Abstract
Purpose of Review
Comorbidity of posttraumatic stress disorder (PTSD) and insomnia, nightmares, and obstructive sleep apnea (OSA) is high. We review recent research on psychotherapeutic and pharmacological interventions for sleep disorders in PTSD.
Recent Findings
PTSD treatments decrease PTSD severity and nightmare frequency, but do not resolve OSA or insomnia. Research on whether insomnia hinders PTSD treatment shows mixed results; untreated OSA does interfere with PTSD treatment. Cognitive behavioral therapy for insomnia is the recommended treatment for insomnia; however, optimal ordering with PTSD treatment is unclear. PTSD treatment may be most useful for PTSD-related nightmares. CPAP therapy is recommended for OSA but adherence can be low.
Summary
Targeted treatment of sleep disorders in the context of PTSD offers a unique and underutilized opportunity to advance clinical care and research. Research is needed to create screening protocols, determine optimal order of treatment, and elucidate mechanisms between sleep and PTSD treatments.
Keywords: PTSD, Sleep disorders, Insomnia, Obstructive sleep apnea, Treatment
Introduction
Comorbidity of posttraumatic stress disorder (PTSD) and sleep disorders is staggeringly high, with 70–91% of individuals with PTSD reporting sleep disturbances [1–3]. The most common sleep disturbances include insomnia [1, 4], obstructive sleep apnea (OSA) [5, 6••], and nightmares [4], with prevalence rates in PTSD that are considerably higher than in unaffected individuals. Furthermore, sleep disorders, even when controlling for PTSD symptoms, contribute to major depression, substance abuse, impaired daytime functioning [7], negative long-term health consequences [8], and suicide risk [7]. Treatments for sleep disorders, in the context of co-occurring PTSD, offer opportunity to advance client-centered clinical care and research.
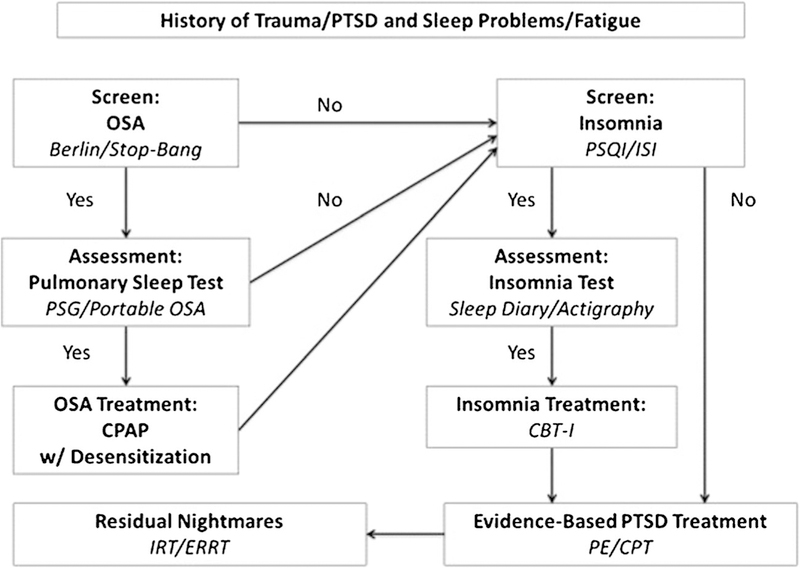
We review recent research on pharmacological and psychotherapeutic interventions for the most common sleep disturbances in PTSD: insomnia, nightmares, and OSA. First, we review sleep disorder prevalence and assessment in patients with PTSD and the relationships between sleep disorders and PTSD severity. Second, we review sleep disorder treatments in patients with PTSD. Finally, we make suggestions for screening (see Fig. 1) and research to advance sleep treatments with co-occurring PTSD.
Fig. 1.
Flow chart for assessment and treatment of sleep disorders in PTSD
Prevalence of Sleep Disorder with PTSD
Prevalence of Insomnia in PTSD
“Difficulty sleeping” was reported by up to 90% of individuals with PTSD [9] whereas application of DSM-5 criteria for insomnia suggest a range of 35–61% [1–3, 5]. Interestingly, civilian and military samples with PTSD showed similar rates of insomnia [1, 2]. However, the rates of insomnia depend on a range of factors that include definition of insomnia (“trouble sleeping,” DSM-5 criteria), sample characteristics (treatment seeking, community), trauma type (sexual assault, combat, natural disaster), objective/ subjective measurement (self-report questionnaire, actigraphy), instrument (sleep items from PCL, validated sleep questionnaire), time from incident trauma (childhood, adult), co-occurring disorders (depression/OSA/TBI), and age [1, 2, 4, 5, 9–14].
Prevalence of Nightmares in PTSD
Recurrent nightmares are one of two sleep items in the PTSD diagnosis and are highly prevalent in PTSD. Prevalence estimates range from 50 to 96% [4, 15]. Nightmare frequency was estimated at more than five per week in a sample of sexual assault survivors with PTSD [5], while increased combat exposure in Vietnam veterans was related to increased nightmare frequency [4]. Rates of nightmares seems to depend upon criteria, assessment, and methodology [16]. In a retrospective review of 500 active military personnel, Creamer et al. [17•] found 31.2% had nightmares weekly, but only 3.9% reported nightmares as a reason for seeking treatment.
Prevalence of OSA in PTSD
Sleep-disordered breathing (SDB) is a spectrum [18] ranging from mild upper airway resistance (e.g., snoring) to severe OSA. OSA is defined by repeated episodes of apneas (pauses in breathing) and hypopneas (shallow breathing) with decreases in blood oxygenation during sleep. The apnea–hypopnea index (AHI) per hour is the most commonly used metric of OSA severity. Research suggests that individuals with PTSD have higher rates of OSA than the general population; estimates range from 13.5 to 83% [19, 20]. However, not all studies found a higher prevalence of OSA in PTSD [21]. Rates of OSA seem to depend on objective/subjective measurement, diagnostic criteria (SDB, OSA), AHI thresholds, sample characteristics (military, civilian), age, body mass index (BMI), and sex (see Gupta et al. [22•] and Zhang et al. for reviews [23••]). In a meta-analysis on CPAP [23••], pooled variance % of OSA was reported in 10 studies on individuals with PTSD (mean age 42.4 years). OSA prevalence was 75.7% when using criteria of AHI > 5 and 43.6% when using AHI > 10; rates are significantly higher in individuals with PTSD than without. Of note, a majority of their studies (N = 9) used veteran samples, limiting generalizability to civilian samples. Their analyses showed no difference in rates of OSA by U.S. compared to non-U.S. or mixed samples (60.4 vs. 42.4%). They did, however, find differences based on veterans and non-veterans (62.5 vs. 7.0%), but the civilian numbers may be skewed. While the pooled variance is similar to findings in studies not included in the review, increasing confidence in the findings [24], Zhang et al. noted that they could not control for psychotropic medications that may affect OSA prevalence (e.g., benzodiazepines, opioids). Gupta et al. noted that no conclusion could be drawn about the role of medications on OSA prevalence due to the wide range of medications and quality of the studies but suggests that medications that lead to weight gain (e.g., antipsychotics) or affecting upper airway and breathing (e.g., benzodiazepines) may be risk factors for OSA.
There is increasing evidence that the classic predictors of OSA, such as BMI and age, may not apply to younger veterans with PTSD. Two recent studies found 67.3–69.2% were at high risk of OSA in younger veterans (mean age = 33.40–35.1 years) with lower BMI (BMI = 19.08–28.9) [6, 25]. Similarly, in a recent PSG study comparing Iranian veterans with and without PTSD, AHI was higher and BMI lower in the PTSD group compared to the non-PTSD group, and that AHI was unrelated to BMI [26•].
Relationship Between Sleep Disorders and PTSD
Relationship Between Insomnia and PTSD
Although sleep disturbances are symptoms of PTSD, insomnia may be best considered a co-occurring and independent disorder [27•, 28]. For instance, insomnia may precede the trauma and predict the development of PTSD [29–33]. This is especially true in military populations where short sleep duration and irregular sleep patterns are common [9, 34]. Second, when insomnia initially occurs as a symptom of PTSD, it can become an independent disorder when the behavioral and cognitive responses to acute insomnia lead to perpetuating factors (e.g., napping, sleeping pills) and conditioned arousal [35]. Additionally, nightmares and hyperarousal symptoms may lead to the pairing of the bed with wakefulness (i.e., conditioned arousal). Thus, perpetuating factors and conditioned arousal are often responsible for the maintenance of insomnia even in the absence of PTSD [36]. This suggests that insomnia may need to be assessed and treated separately from, or in conjunction with, PTSD.
Relationship Between Nightmares and PTSD
Nightmares in PTSD are associated with increased anxiety, depression, and suicide [37, 38]. Similar to both insomnia and OSA, the temporal relationship between nightmares and PTSD is unknown; however, there is evidence that nightmares may precede PTSD [4, 39, 40]. Nightmares may also influence insomnia through conditioned arousal (e.g., chronic nightmares pair the bed with arousal) and OSA (e.g., nighttime fragmentation leading to increased AHI).
Relationship Between PTSD and OSA
Both PTSD and OSA are associated with common medical comorbidities including heart attacks, hypertension, stroke [41–43], pain [43], and diabetes [41, 43]. However, there is a dearth of research examining both OSA and PTSD together on health outcomes. In a study of 187 sexual assault victims with PTSD, patients with both PTSD and SDB had worse physical functioning, bodily pain, less energy, and worse social/emotional/mental health functioning than patients with PTSD alone [5]. One study found that while PTSD was not associated with a higher prevalence of OSA, AHI predicted PTSD severity [21].
While no definitive conclusions can be drawn about the temporal relationship between OSA and PTSD, there may be a bidirectional relationship through which PTSD/chronic arousal affects OSA onset and severity, and a pathway through which OSA negatively affects PTSD and chronic arousal [44]. Jaoude et al. [45••] suggests several possible shared pathways between OSA and PTSD including HPA axis dysfunction [46, 47] and reduced fear extinction [48]. Additionally, there is evidence that SDB or nighttime fragmentation, when paired with trauma, may decrease processing, resiliency, and coping capacity and lead to higher likelihood of stress symptoms [25, 49].
Relationships among PTSD, OSA, and Insomnia
Despite high co-occurrence among PTSD, OSA, and insomnia [14, 26•, 50, 51], clear diagnosis of each disorder is often underreported due to symptom overlap [45••] and absence of differential diagnostic criteria [52•]. One study compared PSG patterns of OSA in veterans and found that those with PTSD were more likely to also have insomnia compared to those without PTSD [26]. Further, recent studies suggest that having PTSD, OSA, and insomnia all together shows a more severe clinical profile than PTSD/OSA or PTSD/insomnia combinations. A nationally representative sample found individuals with OSA and insomnia had worse hypertension and cerebrovascular disease than those with OSA alone [53]. In a sample with PTSD, it was found that veterans with PTSD, insomnia, and OSA had worse quality of life, sleep, and depression than veterans with just PTSD/OSA [54•].
Assessment of Sleep Disorders
Due to the high overlap of symptoms between sleep disorders and PTSD, accurate assessment of sleep disturbance is necessary prior to treatment.
Assessment of Insomnia
One option is to extract existing sleep items from measures of PTSD, such as the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) interview [55] or PTSD Checklist for DSM-5 (PCL-5) self-report questionnaire [56]. While this approach may reduce patient burden, it provides only very basic information about sleep and is inadequate for research or treatment planning. Several validated subjective measures are available to assess the severity, duration, and nature of disruptions to sleep more thoroughly. The Pittsburgh Sleep Quality Index (PSQI) [57] is an 18-item self-report questionnaire which measures global sleep quality over the past month. The Insomnia Severity Index (ISI) [58] is a seven-item measure, evaluating perceived severity of sleep difficulties with sleep satisfaction, daily functioning, and impairment. Prospective sleep diaries allow for measurement of an individual’s sleep over several days, including bed times, wake times, sleep latency, wake after sleep onset, total sleep time, and sleep efficiency.
Validated actigraphy offer a convenient option for objective, prospective measurement of sleep. Actigraphy involves wearing an activity monitor, typically similar to a wristwatch, that generates estimates of sleep and wake based on movement. Though collecting several days of sleep data is always ideal, it is particularly important in the case of PTSD, as sleep has been shown to be more variable than in primary insomnia patients without PTSD [59]. Note that actigraphy is not considered a valid methodology for the measurement of sleep stages or arousals from sleep. In contrast to medical-grade actigraphs, consumer-grade activity watches have not been validated in individuals with PTSD and cannot be recommended. Furthermore, proprietary and changing algorithms in many popular, non-clinical devices create difficulties conducting research or measuring clinical change.
Assessment of Nightmares
Similar to insomnia, researchers often extract the nightmare item from the CAPS-5 interview or PCL-5. Less utilized is the Disturbing Dream and Nightmare Severity Index, which assesses the frequency, intensity, and severity of nightmares [60]. Often sleep diaries include the number of nightmares and distress from night-mares. This is important to track in PTSD as there have been significant associations between number of daily stressors and sleep latency, number of nightmares, and distress from night-mares [61].
Assessment of OSA
Common screening measures such as the STOP-BANG [62] and Berlin [63] have not been validated against polysomnography (PSG) in PTSD populations. PSG is the gold standard method for the evaluation of sleep apnea and sleep architecture (e.g., stages of sleep, sleep spindles). PSG has traditionally been conducted in the hospital setting, but this might not be advantageous when assessing patients with PTSD where environmental factors may alter symptom severity [64]. Ambulatory PSG may offer a better option for those with PTSD to reflect their sleep in their home environment. There is increasing use of validated portable devices for the detection of sleep apnea that are increasingly affordable and easy to use. While these devices cannot report stages of sleep or sleep architecture, they accurately track apneas/ hypopneas. Jaoude [45••] suggests that overestimation of AHI may be encountered when interpreting PSG in patients with PTSD due to PTSD specific arousals and awakenings.
Pharmacological Treatments of Sleep Disorders
Selective serotonin reuptake inhibitors (SSRI) and serotonin– norepinephrine reuptake inhibitors (SNRIs) are recommended as first-line treatments for PTSD [65]. However, the effects of SSRI/SNRI on sleep are typically modest or even adverse. Accordingly, adjunctive medication is commonly indicated for the treatment of insomnia.
GABA Receptor Agonists
Benzodiazepines are commonly used, but controversial in the treatment of insomnia. A recent meta-analysis revealed that short-acting benzodiazepines have modest, beneficial effects on sleep in PTSD; their use is not recommended due to the emergence of tolerance, and their association with depression, aggression, and worse psychotherapy outcomes [66••]. In a review of benzodiazepines and OSA, results suggest that benzodiazepine use was associated with reduced upper airway muscle tone, decreased ventilatory response to hypoxia, increased AHI and oxygen desaturations, and prolonged apneas [67]. It is suggested that benzodiazepines should be avoided in patients with OSA [68].
The non-benzodiazepine hypnotics carry fewer risks, but need further evaluation with PTSD patients. In a meta-analysis in non-PTSD samples, non-benzodiazepine hypnotics were found to have only slight improvements in sleep over placebo [69]. In 24 subjects with PTSD, eszopiclone was shown to have greater beneficial effects than placebo on sleep quality, duration and latency, while reducing waking and improving daytime function [70]. In a meta-analysis, non-benzodiazepine hypnotics in patients with OSA were shown to improve objective sleep quality without worsening AHI [71]; however, this has not been examined in a PTSD sample.
Trazodone and Nefazodone
Two 5HT2A antagonists, nefazodone and trazodone, cause sedation and promote sleep. In small unblinded studies, trazodone has been shown to promote sleep and reduce nightmares in PTSD and depressed patients [72, 73]. Trazodone may be particularly helpful for patients with alcohol use disorders [74] and OSA [75], where GABA receptor agonists are contraindicated. However, the use of trazodone is limited by common side effects including cognitive and motor impairment [76], and tolerance [73].
Antipsychotics Drugs
Many atypical antipsychotic drugs are sedating and show evidence of efficacy in PTSD related insomnia and nightmares. In a placebo-controlled trial, adjunctive olanzapine was reported to have beneficial effects on sleep over 12 weeks in subjects who had failed to respond fully to SSRI [77]. Similar effects were shown for risperidone. In a large, 24-week study of 267 veterans, risperidone significantly improved scores on the PSQI and reduced nightmares [78]. In a 12-week, placebo-controlled study of quetiapine monotherapy, there were only modest and transient effects on insomnia, even as there was an overall improvement in PTSD symptoms [79•]. Antipsychotic drugs are commonly associated with high rates of adverse events [80]. Antipsychotic are associated with weight gain that may also increase risk of OSA [22•]. Therefore, patient selection may be especially important with antipsychotics to identify those with favorable clinical profiles.
Adrenergic Drugs
Prazosin is an alpha1 receptor antagonist and is the best-supported drug treatment for insomnia in PTSD. Including case series, more than 10 trials have reported favorable effects of prazosin in PTSD on sleep, improving insomnia, and reducing nightmares across a range of civilian, military, and veteran groups [81, 82•]. In a meta-analysis of six randomized trials encompassing 240 subjects, prazosin had significant effects on promoting sleep quality and reducing nightmares [83••]. However, a recent multi-center study of prazosin in veterans found no effects on sleep or any other PTSD symptom cluster [84•]. This large, well-powered study found relatively strong placebo effects that could have limited the ability to detect prazosin effects. Moreover, as prazosin was already commonly used in veterans with PTSD during the study, treatment-naïve patients may have been difficult to recruit, perhaps leading to selection bias. However, the work indicates that additional studies are needed to identify the circumstances and patients under which prazosin treatment should be selected.
For OSA, there are currently no studies examining the effects of prazosin for decreasing AHI. However, it is possible that prazosin, as a REM suppressor, may decrease nighttime arousals, and thus AHI [85].
Others
Diphenhydramine, gabapentin, hydroxyzine, and tiagabine are commonly used in the general insomnia population but are not well supported by evidence [86]. For example, the only study examining hydroxyzine in a PTSD sample found that hydroxyzine decreased nightmares and improved sleep better than placebo, and prazosin outperformed both [87]. These agents have not yet been systematically evaluated in PTSD. Melatonin agonists (e.g., ramelteon), orexin antagonists (e.g., suvorexant), and low-dose doxepin are approved treatments for insomnia in the general population but have not yet been systematically evaluated in PTSD.
Non-Pharmacological Treatment of Sleep Disorders
Effect of PTSD Treatment on Sleep Disorders
While insomnia tends to improve over the course of PTSD treatment, it often remains disturbed post-treatment. For example, two studies comparing prolonged exposure therapy (PE) and cognitive processing therapy (CPT) [88, 89] and one study examining cognitive-behavioral therapy (CBT) for PTSD [90] found that while sleep improved over the course of treatment, sleep disturbance remained above the clinical cut-off. Further, some of the sleep improvements deteriorated by the 6-month post-treatment assessment [90]. More recently, in a study of active-duty military personnel randomized to group CPT or group present-centered therapy (PCT) [91••], sleep disturbance was the most frequently reported symptom of PTSD both before and after treatment. Of 108 participants, 92% reported sleep disturbance pre-treatment and 74–80% (CPT and PCT, respectively) reported sleep disturbances post-treatment. Among participants who no longer met criteria for PTSD post-treatment, 57% still reported sleep disturbances.
Nightmares were more responsive to PTSD treatment than insomnia. In one study, 69% reported nightmares pre-treatment and 49–55% at follow-up. However, among participants who no longer met criteria for PTSD, only 13% continued to report nightmares. This is consistent with previous findings showing nightmares decreasing following PTSD treatment [92, 93•]. Finally, a study of PE compared to client-centered treatment found that both insomnia and night-mares decreased, but that while only 20% of participants endorsed nightmares, 55.1% still reported residual insomnia following treatment [94••].
Studies examining whether baseline insomnia affected change in PTSD symptoms over the course of psychotherapy have shown mixed results. Individuals with residual sleep problems following PE were predictive of smaller treatment gains [95•]. In a study of 246 patients who received CT-PTSD, poorer self-reported sleep together with greater depression symptoms were associated with worse PTSD treatment out-comes [96••]. Finally, a study of CBT for PTSD found that individuals with residual sleep difficulties following treatment experienced worse residual PTSD [90]. Beyond PTSD symptoms, one study examining PE to client-centered therapy found that baseline insomnia and nightmares predicted worse quality of life up to 6 months following treatment [94••]. On the other hand, initial sleep duration was not associated with treatment outcomes in a sample of 121 individuals who received CT-PTSD, supportive therapy, or were waitlisted [97••]. Similarly, one study (N = 21) found that while higher PSQI scores were related to higher baseline PCL scores, PSQI scores were not associated with reduced effectiveness of PE treatment or slope of PTSD symptom changes [98••].
Studies that examined whether baseline OSA affected change in PTSD symptoms over the course of psychotherapy were more consistent. A retrospective study of Veterans who had completed CPT at a VA found that those with OSA (n = 69) showed less symptom improvement than those without OSA (n = 276) [99••]. However, those with OSA who were being treated with CPAP showed more improvement than those who were not engaging in OSA treatment. Reist et al. [100••] found similar finding in a smaller sample (N = 18) undergoing PE, where PCL scores reduced by 28.25 points in those without SDB and only 7.17 points in the SDB group. Reist et al. suggest that OSA and insomnia may have differential impacts on PTSD treatment effectiveness and should both be assessed for treatment planning.
Treatment of Insomnia in PTSD
Non-pharmacological treatments may be more effective to treat insomnia in individuals with PTSD than pharmacological treatments. Cognitive-behavioral therapy for insomnia (CBT-I) is considered to be the front-line treatment for insomnia by the American College of Physicians [101] and shows promise in PTSD patients. CBT-I is a protocol typically involving (1) sleep restriction, or limiting patients’ time in bed to more closely correspond to total sleep time; (2) stimulus control, or instructing patients to use bed for sleep only in order to strengthen the association between bed and sleep; (3) sleep hygiene, or providing additional suggestions for behavioral modifications to improve sleep; and (4) modification of dysfunctional thoughts about sleep. CBT-I can be delivered individually or in group format over 4 to 8 weeks [102].
Efficacy of CBT-I has been established in patients with primary insomnia [103] and has been shown to outperform sleep medication in studies conducted in primary insomnia patients [104, 105]. Several studies have also shown that CBT-I improves insomnia symptoms in PTSD patients; recent meta-analyses show large effect sizes for CBT-I in reducing insomnia symptoms in PTSD [106••] and medium effect sizes for reducing PTSD symptoms [107••]. For example, in an RCT involving mostly civilian PTSD patients, eight-session individual CBT-I improved subjective insomnia and increased objective total sleep time in comparison to waitlist control [108]. However, both groups showed decreases in PTSD, limiting the conclusions on the effects of CBT-I on PTSD symptoms. Other studies support the use of CBT-I in veterans with PTSD as a part of routine clinical care [61]. Taken together, these studies support the use of CBT-I in patients with PTSD.
Several studies in veterans with PTSD used CBT-I and Imagery Rehearsal Therapy (IRT, described below) together, which improved insomnia and PTSD symptoms as compared to treatment as usual [109]. An RCT conducted in veterans with PTSD used combined CBT-I and IRT and showed improvements in insomnia, PTSD, and depressive symptoms compared to the waitlist [110]. It is unclear if combined treatment is more effective than either treatment alone.
As supplemental treatments to trauma-focused or pharmacotherapy interventions, several other behavioral interventions for insomnia have been studied in PTSD, including physical exercise [111], mind–body bridging [112], acupuncture [113], and hypnotherapy [114•, 115], with improvements across a variety of insomnia measures. Additionally, due to the overlap of insomnia and OSA, there is some suggestion that treating both together can improve insomnia symptoms better than either insomnia or OSA treatment alone [67]. The research on these interventions is preliminary and improvements are modest. If supported by larger and more rigorous trials, these interventions have the potential to provide additional options for treating insomnia in PTSD.
Taken together, research suggests CBT-I is the best-supported intervention for treating insomnia in PTSD patients.
Treatment of Nightmares in PTSD
Several non-pharmacological interventions show promise for treating nightmares related to PTSD. Imagery rehearsal therapy (IRT) has been the most researched. IRT involves (1) psychoeducation about sleep and nightmares; (2) relaxation training, (3) rescripting selected nightmares, i.e., writing out the nightmare and changing the storyline, ending or any part of the dream to be more positive; and (4) rehearsing these scripts during the day. Several studies have suggested IRT improves subjective sleep quality and reduces nightmares in PTSD patients, with large effects in several studies (see Casement and Swanson [116] and Hansen et al. [117] for meta-analyses). Notably, most studies included in these meta-analyses lacked controls, not all were conducted in PTSD samples, and several versions of IRT were used. Some research suggests that IRT may be more beneficial for patients with a primary nightmare disorder than for patients with PTSD and nightmares [118]. One of the few studies with an active control condition only showed small effects of IRT and no differences between groups on nightmare frequency [119]. An RCT comparing IRT to prazosin suggested that both treatments outperformed placebo in reducing insomnia and PTSD symptoms, but did not find differences between the two active treatments [120]. Findings from a recent meta-analysis suggest combining IRT with CBT-I may enhance treatment outcomes in comparison to IRT alone [121••], though it is unclear whether combined treatment outperforms CBT-I alone [122]. Finally, in 108 veterans randomized to CBT-I or IR + CBT-I, no differences were found between the groups in frequency or distress of nightmares [123••]. They conclude that IR may not be a necessary additive to CBT-I.
Another non-pharmacological treatment for nightmares is exposure, relaxation, and rescripting therapy (ERRT). Similar to IRT, this therapy involves rescripting selected nightmares during the day. ERRT involves an exposure therapy component that includes (1) psychoeducation regarding trauma; (2) discussion of the trauma; and (3) identifying trauma-related themes evidenced in the nightmare; thus, ERRT combines elements of trauma-focused psychotherapy with elements from nightmare-specific treatment [124]. Two RCTs have shown ERRT to be more effective than waitlist control in improving nightmares and reducing PTSD symptoms [125, 126]. Recently, a small pilot study showed ERRT may be efficacious in veterans with PTSD [127]. Interestingly, ERRT was less effective in those with suspected OSA as compared to the non-apnea group [128•]. As with IRT, future research in studies with larger study samples and active control conditions would provide additional evidence of ERRT’s efficacy as a non-pharmacological treatment for nightmares in PTSD.
Treatment of OSA in PTSD
Continuous Positive Airway Pressure Therapy (CPAP)
Nasal continuous positive airway pressure (CPAP) is the gold-standard treatment for OSA, with meta-analytic reports showing improvement in daytime sleepiness and health-related quality of life [129]. The standard prescription is to use CPAP whenever asleep, including during daytime naps. However, despite CPAP being the most efficacious treatment available to OSA patients, adherence is substandard (3 to 5 h per night), thereby significantly limiting its effectiveness [130].
Early studies of CPAP in patients diagnosed with OSA and PTSD were primarily concerned with investigating adherence. A recent meta-analysis found that CPAP adherence was lower in patients with both OSA and PTSD than OSA alone [23]. One study found that less use of CPAP was associated with greater baseline nightmare severity and greater daytime sleepiness [131]. Other studies found that greater use of CPAP was associated with a lower nightmare frequency [132, 133, 134••]. Additionally, one study found that CPAP use decreased nightmare frequency (from 10.32 nightmares per week to 5.26 with CPAP) and was predicted by CPAP adherence [85].
More recent studies directly examined the effect of CPAP therapy on PTSD symptom reduction. Three studies of CPAP therapy found small but consistent decreases in PTSD severity at 12 weeks [135•] and 6 months [136•, 137•]. Due to the dose response with outcomes, increasing adherence with desensitization requires further review [138]. While treating OSA only moderately affects PTSD severity, it may be considered a barrier to successful PTSD treatment and requiring intervention prior to initiating treatment.
Mandibular Repositioning Devices (MRDs)
AASM Clinical Guidelines for the treatment of snoring and OSA with oral appliances state that they are indicated for the treatment of mild to moderate OSA in patients (1) who prefer oral appliances to CPAP, (2) who do not respond to CPAP, (3) who are not suitable for treatment with CPAP, or (4) for whom treatment attempts with CPAP are unsuccessful [139]. There are two main classes of oral appliances: (1) mandibular repositioning devices (MRDs) and (2) tongue-retaining devices. Most research has been performed on MRDs. MRDs work through protruding the mandible to increase the anteroposterior dimensions of the oropharynx and the patency of the upper airway. A review of the literature suggests that 65% of patients experience a 50% reduction in AHI and that 35–40% of patients experience a normalization of the AHI (i.e., AHI ≤ 5) [140]. When compared directly to PAP in cross-over trials, PAP consistently shows greater improvements in AHI [141, 142]. Only one study examined MRDs in individuals with PTSD. One study compared CPAP to MRDs and found that while CPAP was more efficacious in reducing AHI, both treatments had mild reductions in PTSD severity [135•]. Importantly, the reported adherence to MRDs was significantly higher than CPAP with 58% preferring MAD to CPAP. MRDs may offer a viable alternative for veterans with OSA and PTSD who are non-adherent to CPAP.
Weight Loss/Exercise
Weight gain is a risk factor for OSA, with one study showing a dose–response relationship between weight gain and OSA such that a 10% weight gain is associated with a sixfold increase in the odds of moderate to severe OSA and a 32% increase in the AHI [143]. A meta-analysis found that while CPAP was the most efficacious in decreasing AHI, exercise training and dietary weight loss also were associated with decreases in AHI [144••]. While this was not examined in a co-occurring PTSD sample, it may be reasonable to assume these findings could carry over especially as PTSD is associated weight gain and low CPAP adherence [133].
Combined Sleep and PTSD Treatments
There are a limited number of studies examining combined treatment for sleep and PTSD. There is a case study that used CBT-I prior to trauma-specific exposure therapy which suggests that CBT-I helped transition the patient into the trauma therapy [145]. An RCT compared hypnosis prior to CPT to symptom monitoring prior to CPT found that both conditions showed improvement in sleep and PTSD, but the hypnosis condition showed significantly greater improvement than the control condition in sleep and depression, but not PTSD [114•]. Finally, a recent pilot study examined CBT-I prior to PE in veterans and found large effects for decreases in insomnia and PTSD symptoms and increases in quality of life [146••].
Summary and Future Directions
Advancement of evidence-based treatment of sleep disorders in the context of co-occurring PTSD offers a unique and underutilized opportunity to improve clinical care and research. While PTSD treatments are effective for PTSD symptom reduction, insomnia and OSA seem to require direct intervention. Our review suggests that PTSD treatments decrease PTSD severity and nightmare frequency, but do not fully resolve insomnia. There are no studies examining change in AHI over the course of PTSD treatment, but it is unlikely that PTSD treatment would affect OSA. While there are mixed findings as to whether insomnia affects PTSD treatment outcomes, untreated OSA seems to interfere with PTSD treatment.
There are currently no clinical guidelines for screening for sleep disorders in PTSD. We suggest a sleep and PTSD treatment decision tree (see Fig. 1). Clinically, we recommend a comprehensive sleep assessment to include OSA and insomnia screening, with treatment planning to match. Unfortunately, OSA is rarely screened due to the overlap with PTSD and insomnia symptoms. Due to the detrimental effect of OSA on PTSD treatments and health outcomes, we strongly recommend screening and treating OSA, even in lighter, younger individuals with PTSD prior to the start of PTSD treatment. We also recommend using independent measures for insomnia, such as the ISI or PSQI.
For sleep-specific interventions, CPAP therapy is recommended for OSA; however, there is lower CPAP adherence in PTSD samples. Given the importance of CPAP adherence to health and symptom outcomes, other treatment modalities and/or combination therapies may be warranted, such as CPAP desensitization, mandibular devices, exercise, or weight loss. For insomnia, CBT-I is the recommended treatment. While optimal sequencing with PTSD treatment is unclear, there is preliminary evidence that treating sleep prior to PTSD has benefits to sleep, PTSD, and quality-of-life out-comes. Nightmares significantly decrease with PTSD treatment and CBT-I, but nightmare-specific treatments are also effective and may be most beneficial for patients with primary nightmare disorder.
For pharmacological interventions for addressing sleep disturbances, we recommend following the 2017 VA/DOD guidelines [65], which are evidence-based and mimic the findings from our review. Specifically, there is a strong recommendation against the use of benzodiazepines for PTSD or insomnia due to a myriad of negative side effects. However, non-benzodiazepine hypnotics carry fewer risks, do not seem to increase risk of OSA, and increase sleep duration/quality, but need further evaluation with PTSD patients. While there are mixed reviews of prazosin, there is substantial evidence that it decreases nightmares, increases sleep quality, and may decrease nighttime arousals. However, future research is needed to identify the circumstances under which prazosin treatment should be selected and its effect on OSA. Antipsychotics are not recommended for routine use due to limited evidence supporting their efficacy and high propensity for adverse side effects. Finally, there are a host of commonly prescribed drugs (e.g., trazodone, hydroxyzine) that have insufficient evidence for recommendation for or against that require future research. Taken together, behavioral treatments, such as CBT-I for insomnia or CPAP for OSA, should be the first-line interventions for sleep disturbances in PTSD.
Future research is needed to examine the sequencing/combination of PTSD and sleep treatments and to elucidate the mechanisms between sleep and PTSD treatments outcomes (e.g., memory, concentration, extinction/safety learning). Moderating factors to consider in research for co-occurring PTSD and sleep disorders will be demographics (gender, age, ethnicity/race), type of trauma exposure (interpersonal, combat), medications, and sample (military, civilian). While future research is unlikely to identify a unique set of PTSD-specific sleep difficulties, examining sleep disorders offers potential to increase client-centered care and advance efficacy of current treatments.
There is limited research examining the role of treating sleep in individuals with PTSD and other co-occurring disorders. Anxiety, depression, chronic pain, traumatic brain injury, and substance use show the highest prevalence with PTSD [147], and each negatively affects sleep. Similar to previous findings where insomnia did not resolve following PTSD treatment, there is evidence that insomnia does not resolve when PTSD and the co-occurring disorder are adequately addressed [148]. This suggests that sleep disturbances may need direct intervention even when PTSD and the co-occurring disorder are treated.
Offering sleep treatment to individuals with PTSD is patient-focused and prudent. First, it addresses a common and impairing co-occurring disorder. Treating sleep in those with PTSD may translate to higher patient satisfaction and better quality-of-life outcomes. Second, offering sleep treatments may be a “stepping stone” before starting PTSD treatment. Third, addressing sleep problems first may impact the mechanisms involved with trauma-focused treatment. Better sleep may influence fear learning/recall, decrease emotional reactivity, increasing emotional coping and emotional processing, and increase cognitive abilities/concentration necessary for successful trauma-focused therapy. Together, increasing focus on sleep treatment among those with PTSD offers a logical, innovative, and empirically informed method for expanding patient care, augmenting existing treatments, and optimizing global outcomes.
Acknowledgments
The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. Writing was supported by VA RR&D CDA Grant #1lK2Rx002120–01 (P.J.C.) and by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs (L.D.S. and L.A.G.).
Footnotes
Compliance with Ethical Standards
Conflict of Interest P.J.C., L.D.S., C.S., L.A.G., and S.B.N. each declare no potential conflicts of interest.
M.J.M. is an unpaid member of the scientific advisory board for Owaves.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Compr Psychiatry 2000;41(6):469–78. [DOI] [PubMed] [Google Scholar]
- 2.Plumb TR, Peachey JT, Zelman DC. Sleep disturbance is common among servicemembers and veterans of Operations Enduring Freedom and Iraqi Freedom. Psychol Serv 2014;11(2):209–19. [DOI] [PubMed] [Google Scholar]
- 3.Jenkins MM, Colvonen PJ, Norman SB, Afari N, Allard CB, Drummond SP. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep 2015;38(10):1547–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neylan TC, Marmar CR, Metzler TJ, Weiss DS, Zatzick DF, Delucchi KL, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Sleep 1998;155(7):929–33. [DOI] [PubMed] [Google Scholar]
- 5.Krakow B, Melendrez D, Johnston L, Warner TD, Clark JO, Pacheco M, et al. Sleep-disordered breathing, psychiatric distress, and quality of life impairment in sexual assault survivors. J Nerv Ment Dis 2002;190(7):442–52. [DOI] [PubMed] [Google Scholar]
- 6. ••.Colvonen PJ, Masino T, Drummond SP, Myers US, Angkaw AC, Norman SB. Obstructive sleep apnea and posttraumatic stress disorder among OEF/OIF/OND veterans. J Clin Sleep Med 2015;11(5):513–8. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found high rates of OSA in younger, lower BMI veterans with PTSD suggesting the classic signs of OSA may not fit for OEF/OIF/OND veterans.
- 7.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep 2011;34(1):93–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baran B, Pace-Schott EF, Ericson C, Spencer RM. Processing of emotional reactivity and emotional memory over sleep. J Neurosci 2012;32(3):1035–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seelig AD, Jacobson IG, Smith B, Hooper TI, Boyko EJ, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. DTIC Document, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharon A, Levav I, Brodsky J, Shemesh AA, Kohn R. Psychiatric disorders and other health dimensions among holocaust survivors 6 decades later. Br J Psychiatry 2009;195(4):331–5. [DOI] [PubMed] [Google Scholar]
- 11.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol 2005;31(5):469–80. [DOI] [PubMed] [Google Scholar]
- 12.Brown TH, Mellman TA, Alfano CA, Weems CF. Sleep fears, sleep disturbance, and PTSD symptoms in minority youth exposed to hurricane Katrina. J Trauma Stress 2011;24(5):575–80. [DOI] [PubMed] [Google Scholar]
- 13.MC USNR RNM, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in US service members returning from military deployments. Mil Med 2010;175(10):759. [DOI] [PubMed] [Google Scholar]
- 14.Wallace D, Shafazand S, Ramos A, Carvalho D, Gardener H, Lorenzo D, et al. Insomnia characteristics and clinical correlates in operation enduring freedom/operation Iraqi freedom veterans with post-traumatic stress disorder and mild traumatic brain injury: an exploratory study. Sleep Med 2011;12(9):850–9. [DOI] [PubMed] [Google Scholar]
- 15.Levin R, Nielsen TA. Disturbed dreaming, posttraumatic stress disorder, and affect distress: a review and neurocognitive model. Psychol Bull 2007;133(3):482–528. [DOI] [PubMed] [Google Scholar]
- 16.Hasler BP, Germain A. Correlates and treatments of nightmares in adults. Sleep medicine clinics 2009;4(4):507–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. •.Creamer JL, Brock MS, Matsangas P, Motamedi V, Mysliwiec V. Nightmares in United States military personnel with sleep disturbances. J Clin Sleep Med 2018;14(03):419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study suggests that rates of nightmares were high in active duty personnel, but were rarely the reason for seeking sleep evaluations.
- 18.Schwab R, Goldberg A, Pack A. Sleep apnea syndromes. Fishman’s pulmonary diseases and disorders, vol. 1617 New York: McGraw-Hill Book Company; 1998. p. 37. [Google Scholar]
- 19.Krakow B, Melendrez D, Warner TD, Clark JO, Sisley BN, Dorin R, et al. Signs and symptoms of sleep-disordered breathing in trauma survivors: a matched comparison with classic sleep apnea patients. J Nerv Ment Dis 2006;194(6):433–9. [DOI] [PubMed] [Google Scholar]
- 20.Kinoshita LM, Yesavage JA, Noda A, Jo B, Hernandez B, Taylor J, et al. Modeling the effects of obstructive sleep apnea and hypertension in Vietnam veterans with PTSD. Sleep Breath 2012;16(4):1201–9. [DOI] [PubMed] [Google Scholar]
- 21.Liempt S, Westenberg HM, Arends J, Vermetten E. Obstructive sleep apnea in combat-related posttraumatic stress disorder: a controlled polysomnography study. Eur J Psychotraumatol 2011;2(1):8451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. •.Gupta MA, Simpson FC. Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med 2015;11(2):165–75. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study examined the prevalence and treatment of OSA in psychiatric populations, including PTSD; they found increased prevlence of OSA in those with PTSD compared to those without.
- 23. ••.Zhang Y, Weed JG, Ren R, Tang X, Zhang W. Prevalence of obstructive sleep apnea in patients with posttraumatic stress disorder and its impact on adherence to continuous positive airway pressure therapy: a meta-analysis. Sleep Med 2017;36:125–32. [DOI] [PubMed] [Google Scholar]; A meta-analysis to detect the pooled prevalence of OSA in PTSD and its impact on adherence to continuous positive airway pressure (CPAP) therapy.
- 24.Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 2005;28(11):1405–11. [DOI] [PubMed] [Google Scholar]
- 25.Williams SG, Collen J, Orr N, Holley AB, Lettieri CJ. Sleep disorders in combat-related PTSD. Sleep and Breathing 2015;19(1): 175–82. [DOI] [PubMed] [Google Scholar]
- 26. •.Rezaeitalab F, Mokhber N, Ravanshad Y, Saberi S, Rezaeetalab F. Different polysomnographic patterns in military veterans with obstructive sleep apnea in those with and without post-traumatic stress disorder. Sleep and Breathing 2018:1–6. [DOI] [PubMed] [Google Scholar]; In veterans with OSA, the authors compare sleep architecture between those with and without PTSD.
- 27. •.Germain A, McKeon AB, Campbell RL. Sleep in PTSD: conceptual model and novel directions in brain-based research and interventions. Current opinion in psychology 2017;14:84–9. [DOI] [PubMed] [Google Scholar]; This paper underscores sleep as a comorbid, rather than secondary, condition to PTSD. They review the temporal relationship and neurobilogical correlates of the two disorders.
- 28.Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev 2008;12(3):169–84. [DOI] [PubMed] [Google Scholar]
- 29.Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep 2010;33(1):69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev 2008;12(3):185–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bonn-Miller MO, Babson KA, Vujanovic AA, Feldner MT. Sleep problems and PTSD symptoms interact to predict marijuana use coping motives: a preliminary investigation. Journal of Dual Diagnosis 2010;6(2):111–22. [Google Scholar]
- 32.Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep 2013;36(7):1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol 2011;67(12):1240–58. [DOI] [PubMed] [Google Scholar]
- 34.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med 2008;173(3):230–5. [DOI] [PubMed] [Google Scholar]
- 35.Perlis ML, Giles DE, Mendelson WB, Bootzin RR, Wyatt JK. Psychophysiological insomnia: the behavioural model and a neurocognitive perspective. J Sleep Res 1997;6(3):179–88. [DOI] [PubMed] [Google Scholar]
- 36.Bootzin RR, Epstein D, Wood JM. Stimulus control instructions. Case studies in insomnia: Springer; 1991. p. 19–28. [Google Scholar]
- 37.Sjöström N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt. Psychiatry Res 2009;170(2): 208–11. [DOI] [PubMed] [Google Scholar]
- 38.Bernert RA, Joiner TE Jr, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep 2005;28(9):1135–41. [DOI] [PubMed] [Google Scholar]
- 39.Van Liempt S, Vermetten E, Geuze E, Westenberg H. Pharmacotherapeutic treatment of nightmares and insomnia in posttraumatic stress disorder. Ann N Y Acad Sci 2006;1071(1): 502–7. [DOI] [PubMed] [Google Scholar]
- 40.Kobayashi I, Sledjeski EM, Spoonster E, Fallon WF, Delahanty DL. Effects of early nightmares on the development of sleep disturbances in motor vehicle accident victims. J Trauma Stress 2008;21(6):548–55. [DOI] [PubMed] [Google Scholar]
- 41.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Physical health conditions associated with posttraumatic stress disorder in US older adults: results from wave 2 of the National Epidemiologic Survey on alcohol and related conditions. J Am Geriatr Soc 2012;60(2):296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA 2003;290(14):1906–14. [DOI] [PubMed] [Google Scholar]
- 43.Sledjeski EM, Speisman B, Dierker LC. Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey-Replication (NCS-R). J Behav Med 2008;31(4):341–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krakow BJ, Ulibarri VA, Moore BA, McIver ND. Posttraumatic stress disorder and sleep-disordered breathing: a review of comorbidity research. Sleep Med Rev 2015;24:37–45. [DOI] [PubMed] [Google Scholar]
- 45. ••.Jaoude P, Vermont LN, Porhomayon J, El-Solh AA. Sleep-disordered breathing in patients with post-traumatic stress disorder. Ann Am Thorac Soc 2015;12(2):259–68. [DOI] [PubMed] [Google Scholar]; The article is a thorough review of the literature on the relationship between SDB and PTSD; they propose pathways and mechanisms between the two disorders.
- 46.De Kloet C, Vermetten E, Geuze E, Lentjes E, Heijnen C, Stalla G, et al. Elevated plasma corticotrophin-releasing hormone levels in veterans with posttraumatic stress disorder. Prog Brain Res 2007;167:287–91. [DOI] [PubMed] [Google Scholar]
- 47.Kim E, Grover LM, Bertolotti D, Green TL. Growth hormone rescues hippocampal synaptic function after sleep deprivation. Am J Phys Regul Integr Comp Phys 2010;298(6):R1588–R96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spoormaker VI, Schröter MS, Andrade KC, Dresler M, Kiem SA, Goya-Maldonado R, et al. Effects of rapid eye movement sleep deprivation on fear extinction recall and prediction error signaling. Hum Brain Mapp 2012;33(10):2362–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arnetz BB, Templin T, Saudi W, Jamil H. Obstructive sleep apnea, posttraumatic stress disorder, and health in immigrants. Psychosom Med 2012;74(8):824–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Krakow B, Melendrez D, Ferreira E, Clark J, Warner TD, Sisley B, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest 2001;120(6):1923–9. [DOI] [PubMed] [Google Scholar]
- 51.Krakow B, Melendrez D, Pedersen B, Johnston L, Hollifield M, Germain A, et al. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry 2001;49(11):948–53. [DOI] [PubMed] [Google Scholar]
- 52. •.Brock MS, Mysliwiec V. Comorbid insomnia and sleep apnea: a prevalent but overlooked disorder. Sleep Breath 2018;22:1–3. [DOI] [PubMed] [Google Scholar]; A letter to the editor which suggests that OSA is often overlooked and may contribute to detrimental outcomes. They make treatment recommendations to include OSA screening and CPAP therapy.
- 53.Gupta MA, Knapp K. Cardiovascular and psychiatric morbidity in obstructive sleep apnea (OSA) with insomnia (sleep apnea plus) versus obstructive sleep apnea without insomnia: a case–control study from a nationally representative US sample. PLoS One 2014;9(3):e90021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. •.El-Solh AA, Adamo D, Kufel T. Comorbid insomnia and sleep apnea in veterans with post-traumatic stress disorder. Sleep Breath 2018:1–9. [DOI] [PubMed] [Google Scholar]; This study found that veterans with PTSD, insomnia, and OSA had worse quality of life, sleep, and depression than veterans with PTSD and OSA only.
- 55.Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The clinician-administered PTSD scale for DSM-5 (CAPS-5). Interview available from the National Center for PTSD at www.ptsd.va.gov. 2013. [Google Scholar]
- 56.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD checklist for DSM-5 (PCL-5) www.ptsd.va.gov. 2013. [Google Scholar]
- 57.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 58.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2(4):297–307. [DOI] [PubMed] [Google Scholar]
- 59.Straus LD, Drummond S, Nappi CM, Jenkins MM, Norman SB. Sleep variability in military-related PTSD: a comparison to primary insomnia and healthy controls. J Trauma Stress 2015;28(1):8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Krakow B Nightmare complaints in treatment-seeking patients in clinical sleep medicine settings: diagnostic and treatment implications. Sleep 2006;29(10):1313–9. [DOI] [PubMed] [Google Scholar]
- 61.Gehrman P CBT for insomnia in veterans with PTSD. Sleep Med 2015;16:S9–S10. [Google Scholar]
- 62.Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. STOP Questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008;108(5):812–21. [DOI] [PubMed] [Google Scholar]
- 63.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999;131(7):485–91. [DOI] [PubMed] [Google Scholar]
- 64.Germain A, Hall M, Katherine Shear M, Nofzinger EA, Buysse DJ. Ecological study of sleep disruption in PTSD. Ann N Y Acad Sci 2006;1071(1):438–41. [DOI] [PubMed] [Google Scholar]
- 65.guideline VDcp. VA/DOD clinical practice guideline for management of post-traumatic stress Washington (DC): Department of Veterans Affairs, Department of Defense; 2010. 2016. [Google Scholar]
- 66. ••.Guina J, Rossetter SR, DeRHODES BJ, Nahhas RW, Welton RS. Benzodiazepines for PTSD: a systematic review and meta-analysis. J Psychiatr Pract 2015;21(4):281–303. [DOI] [PubMed] [Google Scholar]; This meta-analysis suggests benzodiazepines have modest, beneficial effects on PTSD and sleep but risks associated with their use outweigh potential short-term benefits.
- 67.Luyster FS, Buysse DJ, Strollo PJ Jr. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med 2010;6(2):196–204. [PMC free article] [PubMed] [Google Scholar]
- 68.Sloan EP, Shapiro CM. Hypnotics should never be used in patients with sleep apnea. J Psychosom Res 1993;37:59–65. [PubMed] [Google Scholar]
- 69.Huedo-Medina TB, Kirsch I, Middlemass J, Klonizakis M, Siriwardena AN. Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: meta-analysis of data submitted to the Food and Drug Administration. BMJ 2012;345:e8343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pollack MH, Hoge EA, Worthington JJ, Moshier SJ, Wechsler RS, Brandes M, et al. Eszopiclone for the treatment of posttraumatic stress disorder and associated insomnia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 2011;72(7): 892–7. [DOI] [PubMed] [Google Scholar]
- 71.Zhang XJ, Li QY, Wang Y, Xu HJ, Lin YN. The effect of non-benzodiazepine hypnotics on sleep quality and severity in patients with OSA: a meta-analysis. Sleep Breath 2014;18(4):781–9. [DOI] [PubMed] [Google Scholar]
- 72.Warner M, Dorn M, Peabody C. Survey on the usefulness of trazodone in patients with PTSD with insomnia or nightmares. Pharmacopsychiatry 2001;34(04):128–31. [DOI] [PubMed] [Google Scholar]
- 73.Mendelson WB. A review of the evidence for the efficacy and safety of trazodone in insomnia. J Clin Psychiatry 2005;66(4): 469–76. [DOI] [PubMed] [Google Scholar]
- 74.Friedmann PD, Rose JS, Swift R, Stout RL, Millman RP, Stein MD. Trazodone for sleep disturbance after alcohol detoxification: a double-blind, placebo-controlled trial. Alcohol Clin Exp Res 2008;32(9):1652–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smales ET, Edwards BA, Deyoung PN, McSharry DG, Wellman A, Velasquez A, et al. Trazodone effects on obstructive sleep apnea and non-REM arousal threshold. Ann Am Thorac Soc 2015;12(5):758–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Roth AJ, McCall WV, Liguori A. Cognitive, psychomotor and polysomnographic effects of trazodone in primary insomniacs. J Sleep Res 2011;20(4):552–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatr 2002;159(10):1777–9. [DOI] [PubMed] [Google Scholar]
- 78.Krystal JH, Pietrzak RH, Rosenheck RA, Cramer JA, Vessicchio J, Jones KM, et al. Sleep disturbance in chronic military-related PTSD: clinical impact and response to adjunctive risperidone in the Veterans Affairs Cooperative Study #504. J Clin Psychiatry 2016;77(4):483–91. [DOI] [PubMed] [Google Scholar]
- 79. •.Villarreal G, Hamner MB Cañive JM, Robert S, Calais LA, Durklaski V, et al. Efficacy of quetiapine monotherapy in post-traumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatr 2016;173(12):1205–12. [DOI] [PubMed] [Google Scholar]; This study found that quetiapine monotherapy improved PTSD symptoms overall, but had modest and transient effects on insomnia.
- 80.Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353(12):1209–23. [DOI] [PubMed] [Google Scholar]
- 81.Green B Prazosin in the treatment of PTSD. J Psychiatr Pract 2014;20(4):253–9. [DOI] [PubMed] [Google Scholar]
- 82. •.George KC, Kebejian L, Ruth LJ, Miller CW, Himelhoch S. Meta-analysis of the efficacy and safety of prazosin versus placebo for the treatment of nightmares and sleep disturbances in adults with posttraumatic stress disorder. J Trauma Dissociation 2016;17(4): 494–510. [DOI] [PubMed] [Google Scholar]; This meta-analysis identified prazosin as more effective than placebo in improving nightmares, sleep quality, and illness severity.
- 83. ••.Khachatryan D, Groll D, Booij L, Sepehry AA, Schütz CG. Prazosin for treating sleep disturbances in adults with posttraumatic stress disorder: a systematic review and meta-analysis of randomized controlled trials. Gen Hosp Psychiatry 2016;39:46–52. [DOI] [PubMed] [Google Scholar]; This meta-anlysis examined 6 RTCs and found that prazosin impoved sleep quality and reduced overall PTSD symptoms.
- 84. •.Raskind MA, Peskind ER, Chow B, Harris C, Davis-Karim A, Holmes HA, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med 2018;378(6):507–17. [DOI] [PubMed] [Google Scholar]; This study found that prazosin showed no differences when compared to placebo in alleviate distressing dreams, improve sleep quality, or show improvement in any other PTSD symptom cluster.
- 85.Tamanna S, Parker JD, Lyons J, Ullah M. The effect of continuous positive air pressure (CPAP) on nightmares in patients with post-traumatic stress disorder (PTSD) and obstructive sleep apnea (OSA). J Clin Sleep Med 2014;10(6):631–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med 2017;13(2): 307–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ahmadpanah M, Sabzeiee P, Hosseini SM, Torabian S, Haghighi M, Jahangard L, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology 2014;69(4):235–42. [DOI] [PubMed] [Google Scholar]
- 88.Galovski TE, Monson C, Bruce SE, Resick PA. Does cognitive– behavioral therapy for PTSD improve perceived health and sleep impairment? J Trauma Stress 2009;22(3):197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gutner CA, Casement MD, Gilbert KS, Resick PA. Change in sleep symptoms across cognitive processing therapy and prolonged exposure: a longitudinal perspective. Behav Res Ther 2013;51(12):817–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Belleville G, Guay S, Marchand A. Persistence of sleep disturbances following cognitive-behavior therapy for posttraumatic stress disorder. J Psychosom Res 2011;70(4):318–27. [DOI] [PubMed] [Google Scholar]
- 91. ••.Pruiksma KE, Taylor DJ, Wachen JS, Mintz J, Young-McCaughan S, Peterson AL, Yarvis JS, Borah EV, Dondanville KA, Litz BT, Hembree EA, Resick PA Residual sleep disturbances following PTSD treatment in active duty military personnel. Psychol Trauma 2016;8(6):697–701. [DOI] [PubMed] [Google Scholar]; This study found that insomnia is the most frequently reported symptom before and after PTSD treatment in active duty military participants, and did not decrease following PTSD treatment.
- 92.Zayfert C, DeViva JC. Residual insomnia following cognitive behavioral therapy for PTSD. J Trauma Stress 2004;17(1):69–73. [DOI] [PubMed] [Google Scholar]
- 93. •.Levrier K, Leathead C, Bourdon D-É, Lacerte S, Marchand A, Belleville G. The impact of cognitive-behavioral therapies for nightmares and prazosin on the reduction of post-traumatic night-mares, sleep, and PTSD symptoms: a systematic review and meta-analysis of randomized and non-randomized studies. A multidimensional approach to post-traumatic stress disorder-from theory to practice: InTech; 2016. [Google Scholar]; This meta-analysis found that both prazosin and CBTs for nightmares reduced PTSD, sleep symptoms, and nightmares; however, prazosin had larger effects sizes on reducing nightmares than CBTs for nightmare treatments.
- 94. ••.Brownlow JA, McLean CP, Gehrman PR, Harb GC, Ross RJ, Foa EB. Influence of sleep disturbance on global functioning after posttraumatic stress disorder treatment. J Trauma Stress 2016;29(6):515–21. [DOI] [PubMed] [Google Scholar]; This study found that PE was effective in reducing PTSD and insomnia symptoms, but that higher insomnia and nightmares predicted poorer global functioning post-treatment. This suggests that addressing insomnia and nightmares may extend beyond just PTSD/insomnia symptoms.
- 95. •.López CM, Lancaster CL, Gros DF, Acierno R. Residual sleep problems predict reduced response to prolonged exposure among veterans with PTSD. J Psychopathol Behav Assess 2017;39(4): 755–63. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found that greater residual insomnia symptoms following PE were predictive of smaller improvement in PTSD symptoms.
- 96. ••.Lommen MJ, Grey N, Clark DM, Wild J, Stott R, Ehlers A. Sleep and treatment outcome in posttraumatic stress disorder: results from an effectiveness study. Depress Anxiety 2016;33(7):575–83. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found that patients with worse comorbid depression and poorer sleep showed less decrease in PTSD symptoms with CT-PTSD treatment.
- 97. ••.Woodward E, Hackmann A, Wild J, Grey N, Clark DM, Ehlers A. Effects of psychotherapies for posttraumatic stress disorder on sleep disturbances: results from a randomized clinical trial. Behav Res Ther 2017;97:75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found that CT-PTSD, compared to waitlist, improved self-reported sleep duration and nightmares. Additionally, baseline sleep did not interfere with PTSD treatment outcomes.
- 98. ••.Sexton MB, Avallone KM, Smith ER, Porter KE, Ashrafioun L, Arnedt JT, et al. Sleep disturbances as predictors of prolonged exposure therapy effectiveness among veterans with PTSD. Psychiatry Res 2017;256:118–23. [DOI] [PubMed] [Google Scholar]; This study found that higher PSQI scores were related to higher baseline PCL scores. PSQI scores were not associated with reduced effectiveness of PE treatment or slope of PTSD symptom changes.
- 99. ••.Mesa F, Dickstein BD, Wooten VD, Chard KM. Response to cognitive processing therapy in veterans with and without obstructive sleep apnea. J Trauma Stress 2017;30(6):646–55. [DOI] [PubMed] [Google Scholar]; This study found that veterans with OSA reported greater PTSD severity over the course of CPT than veterans without OSA. Veterans treated with CPAP reported greater PTSD treatment improvements than veterans with untreated OSA.
- 100. ••.Reist C, Gory A, Hollifield M. Sleep-disordered breathing impact on efficacy of prolonged exposure therapy for posttraumatic stress disorder. J Trauma Stress 2017;30(2):186–9. [DOI] [PubMed] [Google Scholar]; This study found that untreated sleep disordered breathing reduced the efficacy of PE.
- 101.Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2016;165(2):125–33. [DOI] [PubMed] [Google Scholar]
- 102.Bastien CH, Morin CM, Ouellet M-C, Blais FC, Bouchard S. Cognitive-behavioral therapy for insomnia: comparison of individual therapy, group therapy, and telephone consultations. J Consult Clin Psychol 2004;72(4):653–9. [DOI] [PubMed] [Google Scholar]
- 103.Edinger JD, Means MK. Cognitive–behavioral therapy for primary insomnia. Clin Psychol Rev 2005;25(5):539–58. [DOI] [PubMed] [Google Scholar]
- 104.Omvik S, Pallesen S, Havik OE, Kvale G, Nordhus IH. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA 2006;295(24):2851–8. [DOI] [PubMed] [Google Scholar]
- 105.Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia. An American Academy of sleep medicine review. Sleep 1999;22(8):1134–56. [DOI] [PubMed] [Google Scholar]
- 106. ••.Wu JQ, Appleman ER, Salazar RD, Ong JC. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Intern Med 2015;175(9):1461–72. [DOI] [PubMed] [Google Scholar]; This meta-analysis found that CBT-I is efficacious for improving comorbid insomnia in patients with PTSD.
- 107. ••.Ho FY-Y, Chan CS, Tang KN-S. Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: a meta-analysis of randomized controlled trials. Clin Psychol Rev 2016;43:90–102. [DOI] [PubMed] [Google Scholar]; This meta-analysis found that CBT-I is efficacious and feasible in treating PTSD symptoms.
- 108.Talbot LS, Maguen S, Metzler TJ, Schmitz M, McCaslin SE, Richards A, et al. Cognitive behavioral therapy for insomnia in posttraumatic stress disorder: a randomized controlled trial. Sleep 2014;37(2):327–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ulmer CS, Edinger JD, Calhoun PS. A multi-component cognitive-behavioral intervention for sleep disturbance in veterans with PTSD: a pilot study. J Clin Sleep Med 2011;7(1):57–68. [PMC free article] [PubMed] [Google Scholar]
- 110.Margolies SO, Rybarczyk B, Vrana SR, Leszczyszyn DJ, Lynch J. Efficacy of a cognitive-behavioral treatment for insomnia and nightmares in Afghanistan and Iraq veterans with PTSD. J Clin Psychol 2013;69(10):1026–42. [DOI] [PubMed] [Google Scholar]
- 111.Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand 2015;131(5): 350–9. [DOI] [PubMed] [Google Scholar]
- 112.Nakamura Y, Lipschitz DL, Landward R, Kuhn R, West G. Two sessions of sleep-focused mind–body bridging improve self-reported symptoms of sleep and PTSD in veterans: a pilot randomized controlled trial. J Psychosom Res 2011;70(4):335–45. [DOI] [PubMed] [Google Scholar]
- 113.King HC, Spence DL, Hickey AH, Sargent P, Elesh R, Connelly CD. Auricular acupuncture for sleep disturbance in veterans with post-traumatic stress disorder: a feasibility study. Mil Med 2015;180(5):582–90. [DOI] [PubMed] [Google Scholar]
- 114. •.Galovski TE, Harik JM, Blain LM, Elwood L, Gloth C, Fletcher TD. Augmenting cognitive processing therapy to improve sleep impairment in PTSD: a randomized controlled trial. J Consult Clin Psychol 2016;84(2):167–77. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found that hypnosis plus CPT outperformed CPT alone on PTSD symptoms only in deperessed patients.
- 115.Abramowitz EG, Barak Y, Ben-Avi I, Knobler HY. Hypnotherapy in the treatment of chronic combat-related PTSD patients suffering from insomnia: a randomized, zolpidem-controlled clinical trial. Int J Clin Exp Hypn 2008;56(3):270–80. [DOI] [PubMed] [Google Scholar]
- 116.Casement MD, Swanson LM. A meta-analysis of imagery rehearsal for post-trauma nightmares: effects on nightmare frequency, sleep quality, and posttraumatic stress. Clin Psychol Rev 2012;32(6):566–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hansen K, Höfling V, Kröner-Borowik T, Stangier U, Steil R. Efficacy of psychological interventions aiming to reduce chronic nightmares: a meta-analysis. Clin Psychol Rev 2013;33(1):146–55. [DOI] [PubMed] [Google Scholar]
- 118.Thünker J, Pietrowsky R. Effectiveness of a manualized imagery rehearsal therapy for patients suffering from nightmare disorders with and without a comorbidity of depression or PTSD. Behav Res Ther 2012;50(9):558–64. [DOI] [PubMed] [Google Scholar]
- 119.Cook JM, Harb GC, Gehrman PR, Cary MS, Gamble GM, Forbes D, et al. Imagery rehearsal for posttraumatic nightmares: a randomized controlled trial. J Trauma Stress 2010;23(5):553–63. [DOI] [PubMed] [Google Scholar]
- 120.Germain A, Richardson R, Moul DE, Mammen O, Haas G, Forman SD, et al. Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US military veterans. J Psychosom Res 2012;72(2):89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. ••.Seda G, Sanchez-Ortuno MM, Welsh CH, Halbower AC, Edinger JD. Comparative meta-analysis of prazosin and imagery rehearsal therapy for nightmare frequency, sleep quality, and posttraumatic stress. J Clin Sleep Med 2015;11(1):11–22. [DOI] [PMC free article] [PubMed] [Google Scholar]; This meta-analysis suggests that adding CBT to IRT enchances treatment outcomes related to sleep quality and PTSD.
- 122.Scott JC, Harb G, Brownlow JA, Greene J, Gur RC, Ross RJ. Verbal memory functioning moderates psychotherapy treatment response for PTSD-related nightmares. Behav Res Ther 2017;91:24–32. [DOI] [PubMed] [Google Scholar]
- 123. ••.Ross R, Harb G. CBT for nightmares in OEF/OIF veterans. Philadelphia Research and Education Foundation Philadelphia United States, 2015. [Google Scholar]; Compared CBT-I alone to IR + CBT-I and found no differences between the two groups on night-mare frequency or distress, suggesting CBT-I alone may be effective in reducing nightmares.
- 124.Rybarczyk B, Stepanski E, Fogg L, Lopez M, Barry P, Davis A. A placebo-controlled test of cognitive-behavioral therapy for comorbid insomnia in older adults. J Consult Clin Psychol 2005;73(6): 1164–74. [DOI] [PubMed] [Google Scholar]
- 125.Davis JL, Wright DC. Randomized clinical trial for treatment of chronic nightmares in trauma-exposed adults. J Trauma Stress 2007;20(2):123–33. [DOI] [PubMed] [Google Scholar]
- 126.Davis JL, Rhudy JL, Pruiksma KE, Byrd P, Williams AE, McCabe KM, et al. Physiological predictors of response to exposure, relaxation, and rescripting therapy for chronic nightmares in a randomized clinical trial. J Clin Sleep Med 2011;7(6):622–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Balliett NE, Davis JL, Miller KE. Efficacy of a brief treatment for nightmares and sleep disturbances for veterans. Psychol Trauma 2015;7(6):507–15. [DOI] [PubMed] [Google Scholar]
- 128. •.Miller K, Cranston C, Simonet D, Pruiksma K, Davis J. The impact of suspected sleep apnea on exposure, relaxation, and rescripting therapy (ERRT): a preliminary examination. J Sleep Disord Med Care 2018;1(1) [Google Scholar]; This study found symptom levels for participants with suspected OSA remained elevated after ERRT compared to non-apnea, which suggests OSA may be a primary treatment focus.
- 129.Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT. Continuous positive airway pressure therapy for treating gess in a diverse population with obstructive sleep apnea: results of a meta-analysis. Arch Intern Med 2003;163(5):565–71. [DOI] [PubMed] [Google Scholar]
- 130.Stepnowsky CJ, Moore PJ. Nasal CPAP treatment for obstructive sleep apnea: developing a new perspective on dosing strategies and compliance. J Psychosom Res 2003;54(6):599–605. [DOI] [PubMed] [Google Scholar]
- 131.El-Solh AA, Ayyar L, Akinnusi M, Relia S, Akinnusi O. Positive airway pressure adherence in veterans with posttraumatic stress disorder. Sleep 2010;33(11):1495–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Krakow B, Germain A, Tandberg D, Koss M, Schrader R, Hollifield M, et al. Sleep breathing and sleep movement disorders masquerading as insomnia in sexual-assault survivors. Compr Psychiatry 2000;41(1):49–56. [DOI] [PubMed] [Google Scholar]
- 133.Collen JF, Lettieri CJ, Hoffman M. The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med 2012;8(6):667–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. ••.Lettieri CJ, Williams SG, Collen JF. OSA syndrome and posttraumatic stress disorder: clinical outcomes and impact of positive airway pressure therapy. Chest 2016;149(2):483–90. [DOI] [PubMed] [Google Scholar]; This study found that greater use of CPAP was associated with a lower nightmare frequency.
- 135. •.El-Solh AA, Vermont L, Homish GG, Kufel T. The effect of continuous positive airway pressure on post-traumatic stress disorder symptoms in veterans with post-traumatic stress disorder and obstructive sleep apnea: a prospective study. Sleep Med 2017;33:145–50. [DOI] [PubMed] [Google Scholar]; This study found that treatment with CPAP had small symptoms reduction in PTSD that remained at 6-month follow-up.
- 136. •.Orr JE, Smales C, Alexander TH, Stepnowsky C, Pillar G, Malhotra A, et al. Treatment of OSA with CPAP is associated with improvement in PTSD symptoms among veterans. J Clin Sleep Med 2017;13(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]; Evidence showed that treatment with CPAP had small symptoms reduction in PTSD that remained at 6-month follow-up.
- 137. •.Ullah M, Campbell DG, Bhagat R, Lyons JA, Tamanna S. Improving PTSD symptoms and preventing progression of subclinical PTSD to an overt disorder by treating comorbid OSAwith CPAP. J Clin Sleep Med 2017;13(10):1191–8. [DOI] [PMC free article] [PubMed] [Google Scholar]; Found that treatment with CPAP had small symptoms reduction in PTSD that remained at 6-month follow-up and that CPAP therapy may limit progression of sub-clinical PTSD.
- 138.Goldstein LA, Colvonen PJ, Sarmiento KF. Advancing treatment of comorbid PTSD and OSA. J Clin Sleep Med 2017;13(6):843–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015: an American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine clinical practice guideline. J Clin Sleep Med 2015;11(7):773–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep 2006;29(2):244–62. [DOI] [PubMed] [Google Scholar]
- 141.Barnes M, McEvoy RD, Banks S, Tarquinio N, Murray CG, Vowles N, et al. Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med 2004;170(6):656–64. [DOI] [PubMed] [Google Scholar]
- 142.Engleman HM, McDonald JP, Graham D, Lello GE, Kingshott RN, Coleman EL, et al. Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 2002;166(6):855–9. [DOI] [PubMed] [Google Scholar]
- 143.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000;284(23):3015–21. [DOI] [PubMed] [Google Scholar]
- 144. ••.Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R, et al. Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med 2017;30:7–14. [DOI] [PubMed] [Google Scholar]; In a non-PTSD sample, CPAP was efficacious, followed by exercise and dietary weight loss, for reducing AHI.
- 145.Baddeley JL, Gros DF. Cognitive behavioral therapy for insomnia as a preparatory treatment for exposure therapy for posttraumatic stress disorder. Am J Psychother 2013;67(2):199–210. [DOI] [PubMed] [Google Scholar]
- 146. ••.Colvonen PJ, Drummond SP, Angkaw AC, Norman SB. Cognitive behavioral therapy for insomnia integrated with prolonged exposure: rationale and pilot study. Psychological Trauma: Theory, Research, Practice, and Policy. Under Review [DOI] [PMC free article] [PubMed] [Google Scholar]; This study examined CBT-I prior to PE and found statistical and clinical changes in insomnia and PTSD symptoms.
- 147.Galatzer-Levy IR, Nickerson A, Litz BT, Marmar CR. Patterns of lifetime PTSD comorbidity: a latent class analysis. Depress Anxiety 2013;30(5):489–96. [DOI] [PubMed] [Google Scholar]
- 148.Colvonen PJ, Ellison J, Haller M, Norman SB. Examining insomnia and PTSD over time in veterans in residential treatment for substance use disorders and PTSD. Behav Sleep Med 2018:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]