Abstract
Purpose: The purpose of this study was to examine how sexual orientation in adolescence and young adulthood was linked to diabetes risk.
Methods: Data were drawn from the 1994–2008 National Longitudinal Study of Adolescent to Adult Health. The baseline sample included 4330 girls and 3510 boys ages 12–18. Guided by the life course approach, we considered both the timing and continuity of sexual orientation—broadly defined by sexual identity, sexual attraction, sexual contact, and romantic/sexual relationships—by differentiating respondents into four categories: sexual minority in both adolescence and adulthood, sexual minority in adulthood only, sexual minority in adolescence only, and heterosexual in both adolescence and young adulthood. Diabetes was identified using A1c and glucose biomarkers and self-reports of diabetes diagnosis or medication use.
Results: Results from logistic regression models indicated that in comparison with their continuously heterosexual counterparts, respondents reporting sexual minority status in adulthood only or continuously in both adolescence and adulthood had higher diabetes risk in adulthood. However, respondents reporting sexual minority status in adolescence only were not different in diabetes risk in adulthood. The association between diabetes risk and continuous sexual minority status was stronger among women than among men.
Conclusions: Sexual minority health disparities emerge early in the life course during adolescence and young adulthood. These findings highlight the importance of designing and implementing policies and public programs to alleviate minority stress early in life to reduce health disparities.
Keywords: adolescence, diabetes, life course, sexual orientation, young adulthood
Introduction
Agrowing number of studies have suggested that sexual minority individuals experience major health disadvantages in comparison with their heterosexual counterparts.1−4 These studies usually focus on either sexual minority adults or children living with same-sex parents,5,6 with less attention given to the physical health of sexual minority adolescents. A life course perspective, which is increasingly used to guide health research, suggests that the transition from adolescence to young adulthood is a critical life period for sexual development and for the emergence of health disparities.7−10 However, studies exploring health issues of sexual minority individuals tend to treat sexual orientation as a static trait, failing to assess the dynamic experience of sexual orientation and how this process is linked to health outcomes.
We are particularly interested in diabetes (type 1 or 2) in relation to the complex and fluid experience of sexual orientation in adolescence and young adulthood because (1) diabetes is the fastest growing chronic condition in the United States, (2) diabetes is one of the most common diseases in adolescence and young adulthood, and (3) the development of diabetes is directly affected by social and behavioral factors.11 According to the U.S. Centers for Disease Control and Prevention, ∼208,000 American youth younger than age 20 had diabetes (type 1 or 2) in 2012, and this number will continue to grow in the coming decades.12 The consequences of diabetes have been clearly identified, including serious complications and premature mortality,11 and there are even more serious long-term complications associated with early onset of diabetes, relative to onset in older ages.13
Previous empirical evidence on sexual orientation differences in diabetes
A number of studies have found that sexual minority status is associated with a wide range of health outcomes.1−4 Only a few such studies, however, have examined diabetes as an outcome, and the findings are mixed—likely due to different ways of operationalizing sexual orientation and to different study samples.1,14−16 For example, a 24-year longitudinal study of American women ages 24–44 found that, compared with their heterosexual counterparts, women who identified as lesbian or bisexual had a 27% higher risk of developing type 2 diabetes and they developed diabetes at younger ages.17 An analysis of data from the Medical Expenditure Panel Survey (2003–2011) found that the odds of having diabetes for same-sex partnered women were almost three times those of different-sex partnered women.18
In contrast, analyses of data from the 2014 Behavioral Risk Factor Surveillance System (BRFSS) suggested that lesbian and bisexual women were not different from heterosexual women in terms of lifetime diabetes risk (although gay and bisexual men were more likely than heterosexual men to report a lifetime diabetes diagnosis),19 and analysis of pooled data from the 2014–2015 BRFSS found that bisexual women had lower odds of a diabetes diagnosis than heterosexual women.20 In addition, a study based on data from the 2001–2008 Massachusetts BRFSS found no evidence of differences in diabetes between LGB-identified and heterosexual-identified respondents.14 Several review articles have also suggested no evidence of sexual orientation differences in diabetes.21−23
Research on the link between sexual orientation and diabetes has focused primarily on adult samples; however, research on health risks among sexual minority youth suggests that differences in diabetes risk could emerge early in the life course. For example, a recent study using data from the Youth Risk Behavior Survey 2009–2015 found that LGB youth were more likely than heterosexual youth to be overweight or obese—a major risk factor for diabetes.24 Yet, to our knowledge, no studies have directly examined the link between sexual orientation and diabetes among adolescents transitioning to adulthood, which is the aim of the current study.
The minority stress perspective: predicting the links between sexual orientation and diabetes risk
A minority stress perspective provides a framework for understanding how sexual orientation disparities in health, including diabetes, emerge. Sexual minority individuals report more victimization, discrimination, and maltreatment than heterosexual individuals from childhood through adolescence.25−28 These experiences, recognized as major health risk factors,25−28 likely increase the risk of diabetes by directly causing the sympathetic nervous system to induce the release of stress hormones (e.g., catecholamines, cortisol), trigger physiological responses, inhibit insulin production, and metabolize glucose during the “fight-or-flight” process.29 Moreover, cumulative stressors may cause detrimental neurobiological changes and emotional and behavioral problems, such as experiencing depressive symptoms, overeating, smoking, drinking, and engaging in a sedentary lifestyle.30−32 These emotional and behavioral problems, in turn, can lead to elevated glucose levels.33 Consistent high blood glucose levels, along with inadequate levels of insulin or insulin resistance, increase the risk of diabetes.34 In this sense, long-term exposure to minority stress in adolescence and young adulthood may hinder the function of the metabolic system, resulting in potential risk of diabetes.
Moreover, the association between sexual minority status and diabetes risk may differ for men and women, given previous research on gendered responses to stress as well as the ways in which sex/gender and sexual orientation interact to shape health.35−38 For example, women are found to be more likely than men to respond to stress in emotion-focused and avoidant ways,37,39 which are associated with symptoms of depression and anxiety.39,40 Such internalizing symptoms may lead to overeating41 and elevated stress hormone release,42 both of which are associated with higher diabetes risk.33,43 Similarly, research has found that lesbian and bisexual women were at increased risk of overweight/obesity compared to heterosexual women, but gay men were at decreased risk of overweight/obesity compared to heterosexual men.44 Sexual minority women also experience higher rates of externalizing behaviors, such as smoking, relative to heterosexual women.45 In addition, research suggests that the mental health of young women is more negatively impacted by early experiences of same-sex sexuality than that of young men.9 Women's early same-sex experiences are more likely than those of men to occur within existing social relationships,46 and thus may be both more visible and more vulnerable to additional couple-level minority stressors.47 Taken together, these findings suggest that any association between sexual minority status and diabetes risk will be larger among women than among men.
The current study
We conceptualized sexual orientation as a dynamic, multidimensional experience occurring across the life course, and focused on this experience in adolescence (ages 12–18) and in young adulthood (ages 25–31). We analyzed data from four waves of the National Longitudinal Study of Adolescent to Adult Health (Add Health) to test the following hypotheses:
Hypothesis 1: Sexual minority status during adolescence and/or young adulthood will be associated with higher diabetes risk.
Hypothesis 2: The association between sexual minority status and diabetes risk will be larger among women than among men.
Methods
Data and sample
Add Health is the largest, most comprehensive national longitudinal survey of adolescents currently available in the United States. Add Health is a nationally representative sample of 20,745 students who were in 7th −12th grades in 1994/5 (Wave I), of whom 14,738 were followed up in Wave II (excluding Wave I seniors) in 1996. In 2001/2, 15,197 Wave I respondents (ages 18–26) were reinterviewed in Wave III. In 2007/8, 15,701 Wave I respondents (ages 24–32) were reinterviewed in Wave IV.
Because diabetes biomarkers assessing A1c and fasting glucose levels were not collected until Wave IV, our initial focal sample included Wave IV respondents. We further restricted the sample to 11,750 Wave IV respondents who had complete information on diabetes and sexual orientation. We then excluded respondents with missing values on other key covariates (n = 3204) and those with panel sample weights of zero (n = 706). Our final analytic sample included 7840 respondents, including 4330 women and 3510 men (ages 12–18 at Wave I and 25–31 at Wave IV).
Compared with those included in our final analytic sample, those excluded were not different on measures of diabetes; however, they were more likely to be male, older, non-White, to smoke daily and to drink frequently, and they were less likely to have parents with a college degree or to live in two biological parent families (results not shown but available on request). In this sense, the excluded cases were a more vulnerable and disadvantaged group, suggesting that our findings might be conservative estimates of any disadvantage. Moreover, in additional analyses that incorporated multiple imputation techniques to handle the missing data, and a Heckman correction to adjust for potential sample selection bias,48 we found substantively similar findings (not reported but available on request) as reported in this article. This study was approved by the Michigan State University Institutional Review Board.
Measures
Diabetes
We took advantage of the multiple questions asked about diabetes in Wave IV. Specifically, we identified respondents as having diabetes if he or she met any of the following conditions: (1) A1c ≥6.5%, (2) fasting glucose ≥126 mg/dL or nonfasting glucose ≥200 mg/dL; (3) self-report of diabetes diagnosis (types 1 and 2 not distinguished in the data); or (4) self-report of having taken diabetes medication. The cutoff points for A1c and glucose levels are consistent with the recommendations of the American Diabetes Association.34 Additional analysis using different cutoff points (e.g., A1c ≥5.7% for diagnosis of prediabetes34) led to similar results.
Sexual orientation
Following previous studies, we took advantage of the longitudinal data and multiple measures of sexual orientation included in Add Health, paying attention to the timing and continuity of sexual orientation across Waves I–IV.49 The surveys asked a series of questions about multiple dimensions of sexual orientation, including sexual identity, sexual attraction, sexual contact, and romantic/sexual relationships. Each dimension was assessed in both adolescence and young adulthood, with the exception of self-reported sexual identity, which was only measured in adulthood (Waves III and IV).
Sexual identity was measured with the following item: “Please choose the description that best fits how you think about yourself: 100% homosexual, mostly homosexual, bisexual, mostly heterosexual, and 100% heterosexual.” We classified respondents as heterosexual if they chose “100% heterosexual”; all others were classified as sexual minority. Sexual attraction was measured based on the question asking whether the respondent “had ever had a romantic attraction to a female/male.” Sexual contact was measured based on the question: “how many male/female partners have you ever had sex with?” Respondents were also asked to list each romantic and sexual relationship and the sex of each partner. We used this information along with respondent's self-reported sex to identify those respondents who reported any same-sex attraction, same-sex contact, or same-sex romantic/sexual relationship. Respondents were coded as sexual minority if they indicated any one of these four dimensions of same-sex sexuality.
We then categorized respondents' sexual minority status into four categories by life stage: (1) early sexual minority status continuing into adulthood (reported same-sex sexuality in both adolescence and adulthood; 319 [7.4%] women and 156 [4.5%] men), (2) late sexual minority status (reported same-sex sexuality in adulthood only; 439 [10.1%] women and 109 [3.1%] men), (3) early sexual minority status that did not continue into adulthood (reported same-sex sexuality in adolescence only; 337 [7.8%] women and 359 [10.2%] men), and (4) the reference category: heterosexual throughout adolescence and young adulthood (did not report same-sexuality in adolescence or adulthood; 3235 [74.7%] women and 2886 [82.2%] men).
The method of combining multiple dimensions of sexual orientation into one broad measure has been done in previous studies using Add Health data.9,50 There are several advantages to combining dimensions instead of analyzing each separately. For example, while sexual/romantic relationships and sexual contact are valid measures of sexual orientation in adulthood, previous research suggests that attraction might be more appropriate than relationships or contact for identifying sexual orientation in adolescence,51 as adolescents have less opportunity to engage in same-sex relationships or contact. Importantly, adolescents with same-sex attractions only (without same-sex contact or relationships) may experience minority stress, as stigmatized thoughts or identities do not need to be visible to cause stigma.52 Moreover, the sexual identity question was not asked until respondents were adults, in Waves III and IV. We used sexual orientation information across all possible waves and identified someone as reporting sexual minority status even if same-sex sexuality was reported inconsistently across waves. For example, if someone reported same-sex attraction at Wave I (during ages 12–18), we characterized this person as reporting sexual minority status in adolescence, even if she or he did not report same-sex attraction in future waves. Because we were interested in the cumulative impact of sexual minority status during the transition to adulthood, our measure of sexual minority status took advantage of all dimensions of sexual orientation that were available in adolescence and adulthood.
Covariates
We controlled for sociodemographic covariates at Wave I, including respondents' age (in years), sex (0 = male, 1 = female), race/ethnicity (non-Latinx White [reference], Black, Latinx, Asian or Pacific Islander, and other race), parents' highest level of education (ranging from 1 = less than high school to 5 = postgraduate degree), and family structure (including two biological parent family [reference], stepparent family, single parent family, guardian family, and missing reports). Instead of listwise deletion, we generated a missing flag for family structure due to a significant amount of missing values for this variable. We also controlled for the respondents' socioeconomic status at Wave IV, including personal income (ranging from 1 = $0−$2500 to 6 = $150,000 or more) and whether the respondent obtained a 4-year college degree by Wave IV (1 = yes, 0 = no).
In addition, we controlled for health behaviors that are available at Wave IV and that are associated with both sexual orientation30,31,53,54 and diabetes33,34,55,56: body mass index (BMI), whether respondent is a current daily smoker (1 = yes; 0 = no), frequency of drinking alcohol during the past 12 months (0 = none [reference]; 1 = 1 or 2 days; 2 = once a month or less; 3 = 2 or 3 days a month; 4 = once a week or more), and number of drugs used during the past 12 months. Number of drugs used was a sum of the following types of drugs used: any prescription drugs not prescribed for the respondent; steroids, anabolic steroids or “body building” drugs; marijuana; cocaine; crystal meth; and other types of illegal drugs, such as lysergic acid diethylamide (LSD), phencyclidine (PCP), ecstasy, heroin, or mushrooms. Finally, we controlled for depressive symptoms at Wave IV, which was a sum of 5 items of the Center for Epidemiologic Studies Depression (CES-D) scale (range 0–15; alpha = 0.79), including how often in the past week the respondent was bothered by things, could not shake off the blues, had trouble concentrating, felt depressed, and felt sad.
Statistical analysis
We estimated two binary logistic regression models to predict diabetes. The first model included the main effects of sexual orientation to test our first hypothesis, and the second model added an interaction term between sex and sexual orientation to test our second hypothesis. All covariates were included in both models. The complex sampling design of the data was handled using survey commands in STATA.57
Results
Table 1 shows the weighted descriptive statistics for all analytic variables by sexual orientation. As seen in Table 1, respondents categorized as sexual minority in either life stage (in adolescence only or adulthood only) or in both adolescence and adulthood had significantly (p < 0.05) higher proportions of having diabetes, lower proportions of 4-year college degree attainment, lower personal income, higher levels of depression, higher proportions of daily smoking, and more drug use, relative to heterosexual respondents.
Table 1.
Weighted Descriptive Statistics of Analytic Variables by Sexual Orientation (n = 7840)
| Variables | Heterosexual (n = 6121) | Sexual minority adolescence only (n = 696) | Sexual minority adulthood only (n = 548) | Sexual minority both stages (n = 475) |
|---|---|---|---|---|
| Had diabetes, W4 | 338a | 53 | 49 | 39 |
| 4.95% | 7.19%* | 7.68%* | 8.56%* | |
| Female, W1 | 3235 | 337 | 439 | 319 |
| 49.58% | 44.26%* | 72.2%* | 67.12%* | |
| Age, W1, mean (SD) | 14.36 (2.07) | 14.58* (2.12) | 14.34 (1.90) | 14.4 (2.19) |
| Race/ethnicity, W1 | ||||
| Non-Latino/a White (reference) | 3537 | 363 | 331 | 245 |
| 70.37% | 62.61%* | 74.02% | 69.49% | |
| Black | 1081 | 158 | 104 | 101 |
| 11.79% | 16.04%* | 11.32% | 12.73% | |
| Latino/a | 786 | 109 | 72 | 74 |
| 9.45% | 13.77%* | 9.75% | 9.00% | |
| Asian or Pacific Islander | 459 | 38 | 24 | 27 |
| 4.30% | 3.63%* | 2.63% | 2.99% | |
| Others | 207 | 19 | 11 | 26 |
| 3.10% | 2.91% | 0.88%* | 5.40%* | |
| Parents' education, W1 | ||||
| Less than high school (reference) | 606 | 91 | 59 | 61 |
| 9.31% | 16.67%* | 10.35% | 10.69% | |
| High school | 1889 | 234 | 194 | 146 |
| 32.76% | 34.05% | 35.10% | 32.35% | |
| Some college | 1220 | 120 | 117 | 91 |
| 20.97% | 16.82%* | 24.44% | 20.12% | |
| College degree | 1528 | 160 | 108 | 96 |
| 23.79% | 20.17% | 16.33%* | 20.28% | |
| Postgraduate degree | 878 | 91 | 70 | 81 |
| 13.18% | 12.28% | 13.78% | 16.56% | |
| Family structure, W1 | ||||
| Two biological parent family (reference) | 3336 | 337 | 267 | 214 |
| 57.14% | 50.58%* | 53.89%* | 48.58%* | |
| Stepparent family | 1510 | 189 | 153 | 138 |
| 22.26% | 23.19% | 24.84% | 26.32%* | |
| Single parent family | 28 | 5 | 0 | 3 |
| 0.40% | 1.40% | 0.00% | 0.76% | |
| Guardian family | 153 | 24 | 15 | 23 |
| 2.62% | 3.79% | 2.35% | 4.63% | |
| Missing | 1094 | 141 | 113 | 97 |
| 17.58% | 20.04% | 18.92% | 19.71% | |
| Personal income, W4, mean (SD) | 3.58 (1.65) | 3.44* (1.69) | 3.16* (1.39) | 3.34* (1.70) |
| Had 4-year college degree, W4 | 2382 | 192 | 173 | 138 |
| 36.76% | 24.6%* | 28.84%* | 29.38%* | |
| Body mass index, W4, mean (SD) | 28.20 (12.84) | 28.30 (8.62) | 28.70 (10.88) | 28.05 (12.06) |
| Current daily smoker, W4 | 1151 | 168 | 156 | 132 |
| 21.16% | 31.42%* | 32.53%* | 32.16%* | |
| Frequency of drinking, W4 | ||||
| None | 3104 | 406 | 250 | 208 |
| 46.27% | 52.55%* | 44.53% | 37.06%* | |
| 1 or 2 days a year | 1106 | 99 | 101 | 91 |
| 19.27% | 14.93%* | 20.07% | 20.27% | |
| Once a month or less | 723 | 62 | 63 | 58 |
| 12.96% | 9.38%* | 10.75% | 11.93% | |
| 2 or 3 days a month | 544 | 59 | 58 | 50 |
| 9.99% | 10.44% | 10.34% | 10.73% | |
| Once a week or more | 644 | 70 | 76 | 68 |
| 11.52% | 12.69% | 14.30% | 20.00%* | |
| No. of drugs used, W4, mean (SD) | 1.26 (2.02) | 1.44* (1.97) | 1.77* (2.05) | 2.08* (2.25) |
| Depressive symptoms, W4, mean (SD) | 2.34 (3.27) | 2.72* (3.38) | 3.35* (3.70) | 3.17* (3.62) |
Frequencies reported are unweighted.
p < 0.05, two-tailed t-tests comparing each sexual minority group with the heterosexual group.
Table 2 shows estimated odds ratios from logistic regression models predicting diabetes. Results from Model 1 of Table 2 indicate that compared with heterosexual respondents, those categorized as sexual minority in adulthood only (odds ratio [OR] = 1.578, p = 0.041) and, more strikingly, sexual minority in both adolescence and adulthood (OR = 1.714, p = 0.027) had significantly higher odds of having diabetes after controlling for all covariates. Respondents with sexual minority status in adolescence only did not have different odds of having diabetes (OR = 1.188, p = 0.336), relative to their heterosexual counterparts.
Table 2.
Estimated Odds Ratios from Logistic Regression Models Predicting Diabetes Risk (n = 7840)
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Main effects | Sex interaction | |||
| OR (SE) | p | OR (SE) | p | |
| Sexual orientation (reference: heterosexual) | ||||
| Sexual minority in adolescence only | 1.188 (0.303) | 0.336 | 1.399 (0.437) | 0.295 |
| Sexual minority in adulthood only | 1.578 (0.347)* | 0.041 | 1.737 (0.671) | 0.090 |
| Sexual minority in both stages | 1.714 (0.461)* | 0.027 | 0.984 (0.586) | 0.915 |
| Female | 0.863 (0.124) | 0.875 (0.140) | 0.488 | |
| Sexual orientation × female | ||||
| Sexual minority in adolescence only × female | 0.770 (0.351) | 0.985 | ||
| Sexual minority in adulthood only × female | 1.318 (0.313) | 0.298 | ||
| Sexual minority in both stages × female | 1.859 (0.523)* | 0.018 | ||
All models controlled for age, race/ethnicity, parents' education, and family structure at Wave I as well as personal income, college degree, body mass index, current daily smoker, drinking frequency, number of drugs used, and depressive symptoms at Wave IV.
p < 0.05.
OR, odds ratio; SE, standard error.
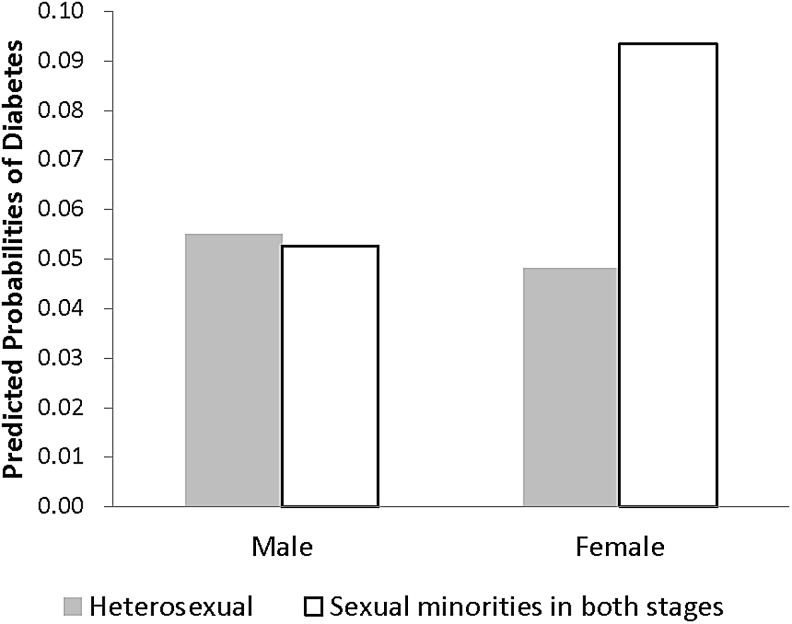
Results in Model 2 of Table 2 suggest that the difference in diabetes risk between respondents with sexual minority status in both adolescence and adulthood and heterosexual respondents varied by sex. Figure 1 shows the predicted probabilities of having diabetes for these two sexual orientation groups by sex based on results from Model 2 of Table 2. These results suggest that men with sexual minority status in both adolescence and adulthood were not significantly different from heterosexual men in terms of their odds of having diabetes (OR = 0.984, p = 0.915; calculated probabilities shown in Fig. 1); yet women with sexual minority status in both adolescence and adulthood had significantly higher odds of having diabetes than heterosexual women (OR = 0.984 × 1.859 = 1.829; calculated probabilities shown in Fig. 1). Additional analyses by sex (Supplementary Table S1) suggested that this effect for women was statistically significant (p = 0.010).
FIG. 1.
Predicted probabilities of diabetes by sexual orientation and sex. Predicted probabilities were calculated using estimates from Model 2 of Table 2.
Discussion
Consistent with our first hypothesis, we found that sexual minority status in adolescence and young adulthood was associated with diabetes risk in adulthood. Respondents who reported sexual minority status in both adolescence and adulthood had the highest risk of having diabetes. Because diabetes can be controlled, with the risk of complications reduced and the onset of disease delayed, identifying relevant risk factors is extremely important in designing effective prevention strategies and disease management programs. Consistent with the life course perspective on cumulative disadvantage, our findings suggest that long-term sexual minority status may comprise a major risk factor for developing diabetes, perhaps due to the stressors associated with a sexual minority status. These results are also consistent with previous studies suggesting that sexual minority individuals (often measured by sexual identity) have a higher risk of developing chronic diseases (e.g., cardiovascular diseases, cancer) than their heterosexual counterparts.18,23,58−61
Moreover, while our results suggest that sexual minority individuals who reported same-sex sexuality only in adulthood (and not in adolescence) had higher diabetes risk in adulthood than their heterosexual counterparts, sexual minority individuals who reported same-sex sexuality only in adolescence (and not in adulthood) did not. While sexual minority status in adolescence is associated with higher levels of emotional distress, substance use, and depression,62,63 it is unclear why sexual minority status in adolescence only was not associated with elevated diabetes risk. Future research should study which factors may protect/harm this specific group of sexual minority individuals.
Consistent with our second hypothesis, our results indicate that the association between sexual orientation (in particular, identifying as a sexual minority in both adolescence and young adulthood) and diabetes was stronger among women than among men. Women and men may experience different types of stressors64 and may respond differently to stressors,65,66 including those related to sexual minority status. Previous research suggests that disparities between sexual minority and heterosexual individuals are greater among women relative to men when examining health outcomes such as substance use, being overweight or obese, and depression.67−69 Some of these differences may be associated with the different contexts in which same-sex experiences occur during the life course stage, as sexual minority women are more likely than sexual minority men to experience early same-sex contact within romantic relationships.38,46 In our sample (results not shown but available on request), sexual minority women showed higher levels of depressive symptoms and BMI and were more likely to report being a daily smoker than sexual minority men, which may put sexual minority women at greater risk of developing diabetes. Indeed, our additional analysis (results not shown but available on request) suggested that including BMI and depression as additional covariates in our final model did reduce the size of the sex interaction effect, yet this estimated interaction effect remained significant, suggesting that BMI and depression may explain part of the sex difference in the association between sexual minority status and diabetes. Future studies should further examine additional possible mechanisms.
Limitations
The study had several limitations. First, it was limited by the relatively small number of sexual minority individuals in the sample, which limited our ability to fully analyze the separate dimensions of sexual orientation. Although we combined multiple dimensions of sexual orientation within different waves of the study for methodological and theoretical reasons, we acknowledge that this technique is not always optimal for studying sexual minority health. Second, the Add Health data are now somewhat dated, as Wave I was collected in 1994–1995 and Wave IV was collected in 2008. A variety of social and cultural changes have occurred within schools and larger society that likely shape risk factors associated with sexual minority status and diabetes. Add Health has currently begun a partial release of Wave V data (collected in 2016–2017) that will be valuable for future researchers to analyze and update trends. A third limitation is that we were unable to distinguish between type 1 and type 2 diabetes. However, given that 90–95% of adults with diabetes have type 2 diabetes, it is likely that most diabetes cases in our sample were type 2. Finally, future research should assess how and when sexual minority status “gets under the skin,”27 incorporating measures of minority stress and biological stress exposure and response.
Conclusions
This study is among the first to use a life course approach to examine sexual orientation during the transition to young adulthood in relation to diabetes risk. We found that individuals who reported sexual minority status in both adolescence and young adulthood and those who reported sexual minority status in adulthood only had higher diabetes risk than their heterosexual counterparts, even after controlling for sociodemographic covariates, health behaviors, and depressive symptoms. In addition, the association between diabetes risk and sexual minority status in adolescence and adulthood was stronger among women than among men.
These findings highlight the importance of designing and implementing policies and programs to alleviate minority stress in childhood and adolescence, especially for girls, to reduce health disparities experienced by sexual minority individuals. The results also highlight the importance of timing of intervention in reducing the risk of diabetes among sexual minority individuals and the complex nature of identifying vulnerable populations for intervention purposes. Our results suggest that interventions should be implemented early in the life course, with programs targeting youth with diverse sexual identities, given the fluid and dynamic nature of sexual orientation. All youth are harmed by sexuality-based discrimination and harassment, and it is challenging to identify all adolescents who are or will experience sexuality-based stigma and discrimination. Policies and programs should aim to reduce heteronormativity and sexuality-based discrimination across all social contexts and to create interventions that reduce the stress responses associated with stigmatized identities that put youth and young adults at risk of diabetes.
Supplementary Material
Acknowledgments
This research was supported by the National Institute on Aging K01 Award (K01AG043417) to Hui Liu. Everyone listed as an author contributed significantly to the work.
Disclaimer
The findings and conclusions in this article are those of the authors and do not represent the official position of the National Institute on Aging.
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Liu H, Reczek C, Brown D: Same-sex cohabitors and health: The role of race-ethnicity, gender, and socioeconomic status. J Health Soc Behav 2013;54:25–45 [DOI] [PubMed] [Google Scholar]
- 2. Strutz KL, Herring AH, Halpern CT: Health disparities among young adult sexual minorities in the U.S. Am J Prev Med 2015;48:76–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jackson CL, Agénor M, Johnson DA, et al. : Sexual orientation identity disparities in health behaviors, outcomes, and services use among men and women in the United States: A cross-sectional study. BMC Public Health 2016;16:807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Operario D, Gamarel KE, Grin BM, et al. : Sexual minority health disparities in adult men and women in the United States: National Health and Nutrition Examination Survey, 2001–2010. Am J Public Health 2015;105:e27−e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rosenfeld MJ: Nontraditional families and childhood progress through school. Demography 2010;47:755–775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stacey J, Biblarz TJ: (How) does the sexual orientation of parents matter? Am Sociol Rev 2001;66:159–183 [Google Scholar]
- 7. Johnson MK, Crosnoe R, Elder GH, Jr: Insights on adolescence from a life course perspective. J Res Adolesc 2011;21:273–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kann L, Olsen EO, McManus T, et al. : Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12—United States and selected sites, 2015. MMWR Surveill Summ 2016;65:1–202 [DOI] [PubMed] [Google Scholar]
- 9. Ueno K: Same-sex experience and mental health during the transition between adolescence and young adulthood. Sociol Q 2010;51:484–510 [DOI] [PubMed] [Google Scholar]
- 10. Martin KA: Puberty, Sexuality, and the Self: Boys and Girls at Adolescence. New York: Routledge, 1996 [Google Scholar]
- 11. National Diabetes Education Program. Overview of diabetes in children and adolescents. 2011. Available at http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.226.1551&rep=rep1&type=pdf Accessed April3, 2019
- 12. Centers for Disease Control and Prevention: National Diabetes Statistics Report, 2014: Estimates of Diabetes and Its Burden in the United States. Atlanta, GA: Department of Health and Human Services, 2014 [Google Scholar]
- 13. Hillier TA, Pedula KL: Complications in young adults with early-onset type 2 diabetes: Losing the relative protection of youth. Diabetes Care 2003;26:2999–3005 [DOI] [PubMed] [Google Scholar]
- 14. Conron KJ, Mimiaga MJ, Landers SJ: A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health 2010;100:1953–1960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dilley JA, Simmons KW, Boysun MJ, et al. : Demonstrating the importance and feasibility of including sexual orientation in public health surveys: Health disparities in the Pacific Northwest. Am J Public Health 2010;100:460–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hatzenbuehler ML, Phelan JC, Link BG: Stigma as a fundamental cause of population health inequalities. Am J Public Health 2013;103:813–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Corliss HL, VanKim NA, Jun HJ, et al. : Risk of Type 2 diabetes among lesbian, bisexual, and heterosexual women: Findings from the Nurses' Health Study II. Diabetes Care 2018;41:1448–1454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blosnich JR, Hanmer J, Yu L, et al. : Health care use, health behaviors, and medical conditions among individuals in same-sex and opposite-sex partnerships: A cross-sectional observational analysis of the Medical Expenditures Panel Survey (MEPS), 2003–2011. Med Care 2016;54:547–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Beach LB, Elasy TA, Gonzales G: Prevalence of self-reported diabetes by sexual orientation: Results from the 2014 Behavioral Risk Factor Surveillance System. LGBT Health 2018;5:121–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Newlin Lew K, Dorsen C, Melkus GD, Maclean M: Prevalence of obesity, prediabetes, and diabetes in sexual minority women of diverse races/ethnicities: Findings from the 2014–2015 BRFSS surveys. Diabetes Educ 2018;44:348–360 [DOI] [PubMed] [Google Scholar]
- 21. Eliason MJ: Chronic physical health problems in sexual minority women: Review of the literature. LGBT Health 2014;1:259–268 [DOI] [PubMed] [Google Scholar]
- 22. Meads C, Martin A, Grierson J, Varney J: Systematic review and meta-analysis of diabetes mellitus, cardiovascular and respiratory condition epidemiology in sexual minority women. BMJ Open 2018;8:e020776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Simoni JM, Smith L, Oost KM, et al. : Disparities in physical health conditions among lesbian and bisexual women: A systematic review of population-based studies. J Homosex 2017;64:32–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Beach LB, Turner B, Marro R, Phillips G: Diabetes risk behaviors are higher among sexual minority U.S. high school students. Diabetes 2018;67:Supplement 1:1650-P29875100 [Google Scholar]
- 25. Bontempo DE, D'Augelli AR: Effects of at-school victimization and sexual orientation on lesbian, gay, or bisexual youths' health risk behavior. J Adolesc Health 2002;30:364–374 [DOI] [PubMed] [Google Scholar]
- 26. Faulkner AH, Cranston K: Correlates of same-sex sexual behavior in a random sample of Massachusetts high school students. Am J Public Health 1998;88:262–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hatzenbuehler ML: How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull 2009;135:707–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Meyer IH: Minority stress and mental health in gay men. J Health Soc Behav 1995;36:38–56 [PubMed] [Google Scholar]
- 29. Taylor SE, Klein LC, Lewis BP, et al. : Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychol Rev 2000;107:411–429 [DOI] [PubMed] [Google Scholar]
- 30. Austin SB, Ziyadeh NJ, Corliss HL, et al. : Sexual orientation disparities in purging and binge eating from early to late adolescence. J Adolesc Health 2009;45:238–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Burgard SA, Cochran SD, Mays VM: Alcohol and tobacco use patterns among heterosexually and homosexually experienced California women. Drug Alcohol Depend 2005;77:61–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hatzenbuehler ML, Slopen N, McLaughlin KA: Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States. Health Psychol 2014;33:1185–1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hu FB, Manson JE, Stampfer MJ, et al. : Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001;345:790–797 [DOI] [PubMed] [Google Scholar]
- 34. American Diabetes Association: Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33:S62–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nolen-Hoeksema S: Gender differences in depression. Curr Dir Psychol Sci 2001;10:173–176 [Google Scholar]
- 36. Turner RJ, Avison WR: Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. J Health Soc Behav 2003;44:488–505 [PubMed] [Google Scholar]
- 37. Matud MP: Gender differences in stress and coping styles. Pers Individ Dif 2004;37:1401–1415 [Google Scholar]
- 38. Herdt GH, Boxer A: Children of Horizons: How Gay and Lesbian Teens Are Leading a New Way Out of the Closet. Boston, MA: Beacon Press, 1996 [Google Scholar]
- 39. Rosenfield S, Mouzon DM: Gender and mental health. In: Handbook of the Sociology of Mental Health, 2nd ed. Edited by Aneshensel CS, Phelan JC, Bierman A. New York: Springer, 2013, pp 277–296 [Google Scholar]
- 40. Wardle J, Steptoe A, Oliver G, Lipsey Z: Stress, dietary restraint and food intake. J Psychosom Res 2000;48:195–202 [DOI] [PubMed] [Google Scholar]
- 41. Puder JJ, Munsch S: Psychological correlates of childhood obesity. Int J Obes (London) 2010;34 Suppl 2:S37−S43. [DOI] [PubMed] [Google Scholar]
- 42. Chong LS, Thai M, Cullen KR, et al. : Cortisol awakening response, internalizing symptoms, and life satisfaction in emerging adults. Int J Mol Sci 2017;18: pii: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Knol MJ, Twisk JW, Beekman AT, et al. : Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia 2006;49:837–845 [DOI] [PubMed] [Google Scholar]
- 44. Semlyen J, Curtis TJ, Varney J: Sexual orientation identity in relation to unhealthy body mass index: Individual participant data meta-analysis of 93 429 individuals from 12 UK health surveys. J Public Health (Oxf) 2019. Feb 21. pii: . doi: 10.1093/pubmed/fdy224. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cochran SD, Bandiera FC, Mays VM: Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20–59 years: 2003–2010 National Health and Nutrition Examination Surveys. Am J Public Health 2013;103:1837–1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Savin-Williams RC, Diamond L: Sex. In: Handbook of Adolescent Psychology, 2nd ed. Edited by Lerner RM, Steinberg L. New York: Wiley, 2004, pp. 189–231 [Google Scholar]
- 47. Frost DM, LeBlanc AJ, de Vries B, et al. : Couple-level minority stress: An examination of same-sex couples' unique experiences. J Health Soc Behav 2017;58:455–472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Heckman JJ: Sample selection bias as a specification error. Econometrica 1979;47:153–161 [Google Scholar]
- 49. Wilkinson L, Pearson J: Same-sex sexuality and postsecondary outcomes: The role of high school locale. Soc Perspect 2015;58:380–401 [Google Scholar]
- 50. Pearson J, Wilkinson L: Same-sex sexuality and educational attainment: The pathway to college. J Homosex 2017;64:538–576 [DOI] [PubMed] [Google Scholar]
- 51. Savin-Williams RC: The New Gay Teenager. Cambridge, MA: Harvard University Press, 2005 [Google Scholar]
- 52. Goffman E: Stigma: Notes on the Management of Spoiled Identity. New York: Simon & Schuster, 1963 [Google Scholar]
- 53. Gruskin EP, Gordon N: Gay/lesbian sexual orientation increases risk for cigarette smoking and heavy drinking among members of a large Northern California health plan. BMC Public Health 2006;6:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Reczek C, Liu H, Spiker R: A population-based study of alcohol use in same-sex and different-sex unions. J Marriage Fam 2014;76:557–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ganz ML, Wintfeld N, Li Q, et al. : The association of body mass index with the risk of type 2 diabetes: A case–control study nested in an electronic health records system in the United States. Diabetol Metab Syndr 2014;6:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wray LA, Alwin DF, McCammon RJ, et al. : Social status, risky health behaviors, and diabetes in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci 2006;61:S290−S298. [DOI] [PubMed] [Google Scholar]
- 57. StataCorp: Stata Statistical Software: Release 13. College Station, TX: StataCorp LP, 2013 [Google Scholar]
- 58. Caceres BA, Brody AA, Halkitis PN, et al. : Cardiovascular disease risk in sexual minority women (18–59 years old): Findings from the National Health and Nutrition Examination Survey (2001–2012). Womens Health Issues 2018;28:333–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Caceres BA, Brody AA, Luscombe RE, et al. : A systematic review of cardiovascular disease in sexual minorities. Am J Public Health 2017;107:e13−e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bränström R, Hatzenbuehler ML, Pachankis JE: Sexual orientation disparities in physical health: Age and gender effects in a population-based study. Soc Psychiatry Psychiatr Epidemiol 2016;51:289–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Rosario M, Corliss HL, Everett BG, et al. : Sexual orientation disparities in cancer-related risk behaviors of tobacco, alcohol, sexual behaviors, and diet and physical activity: Pooled Youth Risk Behavior Surveys. Am J Public Health 2014;104:245–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Everett B: Sexual orientation identity change and depressive symptoms: A longitudinal analysis. J Health Soc Behav 2015;56:37–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Pearson J, Wilkinson L: Family relationships and adolescent well-being: Are families equally protective for same-sex attracted youth? J Youth Adolesc 2013;42:376–393 [DOI] [PubMed] [Google Scholar]
- 64. Meyer IH, Schwartz S, Frost DM: Social patterning of stress and coping: Does disadvantaged social status confer more stress and fewer coping resources? Soc Sci Med 2008;67:368–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Aneshensel CS, Rutter CM, Lachenbruch PA: Social structure, stress, and mental health: Competing conceptual and analytic models. Am Soc Rev 1991;56:166–178 [Google Scholar]
- 66. Rosenfield S, Lennon MC, White HR: The self and mental health: Self-salience and the emergence of internalizing and externalizing problems. J Health Soc Behav 2005;46:323–340 [DOI] [PubMed] [Google Scholar]
- 67. Coker TR, Austin SB, Schuster MA: The health and health care of lesbian, gay, and bisexual adolescents. Annu Rev Public Health 2010;31:457–477 [DOI] [PubMed] [Google Scholar]
- 68. Marshal MP, Dermody SS, Cheong J, et al. : Trajectories of depressive symptoms and suicidality among heterosexual and sexual minority youth. J Youth Adolesc 2013;42:1243–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Institute of Medicine (US) Committee on Lesbian, Gay Bisexual, and Transgender Health Issues and Research Gaps and Opportunities: The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: National Academies Press; (US), 2011 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.