Abstract
Introduction:
There is a lack of consensus regarding indications for surgical management of rotator cuff disease, which can lead to increased regional variation. The objective of this study was to describe the geographic variation in rates of rotator cuff repair (RCR) in the United States over time, and identify regional characteristics associated with utilization.
Methods:
The United States was divided into 306 hospital referral regions. The adjusted per capita RCR rate was calculated using procedural counts derived from the Medicare Part B Carrier File from 2004-2014. Population-weighted multivariable regression was used to identify regional characteristics independently associated with utilization in 2014.
Results:
In 2014, there was an 8-fold difference in rates of RCR between regions. Between 2010 and 2014, the overall rate of RCR grew only 3.6% and regional variation decreased. Higher regional utilization of several other orthopedic procedures (p<0.02), and the regional supply of orthopedic surgeons (p=0.002), were independently associated with significantly increased utilization. The South, Southeast, and Southwest were independently associated with significantly higher utilization (p<0.001) when compared to the Northeast. A higher prevalence of resident physicians, a marker of the academic presence within a region, was independently associated with decreased utilization (p<0.001).
Conclusion:
Utilization of rotator cuff repair has increased substantially over the past decade but the rate of growth appears to be slowing. RCR remains a procedure with significant regional variation and increased utilization across regions is associated with higher orthopedic surgeon supply and increased rates of other orthopedic procedures.
Keywords: Rotator Cuff Tear, Rotator Cuff Repair, Geographic Variation
Geographic variation in rates of common surgical procedures is an important issue first quantified over 40 years ago in a landmark study by Gittelsohn and Wennberg (1973).47 Substantial variation in orthopedic procedure rates in the United States has also been observed historically4, 10, 11, 28, 30, 40, 45, 46 including a study demonstrating 4.7 and 6.5 fold regional differences in hip replacement and back surgery, respectively.5 Variation is usually greatest in procedures with controversial indications and a lack of consensus on optimal treatment, and can be quite significant.44, 47 This variation can indicate potential overutilization in some areas, and associated increases in the cost to the healthcare system, as well as possible underutilization in others, where patients may not have access to the care they desire or need. 34
Utilization rates of rotator cuff repair (RCR), the number of procedures per capita, were marked by high geographic variation in a study by Vitale et al which observed 9-fold differences in utilization of RCR across the United States in 1992.44 Rotator cuff tears can be successfully treated both surgically8, 9, 20, 21, 31-33, 35, 41 and nonsurgically.14, 22, 31, 35, 41 While the majority of patients are treated nonoperatively, approximately 25% will undergo surgical repair.27 Rates of RCR in the United States have grown substantially with growth of 141%-238% between the 1990s and 2000s13, 18 and 30% between 2005 and 2011.27 Rotator cuff repairs were historically completed in an open fashion12 until the development and dissemination of arthroscopic techniques in the 1990s,6-8, 19, 20, 41, 42 and use of this technique has grown rapidly.25, 27 Randomized control trials comparing operative and non-operative treatment have produced conflicting results,31, 32, 35 and a recent meta-analysis demonstrates clinically similar outcomes.39 Since both operative and non-operative treatments have proven effective, clinical practice guidelines regarding RCR provide only a weak recommendation for surgery,37 and there is heterogeneity among orthopedic surgeons regarding indications for surgery.17
Although geographic variation in rotator cuff repair has been studied in the past, the data is over 25 years old, and it is unknown how the rapid growth of the procedure, and the introduction of arthroscopic techniques, have impacted regional utilization. Therefore, the objectives of this study were to evaluate changes in RCR utilization between 2004 and 2014 in the United States, to describe the current status of geographic variation in RCR, and to identify regional characteristics associated with increased utilization rates.
Methods
Procedural Data
In this retrospective database study we first queried the Medicare Part B File (Carrier File) from 2004-2014 to determine procedure counts. This source provided a 40% nationwide sample in 2004-2005, and a 100% nationwide sample from 2006-2014. Procedure counts from 2004-2005 were extrapolated to the total Medicare population based upon the 40% sampling rate. We accessed the Medicare denominator file from 2004-2014 to determine the number of eligible beneficiaries annually based upon the mid-year population. All individuals included in the study were age 65 and older, as patients on Medicare due to disability or dialysis were excluded. All patients with traditional Medicare were included, while those with Medicare Advantage were excluded. The procedure of interest, rotator cuff repair, was identified using relevant CPT codes: open rotator cuff repair (acute)- 23410; open rotator cuff repair (chronic)- 23412; and arthroscopic rotator cuff repair- 29827.
Geographic Data
Hospital referral regions (HRRs) were defined across the United States using a previously described protocol developed by Wennberg and Cooper and the Dartmouth Atlas.16, 26 In summary, the methodology involved assigning each United States zip code to a hospital service area based upon the facility used most often by its inhabitants, which were then aggregated into 306 HRRs centered around tertiary-care facilities. The grouping according to tertiary-care facility was based upon the referral patterns for cardiac and neurosurgical procedures. Characteristics of HRRs were obtained from publicly available databases from The Dartmouth Atlas of Health Care.15, 16 Hospital referral region procedural rate data was available in less than 80% of HRRs in years 2004 and 2005 due to the 40% nationwide sample, precluding HRR-level analyses. In 2006, HRR level data was available in 304 regions, and 305 regions in 2014. The 2010 United States Census was used to determine the population density and mean income by region in the HRR databases. Physician densities were based upon information from the American Medical Association Physician Masterfile. The rates of surgical procedures, identified by ICD-9 codes, were derived from the Medicare MedPAR file and indirectly adjusted for the age, sex, and race distributions of the HRR.16 The Medicare 100% Claims File was used to calculate Total Medicare spending per capita, indirectly adjusted for price, age, sex, and race. When HRR data was not available for the year 2014, we utilized the closest year available. Accordingly, we referenced 2012 data for orthopedic procedure rates, 2001-2011 aggregate data for spinal surgery rates, and 2011 data for the supply of orthopedic surgeons and resident physicians. The presence of an academic medical center within a region was determined using the membership list of the Council of Teaching Hospitals from 2017, based upon the street address of member hospitals.1
Outcomes
Crude rotator cuff repair rates for each HRR were calculated by determining the number of procedures that met the inclusion criteria per year and then dividing by the mid-year Medicare population of the HRR. These rates were then adjusted using the indirect method16 for age, sex, and race; adjusted values were utilized for all additional analyses. Due to patient confidentiality, hospital referral regions with less than 11 procedures in a given year were suppressed, while rates based upon procedural counts of 12-26 annually were suppressed due to statistical imprecision due to the small sample size. The main outcome of interest was the per capital rotator cuff repair rate in each HRR.
Analysis
The degree of geographic variation rotator cuff repair rates between HRRs was evaluated annually using extremals (highest regional rate divided by lowest regional rate), inter-quartile ranges, coefficients of variation, and the systematic component of variation (SCV). The SCV was based upon age, race, sex- adjusted rates and reflects a measure of the non-random variation in rates across HRRs.5 We utilized ordinary least squares linear regression to complete population-weighted, multivariable analyses to evaluate associations between HRR characteristics and RCR rates in 2014. In all analyses a p-value < 0.05 was considered significant, and all statistical testing was completing using STATA v15.0 (College Station, TX, USA). The data utilized within this study did not contain identifiable patient information and was thereby exempt from IRB review at our institution.
Results
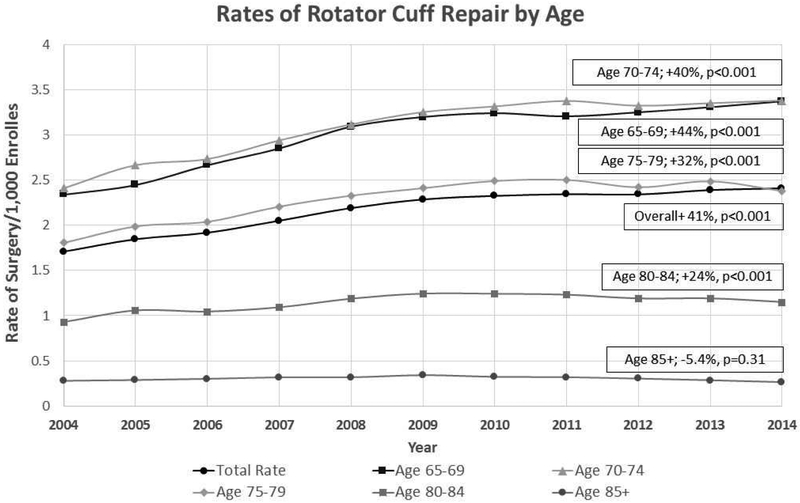
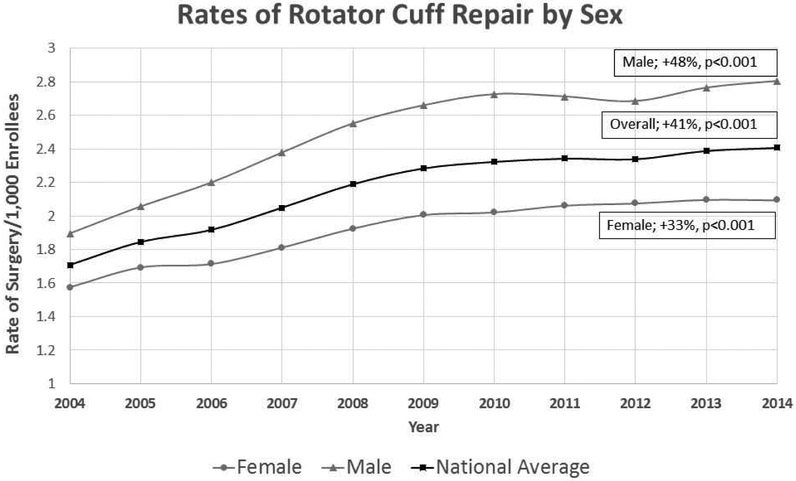
There were 19,402 RCR procedures observed in the 40% Medicare sample in 2004, and 66,804 RCR procedures observed in the 100% Medicare sample in 2014. These counts equated to a 41% increase between 2004-2014 in RCR utilization as the rate shifted from 1.7 to 2.4 procedures per 1,000 Medicare beneficiaries (p<0.001). Utilization of RCR increased 41.0% nationwide from 2004-2014 (p<0.001) but only increased 3.6% between 2010 and 2014 (p<0.001). Between 2004 and 2014, the 65-69 year-old age group increased the most with a 44% gain (p<0.001) while the age 85 and above group did not change significantly (p=0.31; Figure 1). The rates in females increased 33% (p<0.001) while the rates in males increased 48% (p<0.001) between 2004-2014 (Figure 2). The per capita rate of RCR in African American beneficiaries increased from 0.9 per 1,000 in 2004 to 1.4 per 1,000 in 2014, a 61% increase (p<0.001). In non-African Americans beneficiaries, the rate moved from 1.8 per 1,000 in 2004 to 2.5 per 1,000 in 2014, a 40% increase (p<0.001). In comparison to non-African American beneficiaries, the utilization of RCR was significantly lower in African Americans in both 2004 and 2014 (p<0.001).
Figure 1:
Rotator Cuff Repairs by Age.
Figure 2:
Rotator Cuff Repairs by Sex.
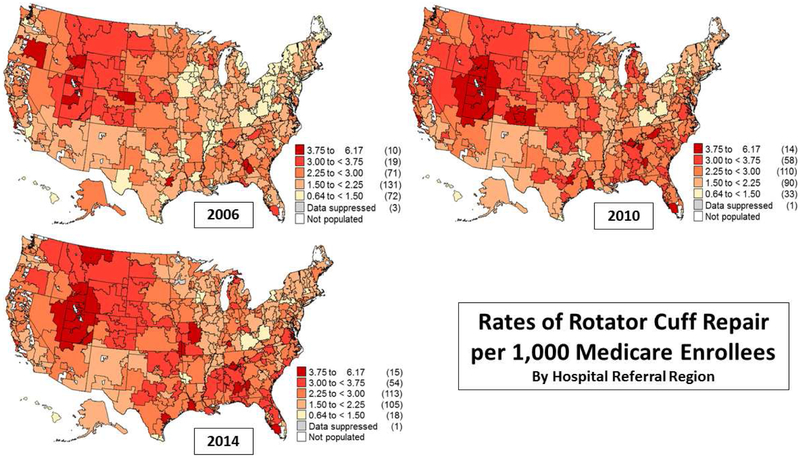
The rates of RCR in 2006 ranged from a high of 5.4 per 1,000 in Provo, UT to a low of 0.7 per 1,000 in Elmira, NY, and in 2014, from 5.0 per 1,000 in Provo, UT to a low of 0.7 per 1,000 in Scranton, PA, representing a nearly 8-fold difference in per capita rates between regions (Tables 1-2). The systematic component of variation, a quantifiable measure of non-random geographic variation, decreased slightly over the study period with a high of 116.7 in 2006 and a low of 83.7 in 2014 (Table 1). Additional measures of variation, including the extremal ratios (high/low) and interquartile ranges, did not change meaningfully during the study period. Rate maps demonstrated that utilization was generally higher in the Mountain West and Southeast while it was lower in the Upper Midwest and Northeast (Figure 3).
Table 1:
Measures of Geographic Variation over Time.
| 2006 (N=303) |
2007 (N=305) |
2008 (N=306) |
2009 (N=305) |
2010 (N=305) |
2011 (N=303) |
2012 (N=304) |
2013 (N=304) |
2014 (N=305) |
|
|---|---|---|---|---|---|---|---|---|---|
| Mean HRR rate* (SD) |
2.07 (0.74) |
2.19 (0.70) |
2.33 (0.72) |
2.45 (0.78) |
2.46 (0.78) |
2.47 (0.74) |
2.44 (0.74) |
2.51 (0.75) |
2.50 (0.71) |
| Median HRR rate* | 2.00 | 2.17 | 2.27 | 2.38 | 2.40 | 2.41 | 2.37 | 2.44 | 2.43 |
| Max. HRR rate* | 5.41 | 5.71 | 5.33 | 5.85 | 6.16 | 5.30 | 5.11 | 5.95 | 5.01 |
| Min. HRR rate* | 0.718 | 0.75 | 0.82 | 0.89 | 0.75 | 0.84 | 0.76 | 0.70 | 0.65 |
| Extremal quotient | 7.53 | 7.61 | 6.49 | 6.58 | 8.19 | 6.29 | 6.71 | 8.50 | 7.69 |
| Interquartile ratio | 1.59 | 1.50 | 1.49 | 1.47 | 1.51 | 1.49 | 1.52 | 1.45 | 1.50 |
| Coefficient of variation | 35.8 | 32.1 | 31.0 | 31.7 | 31.6 | 30.1 | 30.3 | 30.1 | 28.5 |
| Systematic Component of Variation | 116.7 | 102.4 | 89.5 | 95.5 | 103.6 | 92.0 | 100.5 | 90.9 | 83.7 |
Table 2:
Rotator Cuff Repair High and Low Rates by Hospital Referral Regions.
| 2006 Cohort | 2010 Cohort | 2014 Cohort | |||
|---|---|---|---|---|---|
| Region | RCR per 1,000 | Region | RCR oer 1,000 | Region | RCR per 1,000 |
| Highest 20 HRRs | Highest 20 HRRs | Highest 20 HRRs | |||
| UT- PROVO | 5.41 | UT- PROVO | 6.16 | UT- PROVO | 5.01 |
| UT- OCDEN | 5.25 | ID- IDAHO FALLS | 5.10 | UT- OGDEN | 4.71 |
| TX- BRYAN | 4.44 | FL- FORT MYERS | 4.80 | ID- IDAHO FALLS | 4.65 |
| OR- BEND | 4.30 | UT- OGDEN | 4.68 | MT- GREAT FALLS | 4.24 |
| ID- IDAHO FALLS | 4.22 | GA- ROME | 4.31 | LA- LAKE CHARLES | 4.15 |
| CO- GREELEY | 4.01 | CO-PUEBLO | 4.30 | FL- FORT MYERS | 4.10 |
| OR- SALEM | 3.95 | TX- BRYAN | 4.26 | AL- MONTGOMERY | 4.08 |
| GA- ALBANY | 3.95 | NC- ASHEVILLE | 4.17 | MO- JOPLIN | 4.07 |
| CA- SANTA BARBARA | 3.84 | UT- SALT LAKE CITY | 4.06 | AL- HUNTSVILLE | 4.03 |
| GA- COLUMBUS | 3.78 | CO- COLORADO SPRG | 4.05 | KY- OWENSBORO | 4.02 |
| MT- MISSOULA | 3.65 | AL- HUNTSVILLE | 4.03 | MO- COLUMBIA | 3.91 |
| UT- SALT LAKE CITY | 3.63 | CA- SAN LUIS OBISPO | 3.88 | TX- VICTORIA | 3.85 |
| CA- SALINAS | 3.62 | GA- COLUMBUS | 3.86 | VA- NEWPORT NEWS | 3.79 |
| FL- FORT MYERS | 3.51 | LA- LAKE CHARLES | 3.81 | GA- COLUMBUS | 3.79 |
| MT- BILLINGS | 3.51 | NE- LINCOLN | 3.75 | UT- SALT LAKE CITY | 3.79 |
| FL- PANAMA CITY | 3.49 | CA- SAN MATEO CO. | 3.73 | OR- BEND | 3.72 |
| CO- COLORADO SPRG | 3.40 | OR- BEND | 3.69 | TX- ABILENE | 3.66 |
| CO- GRAND JUNCTION | 3.38 | NC- WILMINGTON | 3.62 | NC- ASHEVILLE | 3.65 |
| WY- CASPER | 3.38 | MI- MUSKEGON | 3.58 | MI- MUSKEGON | 3.61 |
| AL- HUNTSVILLE | 3.35 | PA- LANCASTER | 3.52 | OK- OKLAHOMA CITY | 3.58 |
| Lowest 20 HRRs | Lowest 20 HRRs | Lowest 20 HRRs | |||
| RI- PROVIDENCE | 1.12 | IN- MUNSTER | 1.36 | IL- AURORA | 1.58 |
| TX- WICHITA FALLS | 1.11 | AR- TEXARKANA | 1.36 | IL- PEORIA | 1.55 |
| PA- SCRANTON | 1.10 | NJ- HACKENSACK | 1.35 | NJ- NEWARK | 1.47 |
| NJ- MORRISTOWN | 1.09 | IA- DAVENPORT | 1.35 | WV- CHARLESTON | 1.41 |
| WV- CHARLESTON | 1.09 | PA- ALTOONA | 1.34 | NJ- PATERSON | 1.41 |
| KY- PADUCAH | 1.08 | IL- PEORIA | 1.33 | FL- MIAMI | 1.41 |
| IA- MASON CITY | 1.08 | HI- HONOLULU | 1.33 | NY- BUFFALO | 1.41 |
| NJ- RIDGEWOOD | 1.06 | TX- HARLINGEN | 1.32 | PA-SAYRE | 1.39 |
| KY- LEXINGTON | 1.03 | IA- CEDAR RAPIDS | 1.32 | MA- SPRINGFIELD | 1.39 |
| MA- SPRINGFIELD | 1.00 | PA- WILKES-BARRE | 1.30 | HI- HONOLULU | 1.38 |
| PA- PHILADELPHIA | 1.00 | KY- LEXINGTON | 1.30 | IL- CHICAGO | 1.36 |
| NY- BUFFALO | 0.97 | PA- ERIE | 1.29 | KY- LEXINGTON | 1.31 |
| NY- MANHATTAN | 0.93 | NJ- PATERSON | 1.17 | AR- TEXARKANA | 1.18 |
| IL- BLUE ISLAND | 0.92 | NY- BRONX | 1.14 | NY- MANHATTAN | 1.18 |
| NY- BRONX | 0.90 | NY- MANHATTAN | 1.00 | PA- WILKES-BARRE | 1.06 |
| HI- HONOLULU | 0.87 | WI- LA CROSSE | 1.00 | NY- BRONX | 1.01 |
| WI- LA CROSSE | 0.85 | NJ- NEWARK | 0.91 | TX- MCALLEN | 0.95 |
| IL- CHICAGO | 0.84 | IL- CHICAGO | 0.87 | WI- LA CROSSE | 0.90 |
| NJ- NEWARK | 0.81 | MA- SPRINGFIELD | 0.81 | TX- HARLINGEN | 0.87 |
| NY- ELMIRA | 0.72 | PA- SCRANTON | 0.75 | PA- SCRANTON | 0.65 |
Figure 3:
Maps or Rotator Cuff Repair Rates in 2006-2014.
Multivariable, weighted regression analysis of 2014 data demonstrated that in comparison to regions in the bottom quartiles, HRRs in the top quartiles of either total shoulder arthroplasty (+ 0.35 procedures/1,000 beneficiaries; p=0.006), total knee arthroplasty (+ 0.48 procedures/1,000 beneficiaries; p=0.001), or spinal decompression (+ 0.27 procedures/1,000 beneficiaries; p=0.012) were independently associated with significantly higher RCR rates (Table 3). The supply of orthopedic surgeons in a region was also indepedently associated with increased RCR utilization in a dosewise fashion with successively higher procedure rates observed in each quartile of orthopedic surgeons per capita (test of trend p=0.004), and an associated increase of 0.35 procedures/1,000 beneficiaries in the top quartile of orthopedic surgeon supply (p=0.002).
Table 3:
Multivariable linear regression model evaluating the association between HRR characteristics and the rate of rotator cuff repair by HRR in 2014. The adjusted R2= 0.55.
| Variable | Change in RCR Rate (per/1,000 beneficiaries) |
95% Confidence Interval |
P-Value |
|---|---|---|---|
| Surgical Intensity | |||
| Total Shoulder Arthroplasty Rate^ | |||
| 1st Quartile (0.4 < 1.0) | Reference | Reference | Ref |
| 2nd Quartile (1.0 < 1.3) | +0.20 | +0.02 – +0.39 | 0.031* |
| 3rd Quartile (1.3 < 1.6) | +0.20 | −0.005 – +0.40 | 0.055 |
| 4th Quartile (1.6 - 2.8) | +0.35 | +0.10 – +0.60 | 0.006* |
| Knee Arthroplasty Rate^ | |||
| 1st Quartile (3.7 < 7.6) | Reference | Reference | Ref |
| 2nd Quartile (7.6 < 8.5) | + 0.14 | −0.04 – +0.32 | 0.14 |
| 3rd Quartile (8.5 < 9.5) | + 0.26 | +0.06 – +0.47 | 0.013* |
| 4th Quartile (9.5 -14.7) | + 0.48 | +0.21 – +0.75 | 0.001* |
| Hip Arthroplasty^ | |||
| 1st Quartile (1.5 < 3.3) | Reference | Reference | Ref |
| 2nd Quartile (3.3 < 3.9) | + 0.04 | −0.15 – +0.23 | 0.67 |
| 3rd Quartile (3.9 < 4.6) | + 0.09 | −0.14 – +0.32 | 0.46 |
| 4th Quartile (4.6 - 6.3) | + 0.34 | −0.29 – +0.28 | 0.98 |
| Spinal Decompression# | |||
| 1st Quartile (25 < 64) | Reference | Reference | Ref |
| 2nd Quartile (64 < 81) | + 0.12 | −0.06 – +0.30 | 0.20 |
| 3rd Quartile (81 < 102) | + 0.26 | +0.06 – +0.45 | 0.010* |
| 4th Quartile (102 -217) | + 0.27 | +0.06 – +0.48* | 0.012* |
| Healthcare Intensity | |||
| Medicare Spending per Capita$ | |||
| 1st Quartile (6,971 < 8,500) | Reference | Reference | Ref |
| 2nd Quartile (8,500 < 9,400) | + 0.22 | 0.01 – 0.43 | 0.044* |
| 3rd Quartile (9,400< 10,250) | + 0.29 | 0.06 – 0.52 | 0.013* |
| 4th Quartile (10,250 < 13,347) | + 0.20 | −0.06 – +0.45 | 0.14 |
| Physician Intensity | |||
| Supply of Ortho Surgeons+ | |||
| 1st Quartile (2.3 < 5.5) | Reference | Reference | Ref |
| 2nd Quartile (5.5 < 6.3) | + 0.19 | +0.01 – +0.37 | 0.043* |
| 3rd Quartile (6.3 < 7.1) | + 0.22 | +0.03 – +0.41 | 0.022* |
| 4th Quartile (7.1 −12.3) | + 0.35 | +0.13 – +0.57 | 0.002* # |
| Academic Intensity | |||
| Supply of Resident Physicians+ | |||
| 1st Quartile (3.9 < 15.0) | Reference | Reference | Ref |
| 2nd Quartile (15.0 < 23.4) | −0.39 | −0.60 – −0.18 | <0.001* |
| 3rd Quartile (23.4 < 35.7) | −0.47 | −0.70 – −0.23 | <0.001* |
| 4th Quartile (35.7 < 97.8) | −0.30 | −0.57 – −0.03 | 0.034* |
| Presence of Academic Medical Center | |||
| (versus No) | −0.005 | −0.18 – +0.17 | 0.96 |
| Socioeconomic Characteristics | |||
| % of Population with a College Degree | |||
| 1st Quartile (15 < 22) | Reference | Reference | Ref |
| 2nd Quartile (22 < 26) | + 0.15 | −0.07 – +0.37 | 0.19 |
| 3rd Quartile (26 < 31) | + 0.20 | −0.06 – +0.45 | 0.13 |
| 4th Quartile (31 < 57) | + 0.17 | −0.14 – +0.47 | 0.28 |
| % of Region Characterized as Rural | |||
| 1st Quartile (0 < 11) | Reference | Reference | Ref |
| 2nd Quartile (11 < 28) | + 0.06 | −0.12 – +0.24 | 0.52 |
| 3rd Quartile (28 < 41) | + 0.09 | −0.14 – +0.32 | 0.44 |
| 4th Quartile (41 < 75) | + 0.19 | −0.07 – +0.46 | 0.15 |
| Mean Household Income | |||
| 1st Quartile (41,917 < 56,700) | Reference | Reference | Ref |
| 2nd Quartile (56,700 < 61,600) | −0.04 | −0.27 – +0.18 | 0.71 |
| 3rd Quartile (61,600 < 71,000) | + 0.05 | −0.21 – +0.31 | 0.69 |
| 4th Quartile (71,000 < 140,344) | + 0.12 | −0.20 – +0.45 | 0.45 |
| Geography | |||
| Region of United States | |||
| Northeast | Reference | Reference | Ref |
| Southeast | + 0.65 | +0.44 – +0.87 | <0.001* |
| South | + 0.69 | +0.41 – +0.97 | <0.001* |
| Midwest | + 0.07 | −0.16 – +0.30 | 0.53 |
| Northwest | + 0.38 | −0.001 – +0.75 | 0.051 |
| Southwest | + 0.70 | +0.44 – +0.96 | <0.001* |
Model adjusted for all variables within the table in addition to the following non-significant variables: supply of total physicians in 2011 (by quartile), and supply of primary care physicians in 2011 (by quartile).
Rates are per 1,000 HRR Medicare beneficiaries;
Rates are per 100,000 beneficiaries;
Prevalence per 100,000 HRR inhabitants;
Total Medicare spending per beneficiary in 2014.
Denotes p-value <0.05 indicating statistical significance.
In comparison to regions in the bottom quartile, regions with an increased prevalence of resident physicians (all specialties), a marker of the concentration of teaching hospitals, were indepedently associated with significantly decreased RCR rates (Table 3). The presence of an academic medical center was not asssociated with RCR rates (p=0.96). When using the Northeast as a reference, the Southeast (+ 0.65 procedures/1,000 beneficiaries; p<0.001), South (+ 0.69 procedures/1,000 beneficiaries; p<0.001), and Southwest (+ 0.70 procedures/1,000 beneficiaries; p<0.001) were independently associated with higher RCR utilization. The per capita supply of primary care physicians, the education or income level of the population, and the population density of HRRs did not idependently influence utilization rates. The overall r2 value of the regression model was 0.55.
Discussion
As high healthcare spending continues to be a concern in the United States,36 understanding if RCR utilization continues to increase, and identifying regional factors influencing utilization, is critical. The results of this study demonstrated that non-random geographic variation has decreased in recent years despite an essentially stable 7-fold difference in RCR rates across HRRs. This suggests that while outlying regional RCR rates remain generally unchanged, the RCR rates of the majority of HRRs are converging over time. This reduction in variation has occurred in the context of a 40% overall increase in RCR rates nationwide, as well as an unchanged maximum regional RCR rate, indicating that the decrease in variation is occurring due to a shift of low utilizing HRRs upwards and a general consolidation around a higher overall RCR rate. Although there has been a 40% increase in overall utilization of RCR between 2004-2014, there is evidence that this growth is slowing with only a 3.6% increase between 2010 and 2014. Regression analysis demonstrated that several regional characteristics were independently associated with increased utilization including higher rates of shoulder and knee arthroplasty, a greater supply of orthopedic surgeons, and being in a Southern region, highlighting that increased utilization occurs regionally across orthopedic procedures. The model also demonstrated that an increased academic presence in a region was associated with significantly lower utilization, highlighting possible differences between academic and private practice settings.
Previous studies of the general population demonstrated a male to female ratio for RCR of 1.2913 in 2006 and 1.3618 in 2009 which was similar to the range of 1.2-1.3 demonstrated in the Medicare population. Our data also demonstrated that growth in utilization between sexes was not equal with males increasing 48% and females increasing only 33%, in contrast to a previous study demonstrating that RCR procedures in women increased twice as much as those in males between 1996-2006,13 highlighting how utilization trends change over time. We also observed that utilization increased most in the 65-69 year old age group (+44%) and increased less or remained stable in the older cohorts. Additionally, our data demonstrated that the 2004 nationwide rate of RCR in African American patients was less than half that of non-African American beneficiaries, congruent with previous literature highlighting a similar magnitude of racial disparity in knee arthroplasty40 and cervical spine surgery.2 While increased growth of RCR utilization was observed between 2004-2014 in the African American population, the utilization rate in non-African American patients remained 80% higher in 2014. Overall these results demonstrate how the growth in utilization of RCR between 2004-2014 occurred heterogeneously in the Medicare population.
Substantial small-area geographic variation in the utilization of orthopedic surgery has been observed historically across a range of procedures including rotator cuff repair,44 total shoulder arthroplasty,44 carpal tunnel release,29 operative fixation of upper extremity fractures,4, 11 lower extremity arthroplasty,5, 40, 45 and spine surgery.45, 46 Our data indicates that while geographic variation has decreased overall, it remains a high variation procedure. The 2014 systematic component of variation (SCV) value of 84 we observed remains higher than the degree of variation reported historically with knee (SCV 55) or hip (SCV 67) arthroplasty, and is more consistent with the amount of variation associated with spine surgery (SCV 90-93).45 All of these procedures are notably higher than the SCV value of 11 for hip fracture surgeries,5 an example of a low-variation procedure with little debate surrounding best practices. The small-area HRR based high/low (extremal) ratio of 7.69 in 2014 is lower than the 9.09 value reported by Vitale et al (1999),44 despite their use of 1992 statewide data that would have underestimated variation and suggests that overall geographic variation has likely decreased since that time. Similarly, although RCR remains a high-variation procedure, it is by no means at the top of the list with rates of distal radius and proximal humerus fixation and total shoulder arthroplasty demonstrating 10-fold11 or more4, 48 differences between high and low utilizing regions.
Previous literature has suggested that high variation procedures are often associated with scientific uncertainty,5, 45 an observation which applies to RCR as the literature continues to provide conflicting evidence regarding the merits of operative and conservative treatments.31, 32, 35, 37, 39 A survey-based study of orthopedic surgeons has demonstrated significant heterogeneity in the beliefs regarding the efficacy of RCR, and observed that surgeons who were more optimistic completed more surgeries;17 results demonstrating how clinical ambiguity can lead to variations in practice. However, differing rates of underlying RCR pathology among regions could also influence utilization rates. Indeed, a previous study of total knee arthroplasty highlighted that regions with increased utilization demonstrated higher rates of severe knee arthritis.23 Similarly, studies have demonstrated rates of proximal humerus fractures ranging from 0.43 to 5.47 per 1,000 medicare beneficiaries nationwide4, as well as 8-fold variation in the rates of ankle fractures in the elderly nationwide.30 It is important to point out that based upon our results we cannot conclude what the appropriate rate of RCR utilization, and it is difficult to determine what the ideal of RCR, or any elective surgical procedure, should be.34 Although we have identified factors associated with utilization, we cannot determine whether higher or lower utilization is desired.
A recent study from Sweden observed substantial rates of otherwise undiagnosed carpal tunnel syndrome in the population, and concluded that regional variation in procedures could be influenced by how these individuals interact with the medical system.3 This idea rings true in light of our results demonstrating a clear, dose-wise, relationship between the supply of orthopedic surgeons in a region and the rates of utilization in that area. Although RCR generally fits the description of prefererence-sensitive care where decisions made by patients and surgeons drive utilization,34 these results highlight the role that supply has in influencing rates as well. Subspeciality referrals are generally considered to be an example of suppy-sensitive care,34 and it is likely that the improved access afforded by an increased supply of orthopedic surgeons could ultimately increase utilization of surgical repair. These results are in agreement with those from a study by Weinstein et al (2004) which demonstrated increased utlization of hip arthroplasty and spine surgery in areas with greater supplies of orthopedic and neurosurgeons, respectively.45 In contrast, a study of of hip and knee arthroplasty by Peterson et al based upon data from 1988 demonstrated no relationship between statewide utilization and surgeon supply.38 A study by Vitale et al using data from 1992 also found that neither orthopedic-surgeon nor shoulder-specialist densities were independently associated with utilization of shoulder arthroplasty or rotator cuff repairs at the state level.44 These discrepancies with our findings may indicate that orthopedic surgeon supply affects utilization more than it did historically, or may be due to differences in methodology as we evaluted regional variation on a much smaller level.
In our regression model, HRRs in the Southeast, South, or Southwest were all independently associated with significantly higher utilization, and proved to be the regional characteristic with the largest association with utilization. These results highlight the larger regional nature of utilization across a range of upper and lower extremity orthopedic procedures, and are consistent with a previous study of surgical variation across a range of orthopedic, general, and vascular surgery procedures which observed that high-variation procedured often demonstrate larger regional trends of high or low utilization.5 Rate maps of proximal humerus fracture fixation procedures in 2004-2005 demonstrated similar trends to ours with increased surgical rates in the in the South and Southwest.4 Similarly, rate maps of distal radius fracture internal fixation surgeries also demonstrated high use in the South and Southeast, among other regions, in 2007.11 These results are in contrast to a recent study of variation in total shoulder arthroplasty which demonstrated increased utilization in the Mountain West and Upper Midwest but was otherwise very hetergenous indicating that our results do not apply to all shoulder procedures.48 Additionally, observations from a historical study of variation in hip and knee arthroplasty in 1988 demonstrated relatively decreased utilization of these procedures in the South, and highlight that a shift towards increased per capita orthopedic utilization may have occurred in these regions over the last 3 decades.38
Although previous studies have highlighted that lower population density is associated with increased orthpaedic procedure utilization, our results did not find an association between utilization and the proportion of the region considered rural,38, 44 suggesting that these past trends may not be applicable to current practice. It is worth noting that our results demonstrated that total Medicare spending was not independently associated with RCR utilization, similar to previous literature finding no association betwee hip and knee arthroplasty and regional spending.45 Our results also noted that an increased prevalence of resident physicians, a mark of the academic presence within an HRR, was correlated with decreased utilization, a trend similar to a previous study noting decreased utilization of cardiovascular procedures in academic versus private ppractice settings.24 These findings may be due to varying treatment algorithms between treatment settings, as has been shown previously in the treatment of slipped capital epiphysis,43 or could be due to differing patient populations and referral patterns. Alternatively, it is possible that academic practices are less efficient, and thereby less productive, than private practices.
Strengths of this study include the use of a 100% sample of Medicare patients with traditional coverage during the years 2006-2014. This allowed us to accurately assess the entire population and model relevant trends using well-established methods from the Dartmouth Atlas.16, 26 Limitations of this study include those inherent to any retrospective study relying upon Medicare billing data. These include inability to confirm the accuracy of the coding data, as well as being limited to the Medicare population over the age of 65. Although our methodology captured over 66,000 rotator cuff repair surgeries in 2014 alone, it is important to note our study includes only a portion of the rotator cuff repairs completed annually in the United States as many of these procedures are completed in younger patients, with previous studies reporting the overall average age of patients to be 60 years old or less.13, 18 With this in mind our data is important for understanding overall utilization of RCR in the Medicare population but its generalizability to patients under 65 is unknown. Additionally, we were unable to measure the supply of shoulder-specific surgeons in a given HRR and instead used the overall density of orthopedic surgeons for analysis. Evaluating the relationship between the supply of shoulder-specialists and RCR utilization would be more ideal for understanding the relationship between the surgeon supply and utilization of a region. Finally, we have no data on the severity of the underlying rotator cuff tear, or the magnitude of the corresponding surgical repair, for the procedures included within our study. While it would be very difficult to collect this data on a nationwide level, this level of detail would be helpful for further understanding regional variation in RCR utilization and for evaluating more specific trends within the overall picture of ongoing growth
Conclusions
The utilization of rotator cuff repair in the Medicare population has increased substantially between 2004-2014, but has slowed in recent years. Although regional differences have decreased over time, RCR remains a high-variation procedure. Results suggested that increased RCR utilization is correlated with increased rates of other orthopedic procedures and higher concetrations of orthopedic surgeons, while an increased regional academic presence was associated with decreased utilization.
Acknowledgements
Data for this project was obtained from The Dartmouth Atlas, which is funded by the Robert Wood Johnson Foundation and the Dartmouth Clinical and Translational Science Institute, under award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). Neither of these organizations had any role in data collection, data analysis, or the preparation of or editing of the manuscript.
The work for this project was partially funded by NIH Grant 5T32AR049710-14.
Sources of Funding: The project was partially funded by NIH Grant 5T32AR049710-14. This organization had no role in any data collection, data analysis, or the preparation of or editing of the manuscript.
Footnotes
Disclaimer: None
IRB: This study did not contain individually identifiable patient information and was exempt from IRB review at our institution.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Level of Evidence: Level III; Cross Sectional Design; Epidemiology Study
References
- 1.AAMC Hospital/Health System Members. In; 2018. [Google Scholar]
- 2.Alosh H, Riley LH 3rd, Skolasky RL. Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality: an examination of United States trends from 1992 to 2005. Spine 2009;34:1956–1962. 10.1097/BRS.0b013e3181ab930e [DOI] [PubMed] [Google Scholar]
- 3.Atroshi I, Gummesson C, Johnsson R, McCabe SJ, Ornstein E. Severe carpal tunnel syndrome potentially needing surgical treatment in a general population. The Journal of hand surgery 2003;28:639–644. [no doi] [DOI] [PubMed] [Google Scholar]
- 4.Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. The Journal of bone and joint surgery American volume 2011;93:121–131. 10.2106/jbjs.i.01505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE. Variation profiles of common surgical procedures. Surgery 1998;124:917–923. [PubMed] [Google Scholar]
- 6.Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical orthopaedics and related research 2001:107–118. [DOI] [PubMed] [Google Scholar]
- 7.Burkhart SS. The Burden of Craft in Arthroscopic Rotator Cuff Repair: Where Have We Been and Where We Are Going. American journal of orthopedics (Belle Mead, NJ) 2015;44:353–358. [no doi] [PubMed] [Google Scholar]
- 8.Burkhart SS, Danaceau SM, Pearce CE Jr. Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2001;17:905–912. [DOI] [PubMed] [Google Scholar]
- 9.Carr A, Cooper C, Campbell MK, Rees J, Moser J, Beard DJ et al. Effectiveness of open and arthroscopic rotator cuff repair (UKUFF): a randomised controlled trial. The bone & joint journal 2017;99-b:107–115. 10.1302/0301-620x.99b1.bjj-2016-0424.r1 [DOI] [PubMed] [Google Scholar]
- 10.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. The Journal of bone and joint surgery American volume 2009;91:1868–1873. 10.2106/jbjs.h.01297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung KC, Shauver MJ, Yin H, Kim HM, Baser O, Birkmeyer JD. Variations in the use of internal fixation for distal radial fracture in the United States medicare population. The Journal of bone and joint surgery American volume 2011;93:2154–2162. 10.2106/jbjs.j.012802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Codman EA. Complete rupture of the supraspinatus tendon. Operative treatment with report of two successful cases. 1911. Journal of shoulder and elbow surgery 2011;20:347–349. 10.1016/j.jse.2010.10.031 [DOI] [PubMed] [Google Scholar]
- 13.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. The Journal of bone and joint surgery American volume 2012;94:227–233. 10.2106/jbjs.j.00739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dalton SE. The conservative management of rotator cuff disorders. British journal of rheumatology 1994;33:663–667. [DOI] [PubMed] [Google Scholar]
- 15.The Dartmouth Atlas of Health Care- Data by Topic. In; 2018. [Google Scholar]
- 16.The Dartmouth Atlas of Health Care: Research Methods. In; 2018. [Google Scholar]
- 17.Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF et al. Variation in orthopaedic surgeons' perceptions about the indications for rotator cuff surgery. The Journal of bone and joint surgery American volume 2005;87:1978–1984. 10.2106/jbjs.d.02944 [DOI] [PubMed] [Google Scholar]
- 18.Ensor KL, Kwon YW, Dibeneditto MR, Zuckerman JD, Rokito AS. The rising incidence of rotator cuff repairs. Journal of shoulder and elbow surgery 2013;22:1628–1632. 10.1016/j.jse.2013.01.006 [DOI] [PubMed] [Google Scholar]
- 19.Gachter A, Seelig W. Arthroscopy of the shoulder joint. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 1992;8:89–97. [DOI] [PubMed] [Google Scholar]
- 20.Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. The Journal of bone and joint surgery American volume 1998;80:832–840. [DOI] [PubMed] [Google Scholar]
- 21.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clinical orthopaedics and related research 1994:43–53. [PubMed] [Google Scholar]
- 22.Goldberg BA, Nowinski RJ, Matsen FA 3rd. Outcome of nonoperative management of full-thickness rotator cuff tears. Clinical orthopaedics and related research 2001(382):99–107. [DOI] [PubMed] [Google Scholar]
- 23.Hawker GA, Wright JG, Coyte PC, Williams JI, Harvey B, Glazier R et al. Determining the need for hip and knee arthroplasty: the role of clinical severity and patients' preferences. Medical care 2001;39:206–216. [DOI] [PubMed] [Google Scholar]
- 24.Hovanesyan A, Rubio E, Novak E, Budoff M, Rich MW. Comparison of Rate of Utilization of Medicare Services in Private Versus Academic Cardiology Practice. The American journal of cardiology 2017;120:1899–1902. 10.1016/j.amjcard.2017.07.105 [DOI] [PubMed] [Google Scholar]
- 25.Iyengar JJ, Samagh SP, Schairer W, Singh G, Valone FH 3rd, Feeley BT. Current trends in rotator cuff repair: surgical technique, setting, and cost. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2014;30:284–288. 10.1016/j.arthro.2013.11.018 [DOI] [PubMed] [Google Scholar]
- 26.J Wennberg MC. The Quality of Medica Care in the United States: A Report on the Medicare Program, The Dartmouth Atlas of Health Care. Chicago: American Hospital Association Press; 1999. [PubMed] [Google Scholar]
- 27.Jensen AR, Cha PS, Devana SK, Ishmael C, Di Pauli von Treuheim T, D’Oro A et al. Evaluation of the Trends, Concomitant Procedures, and Complications With Open and Arthroscopic Rotator Cuff Repairs in the Medicare Population. Orthopaedic Journal of Sports Medicine 2017;5:2325967117731310 10.1177/2325967117731310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katz JN, Keller RB, Simmons BP, Rogers WD, Bessette L, Fossel AH et al. Maine Carpal Tunnel Study: outcomes of operative and nonoperative therapy for carpal tunnel syndrome in a community-based cohort. The Journal of hand surgery 1998;23:697–710. [DOI] [PubMed] [Google Scholar]
- 29.Keller RB, Largay AM, Soule DN, Katz JN. Maine Carpal Tunnel Study: small area variations. The Journal of hand surgery 1998;23:692–696. [DOI] [PubMed] [Google Scholar]
- 30.Koval KJ, Lurie J, Zhou W, Sparks MB, Cantu RV, Sporer SM et al. Ankle fractures in the elderly: what you get depends on where you live and who you see. Journal of orthopaedic trauma 2005;19:635–639. [no doi] [DOI] [PubMed] [Google Scholar]
- 31.Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T et al. Treatment of Nontraumatic Rotator Cuff Tears: A Randomized Controlled Trial with Two Years of Clinical and Imaging Follow-up. The Journal of bone and joint surgery American volume 2015;97:1729–1737. 10.2106/jbjs.n.01051 [DOI] [PubMed] [Google Scholar]
- 32.Lambers Heerspink FO, van Raay JJ, Koorevaar RC, van Eerden PJ, Westerbeek RE, van 't Riet E et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. Journal of shoulder and elbow surgery 2015;24:1274–1281. 10.1016/j.jse.2015.05.040 [DOI] [PubMed] [Google Scholar]
- 33.Liu J, Fan L, Zhu Y, Yu H, Xu T, Li G. Comparison of clinical outcomes in all-arthroscopic versus mini-open repair of rotator cuff tears: A randomized clinical trial. Medicine 2017;96:e6322 10.1097/md.0000000000006322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lurie JD, Bell JE, Weinstein J. What rate of utilization is appropriate in musculoskeletal care? Clinical orthopaedics and related research 2009;467:2506–2511. 10.1007/s11999-009-0889-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moosmayer S, Lund G, Seljom U, Svege I, Hennig T, Tariq R et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: A randomised controlled study of 103 patients with one-year follow-up. The Journal of bone and joint surgery British volume 2010;92:83–91. 10.1302/0301-620x.92b1.22609 [DOI] [PubMed] [Google Scholar]
- 36.Papanicolas I, Woskie LR, Jha AK. Health Care Spending in the United States and Other High-Income Countries. Jama 2018;319:1024–1039. 10.1001/jama.2018.1150 [DOI] [PubMed] [Google Scholar]
- 37.Pedowitz RA, Yamaguchi K, Ahmad CS, Burks RT, Flatow EL, Green A et al. Optimizing the management of rotator cuff problems. Journal of the American Academy of Orthopaedic Surgeons 2011;19:368–379. [no doi] [DOI] [PubMed] [Google Scholar]
- 38.Peterson MG, Hollenberg JP, Szatrowski TP, Johanson NA, Mancuso CA, Charlson ME. Geographic variations in the rates of elective total hip and knee arthroplasties among Medicare beneficiaries in the United States. The Journal of bone and joint surgery American volume 1992;74:1530–1539. [PubMed] [Google Scholar]
- 39.Piper CC, Hughes AJ, Ma Y, Wang H, Neviaser AS. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. Journal of shoulder and elbow surgery 2017. 10.1016/j.jse.2017.09.032 [DOI] [PubMed] [Google Scholar]
- 40.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. The New England journal of medicine 2003;349:1350–1359. 10.1056/NEJMsa021569 [DOI] [PubMed] [Google Scholar]
- 41.Tauro JC. Arthroscopic rotator cuff repair: analysis of technique and results at 2- and 3-year follow-up. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 1998;14:45–51. [DOI] [PubMed] [Google Scholar]
- 42.Thal R A technique for arthroscopic mattress suture placement. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 1993;9:605–607. [DOI] [PubMed] [Google Scholar]
- 43.Thawrani DP, Feldman DS, Sala DA. Current Practice in the Management of Slipped Capital Femoral Epiphysis. Journal of pediatric orthopedics 2016;36:e27–37. 10.1097/bpo.0000000000000496 [DOI] [PubMed] [Google Scholar]
- 44.Vitale MG, Krant JJ, Gelijns AC, Heitjan DF, Arons RR, Bigliani LU et al. Geographic variations in the rates of operative procedures involving the shoulder, including total shoulder replacement, humeral head replacement, and rotator cuff repair. The Journal of bone and joint surgery American volume 1999;81:763–772. [DOI] [PubMed] [Google Scholar]
- 45.Weinstein JN, Bronner KK, Morgan TS, Wennberg JE. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health affairs (Project Hope) 2004;Suppl Variation:Var81–89. 10.1377/hlthaff.var.81 [DOI] [PubMed] [Google Scholar]
- 46.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States' trends and regional variations in lumbar spine surgery: 1992-2003. Spine 2006;31:2707–2714. 10.1097/01.brs.0000248132.15231.fe [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wennberg J, Gittelsohn. Small area variations in health care delivery. Science (New York, NY) 1973;182:1102–1108. [DOI] [PubMed] [Google Scholar]
- 48.Zmistowski BPEMHMAJW, Gerald Jr; Namdari Surena. Trends and Variability in the Use of Total Shoulder Arthroplasty for Medicare Patients. J Am Acad Orthop Surg 2018;26:133–141. doi: 10.5435/JAAOS-D-16-00720. [DOI] [PubMed] [Google Scholar]