327 awarded to the last author.
Footnotes
Declaration of interest statement
The authors report no conflict of interest.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, AC, upon reasonable request.
Contributor Information
Ateka A. Contractor, Department of Psychology, University of North Texas, Denton, TX, USA
Anne N. Banducci, The National Center for PTSD at VA Boston Healthcare System, Boston, MA, USA; Boston University School of Medicine, Boston, MA, USA
Fallon Keegan, Department of Psychology, University of North Texas, Denton, TX, USA.
Nicole H. Weiss, Department of Psychology, University of Rhode Island, Kingston, RI, USA
References
- Agar E, Kennedy P, & King NS (2006). The role of negative cognitive appraisals in PTSD symptoms following spinal cord injuries. Behavioural and Cognitive Psychotherapy, 34, pp. 437–452. 10.1017/S1352465806002943 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.) Washington, DC: American Psychiatric Association. [Google Scholar]
- Arditte Hall KA, De Raedt R, Timpano KR, & Joormann J (2018). Positive memory enhancement training for individuals with major depressive disorder. Cognitive Behaviour Therapy, 47, pp. 155–168. 10.1080/16506073.2017.136429 Retrieved from Published online 22 Aug 2017 [DOI] [PubMed] [Google Scholar]
- Armour C, Contractor AA, Palmieri PA, & Elhai JD (2014). Assessing latent level associations between PTSD and dissociative factors: Is depersonalization and derealization related to PTSD factors more so than alternative dissociative factors? Psychological Injury and Law, 7, pp. 131–142. 10.1007/s12207-014-9196-9 [DOI] [Google Scholar]
- Askelund AD, Schweizer S, Goodyer IM, & van Harmelen AL (2019). Positive memory specificity is associated with reduced vulnerability to depression. Nature Human Behaviour, 3, pp. 265–273. 10.1101/329409 [DOI] [PubMed] [Google Scholar]
- Aupperle RL, Melrose AJ, Stein MB, & Paulus MP (2012). Executive function and PTSD: Disengaging from trauma. Neuropharmacology, 62, pp. 686–694. 10.1016/j.neuropharm.2011.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barger P, Benrend TS, Sharek DJ, & Sinar EF (2011). IO and the crowd: Frequently asked questions about using Mechanical Turk for research. The Industrial-Organizational Psychologist, 49(2), pp. 11–17. [Google Scholar]
- Barry TJ, Sze WY, & Raes F (2019). A meta-analysis and systematic review of Memory Specificity Training (MeST) in the treatment of emotional disorders. Behaviour Research and Therapy, 116, pp. 36–51. 10.1016/j.brat.2019.02.001 [DOI] [PubMed] [Google Scholar]
- Beck AT (1976). Cognitive therapy and the emotional disorders New York, NY: International Universities Press. [Google Scholar]
- Beck JG, Coffey SF, Palyo SA, Gudmundsdottir B, Miller LM, & Colder CR (2004). Psychometric properties of the Posttraumatic Cognitions Inventory (PTCI): A replication with motor vehicle accident survivors. Psychological Assessment, 16, pp. 289–298. doi: 0.1037/1040-3590.16.3.289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate. A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological), 57, pp. 289–300. Retrieved from Retrieved from: https://www.jstor.org/stable/2346101 [Google Scholar]
- Bernsten D, & Rubin DC (2007). When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology, 21, pp. 417–431. 10.1002/acp.1290 [DOI] [Google Scholar]
- Blaney PH (1986). Affect and memory: A review. Psychological Bulletin, 99, pp. 229–246. 10.1037/0033-2909.99.2.229 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, pp. 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bonde JP, Utzon-Frank N, Bertelsen M, Borritz M, Eller NH, & Nordentoft M (2016). Risk of depressive disorder following disasters and military deployment: Systematic review with meta-analysis. The British Journal of Psychiatry, 208, pp. 330–336. 10.1192/bjp.bp.114.157859 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28, pp. 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Bower GH (1981). Mood and memory. American Psychologist, 36, pp. 129–148. [DOI] [PubMed] [Google Scholar]
- Boyacioglu I, & Akfirat S (2015). Development and psychometric properties of a new measure for memory phenomenology: The Autobiographical Memory Characteristics Questionnaire. Memory, 23, pp. 1070–1092. 10.1080/09658211.2014.953960 [DOI] [PubMed] [Google Scholar]
- Brewin CR, & Holmes EA (2003). Psychological theories of posttraumatic stress disorder. Clinical Psychology Review, 23, pp. 339–376. 10.1016/S0272-7358(03)00033-3 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Reynolds M, & Tata P (1999). Autobiographical memory processes and the course of depression. Journal of Abnormal Psychology, 108, pp. 511–517. 10.1037/0021-843X.108.3.511 [DOI] [PubMed] [Google Scholar]
- Brittlebank AD, Scott J, Williams JM, & Ferrier IN (1993). Autobiographical memory in depression: State or trait marker? The British Journal of Psychiatry, 162, pp. 118–121. 10.1192/bjp.162.1.118 [DOI] [PubMed] [Google Scholar]
- Bryant RA, Sutherland K, & Guthrie RM (2007). Impaired specific autobiographical memory as a risk factor for posttraumatic stress after trauma. Journal of Abnormal Psychology, 116, pp. 837–841. 10.1037/0021-843X.116.4.837 [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk a new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6, pp. 3–5. 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Callahan JL, Maxwell K, & Janis BM (2019). The role of overgeneral memories in PTSD and implications for treatment. Journal of Psychotherapy Integration, 29, pp. 32–41. 10.1037/int0000116 [DOI] [Google Scholar]
- Chandler J, & Shapiro D (2016). Conducting clinical research using crowdsourced convenience samples. Annual Review of Clinical Psychology, 12, pp. 53–81. 10.1146/annurev-clinpsy-021815-093623 [DOI] [PubMed] [Google Scholar]
- Clark DM, & Teasdale JD (1982). Diurnal variation in clinical depression and accessibility of memories of positive and negative experiences. Journal of Abnormal Psychology, 91, pp. 87–95. 10.1037/0021-843X.91.2.87 [DOI] [PubMed] [Google Scholar]
- Clark LF, & Collins JE (1993). Remembering old flames: How the past affects assessments of the present. Personality and Social Psychology Bulletin, 19, pp. 399–408. 10.1177/0146167293194005 [DOI] [Google Scholar]
- Contractor AA, Armour C, Forbes D, & Elhai JD (2016). PTSD’s underlying dimensions and their relation with impulsivity facets. The Journal of Nervous & Mental Disease, 204, pp. 20–25. 10.1097/NMD.0000000000000417 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Banducci AN, Jin L, Keegan F, & Weiss NH (in Review). Effects of processing positive memories on posttrauma mental health: A preliminary study Manuscript submitted for publication [DOI] [PMC free article] [PubMed]
- Contractor AA, Brown LA, Caldas S, Banducci AN, Taylor DJ, Armour C, & Shea MT (2018). Posttraumatic stress disorder and positive memories: Clinical considerations. Journal of Anxiety Disorders, 58, pp. 22–32. 10.1016/j.janxdis.2018.06.007 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Durham TA, Brennan JA, Armour C, Wutrick HR, Frueh CB, & Elhai JD (2014). DSM-5 PTSD’s symptom dimensions and relations with major depression’s symptom dimensions in a primary care sample. Psychiatry Research, 215, pp. 146–153. 10.1016/j.psychres.2013.10.015 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Frankfurt S, Weiss NH, & Elhai JD (2017). Latent-level relations between DSM-5 PTSD symptom clusters and problematic smartphone use. Computers in Human Behavior, 72, pp. 170–177. 10.1016/j.chb.2017.02.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Greene T, Dolan M, & Elhai JD (2018). Relations between PTSD and depression symptom clusters in samples differentiated by PTSD diagnostic status. Journal of Anxiety Disorders, 59, pp. 17–26. 10.1016/j.janxdis.2018.08.004 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Roley-Roberts ME, Lagdon S, & Armour C (2017). Heterogeneity in patterns of DSM-5 posttraumatic stress disorder and depression symptoms: Latent profile analyses. Journal of Affective Disorders, 212, pp. 17–24. 10.1016/j.jad.2017.01.029 [DOI] [PubMed] [Google Scholar]
- Contractor AA, & Weiss NH (2019). Typologies of PTSD clusters and reckless/self-destructive behaviors: A latent profile analysis. Psychiatry Research, 272, pp. 682–691. 10.1016/j.psychres.2018.12.124 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Weiss NH, Dolan M, & Mota N (in press). Examination of the structural relations between PTSD symptoms and reckless/self-destructive behaviors. International Journal of Stress Management [DOI] [PMC free article] [PubMed]
- Conway MA, & Pleydell-Pearce CW (2000). The construction of autobiographical memories in the self-memory system. Psychological Review, 107, pp. 261–268. 10.1037/0033-295X.107.2.261 [DOI] [PubMed] [Google Scholar]
- Crawford JR, & Henry JD (2004). The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 43, pp. 245–265. 10.1348/0144665031752934 [DOI] [PubMed] [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1, pp. 16–29. 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- Dalgleish T, Rolfe J, Golden AM, Dunn BD, & Barnard PJ (2008). Reduced autobiographical memory specificity and posttraumatic stress: Exploring the contributions of impaired executive control and affect regulation. Journal of Abnormal Psychology, 117, pp. 236–241. 10.1037/0021-843X.117.1.236 [DOI] [PubMed] [Google Scholar]
- Dazzi T, Gribble R, Wessely S, & Fear NT (2014). Does asking about suicide and related behaviours induce suicidal ideation? What is the evidence? Psychological Medicine, 44, pp. 3361–3363. 10.1017/S0033291714001299 [DOI] [PubMed] [Google Scholar]
- de Decker A, Hermans D, Raes F, & Eelen P (2003). Autobiographical memory specificity and trauma in inpatient adolescents. Journal of Clinical Child and Adolescent Psychology, 32, pp. 22–31. 10.1207/15374420360533031 [DOI] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behavior Research and Therapy, 38, pp. 319–324. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Fani N, Tone EB, Phifer J, Norrholm SD, Bradley B, Ressler KJ, … Jovanovic T (2012). Attention bias toward threat is associated with exaggerated fear expression and impaired extinction in PTSD. Psychological Medicine, 42, pp. 533–543. 10.1017/S0033291711001565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Lansac V, & Crespo M (2017). Presentation of the Coding and Assessment System for Narratives of Trauma (CASNOT): Application in Spanish battered women and preliminary analyses. The Spanish Journal of Psychology, 20, pp. 1–12. 10.1017/sjp.2017.31 [DOI] [PubMed] [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11, pp. 303–314. 10.1037/1040-3590.11.3.303 [DOI] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, pp. 20–35. 10.1037//0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Foland-Ross LC, Cooney RE, Joormann J, Henry ML, & Gotlib IH (2014). Recalling happy memories in remitted depression: a neuroimaging investigation of the repair of sad mood. Cognitive, Affective, & Behavioral Neuroscience, 14, pp. 818–826. 10.3758/s13415-013-0216-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, pp. 218–226. 10.1037/0003-066X.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadeikis D, Bos N, Schweizer S, Murphy F, & Dunn B (2017). Engaging in an experiential processing mode increases positive emotional response during recall of pleasant autobiographical memories. Behaviour Research and Therapy, 92, pp. 68–76. 10.1016/j.brat.2017.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith JW, Sumner JA, Debeer E, Raes F, Hermans D, Mineka S, … Craske MG (2009). An item response theory/confirmatory factor analysis of the Autobiographical Memory Test. Memory, 17, pp. 609–623. 10.1080/09658210902939348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, & Muñoz RF (1995). Emotion regulation and mental health. Clinical Psychology: Science and Practice, 2, pp. 151–164. 10.1111/j.1468-2850.1995.tb00036.x [DOI] [Google Scholar]
- Harvey AG, Bryant RA, & Dang ST (1998). Autobiographical memory in acute stress disorder. Journal of Consulting and Clinical Psychology, 66, pp. 500–506. 10.1037/0022-006X.66.3.500 [DOI] [PubMed] [Google Scholar]
- Hauer BJ, Wessel I, Engelhard IM, Peeters LL, & Dalgleish T (2009). Prepartum autobiographical memory specificity predicts post-traumatic stress symptoms following complicated pregnancy. Memory, 17, pp. 544–556. 10.1080/09658210902953836 [DOI] [PubMed] [Google Scholar]
- Hayes JP, LaBar KS, McCarthy G, Selgrade E, Nasser J, Dolcos F, & Morey RA (2011). Reduced hippocampal and amygdala activity predicts memory distortions for trauma reminders in combat-related PTSD. Journal of Psychiatric Research, 45, pp. 660–669. 10.1016/j.jpsychires.2010.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes JP, VanElzakker MB, & Shin LM (2012). Emotion and cognition interactions in PTSD: A review of neurocognitive and neuroimaging studies. Frontiers in integrative neuroscience, 6(89) 10.3389/fnint.2012.00089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson D, Hargreaves I, Gregory S, & Williams JMG (2002). Autobiographical memory and emotion in a non-clinical sample of women with and without a reported history of childhood sexual abuse. British journal of clinical psychology, 41, pp. 129–141. 10.1348/014466502163921 [DOI] [PubMed] [Google Scholar]
- Hermans D, Defranc A, Raes F, Williams JMG, & Eelen P (2005). Reduced autobiographical memory specificity as an avoidant coping style. British journal of clinical psychology, 44, pp. 583–589. 10.1348/014466505X53461 [DOI] [PubMed] [Google Scholar]
- Hetherington K, & Moulds ML (2015). Abstract recall of a happy memory to repair sad mood in dysphoria: A possible link to negative cognition. Memory, 23, pp. 817–828. 10.1080/09658211.2014.929149 [DOI] [PubMed] [Google Scholar]
- Hitchcock C, Werner-Seidler A, Blackwell SE, & Dalgleish T (2017). Autobiographical episodic memory-based training for the treatment of mood, anxiety and stress-related disorders: A systematic review and meta-analysis. Clinical Psychology Review, 52, pp. 92–107. 10.1016/j.cpr.2016.12.003 [DOI] [PubMed] [Google Scholar]
- Ho ML, & Brass SD (2011). Obstructive sleep apnea. Neurology International, 3(15) 10.4081/ni.2011.e15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland AC, & Kensinger EA (2010). Emotion and autobiographical memory. Physics of Life Reviews, 7, pp. 88–131. 10.1016/j.plrev.2010.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram RE (1984). Toward an information-processing analysis of depression. Cognitive Therapy and Research, 8, pp. 443–477. 10.1007/BF01173284 [DOI] [Google Scholar]
- Janoff-Bulman R (1992). Shattered assumptions: Toward a new psychology of trauma New York, NY: Free Press. [Google Scholar]
- Janssen SM, Hearne TL, & Takarangi MK (2015). The relation between self-reported PTSD and depression symptoms and the psychological distance of positive and negative events. Journal of Behavior Therapy and Experimental Psychiatry, 48, pp. 177–184. 10.1016/j.jbtep.2015.04.002 [DOI] [PubMed] [Google Scholar]
- Joormann J, & Siemer M (2004). Memory accessibility, mood regulation, and dysphoria: Difficulties in repairing sad mood with happy memories? Journal of Abnormal Psychology, 113, pp. 179–188. 10.1037/0021-843X.113.2.179 [DOI] [PubMed] [Google Scholar]
- Joormann J, Siemer M, & Gotlib IH (2007). Mood regulation in depression: Differential effects of distraction and recall of happy memories on sad mood. Journal of Abnormal Psychology, 116, pp. 484–490. 10.1037/0021-843X.116.3.484 [DOI] [PubMed] [Google Scholar]
- Josephson BR (1996). Mood regulation and memory: Repairing sad moods with happy memories. Cognition and Emotion, 10, pp. 437–444. 10.1080/026999396380222 [DOI] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, & Bender ME (1985). A behavioral approach to assessing and treating post-traumatic stress disorder in Vietnam veterans. In Figley CR (Ed.), Trauma and its wake (pp. 257–294). Bristol, PA: Brunner/Mazel. [Google Scholar]
- Kim JJ, & Diamond DM (2002). The stressed hippocampus, synaptic plasticity and lost memories. Nature Reviews Neuroscience, 3, pp. 453–462. 10.1038/nrn849 [DOI] [PubMed] [Google Scholar]
- Kleim B, & Ehlers A (2008). Reduced autobiographical memory specificity predicts depression and posttraumatic stress disorder after recent trauma. Journal of Consulting and Clinical Psychology, 76, pp. 231–242. 10.1037/0022-006X.76.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloepfer C, Riemann D, Nofzinger EA, Feige B, Unterrainer J, O’, R., … Nissen C (2009). Memory before and after sleep in patients with moderate obstructive sleep apnea. Journal of Clinical Sleep Medicine, 5, pp. 540–548. [PMC free article] [PubMed] [Google Scholar]
- Korrelboom K, Maarsingh M, & Huijbrechts I (2012). Competitive Memory Training (COMET) for treating low self-esteem in patients with depressive disorders: A randomized clinical trial. Depression and Anxiety, 29, pp. 102–110. 10.1002/da.20921 [DOI] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32, pp. 509–515. 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ 9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, pp. 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuyken W, & Brewin CR (1995). Autobiographical memory functioning in depression and reports of early abuse. Journal of Abnormal Psychology, 104, pp. 585–591. 10.1037/0021-843X.104.4.585 [DOI] [PubMed] [Google Scholar]
- Landis JR, & Koch GG (1977). The measurement of observer agreement for categorical data. Biometrics, 1, pp. 159–174. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, & Weathers F (2000). Emotional processing in posttraumatic stress disorder. Journal of Abnormal Psychology, 109, pp. 26–39. 10.1037/0021-843X.109.1.26 [DOI] [PubMed] [Google Scholar]
- Luchetti M, & Sutin AR (2016). Measuring the phenomenology of autobiographical memory: A short form of the Memory Experiences Questionnaire. Memory, 24, pp. 592–602. 10.1080/09658211.2015.1031679 [DOI] [PubMed] [Google Scholar]
- Mathias CW, Michael Furr R, Sheftall AH, Hill-Kapturczak N, Crum P, & Dougherty DM (2012). What’s the harm in asking about suicidal ideation? Suicide and Life-Threatening Behavior, 42, pp. 341–351. 10.1111/j.1943-278X.2012.0095.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matt GE, Vázquez C, & Campbell WK (1992). Mood-congruent recall of affectively toned stimuli: A meta-analytic review. Clinical Psychology Review, 12, pp. 227–255. 10.1016/0272-7358(92)90116-P [DOI] [Google Scholar]
- McFarland C, & Buehler R (1998). The impact of negative affect on autobiographical memory: The role of self-focused attention to moods. Journal of Personality and Social Psychology, 75, pp. 1424–1440. 10.1037//0022-3514.75.6.1424 [DOI] [PubMed] [Google Scholar]
- McNally RJ, Lasko NB, Macklin ML, & Pitman RK (1995). Autobiographical memory disturbance in combat-related posttraumatic stress disorder. Behavior Research and Therapy, 33, pp. 619–630. 10.1016/0005-7967(95)00007-K [DOI] [PubMed] [Google Scholar]
- McNally RJ, Litz BT, Prassas A, Shin LM, & Weathers FW (1994). Emotional priming of autobiographical memory in post-traumatic stress disorder. Cognition and Emotion, 8, pp. 351–367. 10.1080/02699939408408946 [DOI] [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17, pp. 437–455. 10.1037/a0028085 [DOI] [PubMed] [Google Scholar]
- Moradi AR, Herlihy J, Yasseri G, Shahraray M, Turner S, & Dalgleish T (2008). Specificity of episodic and semantic aspects of autobiographical memory in relation to symptoms of posttraumatic stress disorder (PTSD). Acta Psychologica, 127, pp. 645–653. 10.1016/j.actpsy.2007.11.001 [DOI] [PubMed] [Google Scholar]
- Moradi AR, Moshirpanahi S, Parhon H, Mirzaei J, Dalgleish T, & Jobson L (2014). A pilot randomized controlled trial investigating the efficacy of MEmory Specificity Training in improving symptoms of posttraumatic stress disorder. Behavior Research and Therapy, 56, pp. 68–74. 10.1016/j.brat.2014.03.002 [DOI] [PubMed] [Google Scholar]
- Murphy FC, Sahakian BJ, Rubinsztein JS, Michael A, Rogers RD, Robbins TW, & Paykel ES (1999). Emotional bias and inhibitory control processes in mania and depression. Psychological Medicine, 29, pp. 1307–1321. 10.1017/S0033291799001233 [DOI] [PubMed] [Google Scholar]
- Neshat-Doost HT, Dalgleish T, Yule W, Kalantari M, Ahmadi SJ, Dyregrov A, & Jobson L (2013). Enhancing autobiographical memory specificity through cognitive training: An intervention for depression translated from basic science. Clinical Psychological Science, 1, pp. 84–92. 10.1177/2167702612454613 [DOI] [Google Scholar]
- O’Donnell ML, Elliott P, Wolfgang BJ, & Creamer M (2007). Posttraumatic appraisals in the development and persistence of posttraumatic stress symptoms. Journal of Traumatic Stress, 20, pp. 173–182. 10.1002/jts.20198 [DOI] [PubMed] [Google Scholar]
- Ono M, Devilly GJ, & Shum DH (2016). A meta-analytic review of overgeneral memory: The role of trauma history, mood, and the presence of posttraumatic stress disorder. Psychological Trauma Theory Research Practice and Policy, 8, pp. 157–164. 10.1037/tra0000027 [DOI] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, & Davidenko N (2009). Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology, 45, pp. 867–872. 10.1016/j.jesp.2009.03.009 [DOI] [Google Scholar]
- Panagioti M, Gooding PA, & Tarrier N (2012). An empirical investigation of the effectiveness of the broad-minded affective coping procedure (BMAC) to boost mood among individuals with posttraumatic stress disorder (PTSD). Behaviour Research and Therapy, 50, pp. 589–595. 10.1016/j.brat.2012.06.005 [DOI] [PubMed] [Google Scholar]
- Post LM, Feeny NC, Zoellner LA, & Connell AM (2016). Post-traumatic stress disorder and depression co-occurrence: Structural relations among disorder constructs and trait and symptom dimensions. Psychology and Psychotherapy: Theory, Research and Practice, 89, pp. 418–434. 10.1111/papt.12087 [DOI] [PubMed] [Google Scholar]
- Quoidbach J, Mikolajczak M, & Gross JJ (2015). Positive interventions: An emotion regulation perspective. Psychological Bulletin, 141, pp. 655–693. 10.1037/a0038648 [DOI] [PubMed] [Google Scholar]
- Rusting CL, & DeHart T (2000). Retrieving positive memories to regulate negative mood: Consequences for mood-congruent memory. Journal of Personality and Social Psychology, 78, pp. 737–752. 10.1037/0022-3514.78.4.737 [DOI] [PubMed] [Google Scholar]
- Rusting CL, & Larsen RJ (1998). Personality and cognitive processing of affective information. Personality and Social Psychology Bulletin, 24, pp. 200–213. 10.1177/0146167298242008 [DOI] [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 26, pp. 299–309. 10.1002/jts.21814 [DOI] [PubMed] [Google Scholar]
- Schmidt GB (2015). Fifty days an MTurk worker: The social and motivational context for Amazon Mechanical Turk workers. Industrial and Organizational Psychology, 8, pp. 165–171. 10.1017/iop.2015.20 [DOI] [Google Scholar]
- Schnurr PP (2017). Focusing on trauma-focused psychotherapy for posttraumatic stress disorder. Current Opinion in Psychology, 14, pp. 56–60. 10.1016/j.copsyc.2016.11.005 [DOI] [PubMed] [Google Scholar]
- Schönfeld S, & Ehlers A (2017). Posttraumatic stress disorder and autobiographical memories in everyday life. Clinical Psychological Science, 5, pp. 325–340. 10.1177/2167702616688878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligowski AV, & Orcutt HK (2016). Support for the 7-factor hybrid model of PTSD in a community sample. Psychological Trauma: Theory, Research, Practice, and Policy, 8, pp. 218–221. 10.1037/tra0000104 [DOI] [PubMed] [Google Scholar]
- Shapiro DN, Chandler J, & Mueller PA (2013). Using Mechanical Turk to study clinical populations. Clinical Psychological Science, 1, pp. 213–220. 10.1177/2167702612469015 [DOI] [Google Scholar]
- Silverstein MW, Dieujuste N, Kramer LB, Lee DJ, & Weathers FW (2017). Construct validation of the hybrid model of posttraumatic stress disorder: Distinctiveness of the new symptom clusters. Journal of Anxiety Disorders, 54, pp. 17–23. 10.1016/j.janxdis.2017.12.003 [DOI] [PubMed] [Google Scholar]
- Simmons JP, Nelson LD, & Simonsohn U (2011). False-positive psychology: Undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychological Science, 22, pp. 1359–1366. 10.1177/0956797611417632 [DOI] [PubMed] [Google Scholar]
- Smith GE, Petersen RC, Ivnik RJ, Malec JF, & Tangalos EG (1996). Subjective memory complaints, psychological distress, and longitudinal change in objective memory performance. Psychology and Aging, 11, pp. 272–279. 10.1037/0882-7974.11.2.272 [DOI] [PubMed] [Google Scholar]
- Snyder M, & White P (1982). Moods and memories: Elation, depression, and the remembering of the events of one’s life. Journal of Personality, 50, pp. 149–167. 10.1111/j.1467-6494.1982.tb01020.x [DOI] [PubMed] [Google Scholar]
- Sutherland K, & Bryant RA (2008a). Autobiographical memory and the self-memory system in posttraumatic stress disorder. Journal of Anxiety Disorders, 22, pp. 555–560. 10.1016/j.janxdis.2007.03.008 [DOI] [PubMed] [Google Scholar]
- Sutherland K, & Bryant RA (2008b). Social problem solving and autobiographical memory in posttraumatic stress disorder. Behavior Research and Therapy, 46, pp. 154–161. 10.1016/j.brat.2007.10.005 [DOI] [PubMed] [Google Scholar]
- Sutin AR, & Robins RW (2007). Phenomenology of autobiographical memories: The Memory Experiences Questionnaire. Memory, 15, pp. 390–314. 10.1080/09658210701256654 [DOI] [PubMed] [Google Scholar]
- Teasdale JD (1988). Cognitive vulnerability to persistent depression. Cognition and Emotion, 2, pp. 247–274. 10.1080/02699938808410927 [DOI] [Google Scholar]
- Thomas KA, & Clifford S (2017). Validity and mechanical turk: An assessment of exclusion methods and interactive experiments. Computers in Human Behavior, 77, pp. 184–197. 10.1016/j.chb.2017.08.038 [DOI] [Google Scholar]
- Tomarkenand AJ, & Keener AD (1998). Frontal brain asymmetry and depression: A self-regulatory perspective. Cognition and Emotion, 12, pp. 387–420. 10.1080/026999398379655 [DOI] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, & Price M (2018). Crowdsourcing trauma: Psychopathology in a trauma-exposed sample recruited via Mechanical Turk. Journal of Traumatic Stress, 31, pp. 549–557. 10.1002/jts.22303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasterling JJ, Brailey K, Constans JI, & Sutker PB (1998). Attention and memory dysfunction in posttraumatic stress disorder. Neuropsychology, 12, pp. 125–133. 10.1037/0894-4105.12.1.125 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, pp. 1063–1070. Retrieved from Retrived from: https://www.ncbi.nlm.nih.gov/pubmed/3397865 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Life Events Checklist for DSM-5 (LEC-5) Instrument available from the National Center for PTSD at www.ptsd.va.gov
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, & Marx BP (2017). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30, pp. 383–395. 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5) Scale available from the National Center for PTSD at www.ptsd.va.gov. Retrieved Date.
- Weiss NH, Dixon-Gordon KL, Peasant C, & Sullivan TP (2018). An examination of the role of difficulties regulating positive emotions in posttraumatic stress disorder. Journal of Traumatic Stress, 31, pp. 775–780. 10.1002/jts.22330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Nelson R, Contractor AA, & Sullivan TP (in press). Emotion dysregulation and posttraumatic stress disorder: A test of the incremental role of difficulties regulating positive emotions. Anxiety, Stress and Coping [DOI] [PMC free article] [PubMed]
- Werner-Seidler A, & Moulds ML (2011). Autobiographical memory characteristics in depression vulnerability: Formerly depressed individuals recall less vivid positive memories. Cognition and Emotion, 25, pp. 1087–1103. 10.1080/02699931.2010.531007 [DOI] [PubMed] [Google Scholar]
- Werner-Seidler A, Tan L, & Dalgleish T (2017). The vicissitudes of positive autobiographical recollection as an emotion regulation strategy in depression. Clinical Psychological Science, 5, pp. 26–36. 10.1177/2167702616647922 [DOI] [Google Scholar]
- Williams J, Ellis NC, Tyers C, Healy H, Rose G, & Macleod AK (1996). The specificity of autobiographical memory and imageability of the future. Memory & Cognition, 24, pp. 116–125. 10.3758/bf03197278 [DOI] [PubMed] [Google Scholar]
- Williams JM, & Broadbent K (1996). Autobiographical memory in suicide attempters. Journal of Abnormal Psychology, 95, pp. 144–149. 10.1037/0021-843X.95.2.144 [DOI] [PubMed] [Google Scholar]
- Williams JMG, Barnhofer T, Crane C, Hermans D, Raes F, Watkins E, & Dalgleish T (2007). Autobiographical memory specificity and emotional disorder. Psychological Bulletin, 133, pp. 122–148. 10.1037/0033-2909.133.1.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS, Bennett DA, de Leon CFM, Bienias JL, Morris MC, & Evans DA (2005). Distress proneness and cognitive decline in a population of older persons. Psychoneuroendocrinology, 30, pp. 11–17. 10.1016/j.psyneuen.2004.04.005 [DOI] [PubMed] [Google Scholar]
- Wing JF, Schutte NS, & Byrne B (2006). The effect of positive writing on emotional intelligence and life satisfaction. Journal of Clinical Psychology, 62, pp. 1291–1302. 10.1002/jclp.20292 [DOI] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, … Litz BT (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28, pp. 1392–1403. 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Rekart KN, & Mineka S (2006). Autobiographical memory in dysphoric and non-dysphoric college students using a computerised version of the AMT. Cognition and Emotion, 20, pp. 506–515. 10.1080/02699930500341318 [DOI] [PubMed] [Google Scholar]