Abstract
INTRODUCTION
Global initiatives to improve breastfeeding practices have focused on the Ten Steps to Successful Breastfeeding. The aim of this study was to assess the effect of implementing Baby-Friendly Hospital Initiative (BFHI) steps 1–9 and BFHI steps 1–10 on incidence of diarrhea and respiratory illnesses in the first 6 months of life.
METHODS
We reanalyzed a cluster randomized trial in which health-care clinics in Kinshasa, Democratic Republic of Congo, were randomly assigned to standard care (control group), BFHI steps 1–9, or BFHI steps 1–10. Outcomes included episodes of diarrhea and respiratory illness. Piecewise Poisson regression with generalized estimation equations to account for clustering by clinic was used to estimate incidence rate ratios (IRR) and 95% confidence intervals (CI).
RESULTS
Steps 1–9 was associated with a decreased incidence of reported diarrhea (IRR 0.72, 95%CI: 0.53, 0.99) and respiratory illness (IRR 0.48, 95% CI: 0.37, 0.63), health facility visits due to diarrhea (IRR 0.60, 95%CI: 0.42, 0.85) and respiratory illness (IRR 0.47, 95% CI 0.36, 0.63), and hospitalizations due to diarrhea (IRR 0.42, 95%CI: 0.17, 1.06) and respiratory illness (IRR 0.33, 95% CI 0.11, 0.98). Addition of Step 10 attenuated this effect: episodes of reported diarrhea (IRR 1.24, 95% CI 0.93, 1.68) and respiratory illness (IRR 0.77, 95% CI: 0.60, 0.99), health facility visits due to diarrhea (IRR 0.76, 95% CI: 0.54, 1.08) and respiratory illness (IRR 0.75 95% CI: 0.57, 0.97), and hospitalizations due to respiratory illness (IRR 0.48 95% CI: 0.16, 1.40); but strengthened the effect against hospitalizations due to diarrhea (IRR 0.14, 95% CI: 0.03, 0.60).
CONCLUSIONS
Implementation of steps 1–9 significantly reduced incidence of mild and severe episodes of diarrhea and respiratory infection in the first 6 months of life, addition of step 10 appeared to lessen this effect.
Trial registration:
Keywords: diarrhea, respiratory illness, infants, breastfeeding, Baby-Friendly Hospital Initiative (BFHI)
INTRODUCTION
Between 1990 and 2015, the global annual mortality in children younger than 5 years has fallen substantially, from more than 12 million to 5.9 million (You et al., 2015), but progress has been inconsistent between countries. In 2015, the risk of a child dying before five years of age in sub-Saharan Africa, was more than 11 times that of a child in high income countries (You et al., 2015). Diarrhea, along with pneumonia, are the leading infectious causes of childhood morbidity and mortality (Walker et al., 2013). Each year, an estimated 1.3 million children die from pneumonia and 700 000 from diarrhea (Bhutta et al., 2013). Most of those deaths occurred among younger age groups (Das, Salam, & Bhutta, 2014). Pneumonia and diarrhea remain largely preventable diseases and causes of death. If current evidence-based interventions could be scaled up optimally, 95% of diarrhea and 67% of pneumonia deaths could be prevented (Bhutta et al., 2013).
Practicing optimal breastfeeding, including initiation of skin-to-skin contact with breastfeeding within 1 hour of birth, exclusive breastfeeding (EBF) with no additional fluid or food for 6 months, and complementing breastfeeding with age appropriate food after 6 months and continuation of breastfeeding until 24 months and beyond (Kramer & Kakuma, 2012), is the most cost-effective intervention to prevent under five mortality (Victora et al., 2016). Yet, in low-income countries in sub-Saharan Africa where the burden of under-five mortality is highest, just over a third of 0 – 5 month old infants are exclusively breastfed, despite near universal breastfeeding initiation (Victora et al., 2016).
The Democratic Republic of Congo (DRC) is a typical example of this mismatch. With an under-five mortality rate of 98 for every 1000 live births, DRC bears the third largest burden of child deaths worldwide, after Nigeria and India (You et al., 2015). In the DRC, 116 out of every 1000 live newborns in 2010 who survived through the first 28 days, subsequently died before their fifth birthday, with an estimated 20 due to diarrhea and 23 due to pneumonia (Liu et al., 2012). Though nine out of ten children in DRC are still being breastfed at one year of age, poor exclusivity of breastfeeding is a major problem. National surveys show that, only 69% of babies aged 0 – 1 month and 35% of those aged 2 – 3 months (about 10 – 14 weeks) were exclusively breastfed (Ministere du Plan, Institut National de la Statistique, & UNICEF, 2010).
Following the Innocenti conference in 1989, global initiatives to improve breastfeeding practices have focused on maternity-level policies and practices known as the Ten Steps to Successful Breastfeeding (WHO/UNICEF, 1989), which are the basis for the Baby-Friendly Hospital Initiative (BFHI) (UNCEF). In a recent cluster randomized controlled trial in Kinshasa, the capital city of DRC, we showed that implementation of steps 1–9 of the Ten Steps to Successful Breastfeeding (the key component of the BFHI), more than triples the prevalence of EBF at six months, and statistically reduces the prevalence of diarrhea by about half, but reduction in respiratory infections was not statistically significant (Yotebieng et al., 2015). As per the study protocol, only data from week 14 and 24 were analyzed, despite infection incidence data collected every month after week 6. In this analysis, we used all available data to assess the effect of the implementation of BFHI steps 1–9 and BFHI steps 1–10 on incidence of diarrhea and respiratory infections.
METHODS
Study design and participants
Data came from a cluster randomized control trial of breastfeeding promotion in Kinshasa, DRC (trial registration: NCT01428232). Details of the design and primary outcomes have been reported elsewhere (P. Hoddinott, 2016; Yotebieng, Chalachala, Labbok, & Behets, 2013; Yotebieng et al., 2015). Briefly, six health facilities were randomized to either standard of care (control), BFHI steps 1–9 (steps 1–9), or BFHI steps 1–9 with additional support provided in well-child clinics (steps 1–10). In facilities randomized to both steps 1–9 and steps 1–10, health-care staff from antenatal and maternity care (i.e. delivery rooms and post-partum wards) were trained using the WHO/UNICEF materials (Box 1). In facilities randomized to steps 1–10, staff additionally distributed flyers in the post-partum ward to women and families. Flyers contained culturally appropriate messages developed to address the keys behaviors that were identified as main contributors to the sub-optimal breastfeeding practices in the pretrial survey (Yotebieng et al., 2013). Between May 24 and August 25, 2012, all women who had a healthy singleton birth in each of the six health facilities were enrolled if they intended to attend well-baby clinic visits and consented to be part of the study. Participants were followed through 24 weeks after enrollment.
Box 1: Ten Steps to Successful Breastfeeding as basis for the Baby-Friendly Hospital Initiative.
| Step | |
|---|---|
| 1 | Having a written breastfeeding policy that is routinely communicated to health-care staff |
| 2 | Training all health-care staff in skulls necessary to implement this policy |
| 3 | Informing all pregnant women about the benefits and management of breastfeeding |
| 4 | Helping mothers to initiate breastfeeding within 30 minutes of birth |
| 5 | Showing mothers how to breastfeed and maintain lactation even if separated from their infants |
| 6 | Giving newborn infants no food or drink other than breastmilk, unless medically indicated, and not accepting free/low-cost breastmilk substitutes, feeding bottles, or teats |
| 7 | Allowing mothers and infants to remain together 24 hours per day |
| 8 | Encouraging breastfeeding on demand |
| 9 | Giving no artificial teats or pacifiers to breastfeeding infants |
| 10 | Fostering the establishment of breastfeeding support groups and referring mothers to them on discharge from hospital or clinic |
SIGNIFICANCE
Global initiatives to improve breastfeeding practices have focused on the Ten Steps to Successful Breastfeeding. However, the need for additional resources to set up and run community support groups has been a major barrier for scale-up in resource-poor settings. Our findings suggest that Baby-Friendly Hospital Initiative (BFHI) steps 1–9 significantly reduces incidence of mixed feeding through 24 weeks of age and consequently the incidence of diarrhea and respiratory illness episodes of various severity. Addition of step 10 appeared to lessen the protective effect. Together with previous research, there is need for a revised WHO and UNICEF BFHI policy.
Measures
Information on outcomes and other key variables were collected through face-to-face interviews at enrollment (in the post-partum ward 2–3 days after birth), 1 week (during the post-partum clinic visit), 6, 10, 14, 18, and 24 weeks (during well-child visits) following delivery. At each interview, exclusive breastfeeding, defined as breast feeding with no other foods or liquids, was assessed. Starting at 6 weeks, women were asked whether their infant had experienced any diarrhea or respiratory illness (defined as fever and cough) since the previous interview. For infants with reported diarrhea or respiratory illness, women were asked if they sought advice or treatment for their infant’s illness at a health center, and whether their child was hospitalized for the illness.
The primary outcomes of this analysis are: 1) episodes of a) diarrhea, b) respiratory illness; 2) health facility visits attributable to a) diarrhea, b) respiratory illness; and 3) hospitalizations attributable to a) diarrhea, b) respiratory illness. All outcomes were self-reported at interviews. Health facility visits were defined as an infant having the defined illness and their mother reporting taking them to a health center for treatment. Hospitalization was defined as having the illness and being hospitalized for that illness.
Baseline (at delivery) socio-demographic characteristics considered for adjustment in the analyses include: woman’s age in years (continuous), dichotomized education level (primary or less/secondary or higher), dichotomized marital status (married/live-in boyfriend, never married/separated/divorced), dichotomized parity (primipara/multipara), previous child death (yes/no), whether the woman wanted the child at its conception and if not, whether she wanted no more children or wanted a child at a later time (yes, later, no more children), number of antenatal care visits (<4/≥4), and quintiles of socioeconomic status (SES). To determine SES quintiles, principal component analysis (PCA) was used. To determine the SES measure, the average number of household members per room (indication of crowding), number of beds in household, household water source (communal or private pipe), cooking fuel type (electric stove or wood/charcoal), and ownership of durable assets (radio, refrigerator, mobile phone, television) were included in the PCA model. The first component explained 21.2% of the variability in the data. Due to similarities, the top two and bottom two quintiles were merged (1st or 2nd quintile/ 3rd quintile/4th or 5th quintile).
Statistical Analysis
Simple piecewise Poisson regression models were used to estimate the effect of each intervention. To account for potential clustering at the clinic level, generalized estimation equations were used. For each follow-up interval time (time between the previous and the current interview), person-weeks were allotted as follow: half of the interval length for participants with a reported episode of an outcome of interest or who were lost-to-follow-up (LTFU), and the full length of the interval for the rest of participants. Baseline characteristics statistically associated with any of the outcomes considered were included in a multivariate piecewise Poisson regression model. All analyses were performed using SAS 9.4 (SAS Institute, Cary, North Carolina). The study design and implementation were approved by University of North Carolina IRB and the Kinshasa school of Public Health ethical committee and the analysis was approved by Ohio State University IRB.
RESULTS
Population characteristics
Overall, 931 of the 975 mother-infant pairs included in the original sample had at least one follow-up visit at or after week six, and were included in this analysis. The baseline characteristic distributions were similar to the distributions reported for the entire sample (Yotebieng et al., 2015). Women in the control group were on average older and more likely to have attended at least four antenatal visits compared to women in the two intervention groups (Table 1). At one week postpartum, the prevalence of EBF in the steps 1–10 group, the steps 1–9 group, and the control group was 96%, 93%, and 68%, respectively. At week six, the proportion remained relatively unchanged in step 1–9 group (90%), but dropped to 81% in the steps 1–10 group and 51% in the control group. The prevalence of EBF in the step 1–10 group continued to drop at an accelerated pace through 18–24 weeks (Figure 1).
Table 1.
Maternal characteristics at enrollment of the 931 mother-infant pairs, by intervention group
| Overall |
Control |
Steps 1–9 |
Steps 1–10 |
|
|---|---|---|---|---|
| Number (%) | Number (%) | Number (%) | Number (%) | |
| Total | 931 | 297 | 344 | 290 |
| Age in years: median (IQR) | 27 (23, 32) | 28 (24, 33) | 26 (23, 31) | 26 (21, 31) |
| Missing | 22 | 11 | 4 | 7 |
| Maternal education | ||||
| Primary or less | 631 (68.4) | 180 (61.4) | 249 (72.6) | 202 (70.4) |
| Secondary or higher | 292 (31.6) | 113 (38.6) | 94 (27.4) | 85 (29.6) |
| Missing | 8 | 4 | 1 | 3 |
| Marital status | ||||
| Married/live-in boyfriend | 803 (87.0) | 264 (89.8) | 303 (88.3) | 236 (82.5) |
| Never married/separated/divorced | 120 (13.0) | 30 (10.2) | 40 (11.7) | 50 (17.5) |
| Missing | 8 | 3 | 1 | 4 |
| Socio-economic status quintile | ||||
| Fifth / fourth | 363 (39.7) | 106 (36.7) | 117 (34.4) | 140 (48.9) |
| Third | 185 (20.2) | 51 (17.6) | 72 (21.2) | 62 (21.7) |
| Second / first | 367 (40.1) | 132 (45.7) | 151 (44.4) | 84 (29.4) |
| Missing | 16 | 8 | 4 | 4 |
| Parity | ||||
| Primipara | 225 (24.3) | 77 (26.1) | 72 (21.0) | 76 (26.5) |
| Multipara | 700 (75.7) | 218 (73.9) | 271 (79.0) | 211 (73.5) |
| Missing | 6 | 2 | 1 | 3 |
| Previous child death | ||||
| Yes | 193 (20.9) | 70 (23.7) | 80 (23.3) | 43 (15.0) |
| No | 732 (79.1) | 225 (76.3) | 263 (76.7) | 244 (85.0) |
| Missing | 6 | 2 | 1 | 3 |
| Wanted child at conception | ||||
| Yes | 416 (45.0) | 146 (49.7) | 174 (50.7) | 96 (33.5) |
| No later | 413 (44.7) | 118 (40.1) | 145 (42.3) | 150 (52.3) |
| No more children | 95 (10.3) | 30 (10.2) | 24 (7.0) | 41 (14.3) |
| Missing | 7 | 3 | 1 | 3 |
| Number of ANC visits | ||||
| <4 | 441 (47.68) | 92 (31.2) | 185 (53.9) | 164 (57.1) |
| ≥4 | 484 (52.3) | 203 (68.8) | 158 (46.1) | 123 (42.9) |
| Missing | 6 | 2 | 1 | 3 |
Abbreviations: IQR = Interquartile range, ANC = Antenatal clinic
Figure 1.
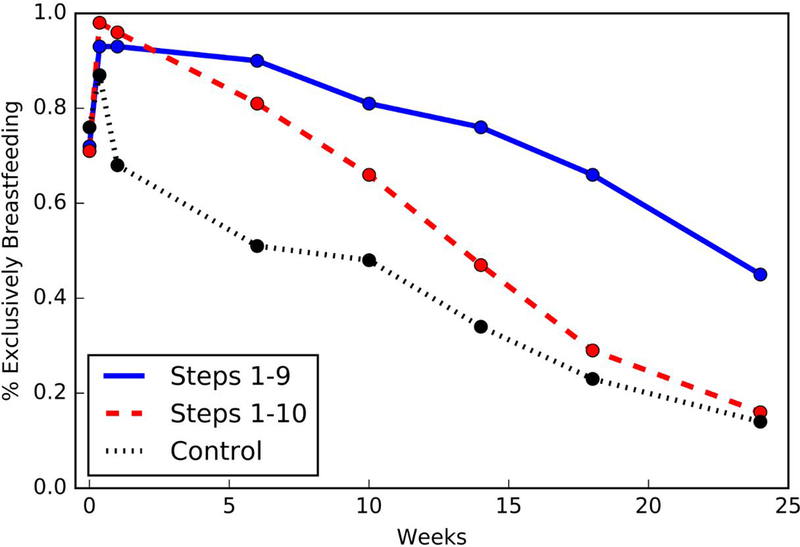
Prevalence of exclusive breastfeeding among mother-infant pairs between 0–24 weeks by clinic randomization. Exclusive breastfeeding was defined as breastfeeding with no additional fluid or food. Exclusive breastfeeding was assessed at 1 hour after birth, 2–3 days after birth, age 1, 6, 10, 14, 18, and 24 weeks. For Baby-Friendly Hospital Initiative (BFHI) steps 1–9, health-care staff from antenatal and maternity care (i.e. delivery rooms and post-partum wards) were trained using the WHO/UNICEF materials. For BHFI steps 1–10, health-care staff were trained using the WHO/UNICEF materials and additionally distributed flyers containing culturally appropriate messages developed to address the keys behaviors that were identified as main contributors to the sub-optimal breastfeeding practices in the pretrial survey to women and their families. Control clinics provided the standard of care.
Incidence of diarrhea, facility care or hospitalization for diarrhea and association with baseline socio-demographic characteristics
During the 18,932 person-weeks of follow-up contributed by the 931 mother-infant pairs for diarrheal illness, 833 episodes of diarrhea were reported (incidence rate (IR) =1.7 episode/100 person-weeks; 95%CI: 1.5, 1.9). Of these episodes, 480 resulted in seeking care for the infant in a health facility (IR=1.0 episode/100 person-weeks; 95%CI: 0.9, 1.2) and 82 in the hospitalization of infant (IR=0.1 episode/100 person-weeks; 95%CI: 0.1, 0.2). Although the incidence rate of diarrhea did not vary by wealth index, infants of women in the lower two quintiles of wealth index were more likely to experience episodes of diarrhea that resulted in hospitalization. The incidence rate of hospitalization among infants of women in the lowest two quintiles of SES was 4.04 (95%CI 1.32, 12.39) times that among infants of women in the highest two quintiles of SES (Table 2).
Table 2.
Episodes of diarrhea, facility care, or hospitalization for diarrhea among 931 infants by their mothers’ sociodemographic characteristics at enrollment
| Diarrhea |
Diarrhea Health facility
care |
Diarrhea
Hospitalization |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Person-weeks | IR (95%CI)* | IRR (95%CI)* | N | Person-weeks | IR (95%CI)* | IRR (95%CI)* | N | Person-weeks | IR (95%CI)* | IRR (95%CI)* | |
| Number | 833 | 18932 | 1.7 (1.5, 1.9) | - | 480 | 19299 | 1.0 (0.9, 1.2) | - | 82 | 19752 | 0.1 (0.1, 0.2) | - |
| Age in years † | 799 | 18510 | 1.5 (1.3, 1.7) | 1.00 (0.98, 1.02) | 453 | 18867 | 0.9 (0.7, 1.0) | 1.00 (0.98, 1.02) | 75 | 19311 | 0.1 (0.1, 0.2) | 0.98 (0.90, 1.06) |
| Maternal education | ||||||||||||
| Primary or less | 570 | 12847 | 1.6 (1.3, 1.8) | - | 338 | 13101 | 0.9 (0.8, 1.1) | - | 70 | 13416 | 0.1 (0.1, 0.2) | - |
| Secondary or Higher | 262 | 5941 | 1.4 (1.1, 1.7) | 0.89 (0.68, 1.15) | 141 | 6054 | 0.8 (0.6, 1.1) | 0.85 (0.62, 1.17) | 12 | 6190 | 0.1 (0.0, 0.2) | 0.42 (0.14, 1.27) |
| Marital status | ||||||||||||
| Never married/separated/divorced | 116 | 2449 | 1.4 (1.0, 2.0) | 0.91 (0.63, 1.31) | 75 | 2486 | 0.9 (0.6, 1.4) | 1.05 (0.71, 1.57) | 17 | 2540 | 0.2 (0.1, 0.4) | 1.65 (0.58, 4.73) |
| Married/live-in boyfriend | 716 | 16339 | 1.4 (1.2, 1.8) | - | 404 | 16669 | 0.9 (0.7, 1.1) | - | 65 | 17066 | 0.1 (0.1, 0.2) | - |
| Socio-economic status quintile | ||||||||||||
| Fifth and Fourth | 3129 | 7410 | 1.5 (1.3, 1.8) | - | 174 | 7544 | 0.9 (0.8, 1.1) | - | 12 | 7718 | 0.1 (0.0, 0.2) | - |
| Third | 184 | 3741 | 1.8 (1.3, 2.3) | 1.27 (0.92, 1.77) | 98 | 3838 | 0.9 (0.7, 1.3) | 1.13 (0.76, 1.68) | 12 | 3937 | 0.1 (0.0, 0.3) | 1.57 (0.32, 7.81) |
| Second and First | 326 | 7470 | 1,5 (1.2, 1.8) | 1.06 (0.81, 1.39) | 206 | 7600 | 1.0 (0.8, 1.2) | 1.18 (0.85, 1.64) | 58 | 7775 | 0.2 (0.1, 0.3) | 4.04 (1.32, 12.39) |
| Parity | ||||||||||||
| Primipara | 237 | 4555 | 1.5 (1.2, 2.0) | 1.01 (0.76, 1.34) | 137 | 4649 | 0.9 (0.7, 1.2) | 1.00 (0.72, 1.39) | 22 | 4748 | 0.1 (0.1, 0.3) | 1.55 (0.60, 4.00) |
| Multipara | 595 | 14277 | 1.5 (1.3, 1.8) | - | 342 | 14550 | 0.9 (0.7, 1.1) | - | 60 | 14902 | 0.1 (0.1, 0.2) | - |
| Previous child death | ||||||||||||
| Yes | 175 | 3945 | 1.6 (1.3, 2.1) | 1.11 (0.83, 1.48) | 111 | 4016 | 1.1 (0.8, 1.5) | 1.25 (0.88, 1.77) | 16 | 4130 | 0.1 (0.0, 0.3) | 1.10 (0.42, 2.87) |
| No | 657 | 14887 | 1.5 (1.3, 1.8) | - | 368 | 15183 | 1.0 (0.8, 1.2) | - | 66 | 15520 | 0.1 (0.1, 0.2) | - |
| Wanted child at conception | ||||||||||||
| Yes | 362 | 8405 | 1.6 (1.3, 1.8) | - | 241 | 8527 | 0.9 (0.6, 1.0) | - | 47 | 8739 | 0.1 (0.1, 0.2) | - |
| No later | 377 | 8483 | 1.5 (1.3, 1.8) | 1.08 (0.84, 1.41) | 192 | 8672 | 0.8 (0.7, 1.0) | 0.85 (0.62, 1.16) | 28 | 8864 | 0.1 (0.1, 0.2) | 0.77 (0.30, 2.00) |
| No more children | 92 | 1925 | 1.8 (1.3, 2.4) | 1.26 (0.87, 1.82) | 46 | 1978 | 0.9 (0.6, 1.4) | 0.97 (0.63, 1.51) | 7 | 2025 | 0.1 (0.0, 0.4) | 1.12 (0.30, 4.22) |
| Number of ANC visits | ||||||||||||
| <4 | 409 | 8977 | 1.5 (1.3, 1.8) | 1.06 (0.83, 1.34) | 225 | 9387 | 0.9 (0.7, 1.1) | 0.94 (0.71, 1.26) | 34 | 9387 | 0.1 (0.1, 0.2) | 0.73 (0.30, 1.75) |
| ≥4 | 423 | 9855 | 1.5 (1.3, 1.7) | - | 254 | 10027 | 0.9 (0.7, 1.1) | - | 48 | 10263 | 0.1 (0.1, 0.2) | - |
IR = Incidence rate; IRR = incidence rate ratio; 95%CI = 95% Confidence interval;
For all 95% CIs, generalized estimating equations were used to account for clustering at the clinic level. IR and IRR were estimated using piecewise Poisson models with intervals between study visits as a categorical time variable.
Incidence rate for median age (27 years old).
Incidence of respiratory infections, facility care or hospitalization for respiratory illness and association with baseline socio-demographic characteristics
During the 18,701 person-weeks of follow-up contributed by the 931 mother-infant pairs for respiratory illness, 989 episodes of respiratory infections were reported (IR=2.1 episode/100 person-weeks; 95%CI: 1.9, 2.4). Of these episodes, 860 resulted in participant seeking care in a health facility (IR=1.9 episode/100 person-weeks; 95%CI: 1.7, 2.1) and 59 in the hospitalization of the infant (IR=0.1 episodes/100 person-weeks; 95%CI: 0.1, 0.2). Infants whose mother had secondary or higher education, or was in the highest two wealth quintile were less likely to have reported respiratory infections and substantially less likely to be hospitalized for respiratory infections (Table 3). Infants of women who reported they wanted their child at a later time were also less likely to experience respiratory infections during follow-up.
Table 3.
Episodes of respiratory infections, facility care or hospitalization for respiratory illness among 931 infants by their mothers’ sociodemographic characteristics at enrollment
| Respiratory |
Respiratory Health facility
care |
Respiratory
Hospitalization |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Time at Risk | IR (95%CI)* | IRR (95%CI)* | N | Time at Risk | IR (95%CI)* | IRR (95%CI)* | N | Time at Risk | IR (95%CI)* | IRR (95%CI)* | |
| Number | 989 | 18701 | 2.1 (1.9, 2.4) | - | 860 | 18843 | 1.9 (1.7, 2.1) | - | 59 | 19766 | 0.1 (0.1, 0.2) | - |
| Age in years † | 961 | 18280 | 1.7 (1.5, 2.0) | 1.01 (0.99, 1.03) | 835 | 18420 | 15 (1.3, 1.8) | 1.01 (0.99, 1.03) | 53 | 19322 | 0.1 (0.0, 0.2) | 1.04 (0.95, 1.14) |
| Maternal education | ||||||||||||
| Primary or less | 709 | 12675 | 1.9 (1.6, 2.1) | - | 623 | 12764 | 1.7 (1.4, 2.0) | - | 55 | 13418 | 0.1 (0.1, 0.2) | |
| Secondary or Higher | 273 | 5888 | 1.6 (1.3, 1.9) | 0.85 (0.67, 1.08) | 230 | 5941 | 1.3 (1.0, 1.6) | 0.78 (0.61, 1.00) | 4 | 6202 | 0.0 (0.0, 0.1) | 0.09 (0.01, 0.65) |
| Marital status | ||||||||||||
| Never married/separated/divorced | 98 | 2432 | 1.5 (1.1, 2.0) | 0.80 (0.58, 1.11) | 86 | 2449 | 1.3 (0.9, 1.8) | 0.79 (0.56, 1.12) | 3 | 2556 | 0.0 (0.0, 0.2) | 0.29 (0.04, 2.15) |
| Married/live-in boyfriend | 886 | 16129 | 1.6 (1.4, 2.0) | - | 769 | 16254 | 1.4 (1.2, 1.7) | - | 56 | 17064 | 0.1 (0.0, 0.2) | - |
| Socio-economic status quintile | ||||||||||||
| Fifth and Fourth | 309 | 7348 | 1.8 (1.6, 2.1) | - | 270 | 7394 | 1.6 (1.4, 1.8) | - | 7 | 7725 | 0.1 (0.0, 0.1) | - |
| Third | 184 | 3686 | 2.1 (1.7, 2.6) | 1.37 (1.04, 1.81) | 211 | 3714 | 1.9 (1.5, 2.4) | 1.38 (1.04, 1.84) | 5 | 3942 | 0.0 (0.0, 0.2) | 1.21 (0.16, 8.99) |
| Second and First | 326 | 7362 | 1.8 (1.5, 2.2) | 1.17 (0.92, 1.51) | 366 | 7430 | 1.5 (1.3, 1.9) | 1.14 (0.88, 1.48) | 47 | 7777 | 0.2 (0.1, 0.3) | 5.56 (1.19, 26.00) |
| Parity | ||||||||||||
| Primipara | 243 | 4503 | 1.8 (1.4, 2.2) | 1.01 (0.79, 1.29) | 223 | 4530 | 1.6 (1.3, 2.0) | 1.05 (0.81, 1.35) | 13 | 4761 | 0.1 (0.0, 0.2) | 0.91 (0.33, 2.54) |
| Multipara | 741 | 14102 | 1.8 (1.5, 2.0) | - | 632 | 14217 | 1.6 (1.3, 1.8) | - | 46 | 14903 | 0.1 (0.1, 0.2) | - |
| Previous child death | ||||||||||||
| Yes | 241 | 3882 | 2.0 (1.6, 2.6) | 1.18 (0.90, 1.54) | 212 | 3913 | 1.8 (1.4, 2.3) | 1.21 (0.91, 1.60) | 22 | 4122 | 0.2 (0.1, 0.4) | 2.72 (1.08, 6.89) |
| No | 743 | 14723 | 1.8 (1.6, 2.2) | - | 643 | 14834 | 1.6 (1.4, 1.9) | - | 37 | 15542 | 0.1 (0.1, 0.2) | - |
| Wanted child at conception | ||||||||||||
| Yes | 506 | 8211 | 1.9 (1.6, 2.2) | - | 448 | 8274 | 1.6 (1.4, 2.0) | - | 32 | 8744 | 0.1 (0.1, 0.2) | - |
| No later | 358 | 8474 | 1.5 (1.2, 1.8) | 0.74 (0.59, 0.93) | 310 | 8530 | 1.3 (1.0, 1.6) | 0.72 (0.57, 0.91) | 18 | 8873 | 0.1 (0.0, 0.1) | 0.64 (0.23, 1.76) |
| No more children | 120 | 1898 | 2.3 (1.6, 3.3) | 1.18 (0.81, 1.70) | 97 | 1921 | 1.9 (1.3, 2.8) | 1.09 (0.73, 1.64) | 9 | 2025 | 0.2 (0.1, 0.6) | 2.06 (0.60, 7.07) |
| Number of ANC visits: median (IQR) | ||||||||||||
| <4 | 456 | 8902 | 1.7 (1.4, 2.0) | 0.92 (0.74, 1.14) | 401 | 8966 | 1.5 (1.2, 1.8) | 0.93 (0.74, 1.16) | 35 | 9384 | 0.1 (0.0, 0.2) | 1.62 (0.63, 4.13) |
| ≥4 | 528 | 9703 | 1.8 (1.5, 2.0) | - | 454 | 9781 | 1.5 (1.3, 1.8) | - | 24 | 10280 | 0.1 (0.1, 0.2) | - |
IR = Incidence rate; IRR = incidence rate ratio; 95%CI = 95% Confidence interval;
For all 95% CIs, generalized estimating equations were used to account for clustering at the clinic level. IR and IRR were estimated using piecewise Poisson models with intervals between study visits as a categorical time variable.
Incidence rate for median age (27 years old).
Effect of implementing steps 1–9, or steps 1–9 plus additional support during well-child visits (steps 1–10 group) on episodes of diarrhea and respiratory infections
The incidence rate of diarrhea was lower among infants randomized to the steps 1–9 group compared to control group (IRR 0.72; 95%CI 0.53, 0.99). Infants in clinics that implemented steps 1–9 experienced fewer episodes of severe diarrhea that led to seeking care at health care facilities (IRR 0.60; 95% 0.42, 0.85) and hospitalization (IRR = 0.42; 95%CI 0.17, 1.06), compared to control clinics. Adjusting for baseline characteristics did not change results substantially (Table 5). Although not statistically significant, the rate of diarrhea was higher among infants who received care in clinics implementing steps 1–10 groups (IRR 1.24; 95%CI 0.93, 1.68), compared to control clinics. However, the steps 1–10 group had a lower rate of episodes of diarrhea that resulted in hospitalization (IRR 0.12; 95%CI 0.03, 0.53).
The rate of any respiratory infections among infants in steps 1–9 group was half that of infants in the control group (IRR 0.48; 95%CI 0.37, 0.63). Steps 1–9 offered similar protection for respiratory infections that resulted in seeking care in a health facility (IRR 0.47; 95% 0.36, 0.63) and protection against severe episodes that resulted in hospitalization (IRR 0.33; 95%CI 0.11, 0.98), compared to controls. Steps 1–10 was also associated with lower rates of respiratory infection, although the effect was weaker (Table 4). Adjustment for baseline socio-demographic characteristics did not change either of the results substantially.
Table 4.
Effect of implementing steps 1–9, or steps 1–9 plus additional support during well-child visits (steps 1–10 group) on episodes of diarrhea and respiratory infections
| Control | Steps 1–9 group | Steps 1–10 group | ||||||
|---|---|---|---|---|---|---|---|---|
| Cases | Person weeks |
Cases | Person weeks |
IRR (95% CI)* | Cases | Person weeks |
IRR (95% CI)* | |
| Diarrhea | ||||||||
| Crude IRR (95%CI) | 275 | 6047 | 253 | 7014 | 0.72 (0.53, 0.99) | 305 | 5871 | 1.24 (0.94, 1.64) |
| Adjusted IRR (95%CI) † | 0.72 (0.52, 0.99) | 1.25 (0.93, 1.68) | ||||||
| Diarrhea & health facility care | ||||||||
| Crude IRR (95%CI) | 189 | 6130 | 189 | 7110 | 0.60 (0.42, 0.85) | 139 | 6059 | 0.76 (0.54, 1.06) |
| Adjusted IRR (95%CI) † | 0.57 (0.40, 0.82) | 0.76 (0.54, 1.08) | ||||||
| Diarrheal hospitalization | ||||||||
| Crude IRR (95%CI) | 52 | 6299 | 26 | 7239 | 0.42 (0.17, 1.06) | 4 | 6214 | 0.12 (0.03, 0.53) |
| Adjusted IRR (95%CI) † | 0.41 (0.15, 1.07) | 0.14 (0.03, 0.60) | ||||||
| Respiratory | ||||||||
| Crude IRR (95%CI) | 443 | 5858 | 257 | 6987 | 0.48 (0.37, 0.63) | 289 | 5856 | 0.77 (0.60, 0.98) |
| Adjusted IRR (95%CI) † | 0.48 (0.36, 0.62) | 0.77 (0.60, 0.99) | ||||||
| Respiratory Health Facility care | ||||||||
| Crude IRR (95%CI) | 388 | 5914 | 228 | 7026 | 0.47 (0.36, 0.63) | 244 | 5903 | 0.75 (0.59, 0.97) |
| Adjusted IRR (95%CI) † | 0.46 (0.35, 0.61) | 0.75 (0.57, 0.97) | ||||||
| Respiratory Hospitalization | ||||||||
| Crude IRR (95%CI) | 42 | 6309 | 8 | 7251 | 0.33 (0.11, 0.98) | 9 | 6206 | 0.39 (0.12, 1.32) |
| Adjusted IRR (95%CI) † | 0.34 (0.12, 1.02) | 0.48 (0.16, 1.40) | ||||||
IRR = incidence rate ratio; 95%CI = 95% Confidence interval;
For all 95% CIs, generalized estimating equations were used to account for clustering at the clinic level. IR and IRR were estimated using piecewise Poisson models with intervals between study visits as a categorical time variable.
Adjusted for socio-economic status, whether the woman wanted a child at its conception, education, and previous child death.
DISCUSSION
In this reanalysis, we used all available data from the original trial to assess a “short cut” implementation of the Ten Steps to Successful Breastfeeding (step 1–9 interventions), on incidence of diarrhea and respiratory illness, and the severity of the episodes. The original analysis was limited to the incidence of diarrhea at 14 and 24 weeks, and though the intervention was found to reduce diarrhea, statistically significance was not achieved for respiratory infections (Yotebieng et al., 2015). Our updated analysis used all available information, showing that implementation BFHI steps 1–9 was highly protective against diarrhea and respiratory illness in the first six months of life. Addition of step 10, in the form of breastfeeding support provided by healthcare workers during well-baby clinic visit and educational materials printed in local languages, attenuated this effect except for severe diarrhea that resulted in hospitalization. For diarrhea cases requiring hospitalization it appeared to strengthen the protective effect compared to steps 1–9.
Optimal breastfeeding is well known to protect against diarrhea or lower respiratory tract infections (Ip et al., 2007). For the past three decades, global initiatives to improve breastfeeding practices have focused on the Ten Steps to Successful Breastfeeding. Recently, BFHI has been revised and updated to address intertwined HIV/AIDS issues (WHO/UNICEF, 2009). However, the need for additional resources to set up and run community support groups (one approach to step 10 in the initiative) has been a major barrier for BFHI’s scale-up in resource-poor settings. In the DRC, the main attempt to implement BFHI steps was headed by UNICEF in the early 2000s as part of a national breastfeeding promotion campaign. Overall, 25 out of more than 6,000 eligible health facilities were certified through this effort, including 13 in Kinshasa. The last hospital certified was in 2004 in the Katanga province before the funding stopped. The DRC simply does not have the means to invest in establishing community support groups. This analysis provides additional evidence that promotion of EBF is a key intervention to accelerate gains in child survival in poor resource settings where infectious diseases and nutritional deficiencies are the dominant causes of mortality among children, like the DRC (Wang et al.). Results from this re-analysis also support the conclusion of the initial analysis that implementation of BFHI steps 1–9 is an effective strategy that is scalable in low resource settings. These results also lend additional support to recent calls to revisit BFHI steps that followed publication of initial results (P. Hoddinott, 2016; Marcel Yotebieng & Frieda Behets, 2016).
The reason why the addition of step 10 attenuates the protective effect of steps 1–9 has been discussed previously (Pat Hoddinott, 2016; Simmer & Patole; M. Yotebieng & F. Behets, 2016). Concerns about breastfeeding that arise in the first weeks after hospital discharge are the strongest predictors of cessation of EBF (Wagner, Chantry, Dewey, & Nommsen-Rivers, 2013). Between week one and week six, a rapid drop in prevalence of EBF in the step 1–10 group (96% to 81%) compared to a relatively stable prevalence (93% to 90%) in step 1–9 group, was observed. A possible result of the flyers women took home after discharge from the maternity ward and increased family member involvement, is that it might have brought about more concerns regarding EBF. In addition, after those women returned to the clinic for the week six visit, feeling pressure from nurses regarding EBF may have led to some discouragements and thus the continuous drop in EBF prevalence. Generally, efforts to implement step 10 have not been successful at increasing or maintaining optimal breastfeeding practices (Hoddinott, Craig, Maclennan, Boyers, & Vale, 2012), thus the call for the WHO and UNICEF to revised the BFHI policy (Pat Hoddinott, 2016; Marcel Yotebieng & Frieda Behets, 2016).
Despite the fact that the data comes from a well-implemented cluster randomized trial, this analysis has several limitations. First, only participants in the original trial who remained in care through at least the six-week visit were eligible for inclusion. However, baseline characteristics of excluded mother-infant pairs were not substantively different. Second, outcomes were reported by mothers and misclassification is possible. Time between follow-up visits was also several weeks (4–6 weeks), increasing the possibility of recall bias. Nonetheless, given the randomized nature of the study and the fact that participants were not told which group they were in, any potential misclassification is likely non-differential, meaning the observed effect is likely conservative. Third, the exact time of occurrence of each episode of outcomes is unknown, and midpoints were used instead. Lastly, about 12% of participants were LTFU before the end of the study. However, in a sensitivity analysis where the infants of women LTFU were considered to have the outcome of interest, the results did not change substantially (Supplement 1).
Conclusion
Implementation of basic training in BFHI steps 1–9 significantly reduced incidence of mild and severe episodes of diarrhea and respiratory infection in the first 6 months from birth. Additional support based on the same training materials and locally available breastfeeding support materials, offered during well-child visits (i.e. step 10) lessened, the protective effect by reducing EBF.
Acknowledgements
We are grateful for the participation and time of the mothers and infants who participated in the study; the time and efforts of the personnel at the participating clinics (Esengo, Kikenda, Kitega, Libikisi, Lukunga, and Luyindu); the technical support of Drs. Aimee Lulebo, Dinah Kayembe, Landry Kiketa, Jean Lambert S. Chalachala, Mrs. Kathryn Salisbury, and Deidre Thompson; the data collection and data entry contributions of Clever Akili, Dyna Anambatu, Valerie B. Chalachala, Marie Dauly, Dydy Kayembe, Mamie Lulebo, Fanny Matadi, Myriam Mbonze, Espérance Mindia, Sarah Mushiya, Gisèle Mvumbi, Dodo Mwela, Jolly Ntirume, Ros Samba; and the administrative support of the UNC, KSPH, and Alive & Thrive administrative teams.
Funding
The original trial was supported by a grant from the Bill & Melinda Gates Foundation to FHI 360, through the Alive & Thrive Small Grants Program managed by UC Davis via a sub-award to the University of North Carolina at Chapel Hill. MY is partially supported by the NIAID U01AI096299-01 and the NICHD R01HD087993. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, writing of the report, or the decision to submit the paper for publication.
REFERENCES
- Bhutta ZA, Das JK, Walker N, Rizvi A, Campbell H, Rudan I, & Black RE (2013). Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet, 381(9875), 1417–1429. doi: 10.1016/s0140-6736(13)60648-0 [DOI] [PubMed] [Google Scholar]
- Das JK, Salam RA, & Bhutta ZA (2014). Global burden of childhood diarrhea and interventions. Curr Opin Infect Dis, 27(5), 451–458. doi: 10.1097/qco.0000000000000096 [DOI] [PubMed] [Google Scholar]
- Hoddinott P (2016). Step 10: the breastfeeding support paradox. Lancet Glob Health, 4(1), e19. doi: 10.1016/s2214-109x(15)00220-x [DOI] [PubMed] [Google Scholar]
- Hoddinott P (2016). Step 10: the breastfeeding support paradox. The Lancet Global Health, 4(1), e19. doi: 10.1016/S2214-109X(15)00220-X [DOI] [PubMed] [Google Scholar]
- Hoddinott P, Craig L, Maclennan G, Boyers D, & Vale L (2012). The FEeding Support Team (FEST) randomised, controlled feasibility trial of proactive and reactive telephone support for breastfeeding women living in disadvantaged areas. BMJ Open, 2(2). doi: 10.1136/bmjopen-2011-000652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, … Lau J. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep)(153), 1–186. [PMC free article] [PubMed] [Google Scholar]
- Kramer MS, & Kakuma R (2012). Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev(8), Cd003517. doi: 10.1002/14651858.CD003517.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, … Black RE. (2012). Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. The Lancet, 379(9832), 2151–2161. [DOI] [PubMed] [Google Scholar]
- Ministere du Plan, Institut National de la Statistique, & UNICEF. (2010). Enquete par grappes a indicateurs multiples - RDC 2010: Resultat Preliminaires. Retrieved from http://www.childinfo.org/files/MICS_RDC_2010.pdf
- Simmer K, & Patole S Implementation of the Ten Steps to Successful Breastfeeding programme in DR Congo. The Lancet Global Health, 3(9), e506–e507. doi: 10.1016/S2214-109X(15)00005-4 [DOI] [PubMed] [Google Scholar]
- UNCEF. (January 12, 2005). The Baby-Friendly Hospital Initiative. Retrieved from http://www.unicef.org/nutrition/index_24806.html
- Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, … Rollins NC. (2016). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475–490. doi: 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Wagner EA, Chantry CJ, Dewey KG, & Nommsen-Rivers LA (2013). Breastfeeding Concerns at 3 and 7 Days Postpartum and Feeding Status at 2 Months. Pediatrics. doi: 10.1542/peds.2013-0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker CL, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, … Black RE. (2013). Global burden of childhood pneumonia and diarrhoea. Lancet, 381(9875), 1405–1416. doi: 10.1016/s0140-6736(13)60222-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Bhutta ZA, Coates MM, Coggeshall M, Dandona L, Diallo K, … Murray CJL. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet, 388(10053), 1725–1774. doi: 10.1016/S0140-6736(16)31575-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO/UNICEF. (1989). Protecting, promoting and supporting breast-feeding: The special role of maternity services - a joint WHO/UNICEF statement Retrieved from Geneva, Switzerland: http://www.who.int/nutrition/publications/infantfeeding/9241561300/en/index.html
- WHO/UNICEF. (2009). Baby-friendly hospital initiative : revised., updated and expanded for integrated care Retrieved from http://www.unicef.org/nutrition/files/BFHI_2009_s3.1and2.pdf [PubMed]
- Yotebieng M, & Behets F (2016). Step 10: the breastfeeding support paradox - Authors’ reply. Lancet Glob Health, 4(1), e20. doi: 10.1016/s2214-109x(15)00221-1 [DOI] [PubMed] [Google Scholar]
- Yotebieng M, & Behets F (2016). Step 10: the breastfeeding support paradox – Authors’ reply. The Lancet Global Health, 4(1), e20. doi: 10.1016/S2214-109X(15)00221-1 [DOI] [PubMed] [Google Scholar]
- Yotebieng M, Chalachala JL, Labbok M, & Behets F (2013). Infant feeding practices and determinants of poor breastfeeding behavior in Kinshasa, Democratic Republic of Congo: a descriptive study. Int Breastfeed J, 8(1), 11. doi: 10.1186/1746-4358-8-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yotebieng M, Labbok M, Soeters HM, Chalachala JL, Lapika B, Vitta BS, & Behets F (2015). Ten Steps to Successful Breastfeeding programme to promote early initiation and exclusive breastfeeding in DR Congo: a cluster-randomised controlled trial. Lancet Glob Health, 3(9), e546–555. doi: 10.1016/s2214-109x(15)00012-1 [DOI] [PubMed] [Google Scholar]
- You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C, … Alkema L. (2015). Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. The Lancet, 386(10010), 2275–2286. doi: 10.1016/S0140-6736(15)00120-8 [DOI] [PubMed] [Google Scholar]


