Abstract
Purpose: This study updates psychiatric epidemiological research by providing recent prevalence estimates of major depression and alcohol and illicit drug abuse or dependence among sexual minority (SM) adults.
Methods: Using the 2015 National Survey on Drug Use and Health, we estimated prevalence differences between SM and heterosexual adults, and within SM subgroups, with logistic regression models.
Results: Bisexual adults faced an increased burden across all outcomes compared with other SM adults. Gay males had the highest prevalence of alcohol and illicit drug abuse or dependence.
Conclusions: Future research must consider sex differences within SM subgroups for development of targeted interventions.
Keywords: major depressive disorder, mental health, sexual minority, substance abuse disorder
Introduction
Sexual minority (SM) refers to gay, lesbian, bisexual, and other diverse sexual identity populations that are not heterosexual. In psychiatric epidemiological research in the 2000s, several U.S. population-based surveys revealed pervasive mental health and substance abuse disparities for SM individuals relative to heterosexual individuals.1–5 Several theoretical frameworks have been used to explicate these trends. The minority stress model is most commonly cited, which describes mental health disparities that SM individuals face as the result of stressors such as discrimination, stigma, structural prejudices, and concealment of sexual orientation.6–8 If individuals are unable to develop coping mechanisms, such as learning resiliency skills, seeking out support networks in the community, and creating a positive view of their SM identity, their mental health can be affected negatively.7
In the 10 to 20 years since these early psychiatric epidemiological studies, there have been policy changes on a national level (i.e., antidiscrimination laws in health care and housing) and evolving social attitudes (i.e., greater acceptance of marriage equality).9,10 It is, thus, critical to obtain updated prevalence estimates of mental health and substance abuse disorders by sexual orientation drawn from more recent U.S. probability-based survey data that reflect the current social climate. Further, it is important to re-visit SM subgroup differences (e.g., lesbian/gay vs. bisexual) in mental health and substance abuse disorder prevalence and examine within-group disparities to inform targeted interventions. One recent study by Kerridge et al. evaluated data from the 2012 to 2013 National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) and determined that gay/lesbian and bisexual individuals had higher prevalence of major depressive disorder in the past 12 months, ranging from 13.9% to 17.2% in males and from 19.1% to 28.2% in females, compared with their heterosexual male (6.9%) and female (13%) counterparts. Gay/lesbian and bisexual individuals also had a higher prevalence of alcohol use disorder in the past 12 months, ranging from 26.6% to 31.4% in males and from 24.9% to 29.7% in females, compared with their heterosexual male (17.3%) and female (9.7%) counterparts. Similarly, the prevalence of drug use disorder in the past 12 months was high, ranging from 7.1% to 10.3% in males and from 7.9% to 11.3% in females, compared with their heterosexual male (4.8%) and female (2.7%) counterparts.11
In addition to elevated risks for mental health disorders in SM populations, it is well established that there are several sociodemographic and economic risk factors for mental health disorders in the general population, including sex, age, education, race, employment, overall wellbeing, and marital status.12,13 Examining these sociodemographic and economic risk factors in relation to sexual orientation differences in mental health disparities research is important from an intersectionality perspective.14 A person's mental health is influenced by multiple and sometimes intersecting identities, social positions, and processes. Using data from the 2015 National Survey on Drug Use and Health (NSDUH), focusing on major depressive episode (MDE) and alcohol and illicit drug abuse or dependence, this study aimed to assess the magnitude of these disparities for SM versus heterosexual adults and to evaluate differences in prevalence within SM subgroups.
Methods
Data source
The NSDUH is a nationally representative survey administered by the Substance Abuse and Mental Health Services Administration of the United States Department of Health and Human Services. The survey is open to the U.S. civilian noninstitutionalized population aged 12 years or older and uses stratified multistage area probability sampling. The NSDUH used audio computer-assisted self-interview software methods of interviewing. Interviewers set up the computerized survey for participants during in-person visits.
The weighted interview response rate in 2015 was 68.4% for adults.15 Additional methodological details have been published elsewhere.16 Using the provided analysis weight from the NSDUH, the weighted sample size for the lifetime MDE model was N = 42,545 and for the past 12-month MDE model it was N = 42,483. For alcohol and illicit drug abuse or dependence, it was N = 50,951. The study population only included adults who responded to the question about sexual orientation identity; those who selected “don't know” or “refused to answer” were excluded from the analysis due to small sample sizes when stratified by sex and type of response (total n = 597 [depression]; total n = 741 [alcohol and illicit drugs]). As this is a secondary data analysis, the study was exempt from institutional review board review; informed consent was not obtained by the authors of this study as the data were from a publicly available de-identified dataset.
Outcomes
Using data from the 2015 NSDUH, the four main outcomes of interest were: (1) lifetime MDE, (2) an MDE in the past 12 months, (3) any alcohol abuse or dependence in the past 12 months, and (4) any illicit drug abuse or dependence in the past 12 months. The illicit drugs that were queried were: marijuana, heroin, cocaine, methamphetamine, hallucinogens, inhalants, or prescription psychotherapeutic drugs that were misused, which included pain relievers, tranquilizers, and sedatives. Due to small weighted prevalence estimates of each of these drugs, as seen in Table 1, the abuse or dependence of these drugs was grouped into a single outcome variable.
Table 1.
Weighted Prevalence of Illicit Drug Abuse or Dependence in the Past 12 Months Stratified by Sexual Orientation and Sex (N = 2,271)
| Illicit drug abuse or dependence | Heterosexual, N (%) | Gay, lesbian, or bisexual, N (%) | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Marijuana | 432 (1.89) | 171 (0.66) | 46 (5.23) | 50 (3.57) |
| Heroin | 79 (0.34) | 25 (0.10) | 5 (0.63) | 9 (0.63) |
| Stimulants (including cocaine and methamphetamine) | 230 (1.00) | 110 (0.43) | 27 (3.11) | 27 (1.94) |
| Hallucinogens and inhalants | 27 (0.12) | 10 (0.04) | 9 (1.08) | 5 (0.33) |
| Prescription drugs (sedatives, tranquilizers, and pain relievers) | 256 (1.12) | 163 (0.63) | 23 (2.67) | 30 (2.12) |
Measures
All outcome measures were assessed based on the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV).17,18 Lifetime MDE is defined as experiencing at least five or more of nine symptoms almost every day in a 2-week period, with at least one of the symptoms being depressed mood or loss of interest or pleasure in daily activities. For past 12-month MDE, respondents have to report experiencing a period of depression that lasts for 2 weeks or longer as well as having some of the other symptoms during the past 12 months. For past 12-month alcohol or illicit drug dependence, three or more of six criteria (or seven criteria if a withdrawal criterion is included) have to be met. For past 12-month alcohol or illicit drug abuse, one or more of four criteria have to be met and the respondent must not have been dependent on alcohol or the illicit drug in the past year.17,18 The NSDUH asked about sexual orientation by using the following question, “Do you consider yourself to be…,” with response options of heterosexual, lesbian/gay, bisexual, don't know, or refused.
Statistical analyses
We calculated the crude weighted prevalence for each outcome by sexual orientation stratified by sex. Three logistic regression models were developed, one generating crude odds ratios for each of the outcomes, one for age-adjusted estimates, and the third adjusted for the following variables: sexual orientation identity (heterosexual, lesbian/gay, or bisexual), age category (18–25, 26–34, or 35 and older), sex (male/female), education (fifth grade or less grade completed, some middle or high school completed, high school diploma/General Education Development, some college credit no degree, associate's degree, or college degree or higher), race/ethnicity (non-Hispanic White, Black/African American, Native American/Alaskan Native/Hawaiian Native/Other Pacific Islander, Asian, more than one race, or Hispanic), and income (less than $20,000, $20,000–$49,999, $50,000–$74,999, or $75,000 or more). These variables were selected a priori based on the expertise of the research team and a review of existing research literature.
Mantel–Haenszel tests were performed to test for interaction (effect modification) between sexual orientation, the main explanatory variable of interest, and sex. Significant interactions between these variables warranted sex stratification in the logistic regression models. Logistic regression models were fit for all of the aforementioned sociodemographic and economic factors to estimate adjusted odds ratios. Due to complex sampling and study design, for all of these models the NSDUH sampling weight (ANALWT_C) was applied. Sample size varied slightly as the weighted total number for the lifetime MDE model was N = 42,545 and for the past 12-month MDE model it was N = 42,483. For the outcome variables on alcohol and illicit drug abuse or dependence, it was N = 50,951. To calculate age-adjusted prevalence rates, the prevalence estimates from this sample were standardized to the same age groups and sex-specific population data from the 2015 census. After applying these weights to each crude age- and sex-specific prevalence, the results were summed and age-adjusted sex-specific prevalence rates were calculated.
Results
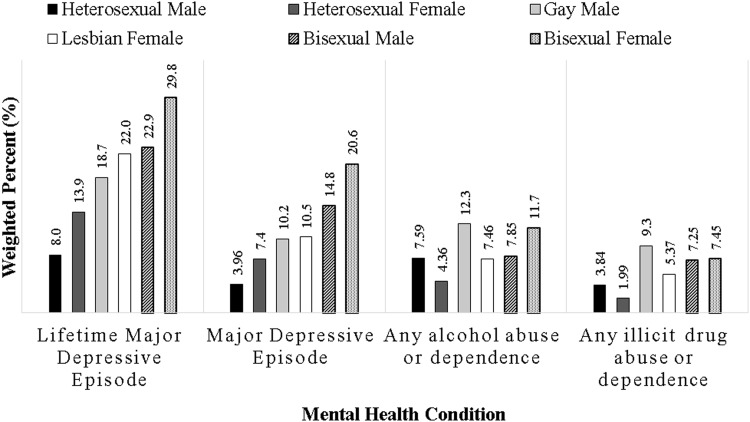
The results of the study are presented in Table 2 and Figure 1. The total number of participants varied for each model. Weighted estimates by sexual orientation and sex are shown in Table 2. Females had higher prevalence than males of MDE in the past 12 months or at least once in their lifetime. Bisexual males and females had the highest lifetime MDE prevalence at 30.8% and 35.8%, respectively; bisexual males and females also had the highest 12-month MDE prevalence at 22% and 24.4%, respectively. Although females had the highest absolute prevalence, gay males had 2.38 (95% confidence interval [95% CI] 1.70–3.33) times and bisexual males had 4.22 (95% CI 2.99–5.96) times higher odds of lifetime MDE compared with heterosexual males. Bisexual males had 5.82 (95% CI 3.87–8.74) times higher odds for MDE in the past 12 months compared with heterosexual males. When comparing the different logistic regression models for both depression outcomes, the effect sizes decreased slightly after adjusting for all sociodemographic and economic factors.
Table 2.
Weighted Prevalence of Lifetime (N = 42,545) and Past 12-Month Major Depressive Episode (N = 42,483) and Past 12-Month Alcohol and Illicit Drug Abuse or Dependence (N = 50,951) and Crude and Adjusted Odds Ratios Comparing Sexual Orientation Groups
| Heterosexual | Gay/Lesbian | Bisexual | ||||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| Total Na | 18,710 | 21,935 | 415 | 356 | 296 | 833 |
| Lifetime major depressive episode | ||||||
| Prevalenceb | 9.19% | 16.0% | 20.9% | 22.5% | 30.8% | 35.8% |
| Age-adjusted prevalence | 8.0% | 13.9% | 18.7% | 22.0% | 22.9% | 29.8% |
| Crude odds ratio (95% CI)c | 1.00 | 1.00 | 2.61* (1.87–3.64) | 1.53* (1.13–2.07) | 4.41* (3.16–6.14) | 2.93* (2.47–3.48) |
| Age-adjusted odds ratio (95% CI)d | 1.00 | 1.00 | 2.52* (1.80–3.53) | 1.49* (1.11–2.01) | 4.18* (3.00–5.82) | 2.72* (2.28–3.23) |
| Adjusted odds ratio (95% CI)e | 1.00 | 1.00 | 2.38* (1.70–3.33) | 1.43* (1.05–1.96) | 4.22* (2.99–5.96) | 2.74* (2.31–3.26) |
| Total Na | 18,691 | 21,897 | 415 | 355 | 296 | 829 |
| Major depressive episode (past 12 months) | ||||||
| Prevalenceb | 4.16% | 8.21% | 9.89% | 11.6% | 22.0% | 24.4% |
| Age-adjusted prevalence | 3.96% | 7.4% | 10.2% | 10.5% | 14.8% | 20.6% |
| Crude odds ratio (95% CI)c | 1.00 | 1.00 | 2.53* (1.63–3.92) | 1.47* (1.03–2.11) | 6.52* (4.42–9.60) | 3.61* (2.98–4.37) |
| Age-adjusted odds ratio (95% CI)d | 1.00 | 1.00 | 2.41* (1.56–3.76) | 1.40 (0.98–1.99) | 5.96* (4.02–8.82) | 3.10* (2.54–3.78) |
| Adjusted odds ratio (95% CI)e | 1.00 | 1.00 | 2.42* (1.56–3.75) | 1.33 (0.93–1.91) | 5.82* (3.87–8.74) | 2.97* (2.44–3.62) |
| Total Na | 22,941 | 25,744 | 507 | 417 | 363 | 979 |
| Any alcohol abuse or dependence (past 12 months) | ||||||
| Prevalenceb | 8.35% | 3.98% | 14.0% | 7.5% | 9.13% | 12.7% |
| Age-adjusted prevalence | 7.59% | 4.36% | 12.3% | 7.46% | 7.85% | 11.7% |
| Crude odds ratio (95% CI)c | 1.00 | 1.00 | 1.78* (1.23–2.60) | 1.96* (1.27–3.00) | 1.10 (0.68–1.78) | 3.49* (2.77–4.41) |
| Age-adjusted odds ratio (95% CI)d | 1.00 | 1.00 | 1.66* (1.13–2.44) | 1.67* (1.09–2.56) | 1.00 (0.61–1.62) | 2.25* (1.76–2.87) |
| Adjusted odds ratio (95% CI)e | 1.00 | 1.00 | 1.61* (1.09–2.38) | 1.66* (1.08–2.55) | 0.98 (0.60–1.59) | 2.33* (1.83–2.98) |
| Any illicit drug abuse or dependence (past 12 months) | ||||||
| Prevalenceb | 3.61% | 1.6% | 12.5% | 4.36% | 7.11% | 7.53% |
| Age-adjusted prevalence | 3.84% | 1.99% | 9.30% | 5.37% | 7.25% | 7.45% |
| Crude odds ratio (95% CI)c | 1.00 | 1.00 | 3.83* (2.51–5.83) | 2.80* (1.74–4.50) | 2.04* (1.25–3.32) | 5.00* (3.81–6.59) |
| Age-adjusted odds ratio (95% CI)d | 1.00 | 1.00 | 3.45* (2.22–5.38) | 2.30* (1.46–3.64) | 1.62 (1.00–2.64) | 2.88* (2.18–3.81) |
| Adjusted odds ratio (95% CI)e | 1.00 | 1.00 | 3.93* (2.48–6.23) | 2.12* (1.34–3.36) | 1.49 (0.91–2.44) | 2.61* (1.95–3.50) |
The total N is weighted.
Weighted prevalence.
Crude odds ratios included the NSDUH sampling weight (ANALWT_C).
Using logistic regression models, odds ratios were adjusted for sexual orientation identity and age category (18–25, 26–34, or 35 and older) and the NSDUH sampling weight (ANALWT_C) was applied. The weighted sample size for the lifetime major depressive episode model was N = 42,545 and for the past 12-month major depressive episode model it was N = 42,483. The sample size for the alcohol and illicit drug abuse or dependence model was N = 50,951.
Using logistic regression models, odds ratios were adjusted for sexual orientation identity, age category (18–25, 26–34, or 35 and older), education (fifth grade or less grade completed, some middle or high school completed, high school diploma/GED, some college credit no degree, associate's degree, or college degree or higher), race/ethnicity (non-Hispanic White, Black/African American, Native American/Alaskan Native/Hawaiian Native/Other Pacific Islander, Asian, more than one race, or Hispanic), and income (less than $20,000, $20,000–$49,999, $50,000–$74,999, or $75,000 or more). The NSDUH sampling weight (ANALWT_C) was applied.
Statistical significance at alpha 0.05 level.
CI, confidence interval; NSDUH, National Survey on Drug Use and Health.
FIG. 1.
Weighted age-adjusted prevalence of lifetime (N = 42,545) and past 12-month major depressive episode (N = 42,483) and past 12-month alcohol and illicit drug abuse or dependence (N = 50,951) by sexual orientation and sex.
The prevalence of alcohol and illicit drug abuse or dependence in the past 12 months was higher for males than for females across all sexual orientations except for those who identified as bisexual. Bisexual females reported higher prevalence of alcohol (12.7% vs. 9.13%) and illicit drug (7.53% vs. 7.11%) abuse or dependence than bisexual males. However, gay males had the highest prevalence of alcohol (14%) and illicit drug (12.5%) abuse or dependence compared with any other female or male SM group. Gay males had 3.93 (95% CI 2.48–6.23) times higher odds of any illicit drug abuse or dependence than heterosexual males. After adjusting for age, the effect sizes decreased for each outcome variable. However, the sexual orientation effect estimates did not decrease significantly when adjusting for the remaining sociodemographic and economic factors.
Discussion
In this U.S. nationally representative study, SM groups had stark disparities in MDE and alcohol and illicit drug abuse or dependence relative to heterosexual adults. SM females and males compared with heterosexual females and males, respectively, faced an increased burden of lifetime MDE and MDE in the past 12 months. The odds of each substance abuse or dependence outcome (any alcohol abuse or dependence and any illicit drug abuse or dependence) were statistically significantly higher for bisexual and lesbian females compared with heterosexual females, and for gay males compared with heterosexual males. However, although the substance abuse or dependence prevalence was higher for bisexual males than for heterosexual males, these differences did not reach statistical significance.
Our findings corroborate data from prior research when comparing differences by sex within SM groups.2,11,13 Bisexual females had the highest prevalence of both MDE outcomes and higher prevalence of alcohol and illicit drug abuse or dependence compared with bisexual males. However, gay males had the highest overall prevalence of alcohol and illicit drug abuse or dependence. Kerridge et al. found that the prevalence of major depressive disorder in the past 12 months for lesbian women was 19.1%11 and Cochran et al., in an evaluation of the MacArthur Foundation National Survey of Midlife Development, found that the 12-month prevalence of major depression for the combined category of lesbian and bisexual women reached the upper limit of our results, 33.5%.2 In the McCabe et al. study on the NESARC-II (2004–2005), the prevalence of past-year alcohol dependence was similar to our results at 16.8% (vs. 14%) for gay men.5 Unlike this study, McCabe et al. did not find that bisexual females reported higher prevalence of alcohol abuse or dependence compared with bisexual males, nor did they find that gay males had the highest prevalence of substance abuse or dependence.5
Although prior studies have illustrated that bisexual individuals tend to face a larger burden of depression and substance abuse or dependence disorders,11,13 our study found that gay males may equally be experiencing substance abuse and addictions. As one of the most marginalized SM subgroups, bisexual individuals (particularly females) often encounter unique stigma, discrimination, and isolation from the majority of both heterosexual and lesbian groups.11,19 This has been linked to higher prevalence of alcohol and illicit drug use. Based on the minority stress model, bisexual individuals without coping mechanisms to manage their increased societal stigma may self-medicate through use of alcohol and illicit substances.20,21 Future research is necessary to determine why these prevalence estimates, especially among gay males, appear to have risen over the past decade.
Limitations
Several limitations should be considered alongside the study findings. It is important to note that each study uses its own unique survey tools to measure MDE and substance abuse or dependence. The 2015 NSDUH used the diagnostic criteria of the DSM-IV created in 1994,17 which varies from the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria in 2013.22 We must caution about the generalizability of findings based on a combined abuse and dependence outcome variable. We also did not include those who did not know or refused to respond to the question about their sexual orientation due to small sample sizes. Further, adults aged 35 and older were combined in one subset, which may mask any differences in older populations. Finally, including prescription psychotherapeutic drugs alongside recreational drugs could prove problematic as patterns of prescribing and abuse of prescription drugs may vary compared with those for recreational drugs.
Conclusions
In general, our prevalence estimates align with past representative, population-based studies in the United States. Our study highlights differences both between and within SM groups. Most notably, bisexual adults faced an increased burden of MDE and alcohol and illicit drug abuse or dependence compared with other SM groups and their heterosexual counterparts. Sex differences cannot be ignored within each of the SM groups. Females (especially bisexual females) may be more likely to have lifetime MDE or an MDE in the past 12 months than males. The converse is true for alcohol and illicit drug abuse or dependence, as males tended to predominate in the burden of these mental health conditions. However, bisexual females experienced the greatest disparity compared with heterosexual females. Future research requires an in-depth look not only into SM subgroups but also into sex differences within SM subgroups.
Acknowledgments
This article was supported by a developmental grant awarded to principal investigator S.L.R. (CFAR-FCHC-15-1) by: (1) the Harvard University Center for AIDS Research (CFAR), a National Institutes of Health (NIH)-funded program (P30 AI060354), which is supported by the following NIH Co-Funding and Participating Institutes and Centers: National Institute of Allergy and Infectious Diseases, National Cancer Institute, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Heart, Lung, and Blood Institute, National Institute on Drug Abuse, National Institute of Mental Health, National Institute on Aging, Fogarty International Center, and the Office of AIDS Research; (2) the Harvard Global Health Institute. In addition, the authors thank Shanshan Liu and Charis Crofton at Boston Children's Hospital for lending their expertise in the calculations of weighted age-adjusted prevalence.
Disclaimer
This article uses publicly available data from the 2015 National Survey on Drug Use and Health conducted by the Substance Abuse and Mental Health Services Administration, an agency within the U.S. Department of Health and Human Services. The findings and conclusions in this article are those of the authors and do not necessarily represent any official position of the funders.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Cochran SD, Mays VM: Relation between psychiatric syndromes and behaviorally defined sexual orientation in a sample of the US population. Am J Epidemiol 2000;151:516–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cochran SD, Sullivan JG, Mays VM: Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol 2003;71:53–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gilman SE, Cochran SD, Mays VM, et al. : Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. Am J Public Health 2001;91:933–939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mays VM, Cochran SD: Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. Am J Public Health 2001;91:1869–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McCabe SE, Hughes TL, Bostwick WB, et al. : Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction 2009;104:1333–1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Meyer IH: Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull 2003;129:674–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cochran SD, Björkenstam C, Mays VM: Sexual orientation differences in functional limitations, disability, and mental health services use: Results from the 2013–2014 National Health Interview Survey. J Consult Clin Psychol 2017;85:1111–1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barnhill MM, Lee JGL, Rafferty AP: Health inequities among lesbian, gay, and bisexual adults in North Carolina, 2011–2014. Int J Environ Res Public Health 2017;14:E835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pew Research Center. A Survey of LGBT Americans: Attitudes, Experiences and Values in Changing Times. 2013. Available at www.pewsocialtrends.org/2013/06/13/a-survey-of-lgbt-americans Accessed February20, 2019
- 10. Barnes DM, Hatzenbuehler ML, Hamilton AD, Keyes KM: Sexual orientation disparities in mental health: The moderating role of educational attainment. Soc Psychiatry Psychiatr Epidemiol 2014;49:1447–1454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kerridge BT, Pickering RP, Saha TD, et al. : Prevalence, sociodemographic correlates and DSM-5 substance use disorders and other psychiatric disorders among sexual minorities in the United States. Drug Alcohol Depend 2017;170:82–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kessler RC, Berglund P, Demler O, et al. : The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003;289:3095–3105 [DOI] [PubMed] [Google Scholar]
- 13. Scott RL, Lasiuk G, Norris C: The relationship between sexual orientation and depression in a national population sample. J Clin Nurs 2016;25:3522–3532 [DOI] [PubMed] [Google Scholar]
- 14. Bauer GR: Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Soc Sci Med 2014;110:10–17 [DOI] [PubMed] [Google Scholar]
- 15. Center for Behavioral Health Statistics and Quality: 2015 National Survey on Drug Use and Health: Summary of the Effects of the 2015 NSDUH Questionnaire Redesign: Implications for Data Users. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2016 [PubMed] [Google Scholar]
- 16. Substance Abuse and Mental Health Services Administration. NSDUH 2015 Methodological Resource Book. 2015. Available at www.samhsa.gov/data/report/nsduh-2015-methodological-resource-book-mrb Accessed February20, 2018
- 17. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision. DSM-IV-TR ed. Washington, DC: American Psychiatric Association Publishing, 2000 [Google Scholar]
- 18. Center for Behavioral Health Statistics and Quality: 2015 National Survey on Drug Use and Health: Methodological Summary and Definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2016 [Google Scholar]
- 19. Koh AS, Ross LK: Mental health issues: A comparison of lesbian, bisexual and heterosexual women. J Homosex 2006;51:33–57 [DOI] [PubMed] [Google Scholar]
- 20. Hughes T: Alcohol-related problems among sexual minority women. Alcohol Treat Q 2011;29:403–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Johnson TP, Hughes TL, Cho YI, et al. : Hazardous drinking, depression, and anxiety among sexual-minority women: Self-medication or impaired functioning? J Stud Alcohol Drugs 2013;74:565–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed., Text Revision. DSM-V-TR ed. Washington, DC: American Psychiatric Association Publishing, 2013 [Google Scholar]