Sir,
Epidural abscess is a rare complication of epidural anaesthesia seen despite the adoption of best sterile techniques. Surgical drainage along with intravenous antibiotics is the standard treatment for an epidural abscess. With the advent of early and more accurate diagnosis from MRI, more patients with spinal epidural abscess are being treated by medical management alone. Here, we present a case of an epidural abscess managed successfully with antibiotics alone, without any surgical intervention.
A 52-year-old gentleman, ASA-I (American Society of Anesthesiologists), diagnosed with Carcinoma stomach was planned for a gastrectomy. A 16G epidural catheter was inserted prior to induction of general anaesthesia. A face mask, sterile gown and gloves were worn by the anaesthesiologist for the procedure. The insertion site was disinfected with chlorhexidine scrub and solution. The surgery that followed was uneventful.
Postoperatively, the patient was comfortable on an epidural infusion, and epidural site was inspected daily for any signs of infection as per hospital protocols. On the 4th post-operative day, the patient complained of pain at the epidural injection site and had a fever spike. On examination, a swelling at the epidural insertion site with minimal pus-like discharge was noticed. White blood cell count (WBC) was 11,340/mm3. There was no motor or sensory deficit. MRI spine within the next hour showed an epidural collection from D7-D11, a cranio-caudal length of 10 cm, with a maximum thickness of seven mm [Figure 1a]. The epidural catheter was removed as per American Society of Regional Anaesthesia (ASRA) guidelines. Intravenous (IV) Vancomycin and IV Meropenem were started. Epidural catheter tip and wound site cultures both grew Staphylococcus aureus and Klebsiella. According to culture sensitivity report, IV Vancomycin was continued for 14 days. The patient was then monitored for motor sensory deficit and explained about need for urgent surgical decompression in case of any such deficit. WBC decreased and there was no further fever spike. MRI done subsequently on day 14 revealed complete resolution of the abscess [Figure 1b]. Patient was discharged on T. Augmentin for 14 days, and was later followed up regularly with no fresh complaints.
Figure 1.
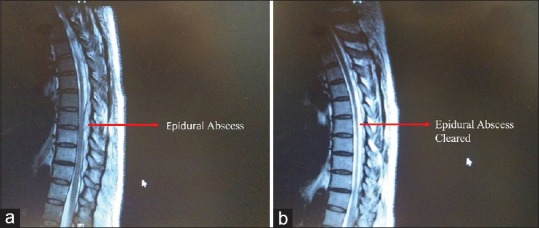
(a) Epidural Abscess observed in MRI on Day one; (b) Epidural Abscess cleared in MRI after 14 days of Intravenous (IV) antibiotics
Infection can originate from the skin flora, by haematological spread of bacteria or via contaminated local anaesthetic. We use chlorhexidine solution for skin disinfection as recommended by Association of Anaesthetists of Great Britain and Ireland,[1] as it is effective against nearly all bacteria and yeasts. Antiseptics have proved to be effective in decontaminating the transient skin flora but not the deeply placed resident flora. The spread of microorganisms via a contaminated anaesthetic solution is unlikely as a new vial is used for each patient. Contamination was further prevented by the use of an in-line bacterial filter.[2] Cancer itself could be a risk factor for development of an abscess in this patient.[3]
Successful medical management in multiple patients was first reported in 1992. Since then, medical treatment has been reported sporadically in literature.[4,5] Staphylococcus aureus is the most common organism implicated in epidural abscess[2,4] isolated in more than 50% of patients while, aerobic and anaerobic Streptococci account for approximately 15% of the isolates. Empirical antibiotics should be started to cover these organisms until a culture report is available. Specific antibiotics can then be started as per sensitivity patterns. A stringent follow up is needed to check for any neurosensory deficit and emergency surgery for decompression is always a possibility and should be available. Risk factors for failure of medical management include diabetes, bacteraemia, age over 65 years, MRSA as causative organism, C-reactive protein level >115 mg/L, leukocytosis >12 × 109 white blood cells/L and positive blood cultures.[4,6] Many studies showed no significant difference between the outcomes of patients treated medically and those treated surgically.[7,8] Curry and colleagues[6] found a statistically significant difference in the results of patients on medical or surgical treatment, with 49% cases failing medical treatment and requiring surgery subsequently. However, 39% of these patients had presented with mild weakness from the beginning and required immediate surgery, but were managed conservatively. This highlights the importance of selecting a management strategy for patients based on the findings of their initial neurological examination.
We chose conservative medical management for our patient as he did not have any neurological deficit nor did he have any risk factors for failure of medical treatment. This was the first patient in whom we managed an epidural abscess conservatively. Over the past 10 years, we have had 4 cases of an epidural abscess, all of whom presented with neurological deficits and were managed surgically along with intravenous antibiotics.
Epidural abscesses can be managed medically with continuous guarded supervision in patients without neurological deficits and at a low risk of failure of medical therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank the patient for allowing us to publish this report. Valid informed consent was taken from the patient.
REFERENCES
- 1.Campbell JP, Plaat F, Checketts MR, Bogod D, Tighe S, Moriarty A, Koerner R. Safety guideline: Skin antisepsis for central neuraxial blockade. Association of Anaesthetists of Great Britain and Ireland. Obstetric Anaesthetists' Association. Regional Anaesthesia UK. Association of Paediatric Anaesthetists of Great Britain and Ireland. doi: 10.1111/anae.12844. [DOI] [PubMed] [Google Scholar]
- 2.Wallace MR. Epidural abscess treatment and Management Medscape. 2018 Jul; Updated. [Google Scholar]
- 3.Rolston KV. Infections in cancer patients with solid tumors: A review. Infect Dis Ther. 2017;6:69–83. doi: 10.1007/s40121-017-0146-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wheeler D, Keiser P, Rigamonti D, Keay S. Medical management of spinal epidural abscesses: Case report and review. Clin Infect Dis. 1992;15:22–7. doi: 10.1093/clinids/15.1.22. [DOI] [PubMed] [Google Scholar]
- 5.Mampalam TJ, Rosegay H, Andrews BT, Rosenblum ML, Pitts LH. Nonoperative treatment of spinal epidural infections. J Neurosurg. 1989;71:208–10. doi: 10.3171/jns.1989.71.2.0208. [DOI] [PubMed] [Google Scholar]
- 6.Curry WT, Jr, Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: Clinical presentation, management, and outcome. Surg Neurol. 2005;63:364–371. doi: 10.1016/j.surneu.2004.08.081. [DOI] [PubMed] [Google Scholar]
- 7.Kim SD, Melikian R, Ju KL, Zurakowski D, Wood KB, Bono CM, et al. Independent predictors of failure of nonoperative management of spinal epidural abscesses. Spine J. 2013;14:1673–9. doi: 10.1016/j.spinee.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Arko L, 4th, Quach E, Nguyen V, Chang D, Sukul V, Kim BS. Medical and surgical management of spinal epidural abscess: A systematic review. Neurosurg Focus. 2014;37:E4. doi: 10.3171/2014.6.FOCUS14127. [DOI] [PubMed] [Google Scholar]


