Abstract
Background
Cardiovascular conditions are common in US Army and civilian populations. The recently developed concept of ideal cardiovascular health provides a new approach to evaluating population cardiovascular status.
Methods and Results
We defined a cohort of 263 430 active duty Army personnel, aged 17 to 64 years, who completed a 2012 physical examination and a corresponding subset of the noninstitutionalized, civilian US population, who participated in the National Health and Nutrition Examination Survey (NHANES) 2011 to 2012 cycle. We compared 4 cardiovascular health metrics (current smoking, body mass index, blood pressure, and diabetic status) between Army and civilian groups overall, and separately by sex, race/ethnicity, and age. The Army population was younger, was less often women or Hispanic, and had less post–high school education than the NHANES population. Smoking rates were ≈20% in the Army and NHANES groups, but <15% among Army women and Hispanics. Overall, one third of the Army and NHANES groups and NHANES women, but nearly half of Army women, demonstrated ideal body mass index. Ideal blood pressure was strikingly less prevalent in the Army than NHANES participants (30% versus 55%). Diabetes mellitus was rare in both groups.
Conclusions
Ideal cardiovascular health was less prevalent in the Army than NHANES group, despite exclusion of the least healthy recruits. Prevalence of ideal body mass index and blood pressure was low in both the Army and NHANES groups, even at early adult ages. This finding reveals the need for policy changes to promote, preserve, and improve ideal cardiovascular health in both the Army and the US population as a whole.
Keywords: cardiovascular disease prevention, cardiovascular health, diabetes mellitus, hypertension, obesity, smoking, US Army
Subject Categories: Primary Prevention; Epidemiology; High Blood Pressure; Obesity; Diabetes, Type 2
Clinical Perspective
What Is New?
This report compares prevalence of 4 ideal cardiovascular health (CVH) metrics (current smoking, body mass index, blood pressure, and diabetic status) between a large sample of active duty US Army personnel and a corresponding subset of the civilian US population, from the National Health and Nutrition Examination Survey.
Even at early adult ages, prevalence of ideal body mass index and blood pressure was strikingly low in both populations, suggesting the age‐related decline in CVH shown in other studies has already adversely affected both Army and civilian populations by the ages of 17 to 29 years.
Ideal CVH was even less prevalent in the Army, despite health‐related exclusion criteria in Army recruitment.
What Are the Clinical Implications?
To improve population CVH for both the US Army and civilian populations, behavioral and policy changes are needed to promote, preserve, and, when compromised, restore ideal CVH.
For clinical practice, this and previous studies support long‐standing recommendations to prevent the emergence of cardiovascular risk, now expressed as loss of ideal CVH, through primordial prevention from early childhood on.
On the basis of the estimated proportion of individuals with ideal CVH in each population, there is compelling need as well as substantial opportunity to improve the health of the nation and, in particular, the fitness of the US Army.
Cardiovascular disease (CVD) is the leading cause of death in the United States among both men and women, accounting for 1 in every 4 deaths annually.1 The active duty component of the US Army (hereafter, “Army”) is afflicted more by CVD than by any other chronic disease.2 Moreover, CVD prevalence rates among active duty Army personnel have increased over the past decade (6.8% in 2007 versus 9.4% in 2014).2 Prevalence of risk factors associated with CVD, cancer, chronic respiratory disease, and other conditions has also increased in US military personnel in recent years.3, 4, 5, 6, 7 In 2011, active duty Army respondents reported the following: overweight or obesity, 68%; cigarette use, 27%; diagnosed high blood pressure (BP), 18%; and diagnosed high cholesterol, 15%.8 Given the likely impact of these factors not only on potential military recruits but on medical readiness to deploy, CVD is a present threat to national security and poses significant financial costs to the military health system.2, 9
The concept of cardiovascular health (CVH) offers a promising new approach to this problem. The American Heart Association (AHA), in 2010, defined ideal, intermediate, and poor CVH (in the absence of manifest CVD) in terms of 7 metrics and a 7‐item composite score, comprising 4 modifiable health behaviors (current smoking, physical activity, diet score, and body mass index [BMI]) and 3 health factors (systolic BP [SBP] and diastolic BP [DBP], total blood cholesterol concentration, and fasting plasma glucose concentration).10 This reframing of the approach to reducing the population burden of CVD replaces the terms “risk behaviors” and “risk factors” with “health behaviors” and “health factors,” respectively, shifting the focus to positive attributes and their promotion and preservation through primordial prevention strategies. The choice of these metrics to define CVH was based, in part, on the supporting evidence: both long‐term prospective population data showing better health, longevity, and quality of life with ideal CVH and intervention trials demonstrating modifiability of these 7 metrics.10, 11, 12, 13, 14, 15, 16 In addition, corresponding data for each one would be available continuously for successive representative samples of the US population, through the National Health and Nutrition Examination Surveys (NHANES), permitting their ongoing surveillance for the civilian, noninstitutionalized US population. On the basis of this definition, AHA adopted as its 2020 Strategic Impact Goal “to improve the cardiovascular health of all Americans by 20% while reducing deaths from cardiovascular diseases and stroke by 20%.”10 Strategies to improve population CVH are potentially applicable to any population, including the US military.
The Army monitors service members' health to sustain a physically fit, combat‐ready military force. This periodic assessment includes 4 of the 7 metrics now identified with CVH: smoking, BMI, BP, and diabetic status. Although some studies have compared CVD risk factors in the military,16, 17 the status of military personnel in terms of this new concept, and how it compares to the CVH of civilians, is unknown. We, therefore, determined the weighted age‐standardized prevalence of each of these 4 CVH metrics in active duty Army personnel, in comparison with the US civilian population, represented by NHANES. We also examined these data by sex, race/ethnicity, and age. Because of Army fitness standards, both at recruitment and after enlistment, we hypothesized that ideal CVH would be more prevalent at every age in the Army than among civilians of comparable age.
Methods
Study Subjects
Army cohort
We examined data for Army personnel, aged 17 to 64 years, who completed the Periodic Health Assessment in 2012. The Periodic Health Assessment monitors service members' medical readiness to deploy.18 Exclusions (aged ≥65 years or pregnant) yielded an analytic cohort of 263 430 active duty (full‐time) service members. Army data were weighted to the estimated 2012 Army population of 497 490 active duty service members using age, sex, race/ethnicity, education, rank, service component, and deployment estimates and adjusting for nonresponse on the 2012 Periodic Health Assessment.
Civilian sample
We examined data from US civilians, aged 17 to 64 years, from the 2011 to 2012 cycle of NHANES, a cross‐sectional survey by the National Center for Health Statistics, Centers for Disease Control and Prevention, to monitor the health and nutritional status of the noninstitutionalized US population.19 In NHANES, participants were interviewed at home and completed anthropometric and physiological examinations at a mobile examination center. NHANES uses a complex, multistage probability design with oversampling of older people, Hispanics, blacks, Asian Americans, and low‐income non‐Hispanic whites. NHANES data are weighted using US population estimates (based on age, sex, race/ethnicity, and income) and adjusted for multistage sampling and response rates.19, 20 We applied exclusions (aged ≥65 years or pregnant) to match those of the Army cohort. This yielded an analytic sample of 4797 civilians, which was weighted to an estimated US population of 198 146 000 civilians in the same age range.
The University of Pennsylvania (Philadelphia, PA) institutional review board and a Department of Defense Human Research Protection Official approved this study. Because this study relied on secondary collected Army and civilian data that were coded and deidentified to not be readily ascertainable by the research team, consent was not required. Under US Army policy, the data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure; however, NHANES data files and documentation are publicly available from the Centers for Disease Control and Prevention website.
Measures
Demographic Characteristics
We obtained service members' demographic information (sex, age, race/ethnicity, educational attainment, and marital status) from the Defense Manpower Data Center (Seaside, CA). Civilian demographic information was assessed during the NHANES household interview.
Cardiovascular Health
We examined 2 CVH behaviors (current smoking status and BMI) and 2 CVH factors (SBP and DBP and diabetes mellitus [presence or absence]).10 Each CVH metric was classified as ideal, intermediate, or poor using the closest possible consistency with AHA criteria when possible, modified when necessary. Army data as of 2012 were insufficient to assess the remaining 3 metrics: diet score, physical activity, and total blood cholesterol.
Smoking
Service members were asked “do you smoke any kind of tobacco products?” and categorized as ideal (if no) or poor (if yes). NHANES youth (aged <20 years) were asked “on how many of the past 30 days did you smoke a cigarette?” and categorized as ideal (if 0) or poor (if ≥1). NHANES adults were asked “do you now smoke cigarettes…?” and categorized as ideal (if not at all) or poor (if every day or some days).
Body Mass Index
BMI (weight [kg]/height2 [m2]), calculated from clinical examination data for both Army personnel and civilians, was classified as either ideal (<25 kg/m2), intermediate (25–29.9 kg/m2), or poor (≥30 kg/m2). Service member BMI was pulled from the Military Health System Data Repository or the Digital Training Management System when necessary to reconcile missing or out of range values.
Blood Pressure
SBP and DBP were recorded during clinical examinations in both populations. On the basis of a combination of SBP and DBP, we categorized respondents' BP as ideal (<120/<80 mm Hg), intermediate (SBP, 120–139 mm Hg; or DBP, 80–89 mm Hg), or poor (≥140 or ≥90 mm Hg).
Diabetes Mellitus Status
Service members were asked “do you or have you ever had diabetes (mellitus)?” and categorized as either ideal (if no) or poor (if yes). NHANES participants were asked, “Other than during pregnancy, have you ever been told by a physician or other health professional that you have diabetes (mellitus) or sugar diabetes (mellitus)?” and categorized as ideal (if no, borderline, or prediabetes) or poor (if yes). Although this definition departs importantly from the AHA measure of fasting plasma glucose, it does permit comparison between Army and civilian populations with a relevant indicator of this factor.
Statistical Analysis
We conducted analyses using SAS, version 9.4. We applied the direct method for age standardization using the year 2000 population projections from the US Census Bureau.21 We accounted for weighting in each group with the SAS SURVEYREG procedure and used the Taylor series linearization method (recommended by the National Center for Health Statistics to obtain corrected SEEs and CIs) for the NHANES complex survey design.19, 22 We used weighted χ2 tests to compare demographic characteristics across the 2 study groups (active duty and NHANES). We next calculated age‐standardized prevalence estimates and 95% CIs for each category of the CVH metrics in the overall populations and in sex and race/ethnicity subgroups. In addition, we conducted significance tests of model effects and linear functions of model parameters, contrasting each CVH metric category in the Army with the civilian population both overall and separately in each sex and each race/ethnicity subgroup. Last, we computed age‐standardized prevalence estimates of the number of ideal CVH criteria met in each population and the subgroups. All tests were 2 sided, with an α level of 0.001.
We conducted all analyses within the Person‐Event Data Environment, a secure Army data repository and analysis environment.23, 24 All data meet Health Insurance Portability and Accountability Act of 1996 Limited Data Set standards, in accordance with Federal and Department of Defense regulations governing use of electronic medical records.
Results
The Table presents demographic characteristics of the active duty Army group and NHANES group. We made statistical comparisons across the 2 study groups (active duty and NHANES [civilian]) and found statistically significant differences for each characteristic. We describe key weight‐adjusted differences below.
Table 1.
Demographic Characteristics of US Army and NHANES Groups, 2011 to 2012
| Characteristic | Active Duty Sample (n=263 430) | Active Duty Estimated Population (n=497 490)a | NHANES Sample (n=4797) | NHANES Estimated Population (N=198 146)b |
|---|---|---|---|---|
| Age group, yc | ||||
| 17–29 | 149 166 (56.63) | 315 669 (63.45) | 1410 (30.00) | 52 340 (27.02) |
| 30–39 | 77 612 (29.46) | 122 860 (24.70) | 940 (20.00) | 38 244 (19.74) |
| 40–49 | 33 269 (12.63) | 52 812 (10.62) | 896 (19.06) | 42 017 (21.69) |
| 50–64 | 3366 (1.28) | 6148 (1.24) | 1454 (30.94) | 61 125 (31.55) |
| Sexc | ||||
| Men | 224 761 (85.32) | 442 358 (88.92) | 2403 (50.09) | 98 467 (49.69) |
| Women | 38 669 (14.68) | 55 132 (11.08) | 2394 (49.91) | 99 679 (50.31) |
| Race/ethnicityc | ||||
| Hispanic | 28 223 (10.71) | 44 107 (8.87) | 1051 (21.91) | 31 400 (15.85) |
| Non‐Hispanic white | 156 840 (59.54) | 307 886 (61.89) | 1548 (32.27) | 126 255 (63.72) |
| Non‐Hispanic black | 57 397 (21.79) | 125 298 (25.19) | 1313 (27.37) | 24 288 (12.26) |
| Other | 20 970 (7.96) | 20 199 (4.06) | 885 (18.45) | 16 203 (8.18) |
| Educationc | ||||
| No HS diploma | 1266 (0.48) | 2635 (0.53) | 1153 (24.04) | 34 202 (17.26) |
| HS diploma or equivalent | 193 703 (74.06) | 408 204 (82.42) | 1005 (20.95) | 39 371 (19.87) |
| Some college | 11 861 (4.53) | 19 273 (3.89) | 1464 (30.52) | 64 269 (32.44) |
| College degree or greater | 54 724 (20.92) | 65 188 (13.16) | 1175 (24.49) | 60 304 (30.43) |
| Marital statusc | ||||
| Married | 158 022 (60.03) | 285 554 (57.40) | 2474 (56.93) | 114 308 (61.35) |
| Never married | 88 999 (33.81) | 184 157 (37.02) | 1121 (25.79) | 42 943 (23.04) |
| Separated/divorced/widowed | 16 225 (6.16) | 27 729 (5.57) | 751 (17.28) | 29 071 (15.60) |
| Length of service, y | ||||
| 0–3 | 89 444 (33.95) | 203 286 (40.86) | N/A | N/A |
| 4–8 | 64 203 (24.37) | 116 241 (23.37) | N/A | N/A |
| 9–15 | 57 089 (21.67) | 92 908 (18.68) | N/A | N/A |
| ≥16 | 52 694 (20.00) | 85 055 (17.10) | N/A | N/A |
Data are given as number (percentage) of each group. HS indicates high school; N/A, not applicable; NHANES, National Health and Nutrition Examination Survey.
Data are weighted for 2012 Periodic Health Assessment availability.
Data are weighted for survey selection and nonresponse and are presented in thousands. Weighted population counts are presented for descriptive purposes. Percentages may not add up to 100% because of rounding. Furthermore, subgroup totals may be less than the corresponding group total because of missing data.
P<0.001.
Among active duty service members, the youngest age category (17–29 years) heavily predominated in frequency (63%), whereas the NHANES population had only 27% in this category. The active duty Army group had few members in the 50 to 64 years category, whereas nearly one third of NHANES participants were in this age range (1% versus 32%). The active duty Army group, but not the NHANES group, was predominantly men. Categories of race/ethnicity were similarly distributed across the 2 groups, except for Hispanics, who were oversampled in NHANES. Fewer Army personnel than NHANES participants (17% versus 63%) had more than a high school diploma or equivalent. Army personnel were more likely to have never married than NHANES participants (37% versus 23%) and less likely to be separated, widowed, or divorced (6% versus 16%). Among active duty Army personnel, 36% reported >8 years of service and 17% reported >15 years of service.
Prevalence of CVH Metrics Categories
We present the prevalence estimates and 95% CIs (indicating the precision of each estimate) for each CVH metric comparison between active duty service members and, separately, the NHANES group. Active duty service members had slightly more frequent ideal status for smoking and diabetes mellitus and substantially greater frequencies of intermediate levels of BMI and BP than the NHANES group (Figure 1). In addition, although ideal BMI was fairly comparable across active duty service members and the NHANES group, ideal BP was substantially less prevalent among active duty Army personnel than among NHANES participants. In addition, although the age‐adjusted prevalence of smoking was fairly comparable in both populations (≈20%), we observed an unadjusted smoking prevalence among active duty personnel 17 to 29 years old of ≈30%, relative to just 23% among those 30 to 39 years old.
Figure 1.
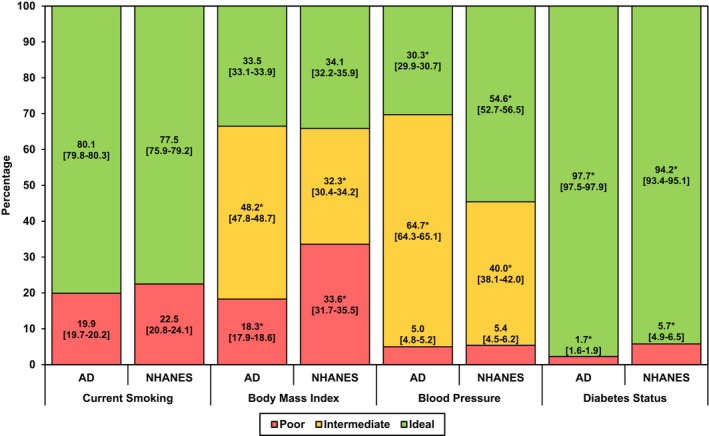
Age‐standardized prevalence estimates (95% CIs) of ideal, intermediate, and poor health, for the 4 metrics of cardiovascular health (CVH) among active duty service members (AD) and the National Health and Nutrition Examination Survey (NHANES) group. *Indicates significant differences in each CVH category between AD and NHANES groups (P<0.001).
Prevalence of CVH Metrics by Sex and by Race/Ethnicity
For both male and female active duty personnel, ideal smoking and diabetes mellitus status were more frequent than among the NHANES group (Figure 2A and 2B). Ideal BMI was equally frequent among active duty and NHANES men, and ideal BP was notably less frequent among active duty men compared with NHANES men (Figure 2A). Ideal BMI was more frequent, and ideal BP was less frequent, among female active duty personnel compared with NHANES women (Figure 2B).
Figure 2.
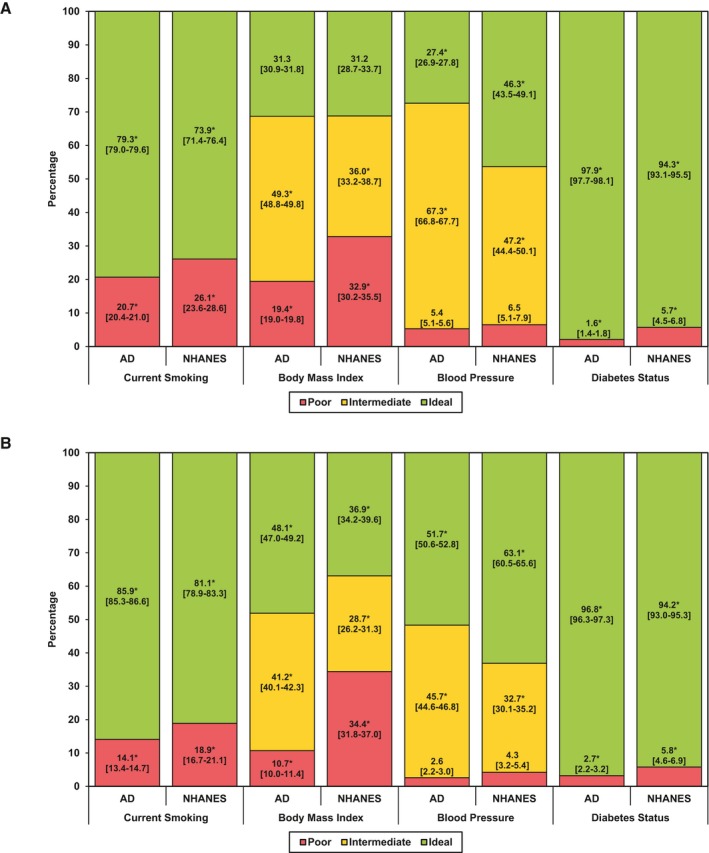
Age‐standardized prevalence estimates (95% CIs) of ideal, intermediate, and poor health, for the 4 metrics of cardiovascular health (CVH) among active duty service members (AD) and the National Health and Nutrition Examination Survey (NHANES) group for men (A) and women (B). *Indicates significant differences in each CVH category between AD and NHANES groups (P<0.001).
For subgroups by race/ethnicity, smoking was less frequent among active duty Hispanics (12.1% [95% CI, 11.1%–13.1%]) and non‐Hispanic blacks (17.1% [95% CI, 16.5%–17.7%]), relative to their NHANES counterparts (17.5% [95% CI, 15.0%–20.0%] and 22.8% [95% CI, 20.2%–25.4%], respectively), whereas we observed only modest differences in smoking rates between active duty and NHANES non‐Hispanic whites (21.8% [95% CI, 21.5%–22.2%] versus 24.1% [95% CI, 21.6%–26.5%]) and active duty and NHANES individuals in the other category (20.5% [95% CI, 19.4%–21.7%] versus 19.8% [95% CI, 15.3%–24.4%]). Ideal BMI was more frequent for Hispanic and non‐Hispanic black active duty personnel compared with NHANES participants, yet ideal BMI was less frequent among active duty personnel in the other category, compared with the NHANES group (Figure 3A). In addition, ideal BP status was lower among active duty personnel relative to NHANES participants across every race/ethnicity subgroup (Figure 3B). Compared with the NHANES group, diabetes mellitus was less frequent among active duty Hispanics (2.8% [95% CI, 1.8%–3.8%] versus 8.4% [95% CI, 6.7%–10.2%]), non‐Hispanic whites (1.2% [95% CI, 1.0%–1.4%] versus 4.4% [95% CI, 3.4%–5.5%]), non‐Hispanic blacks (2.8% [95% CI, 2.4%–3.3%] versus 9.3% [95% CI, 7.7%–10.9%]), and, to a lesser degree, individuals in the other category (2.9% [95% CI, 1.9%–3.9%] versus 6.8% [95% CI, 4.3%–9.2%]). For Hispanics, CVH metrics were generally more favorable than for other groups, both active duty and civilian, except BMI (Figure 3A and 3B).
Figure 3.
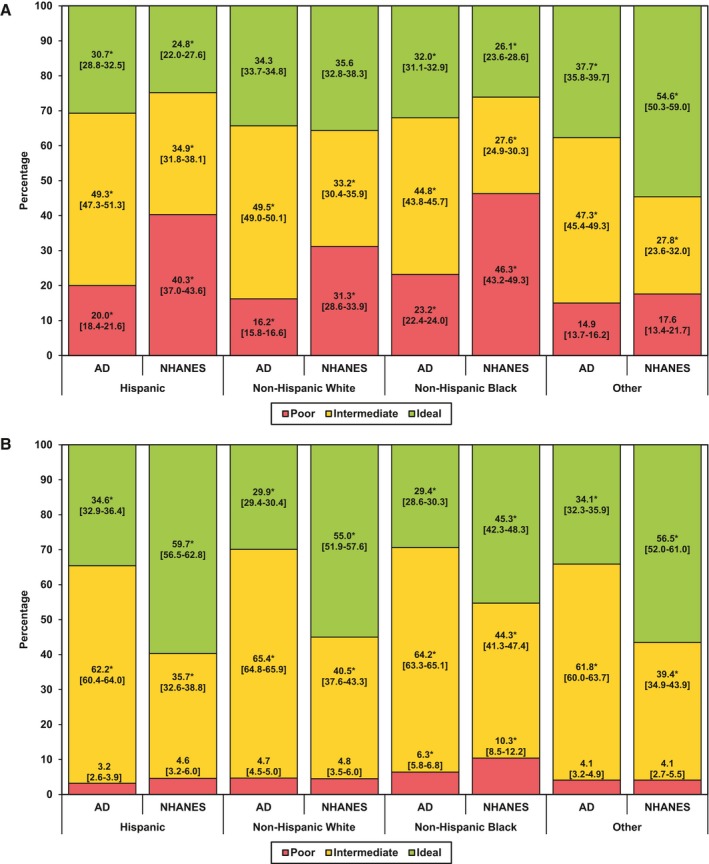
Age‐standardized prevalence estimates (95% CIs) of ideal, intermediate, and poor health, for body mass index (A) and blood pressure (B), among active duty service members (AD) and the National Health and Nutrition Examination Survey (NHANES) group, by race/ethnicity. *Indicates significant differences in each cardiovascular health category between AD and NHANES groups (P<0.001).
Number of Ideal CVH Criteria Met
Overall, a smaller proportion of active duty personnel than NHANES participants met ideal criteria on ≥3 CVH metrics (Figure 4A). (Note: Frequency distributions shifted toward the left are less favorable, whereas those shifted toward the right are more favorable.) The same was generally true for men (Figure 4B, left); however, among women, we observed similar distributions between active duty Army and NHANES groups (Figure 4B, right). As with the overall comparison, we observed a smaller proportion of active duty personnel than NHANES participants who met ideal criteria on ≥3 CVH metrics within subgroups by race/ethnicity (although the difference among non‐Hispanic blacks was minimal; Figure 5). Notably, we also observed this pattern at each age level: higher proportions of active duty Army with only 1 to 2 ideal metrics and lower proportions with 3 to 4 ideal metrics than among NHANES participants (Figure 6A through 6D).
Figure 4.
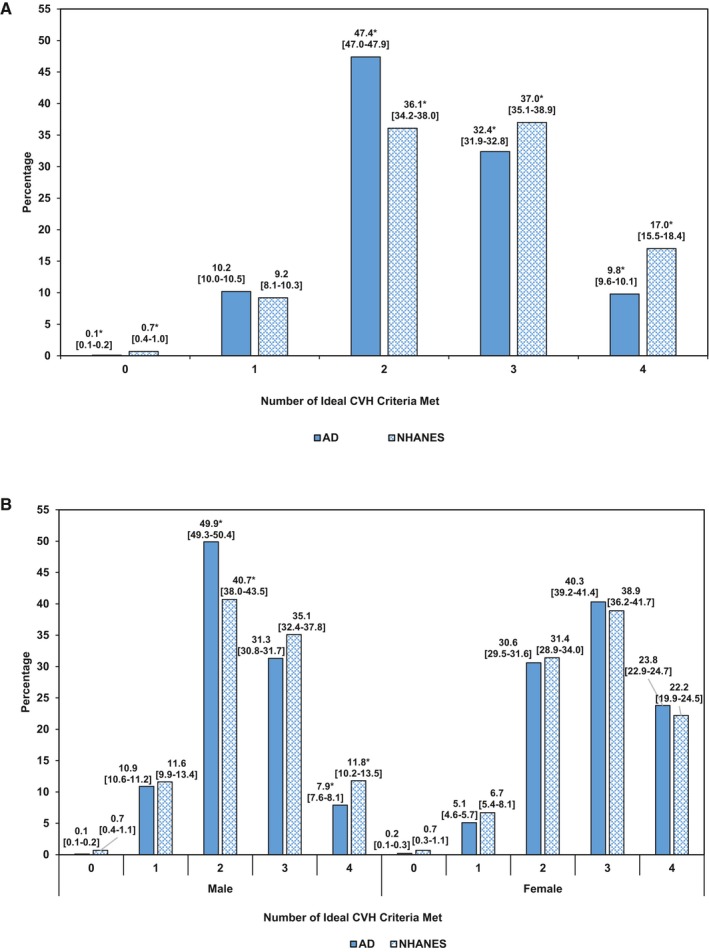
Age‐standardized prevalence estimates (95% CIs) of number of ideal cardiovascular health (CVH) criteria met among active duty service members (AD) and the National Health and Nutrition Examination Survey (NHANES) group, overall (A) and by sex (B). *Indicates significant differences in each CVH category between AD and NHANES groups (P<0.001).
Figure 5.
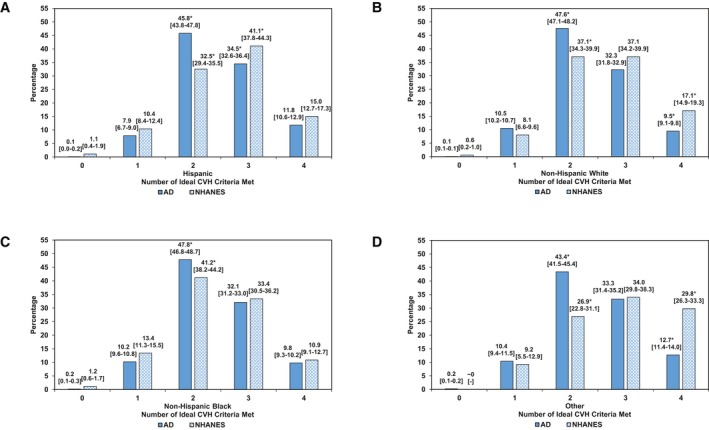
Age‐standardized prevalence estimates (95% CIs) of number of ideal cardiovascular health (CVH) criteria met among active duty service members (AD) and the National Health and Nutrition Examination Survey (NHANES) group, by race/ethnicity. *Indicates significant differences in each CVH category between AD and NHANES groups (P<0.001).
Figure 6.
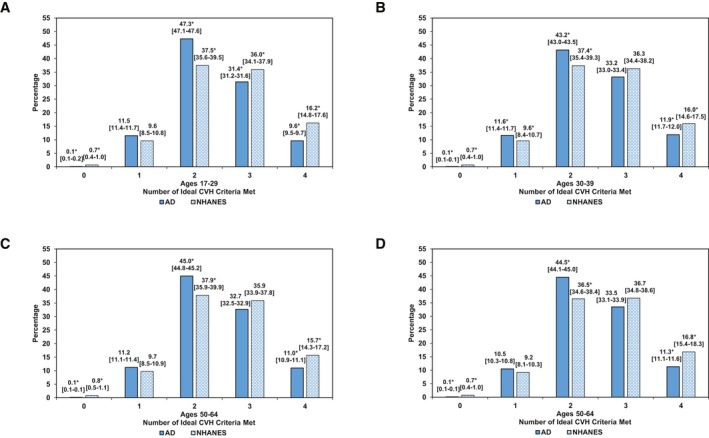
Age‐standardized prevalence estimates (95% CIs) of number of ideal cardiovascular health (CVH) criteria met among active duty service members (AD) and the National Health and Nutrition Examination Survey (NHANES) group, by age subgroup. *Indicates significant differences in each CVH category between AD and NHANES groups (P<0.001).
Discussion
Active duty Army personnel exhibited fewer favorable CVH metrics (classified as ideal versus intermediate or poor) than did NHANES participants, overall and within most sex, race/ethnicity, and age subgroups.
This is the first study of CVH, as defined by the AHA, in Army personnel and compared with a US civilian population. Considering the Army's selective screening and policy of maintaining good physical and psychological health of Army personnel, we hypothesized that CVH metrics would be more favorable in the Army than the civilian population, at all ages. Contrary to our hypothesis, however, we observed less ideal CVH in the Army relative to the NHANES group.
Demographics and Overall CVH
The estimated Army population of nearly 500 000 active duty individuals differed from the estimated NHANES population demographically in several key respects: younger; predominantly men; fewer Hispanics and more non‐Hispanic blacks; and less post–high school education. We were unable to compare the populations in terms of other measures of social disadvantage, which may be presumed to be more prevalent among Army recruits, a potential topic for further investigation. More than 55 000 women, 44 000 Hispanics, and 125 000 non‐Hispanic blacks are included in the estimated Army active duty population, and we estimated >85 000 individuals with >15 years of service longevity. Active duty Army personnel exhibited fewer favorable CVH metrics versus intermediate or poor than did the NHANES participants, overall and within most sex, race/ethnicity, and age subgroups.
In separate analyses comparing Reserve and National Guard personnel with NHANES civilians, we found that aside from having less ideal BMI than NHANES civilians, the differences in CVH observed between active duty personnel and NHANES civilians in this study appear to extend to Reserve and National Guard personnel (data not shown). Future research should further examine differences between Army components and US civilians and examine whether factors, such as deployment history, are associated with differences in CVH between Army components.
Cigarette Use
Both active duty personnel and NHANES civilians exhibited current smoking rates of nearly 20%, with the exception of female and Hispanic service members (<15%). Studies of smoking behaviors among military personnel typically find either an elevated smoking prevalence8, 17 or no difference when compared with civilian populations.25 In addition, the greater unadjusted smoking prevalence found among younger active duty personnel in this and other studies is particularly problematic given 17 to 29 year old service members (the age group with the greatest smoking prevalence) represent nearly two thirds of the active duty population.25, 26, 27 Many young service members report initiating smoking after joining the Army,25, 26 and this could, in part, be because of substantially lower cigarette prices in military compared with civilian stores.28, 29 Targeted Army interventions and population‐based prevention strategies are needed to reduce the healthcare burden and economic impact of smoking behaviors, particularly among young service members.9, 30, 31, 32, 33, 34
Overweight and Obesity
This major public health problem afflicts the Army as well as civilians.35 Overall, only one third of active duty service members and civilians, but nearly half of female active duty personnel, demonstrated ideal BMI. This finding represents an opportunity to preserve ideal BMI for one segment of the active duty population, particularly given the increases in prevalence (unadjusted) of the poor category through the age of 49 years (data not shown). Poor BMI was nearly twice as prevalent in civilians as in active duty personnel, suggesting selection against obesity in Army recruitment may account for an early relative advantage, but the effect is not sustained at older ages.36 Army training standards and demanding physical requirements may, in part, limit BMI increases in Army personnel, but not sufficiently to offset counterinfluences. In addition, as service members age and attain higher ranks, they typically move into staff positions, which tend to be more sedentary than in “line” positions within units (eg, infantry). Study of measurement, determinants, and preventive strategies for excessive BMI in the Army is warranted.37, 38, 39
Blood Pressure
Ideal BP was strikingly less prevalent among active duty Army personnel than among the NHANES group (30% versus 55%). This was unexpected considering military screening excludes recruits with elevated BP. Nevertheless, this pattern was consistent across race/ethnicity subgroups, although more pronounced among male rather than female active duty service members. Although this contradicts our hypothesis, other studies have also observed a high prevalence of prehypertension and hypertension in military personnel.40 Elevated BP readings may, in part, result from stressful military experiences, such as combat deployments, tobacco and alcohol use, or inconsistent dietary habits resulting from long work hours. Indeed, soldiers reporting multiple combat exposures are 1.33 times more likely to report hypertension compared with others.41 In addition, although NHANES civilians demonstrated a greater prevalence of ideal BP (55%), ample room for improvement remains in both active duty Army and civilians. These findings highlight the need to preserve ideal BP and reverse intermediate and poor BP through targeted intervention programs in both Army and civilian populations.
Diabetes Mellitus
Diabetes mellitus, although slightly less prevalent in active duty Army compared with NHANES, was rare in both populations. This disparity may be caused, in part, by selection against diabetes mellitus at entry to the Army; however, further investigation is needed.36 Consistent with previous research, ideal diabetes mellitus status was less prevalent among non‐Hispanic black and Hispanic individuals and more prevalent among non‐Hispanic white individuals.15, 42 Given diabetes mellitus is associated with a wide range of serious medical conditions (eg, heart disease, stroke, blindness, kidney failure, and coronary microvascular disease),43 prevention and management programs are needed to maintain ideal glucose levels in service members and civilians.
Limitations and Future Directions
This study has several limitations worth noting. First, there may be technical differences in the assessment of CVH metrics between the Army and NHANES groups, especially for BMI (eg, shoes and clothing) and BP (eg, position). Second, we were unable to assess intermediate levels of smoking (ie, former smokers who quit smoking within the past year); we were obliged to substitute self‐reports of diabetes mellitus for fasting plasma glucose; and we were unable to account for medications when classifying BP. Third, lack of Army data on diet, physical activity, and cholesterol (for service members <40 years) limited the current comparison to only 4 of the 7 CVH metrics, precluding calculation of individual CVH scores. Fourth, this study sought to make contemporaneous comparisons between the Army and the US civilian population. Although it is desirable in analysis of NHANES data to combine sequential 2‐year cycles of the survey to increase analytic sample sizes, this practice relies on the assumed absence of secular trends over multiple cycles. This assumption could not be justified in the present case for either study population because of ongoing campaigns attempting to promote the health of service members and, separately, civilians. We, therefore, made the design decision to restrict eligibility to the time period of a single NHANES cycle and, furthermore, recommend caution when interpreting the diabetes mellitus prevalence estimates, which demonstrated low prevalence among Army service members and civilians. Fifth, although we only present prevalence estimates across one dimension at a time (eg, only sex or only race/ethnicity), our samples do contain some groups that may be fairly rare (eg, older, Hispanic, women in the Army), which is reflected in our population weighting. Nonetheless, the current comparisons present an important first step in understanding CVH in the Army relative to the general population.
The present findings can be extended in several important ways. First, because this study compared CVH in Army personnel with that of civilians, we did not examine the role of military‐specific experiences, such as combat exposure, in Army members' CVH. Future research on military samples should examine the role of combat exposure and other military‐specific experiences in Army members' CVH. Second, future research may explore the extent to which the present findings extend to other military service branches (eg, Air Force and Navy). Third, future research may benefit from an economic analysis of the costs associated with treating cardiovascular conditions within the Army (or Department of Defense) compared with civilians, as well as the projected cost savings associated with moving service members from poor to intermediate CVH or from intermediate to ideal CVH. Fourth, an economic analysis of the cost savings resulting from fewer cardiovascular‐related medical visits that can be attributed to large‐scale Army soldier health educational initiatives could be highly informative. One such initiative is Performance Triad, a comprehensive Army health education campaign designed to promote sleep, activity, and nutrition among Army service members and their families.
Conclusions
Overall, ideal CVH in the Army is less prevalent than in the civilian population. This finding is surprising given the Army's selective health screening at entry, as well as the Army's policy commitment to physical and psychological fitness. More important, the low prevalence of ideal BMI and BP in both populations highlights a critical need for impactful efforts to promote, preserve, and improve CVH through both Army‐based and nationwide behavioral and policy changes. Sex‐specific analyses revealed differences in CVH were primarily between active duty Army men and civilian men. Given men represent >80% of the Army, this difference in CVH could have important readiness and cost concerns for the Army. Preventive health interventions aimed at improving the BMI and BP of service members (particularly men) through physical activity and nutrition, for example, may yield substantial gains in CVH for the active duty force. Such efforts have the potential to improve military preparedness, CVH, and quality of life, while at the same time reducing healthcare costs.44
Sources of Funding
Support for this publication is provided by a grant from the Robert Wood Johnson Foundation (grant 68709) awarded to the Positive Psychology Center of the University of Pennsylvania (to M.E.P.S.).
Disclosures
D.R.L. is Co‐Investigator of the American Heart Association Strategically Focused Children's Research Network at the Northwestern University Feinberg School of Medicine.
Acknowledgments
We acknowledge the significant support provided to this project by the men and women of the Office of the Deputy Under Secretary of the Army, the Army Analytics Group, and the Research Facilitation Laboratory. We would also like to thank Dr Douglas Bonett (University of California, Santa Cruz) for statistical guidance and Audrey L. Luken (MEDPROS Program Manager, US Army Medical Command) for providing critical information on the US Army medical data assets. The US Department of Defense (DOD) does not exercise any editorial, security, or other control over the information in this article. The authors assume responsibility for the veracity, accuracy, and source documentation of the material, including no use of classified material and conformity to copyright and use permissions. The views expressed in this article are those of the authors and do not necessarily reflect the official policy of the Department of the Army, DOD, or the US Government.
(J Am Heart Assoc. 2019;8:e009056 DOI: 10.1161/JAHA.118.009056.)
References
- 1. Centers for Disease Control and Prevention . Heart disease facts. http://www.cdc.gov/heartdisease/facts.htm. Accessed August 24, 2017.
- 2. United States Army . Health of the force: create a healthier force for tomorrow. 2015. https://www.army.mil/e2/c/downloads/419337.pdf. Accessed July 26, 2017.
- 3. Daviglus ML, Stamler J, Pirzada A, Yan LL, Garside DB, Liu K, Wang R, Dyer AR, Lloyd‐Jones DM, Greenland P. Favorable cardiovascular risk profile in young women and long‐term risk of cardiovascular and all‐cause mortality. JAMA. 2004;292:1588–1592. [DOI] [PubMed] [Google Scholar]
- 4. Calle EE, Rodriguez C, Walker‐Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. [DOI] [PubMed] [Google Scholar]
- 5. U.S. Department of Health and Human Services . The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 6. Armed Forces Health Surveillance Center (AFHSC) . Incidence and prevalence of select cardiovascular risk factors and conditions, active component, U.S. Armed Forces, 2003–2012. MSMR. 2013;20:16–19. [PubMed] [Google Scholar]
- 7. McGraw LK, Turner BS, Stotts NA, Dracup KA. A review of cardiovascular risk factors in U.S. military personnel. J Cardiovasc Nurs. 2008;23:338–344. [DOI] [PubMed] [Google Scholar]
- 8. Barlas FM, Higgins WB, Pflieger JC, Diecker K. 2011 Department of Defense Health Related Behaviors Survey of Active Duty Military Personnel. Farifax, VA: Department of Defense; 2013. [Google Scholar]
- 9. Dall TM, Zhang Y, Chen YJ, Askarinam Wagner RC, Hogan PF, Fagan NK, Olaiya ST, Tornberg DN. Cost associated with being overweight and with obesity, high alcohol consumption, and tobacco use within the military health system's TRICARE prime‐enrolled population. Am J Health Promot. 2007;22:120–139. [DOI] [PubMed] [Google Scholar]
- 10. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 11. Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ommerborn MJ, Blackshear CT, Hickson DA, Griswold ME, Kwatra J, Djoussé L, Clark CR. Ideal cardiovascular health and incident cardiovascular events: the Jackson Heart Study. Am J Prev Med. 2016;51:502–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks and Hispanics: the Northern Manhattan Study. Circulation. 2012;125:2975–2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all‐cause and CVD mortality among U.S. adults. JAMA. 2012;307:1273–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ford SE, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fryar CD, Herrick K, Afful J, Ogden CL. Cardiovascular disease risk factors among male veterans, U.S., 2009–2012. Am J Prev Med. 2016;50:101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med. 2012;42:473–480. [DOI] [PubMed] [Google Scholar]
- 18. MEDPROS Force Health Protection Documentation Team . Periodic Health Assessment member user guide. http://moncrief.amedd.army.mil/HealthcareServices/Shared%20Documents/PHAMemberUserGuidev7.pdf. Published 2010. Accessed December 25, 2014.
- 19. Mirel LB, Mohadjer LK, Dohrmann SM, Clark J, Burt VL, Johnson CL, Curtin LR. National Health and Nutrition Examination Survey: estimation procedures, 2007–2010. Vital Health Stat 2. 2013;159:1–17. [PubMed] [Google Scholar]
- 20. Johnson CL, Paulose RR, Ogden CL, Carroll MD, Kruszon‐Moran D, Dohrmann SM, Curtin LR. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital Health Stat 2. 2013;161:1–24. [PubMed] [Google Scholar]
- 21. Klein RJ, Schoenborn CA. Age Adjustment Using the 2000 Projected U.S. Population. Healthy People Statistical Notes, No. 20. Hyattsville, MD: National Center for Health Statistics; 2001. [PubMed] [Google Scholar]
- 22. Berglund PA. Analysis of complex sample survey data. Using the SURVEYMEANS and SURVEYREG procedures and macro coding. Statistics and Data Analysis. http://www2.sas.com/proceedings/sugi27/p263-27.pdf. Accessed January 29, 2016.
- 23. Vie LL, Griffith KN, Scheier LM, Lester PB, Seligman MEP. The Person‐Event Data Environment (PDE): leveraging big data for studies of psychological strengths in soldiers. Front Psychol. 2013;4:934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vie LL, Scheier LM, Lester PB, Ho TE, Labarthe DR, Seligman MEP. The U.S. Army Person‐Event Data Environment: a military–civilian big data enterprise. Big Data. 2015;3:67–79. [DOI] [PubMed] [Google Scholar]
- 25. Bray RM, Pemberton M, Hourani LL, Witt M, Olmsted KL, Brown JM, Weimer B, Lance ME, Marsden ME, Scheffler S. Vandermaas‐Peeler R, Vandermaas‐Peeler R, Aspinwall KR, Anderson E, Spagnola K, Close K, Gratton JL, Calvin S, Bradshaw M. 2008 Department of Defense Survey of Health‐Related Behaviors Among Military Personnel. Research Triangle Park, NC: RTI International; 2009. [Google Scholar]
- 26. Cypel YS, Hamlett‐Berry K, Barth SK, Christofferson DE, Davey VJ, Eber S, Schneiderman AL, Bossarte RM. Cigarette smoking and sociodemographic, military, and health characteristics of Operation Enduring Freedom and Operation Iraqi Freedom Veterans: 2009–2011 National Health Study for a New Generation of U.S. Veterans. Public Health Rep. 2016;131:714–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ornelas S, Benne PD, Rosenkranz RR. Tobacco use at Fort Riley: a study of the prevalence of tobacco use among active duty soldiers assigned to Fort Riley, Kansas. Mil Med. 2012;177:780–785. [DOI] [PubMed] [Google Scholar]
- 28. Haddock CK, Jahnke SA, Poston WSC, Williams LN. Cigarette prices in military retail: a review and proposal for advancing military health policy. Mil Med. 2013;178:563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haddock CK, Hyder ML, Poston WSC, Jahnke SA, Williams LN, Lando H. A longitudinal analysis of cigarette prices in military retail outlets. Am J Public Health. 2014;104:e82–e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. U.S. Department of the Army . Army Health Promotion. Army Regulation 600‐63. 2007. (Rapid Action Revision Issue Date: 2010). Available at: https://dmna.ny.gov/r3sp/resources/NGB_and_Army_Guidance/AR_600_63_Army_Health_Promotion.pdf. Accessed October 6, 2016.
- 31. Farrelly MC, Pechacek TF, Thomas KY, Nelson D. The impact of tobacco control programs on adult smoking. Am J Public Health. 2008;98:304–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wakefield MA, Durkin S, Spittal MJ, Siahpush M, Scollo M, Simpson JA, Chapman S, White V, Hill D. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98:1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. National Center for Chronic Disease Prevention and Health Promotion, CDC . Smoking‐attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 34. U.S. Department of Health and Human Services . The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. Printed with corrections, January 2014. [Google Scholar]
- 35. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. U.S. Department of the Army . Standards of medical fitness. Army Regulation 40‐501. 2007. (Rapid Action Revision Issue Date: 2011). Available at: https://www.qmo.amedd.army.mil/diabetes/AR40_5012011.pdf. Accessed October 3, 2016.
- 37. Tilghmand A. The U.S military has a huge problem with obesity and it's only getting worse. Military Times https://www.militarytimes.com/news/your-military/2016/09/11/the-u-s-military-has-a-huge-problem-with-obesity-and-it-s-only-getting-worse/. Published September 11, 2016. Accessed August 3, 2017.
- 38. Eilerman PA, Herzog CM, Luce BK, Chao SY, Walker SM, Zarzabal LA, Carnahan DH. A comparison of obesity prevalence: military health system and United States populations, 2009–2012. Mil Med. 2014;179:462–470. [DOI] [PubMed] [Google Scholar]
- 39. Rona RJ, Sundin J, Wood P, Fear NT. Agreement between body mass index, waist circumference and skin‐fold thickness in the United Kingdom Army. Ann Hum Biol. 2011;38:257–264. [DOI] [PubMed] [Google Scholar]
- 40. Smoley BA, Smith NL, Runkle GP. Hypertension in a population of active duty service members. J Am Board Fam Med. 2008;21:504–511. [DOI] [PubMed] [Google Scholar]
- 41. Granado NS, Smith TC, Swanson GM, Harris RB, Shahar E, Smith B, Boyko EJ, Wells TS, Ryan MA; Millennium Cohort Study Team . Newly reported hypertension after military combat deployment in a large population‐based study. Hypertension. 2009;54:966–973. [DOI] [PubMed] [Google Scholar]
- 42. U.S. Department of Health and Human Services . Diabetes Report Card 2014. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 43. Geiss LS, Wang J, Cheng YJ, Thompson TJ, Barker L, Li Y, Albright AL, Gregg EW. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312:1218–1226. [DOI] [PubMed] [Google Scholar]
- 44. Labarthe DR, Kubzansky LD, Boehm JK, Lloyd‐Jones DM, Berry JD, Seligman ME. Positive cardiovascular health: a timely convergence. J Am Coll Cardiol. 2016;68:860–867. [DOI] [PubMed] [Google Scholar]


