Abstract
Objective
Prolonged preoperative fasting may lead to dehydration, hypoglycaemia, ketoacidosis and delayed recovery. We hypothesised that a patient educational initiative would decrease our preoperative fasting periods for elective caesarean delivery.
Methods
This was an observational quality improvement impact study. Elective caesarean patients who delivered during our study period were included in the study, 40 patients in the pre-intervention and 40 patients in the post-intervention groups. Only English-speaking patients were included. We developed a patient educational pamphlet outlining preoperative fasting and analgesic expectations for caesarean delivery that was given to every patient at her preoperative anaesthesia consultation. The pamphlet included the American Society of Anesthesiologists’ preoperative fasting and enhanced recovery carbohydrate drink recommendations. The primary outcome measure was intended fasting duration for liquids (defined as time from last reported liquid consumption to scheduled caesarean delivery) before and after the patient educational initiative. Secondary outcomes included solid fasting time, types of liquids and solids consumed.
Results
The intended median (interquartile range) fasting time for liquids decreased from 10 (8.9–12) h to 3.5 (2.5–10) h (p<0.001). The fasting period for solids was not significantly different: 12.5 (10.5–14) h pre- versus 12.4 (10.6–14) h post-pamphlet introduction (p=0.384). Despite the recommendation, only 22.5% consumed a carbohydrate-containing drink with a modest decrease in water consumption (87.5% before and 67.5% after; p=0.009).
Conclusion
A patient educational pamphlet significantly reduced fasting time for clear liquids. Future studies are needed to determine what barriers limited adherence to the recommended carbohydrate-containing drink consumption.
Keywords: Caesarean delivery, education, enhanced recovery, fasting, quality assurance
Introduction
The American Society of Anesthesiologists’ (ASA) 2016 Practice Guidelines for Obstetric Anaesthesia (1, 2) recommends that patients restrict clear fluid consumption for at least 2 h and solid foods for 6–8 h before induction of general or neuraxial anaesthesia. Preoperative fasting reduces the risk of emesis; however, prolonged fasting may lead to hypoglycaemia, dehydration, ketoacidosis, delayed recovery and reduced patient satisfaction (3–5). Pregnant women who are hypovolaemic may be at higher risk of hypotension after spinal anaesthesia.
Institutional and national guidelines to withhold food and drink overnight may lead to excessive periods of fasting prior to caesarean delivery. Enhanced recovery after surgery (ERAS) protocols encourage drinking fluids, preferably carbohydrate-containing drinks, up to 2 h before surgery (5–8). Limiting the duration of fasting may enhance recovery after surgery and decrease length of stay (5, 6). To minimise fasting periods prior to caesarean delivery, implementation of a patient educational initiative was undertaken at our institution. The aim of this quality improvement project analysis was to determine fasting times for patients undergoing scheduled caesarean delivery before and after the introduction of this initiative. We hypothesised that providing patients with an educational pamphlet outlining the recommended fasting times the day before their scheduled elective caesarean delivery would reduce preoperative liquid fasting time and increase consumption of carbohydrate-containing drinks.
Methods
Stanford University Institutional Review Board exemption was obtained (7 July 2016) prior to the initiation of this quality improvement project. The Institutional Review Board assessed that the project did not meet the federal definition of research or clinical investigation. No written informed consent was deemed required or obtained during this quality improvement project. We approached women undergoing elective caesarean delivery to determine fasting practices for liquids and solids before and after developing and initiating a patient-directed educational pamphlet (Appendix 1. See appendix https://doi.org/10.5152/TJAR.2019.95770) outlining anaesthesia for caesarean delivery. Prior to the implementation of this educational initiative, all women undergoing elective caesarean delivery underwent a preoperative anaesthesia consultation where they were instructed about the scheduled time of their caesarean delivery, as well as fasting recommendations and the risks and benefits of anaesthesia. Prior to this initiative, patients relied on verbal instruction from anaesthesia providers and nurses, and were not provided with specific instructional handouts from the anaesthesia service to take home following their consultation. We developed an educational pamphlet detailing information regarding anaesthesia for caesarean delivery. The educational pamphlet was written in a sixth-grade reading comprehension level and developed only in English. This pamphlet was implemented into our standard workflow and given to every patient at her preoperative anaesthesia consultation that occurred the day prior to her scheduled caesarean delivery at our labour and delivery unit. Patients received the same information during their preoperative consultation as before we implemented the educational initiative; however, they are now provided with this more standardised educational pamphlet to take home and read.
The pamphlet included the ASA recommendations for fasting guideline of 2 h for clear fluids and 8 h for solids combined with ERAS recommendation for consumption of carbohydrate-containing drinks up to 2 h prior to surgery (5, 7, 9). Patients were encouraged to drink up to 12 oz of a carbohydrate-containing drink; however, the drink was not provided to them at the time of the preoperative anaesthesia consultation.
We interviewed a convenient sample of 40 women undergoing scheduled caesarean delivery on fasting practices for liquids and solids prior to pamphlet implementation and interviewed a sample of 40 women post-pamphlet implementation. All women who undergo elective caesarean delivery at our institution are admitted to the preoperative unit 60–90 min prior to their scheduled caesarean delivery surgery time. During this time, the patients are prepared for their caesarean delivery, for example, a peripheral intravenous line is inserted, and consent and laboratory results are reviewed. We approached the women in the preoperative area on the day of surgery, after they had been admitted for their caesarean delivery, to collect their responses regarding current fasting status. Pre-pamphlet data were collected from June 2016 to July 2016, and post-pamphlet data were collected from January 2017 to June 2017. The following questions were asked in our pre-pamphlet group: (1) when was your last fluid intake prior to surgery and what did you drink? (2) when was your last solid meal prior to surgery and what did you eat? (3) were you hungry prior to your caesarean section? (4) if you were given the option of drinking a liquid energy drink or protein shake prior to your surgery, do you think that would have improved your experience? and (5) were you told ahead of time by a nurse or doctor about fasting prior to surgery? The following questions were asked in our post-pamphlet group: (1) did you receive a copy of the pamphlet? (2) did you read the pamphlet? (3) was the pamphlet helpful? (4) what is your understanding of how many hours before your caesarean that you can drink? (5) when was your last fluid intake? (6) what did you drink? (7) what is your understanding of how many hours before your caesarean that you can eat? (8) when was your last solid intake? (9) what did you eat? (10) are you hungry? and (11) are you thirsty? No demographic, obstetric or patient-identifying data were collected as part of this quality improvement project.
The primary outcome measure was the intended fasting duration for liquids, defined as the time duration between patient last reported liquid consumption and the scheduled caesarean delivery time. Secondary outcomes included the intended fasting duration for solids, the actual fasting duration for liquids and solids (defined as the time duration between patient last reported liquid or food consumption and neuraxial block placement), patient self-reported thirst and hunger, types of drinks consumed (water vs. other liquid) and solids consumed (heavy, defined as a meal containing high fat content vs. light, defined as a meal containing low fat content).
Statistical analysis
Data were analysed using IBM Statistical Package for the Social Sciences Statistics for Windows, version 23 (IBM SPSS Corp.; Armonk, NY, USA). Data are presented as mean±standard deviation, median (interquartile range; range) and count (percentage), as appropriate. Statistical tests for primary and secondary outcome measures included between groups comparisons using the Student’s t-test for normally distributed variables and Mann-Whitney U test for non-parametric comparisons. Data were graphed, and QQ test was performed to assess the normality of data distribution. Categorical variables were investigated using Pearson’s chi-square test. A p-value of <0.05 was considered statistically significant.
Results
We had complete data from 33 out of 40 women in the pre-pamphlet group and 40 out of 40 women in the post-pamphlet implementation group. Missing data were a result of unrecorded scheduled caesarean delivery times and/or unrecorded block placement times in the pre-pamphlet group. We had a 97.5% (39 out of 40) implementation rate of women receiving the pamphlet at their preoperative anaesthesia visit. A self-reported 92.3% (36 out of 39) of those who received the pamphlet at their anaesthesia consult visit reported reading the pamphlet. All patients (36 out of 36) who read the pamphlet reported finding the information helpful.
There was a significant difference in liquid fasting times between the pre- and post-pamphlet group. Median (interquartile range) liquid fasting times were 10 (8.9–12) h in the pre- and 3.5 (2.5–10) h in the post-pamphlet introduction groups (p<0.001; Figure 1). Women’s understanding of liquid fasting duration was 2 (2-2) h, consistent with the recommendation in the pamphlet. Actual liquid fasting times between pre- and post-pamphlet groups were also statistically different (p<0.001; Table 1). The median (interquartile range) delay for surgical start time was 0.5 (0.1–0.8) h. Delay in surgery caused a difference between intended and actual fasting times for both liquids (p=0.007) and solids (p<0.001), respectively. Before intervention, 87.5% (35 out of 40) of women consumed water, and after pamphlet introduction, 67.5% (27 out of 40) of women consumed water (p=0.009). Of the 40 patients, 0% and 22.5% consumed a carbohydrate-containing drink in the pre- and post-pamphlet groups, respectively.
Figure 1.
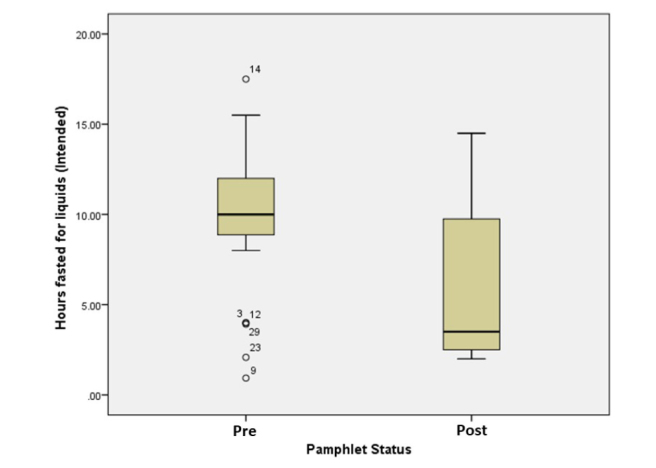
Intended liquid fasting times pre- and post-intervention
Table 1.
Liquid and solid fasting times pre-and post-intervention
| Pre- Intervention n=33 | Post- Intervention n=40 | p | |
|---|---|---|---|
|
| |||
| Intended Fasting Time Liquids | 10 [8.9–12] | 3.5 [2.5–10] | <0.001 |
| Actual Fasting Time Liquids | 10.4 [9.1–12.4] | 3.9 [3.0–10.1] | <0.001 |
| Intended Fasting Time Solids | 12.5 [10.5–14.0] | 12.4 [10.6–14.0] | 0.384 |
| Actual Fasting Time Solids | 13.6 [10.8–14.5] | 12.9 [10.8–14.5] | 0.907 |
Values are median [interquartile range] in hours
Before intervention, 53.8% (21 out of 39) of women reported eating a heavy meal the night prior to caesarean delivery, and after pamphlet introduction, 50% (20 out of 40) consumed a heavy meal the night prior (p=0.732). Pamphlet introduction did not impact patients’ perception of hunger, and 62.5% (25 out of 40) reported hunger before vs. 75% (30 out of 40) reported hunger after the pamphlet implementation (p=0.228). Subjective perception of thirst was only asked in the post-pamphlet group. Although women reported shorter liquid fasting times, a high proportion, 82.5% of women, still reported thirst.
Discussion
This quality improvement project demonstrates that a patient educational pamphlet is effective at decreasing preoperative liquid fasting times in patients undergoing elective caesarean delivery. Successful implementation of a patient educational pamphlet requires integration into the workflow of preoperative anaesthesia consultation for elective caesarean patients. ERAS protocols utilised in other surgical subspecialties, such as colorectal, urology and gynaecology-oncology, recommend pre-admission education and counselling (9–12). Prior to this educational initiative, patients were verbally instructed on the current fasting practice during their preoperative anaesthesia consultation; however, median (interquartile range) liquid fasting time was 10 (8.9–12) h, suggesting that not all women understood nor retained the information relayed to them during their consultation. We had a very high (97.5%) pamphlet distribution rate, and all the patients who read the pamphlet reported finding the information helpful. Our patients also demonstrated understanding of the preoperative fasting recommendation with a median (interquartile range) for their understanding of liquid fasting time of 2 (2-2) h. However, the actual post-intervention liquid fasting times were higher (3.5 h) than the 2 h recommended, and the interquartile range of 2.5–9.9 h suggests variability in patient application of this knowledge.
The ASA 2016 Guidelines for Obstetric Anaesthesia (1, 2) recommends preoperative fasting to 2 h for clear liquids. Prolonged fasting (i.e. nil per os after midnight) has not been shown to lower the amount of gastric contents nor decrease gastric acidity (10, 13, 14). Perioperative fasting is associated with increased surgical stress, increased insulin resistance and impaired gastrointestinal function (6, 7, 15). Impaired gastrointestinal function, such as postoperative ileus, has been demonstrated to significantly prolong post-caesarean delivery length of stay (16). Measures that can improve patient’s nutritional status in the perioperative period could potentially lead to improved clinical outcome in the caesarean delivery patient population. ERAS protocols utilised in colorectal surgery have shortened hospital length of stay and decreased complication rates by up to 30–50% (9, 11, 15). Although there are no national guidelines for enhanced recovery fasting recommendations or guidelines for caesarean delivery, Wrench et al. (17) have successfully demonstrated adoption of ERAS protocol to the obstetric unit and its impact on decreased length of stay for elective caesarean deliveries. Adoption of an ERAS protocol and associated reduction in fasting duration before elective caesarean may have other benefits, such as decreased complication rates and decreased postoperative ileus that have been observed in other surgical subspecialties.
A key component of ERAS protocols is minimising fasting period and increasing nutritional support. Surgery induces a catabolic state; the recommendation of a preoperative carbohydrate-containing drink 2 h prior to caesarean delivery aims to keep the patient metabolically balanced and decrease insulin resistance (5, 6, 8, 12, 15). Our educational pamphlet recommends that women drink a carbohydrate-containing drink as their clear liquid 2 h before their scheduled elective caesarean delivery. Before the implementation of this educational initiative, patients were verbally instructed on the types of liquids that met the criteria for clear liquids but were not consistently instructed to drink a carbohydrate-containing drink as their clear liquid. Our pamphlet initiative standardised our clear liquid recommendations, such that all women were instructed to consume a carbohydrate-containing drink as their clear liquid. Despite this, our recommendation had a modest impact with only 22.5% of patients consuming a carbohydrate-containing drink, such as Gatorade, after the educational intervention, and water was still consumed by most women (87.5% before and 67.5% after introduction of the pamphlet). Self-reported reasons for not choosing a carbohydrate-containing drink include not readily available at home, preference for unsweetened drink and preference for water. Giving patients a carbohydrate-containing drink on the day of their preoperative anaesthesia consultation visit, as is often done for colorectal and other ERAS protocols, may help to improve adherence with this recommendation.
Our pamphlet initiative did not significantly change the intended and actual fasting times for solids for our pre- and post-pamphlet groups. Therefore, patient self-report of hunger was not significantly different between the two groups. Our educational pamphlet did not make recommendations regarding the types of solid food to consume; consequently, the percentage of women who ate a heavy meal in the pre- and post-pamphlet groups was not significantly different. Recommendations for type of solids consumption could be considered when implementing patient fasting educational initiatives; however, we did not find a difference in reported hunger between women consuming or not consuming a ‘heavy meal’.
We found a delay between actual and scheduled caesarean delivery times. On average, this increased fasting times for both liquids and solids by only 0.5 h. During this quality improvement analysis period, wrongful adherence to the fasting guidelines did not contribute to surgical delay. Scheduled elective caesarean deliveries are sometimes delayed to accommodate urgent cases on the obstetric suite, and delays will vary amongst institutions with different workload demands or staffing availability. A prolonged delay can significantly impact a woman’s fasting duration and contribute to hypovolaemia and potentially greater haemodynamic instability after neuraxial anaesthesia. Offering clear fluids to women awaiting caesarean delivery should be considered if significant delays are expected or unexpectedly occur.
Our quality assurance study has several limitations. The goals of our analysis were to examine the feasibility of implementing new fasting recommendations and to observe any change in behaviour with regard to fasting practices. We did not examine barriers to adherence of our recommendations or of the significance the change in liquid fasting time would have on patient outcomes. This patient educational pamphlet was initially developed in English and given to English-speaking patients; therefore, we cannot generalise its effect to patients whose primary language is not English.
Conclusion
This quality assurance analysis demonstrates that a patient educational pamphlet given at the time of preoperative anaesthesia consultation can significantly reduce fasting time for clear liquids. However, the consumption of carbohydrate-containing drinks was limited despite the pamphlet’s recommendation for these liquids rather than water to enhance recovery. Future studies are needed to examine barriers against carbohydrate-containing drink consumption and if different initiatives can increase carbohydrate-containing drink utilisation. The impact of shorter liquid fasting duration and heavy versus light preoperative meals on maternal and foetal outcomes after caesarean delivery need further investigation.
Appendix 1.
Footnotes
Ethics Committee Approval: Notice of Determination of Human Subject Research was obtained 7 July 2016. The Stanford University Institutional Review Board assessed that this quality improvement project did not meet the federal definition of research or clinical investigation, and Institutional Review Board exemption was obtained prior to the initiation of this quality improvement project.
Informed Consent: No written informed consent was deemed required by the Stanford University Institutional Review Board for this quality improvement project.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – B.C.; Design – B.C., M.Y., A.C., J.J.K, A.J.T.; Supervision – B.C., A.J.T.; Resources – B.C.; Materials – B.C., M.Y., A.C., J.J.K.; Data Collection and/or Processing – M.Y., A.C., J.J.K.; Analysis and/or Interpretation – B.C., M.Y., A.C., J.J.K., A.J.T.; Literature Search – B.C., M.Y., A.C., J.J.K.; Writing Manuscript – B.C., M.Y., A.C., J.J.K., A.J.T.; Critical Review – B.C., M.Y., A.C., J.J.K., A.J.T.; Other – B.C., M.Y., A.C.
Conflict of Interest: The authors have no conflicts of interest to declare.
You can reach the questionnaire of this article at https://doi.org/10.5152/TJAR.2019.95770.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Practice Guidelines for Obstetric Anesthesia: An Updated Report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology. 2016;124:270–300. doi: 10.1097/ALN.0000000000000935. [DOI] [PubMed] [Google Scholar]
- 2.Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures: An Updated Report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology. 2017;126:376–93. doi: 10.1097/ALN.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 3.Can MF, Yagci G, Dag B, Ozturk E, Gorgulu S, Simsek A, et al. Preoperative administration of oral carbohydrate-rich solutions: Comparison of glucometabolic responses and tolerability between patients with and without insulin resistance. Nutrition. 2009;25:72–7. doi: 10.1016/j.nut.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 4.Gustafsson UO, Nygren J, Thorell A, Soop M, Hellstrom PM, Ljungqvist O, et al. Pre-operative carbohydrate loading may be used in type 2 diabetes patients. Acta Anaesthesiol Scand. 2008;52:946–51. doi: 10.1111/j.1399-6576.2008.01599.x. [DOI] [PubMed] [Google Scholar]
- 5.Neville A, Lee L, Antonescu I, Mayo NE, Vassiliou MC, Fried GM, et al. Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg. 2014;101:159–70. doi: 10.1002/bjs.9324. [DOI] [PubMed] [Google Scholar]
- 6.Gillis C, Carli F. Promoting Perioperative Metabolic and Nutritional Care. Anesthesiology. 2015;123:1455–72. doi: 10.1097/ALN.0000000000000795. [DOI] [PubMed] [Google Scholar]
- 7.Jankowski CJ. Preparing the Patient for Enhanced Recovery After Surgery. Int Anesthesiol Clin. 2017;55:12–20. doi: 10.1097/AIA.0000000000000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003:CD004423. doi: 10.1002/14651858.CD004423. [DOI] [PubMed] [Google Scholar]
- 9.Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017;152:292–8. doi: 10.1001/jamasurg.2016.4952. [DOI] [PubMed] [Google Scholar]
- 10.Nygren J, Thorell A, Jacobsson H, Larsson S, Schnell PO, Hylen L, et al. Preoperative gastric emptying. Effects of anxiety and oral carbohydrate administration. Ann Surg. 1995;222:728–34. doi: 10.1097/00000658-199512000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466–77. doi: 10.1016/j.clnu.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Ljungqvist O. Jonathan E. Rhoads lecture 2011: Insulin resistance and enhanced recovery after surgery. JPEN J Parenter Enteral Nutr. 2012;36:389–98. doi: 10.1177/0148607112445580. [DOI] [PubMed] [Google Scholar]
- 13.Awad S, Blackshaw PE, Wright JW, Macdonald IA, Perkins AC, Lobo DN. A randomized crossover study of the effects of glutamine and lipid on the gastric emptying time of a preoperative carbohydrate drink. Clin Nutr. 2011;30:165–71. doi: 10.1016/j.clnu.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Ajuzieogu OV, Amucheazi AO, Nwagha UI, Ezike HA, Luka SK, Abam DS. Effect of routine preoperative fasting on residual gastric volume and acid in patients undergoing myomectomy. Niger J Clin Pract. 2016;19:816–20. doi: 10.4103/1119-3077.180049. [DOI] [PubMed] [Google Scholar]
- 15.Group EC. The Impact of Enhanced Recovery Protocol Compliance on Elective Colorectal Cancer Resection: Results From an International Registry. Ann Surg. 2015;261:1153–9. doi: 10.1097/SLA.0000000000001029. [DOI] [PubMed] [Google Scholar]
- 16.Blumenfeld YJ, El-Sayed YY, Lyell DJ, Nelson LM, Butwick AJ. Risk Factors for Prolonged Postpartum Length of Stay Following Cesarean Delivery. Am J Perinatol. 2015;32:825–32. doi: 10.1055/s-0034-1543953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wrench IJ, Allison A, Galimberti A, Radley S, Wilson MJ. Introduction of enhanced recovery for elective caesarean section enabling next day discharge: a tertiary centre experience. Int J Obstet Anesth. 2015;24:124–30. doi: 10.1016/j.ijoa.2015.01.003. [DOI] [PubMed] [Google Scholar]