Despite impressive efforts from tribal communities to support and improve tribal members’ health, disparities in multiple physical, mental, and behavioral health outcomes among American Indian and Alaska Native (AI/AN or Native) populations persist, including disproportionate risk of experiencing intimate partner violence (IPV; Rosay, 2016). Broadly defined, IPV can include physical violence, sexual violence, stalking, and psychological aggression by a current or former intimate partner – a spouse, boyfriend/girlfriend, dating or ongoing sexual partner (Breiding, Basile, Smith, Black, & Mahendra, 2015). In the most recent and largest national survey reporting data on IPV among Native peoples, researchers found that Native women were 1.6 times more likely to have experienced intimate partner physical violence and 1.3 times more likely to have experienced psychological aggression by an intimate partner compared to non-Hispanic Whites (Rosay, 2016). Similarly, Native men were 1.4 times more likely to have experienced intimate partner physical violence and psychological aggression by an intimate partner in their lifetimes in comparison to non-Hispanic White men (Rosay, 2016). While the vast majority of research indicates that AI/AN populations experience more IPV when compared to non-Native groups, much of this work does not discern regional and tribal differences among AI/AN people in the United States. When data from AI/AN individuals representing diverse regions and tribes are combined, it may mask differences relevant to prevention and intervention efforts. Moreover, many tribal nations lack epidemiological data specific to their region or tribe. One aim of this study is to offer data from a particular region to build a body of evidence on the impact of IPV among tribal nations in the United States.
Intimate Partner Violence and Health
Physical health outcomes associated with IPV include injury, chronic pain, gastrointestinal issues, activity limitations, stroke, and chronic disease (Campbell, 2002; Centers for Disease Control and Prevention [CDC], 2008; Coker et al., 2002a). Increased rates of depression and depressive symptoms, chronic mental illness, and post-traumatic stress disorder have been noted among women and men who report experiencing IPV (Bonomi et al., 2006; Campbell, 2002; Coker et al., 2002a). Increased health risk behaviors such as smoking, substance use, heavy or binge drinking, are also associated with IPV (CDC, 2008; Coker et al., 2002a; Nemeth, Bonomi, Lu, Lomax, & Wewers, 2016). Little empirical research has documented these associations among AI/AN women and to our knowledge, researchers have not examined health outcomes of IPV for AI/AN men. We examine associations between IPV and health status among a sample of Ojibwe women and men in the upper Midwest diagnosed and living with type 2 diabetes. We also aim to contribute to the current knowledge of culturally-relevant stress buffers that may reduce negative health outcomes among those who experience IPV.
Indigenist Stress-Coping Model
Stress-coping models generally seek to understand the pathways whereby stressors and negative health outcomes are mediated or moderated by internal or external factors (Dinges & Joos, 1988). The indigenist stress-coping model incorporates social, historical, and structural contexts in the interpretation of epidemiological evidence of AI/AN health disparities – drawing attention to differential exposures and impact of stressors in this population rooted in the settler colonial history of the United States. For example, in work examining AI women’s attitudes toward domestic violence, Tehee and Esqueda (2008) pointed out that many tribes were matrilocal and matrilineal. The authors described the many powers Native women held within families and communities, describe historical community responses to domestic violence, ultimately suggesting that the introduction of European legal and educational systems stripped Native women of much of this power and eliminated traditional practices that discouraged domestic violence (Tehee & Esqueda, 2008). While AI/AN women retain family and community power and esteemed roles within tribal communities, analyses such as Tehee and Esqueda’s (2008) detail impacts of settler colonialism on Indigenous communities in the United States and remind us to consider this context in understanding disproportionate rates of victimization among this population. The moderation model tested in this article is conceptually guided by the indigenist stress-coping model which suggests that health outcomes among AI/AN populations may be moderated by tribally-specific collective and personal factors to buffer the effects of traumatic stressors such as IPV (Walters & Simoni, 2002; Walters, Simoni, and Evans-Campbell, 2002). Using a modified indigenist stress-coping model (Figure 1), we tested the potential buffering effects of communal mastery and social support on relationships between IPV and negative health outcomes.
Figure 1.

Modified Indigenist Stress-Coping Model (Walters, Simoni, & Evans-Campbell, 2002)
Communal Mastery and American Indian Communities
Mastery can be broadly understood as the extent to which people believe they can or do control circumstances or forces in their lives, often in the context of responding to stressors or overcoming life challenges (Hobfoll, Jackson, Hobfoll, Pierce, & Young, 2002; Pearlin, Menaghan, Lieberman & Mullan, 1981). In contrast to self-mastery, which focuses on individuals’ real or perceived abilities to overcome obstacles or control life circumstances based on individual efforts, communal-mastery has been defined as the real or perceived sense by individuals that they can overcome challenges because of their location within a social network or community (Hobfoll et al., 2002). Research on communal mastery measures the level to which one believes that being part of a community results in successful navigation of life’s challenges.
Collectivist cultures, including many AI/AN cultures, have been described as those which emphasize and promote relationships between individuals and promote reliance on the social group (Hobfoll et al., 2002). Community connectedness has long been theorized as an important aspect of Indigenous cultures and a potential protective factor in mental and behavioral health research (Hill, 2009; Schultz et al., 2016). In previous research examining connectedness (defined as the “interrelated welfare” of the individual with their family, community, and natural environment) as a culturally-based protective factor for Alaska Native youth, researchers reported that the measure of connectedness was highly correlated with a measure of communal mastery (Mohatt, Fok, Burket, Henry, & Allen, 2011). In a study of Native women in Montana, researchers found communal mastery to be associated with lower depressive mood, particularly in high stress circumstances (Hobfoll et al., 2002). Consistent with the indigenist stress-coping model call for identifying culturally-specific stress buffers, communal mastery may be a culturally-relevant measure for identifying aspects of community connectedness as protective factors among AI/AN populations. This work examines communal mastery as a possible moderator in the relationships between IPV exposure and health outcomes.
Social Support
Social support – the emotional and instrumental efforts offered to individuals during their life – has been extensively documented as a general protective factor or buffer in cases of adult IPV (Branch, 2008; Carlson, McNutt, Choi & Rose, 2002; Coker, Watkins, Smith & Brandt, 2003; Klein & Milardo, 2000; Kocot & Goodman, 2003; Larance & Porter, 2004). Research has suggested that women with more friends are more likely to disclose abuse (Browning, 2002) and those with more social support have more resources when deciding to leave abusive relationships (Van Wyk, Benson, Fox, & DeMaris, 2003). Research has also suggested that social support may be more effective in buffering impacts of lower level abuse when compared to higher levels of abuse (Carlson et al., 2002; Beeble, Bybee, Sullivan & Adams, 2009). In other findings, receiving social support from family members was associated with lower prevalence and less severe IPV, while social support from friends was related to more severe IPV but demonstrated no relationship to prevalence of IPV (Wright, 2015). This work further suggests the effect of social support may be weakened in areas of high disadvantage (Wright, 2015). These compelling but sometimes discordant findings suggest the need for more research on the relationship between social support and IPV.
Social support has been shown to reduce and/or mitigate health problems associated with violent relationships. In a study examining well-being among IPV survivors, social support was negatively associated with depression, positively related to quality of life, and moderated the impact of IPV on quality of life (Beeble et al., 2009). Other research has demonstrated better physical and mental health and lower psychological distress and depression for participants reporting higher levels of social support compared to participants reporting lower level of social support among women utilizing IPV services (Kamimura, Parekh, & Olson, 2013). Similarly, researchers from another study reported that among women reporting any lifetime IPV, those who reported low or moderate social support were more likely to be depressed than women who reported high levels of social support (Mburia-Mwalili, Clements-Nolle, Lee, Shadley, & Yang, 2010).
A smaller body of work has examined social support among AI/AN populations and findings mirror those among non-AI/AN populations such that greater social support was associated with a variety of better health outcomes. Although not specific to IPV, researchers examining health outcomes among Indigenous Canadians found that social support was a strong determinant of thriving health, particularly for women (Richmond, Ross, & Egeland, 2007). Greater social support has also been associated with lower levels of substance use disorders among AI women (Oetzel, Duran, Jiang, & Lucero, 2007). We seek to further this line of research by examining the role social support plays in the relationships between IPV and health outcomes in the communities under study.
Present Study
Primary objectives of the study were to (a) determine if IPV was significantly associated with three health outcomes – mental health (using a measure of depressive symptoms), physical health (health conditions frequently co-occurring with type 2 diabetes), and substance misuse (drug abuse); (b) determine associations between IPV, health outcomes, social support, and communal mastery; and (c) assess whether relationships between IPV and health outcomes were moderated by social support or communal mastery. Guided by the literature, we hypothesized that (a) experiencing IPV would be related to higher depressive symptoms, poorer physical health, and more drug abuse; (b) higher social support and communal mastery would be associated with less IPV, fewer depressive symptoms, better physical health, and fewer drug abuse; and (c) social support and communal mastery would buffer the effects of IPV on associated health outcomes.
Research Design and Methods
Data Sources and Procedures
Data are from the Maawaji’ idi-oog Mino-ayaawin (Gathering for Health) study, a mixed-method community-based participatory research collaboration between five Ojibwe communities and research partners at the University of Minnesota, University of Nebraska-Lincoln, and Oklahoma State University. All five communities provided tribal government resolutions and tribal clinics granted letters to support the project. Project planning and implementation was done collaboratively between university research and community research councils in place at each participating site. The study received approval from the University of Minnesota and Indian Health Service National Institutional Review Boards. Overall goals of the Gathering for Health study were to improve the measurement and understanding of stress processes among Ojibwe adults, as well as the understanding of interactions between stress processes, health outcomes and health behaviors including type 2 diabetes treatment adherence and disease management. Data are from the baseline quantitative phase of the study collected from surveys administered by computer-assisted personal interviews.
Study Sample
Each of the five tribal communities partnering in this research have reservation health care facilities. At the beginning of four sequential 6-month recruitment periods from 2013 to 2015, trained clinic staff at each site randomly selected patients from clinic records. Clinic staff established a sampling frame by creating a list of individuals 18 or older with a diagnosis of diabetes documented in the electronic medical record within the last 2 years. Additional inclusion criteria included self-identification as American Indian. A total of 344 individuals were sampled. Of those sampled, 43 did not meet inclusion criteria, 11 were unable to be contacted, and 96 declined participation. The baseline study response rate was 67%, with 194 providing consent to participate; the current study includes data from the 192 participants from which survey interviews were completed.
Clinic staff mailed a study invitation letter, study brochure, and both telephone and prepaid mail-in options for refusal to randomly selected patients. Interviewers contacted non-refusing individuals to screen for study eligibility. Participants underwent a formal consent process and completed HIPAA authorization forms to permit clinical chart reviews. Surveys were administered in a location of the participants’ choice, and each participant received a $50 incentive for completion of the survey. Consistent with cultural norms, a small traditional gift of wild rice was also provided. Interviewers transmitted the encrypted survey data electronically to secure servers, where it was converted to data files and cleaned by university partners.
Measurement
All survey measures in this research underwent a review process with Community Research Council (CRC) members and adaptations were made to ensure items were relevant to community members with diabetes and culturally appropriate. Three major dependent variables were included in the analyses. Depressive symptoms were assessed using a continuous scoring of the Patient Health Questionnaire (PHQ-9; Spitzer, Kroenke & Williams, 1999), a widely used 9-item screener of depressive symptoms experienced in the past 2 weeks. Cronbach’s alpha for the PHQ-9 in this sample = .88. Comorbidities are a measure of physical health conditions frequently co-occurring with type 2 diabetes. Participants were asked to self-report co-occurring cardiovascular (e.g., high blood pressure, angina, history of heart attack, etc.), ocular (e.g. retinopathy, macular degeneration, etc.), urinary (e.g., kidney failure, protein in urine, etc.) or circulatory (e.g., gangrene, peripheral vascular disease, foot ulcers, etc.) problems. In addition to self-reports, diagnoses for these same conditions were documented through clinical chart reviews. The variable comorbidities is scored such that an affirmative indication of diagnosis from either survey or chart reviews for each category of comorbidities was scored 1, and a negative response scored 0. As such, the final variable for comorbidities in the current analyses includes a possible range from 0 to 4. The last dependent variable, Drug abuse, was measured using the DAST-10 (Skinner, 1982) which includes 10 items assessing drug abuse/misuse and social, legal, or medical problems related to drug use during the past 6 months. Each item of the index was coded 0 for ‘no’ responses and 1 for ‘yes,’ with a possible range from 0 – 10 where higher values represent more severe drug related problems; Cronbach’s alpha for this measure = .67.
Intimate partner violence was measured using an adaptation of the Composite Abuse Scale (Hegerty, et al., 2005), a comprehensive measure of current or most recent (for those not currently in a relationship) partner abuse. Physical, sexual, and emotional abuse domains are represented in the measure with 13 individual items coded 0 for ‘never’ or 1 for ‘at least once’ answers, then summed for a continuous measure of current/recent IPV used in bivariate and multivariate analyses (Cronbach’s alpha = .86). Following the three abuse domains outlined in the original scale, we categorized the 13 items into physical, sexual, and emotional abuse categories for descriptive analyses.
Two potential protective factors were also assessed. Social support was assessed by 8 items adapted from the two-way social support scale, utilizing those items indicating receipt of perceived emotional and instrumental support (Shakespeare-Finch & Obst, 2011). Responses are coded so that higher values correspond to more support received (Cronbach’s alpha = .89). Communal mastery includes four items from the multicultural mastery scale (Fok, Allen, Henry & Mohatt, 2012) indicating degree of agreement with items assessing problem solving through social and familial networks. Likert-type response options were coded to range from 0 (strongly disagree) to 3 (strongly agree), with higher values thus indicative of a stronger sense of communal mastery (Cronbach’s alpha = .78).
Given robust evidence of gender disparities in mental health (e.g., Eaton et al., 2012), established associations between education and health (e.g., Phelan, Link, & Tehranifar, 2010), and because older participants would likely report higher prevalence and more advanced health issues, we also controlled for three demographic factors. Age was assessed by self-report age in years, gender was coded 0 = male, 1 = female, and educational attainment was coded such that 0 = less than high school diploma, 1 = high school diploma or GED, 2 = some college, and 3 = college graduate or advanced degree. Although most research on IPV has focused on women, given the disproportionate risk of IPV among AI/AN men in comparison to non-Hispanic White men (Rosay, 2016) and to be mindful of sample size, men and women were included in the analysis.
Data Analysis
Data were analyzed in SPSS (v. 24). Descriptive statistics (means, standard deviations) were generated for all study variables and Pearson correlation coefficients were calculated to identify bivariate associations among variables. Ordinary Least Squares (OLS) regression models were employed for multivariate models. We ran numerous diagnostic tests to assess possible violations of regression assumptions for these models. Most of the correlations between variables were quite modest in effect size, and all VIF values were less than 10 indicating no issues with multicollinearity. Examination of scatterplots of residuals revealed possible heteroscedasticity for one outcome (comorbidities); thus, we used a robust estimator for those models using Stata (v. 13). Multiplicative interaction terms were created for IPV × social support and IPV × communal mastery for tests of moderation (buffering).1
Results
Table 1 displays frequency of IPV across physical, sexual and emotional abuse domains by gender. A little over 45% of the total sample (48% women; 43% men) reported at least one IPV experience with their current or most recent partner. While women reported more IPV than men across all abuse categories, this gender difference was statistically significant only in the case of physical abuse (p < .10; two-tailed test).
Table 1.
Frequency of Self-Reported Intimate Partner Violence (Current/Most Recent Partner)
| Total | Male | Female | |
|---|---|---|---|
| % (N) | % (N) | % (N) | |
| Physical Abuse | 22.5 (39) | 16.0 (12) | 27.6* (27) |
| Sexual Abuse | 2.9 (5) | 1.3 (1) | 4.1 (4) |
| Emotional Abuse | 44.3 (77) | 42.1 (32) | 45.9 (45) |
| Any of the Above | 45.9 (80) | 43.4 (33) | 47.9 (47) |
Difference between men and women;
p = .07; two-tailed test
Over half of the study sample was female (55.7%) and the mean age of participants was 46.3 years. The mean value of 1.55 for education indicates that most participants had earned between a high school diploma or GED and some college completion. Additional descriptive statistics and bivariate correlations for all study variables are displayed in Table 2. Participants who were older were more likely to report physical health comorbidities and females more likely to report depressive symptoms than males. Higher IPV scores were positively associated with depressive symptoms, comorbidities, and drug abuse. Intimate partner violence was negatively associated with social support and communal mastery. Receiving social support was negatively associated with depressive symptoms and drug abuse, and communal mastery and depressive symptoms were inversely correlated.
Table 2.
Descriptive Statistics and Bivariate Associations for All Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 1 | ||||||||
| 2. Gender (Female = 1) | .03 | 1 | |||||||
| 3. Education | .11 | .13 | 1 | ||||||
| 4. IPVa | −.05 | .12 | .07 | 1 | |||||
| 5. Depressive Symptoms | −.09 | .19** | −.04 | .33*** | 1 | ||||
| 6. Comorbidities | .26*** | .05 | .17* | .23** | .11 | 1 | |||
| 7. Drug Problems | −.11 | −.14 | .00 | .22** | .14 | −.02 | 1 | ||
| 8. Social Support | −.00 | .08 | .16* | −.20** | .39*** | −.06 | −.21** | 1 | |
| 9. Communal Mastery | .00 | .08 | .18* | −.18* | −.23** | −.11 | −.12 | .42*** | 1 |
| Mean (S.D) % | 46.3 (12.2) | 55.7%% | 1.55 (.91) | 3.22 (5.5) | 5.27 (5.6) | 1.44 (.82) | .52 (1.3) | 2.24 (.68) | 2.24 (.53) |
p </= .001;
p </= .01;
p</= .05;
two-tailed tests; values are Pearson’s correlation coefficients;
intimate partner violence
Results of ordinary least squares regression analyses are displayed in Table 3. After controlling for age, gender, and educational attainment, IPV was positively related to adverse health status across all three dependent variables (depressive symptoms, comorbidities, and drug abuse). Social support was negatively associated with depressive symptoms and drug abuse. Communal mastery was not significantly related to any of the outcomes in these multivariate models. Adjusted R2 values demonstrate that the models explained between 7% and 27% of the variance in outcomes, with the greatest proportion of variance explained for depressive symptoms.
Table 3:
Ordinary Least Squares Regression of Adverse Health Status on Intimate Partner Violence Exposure and Protective Factors
| Depressive Symptoms | Comorbidities | Drug Problems | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β | |
| (Constant) | 5.61 | 5.91 | .41 | .40 | 1.30 | 1.32 | ||||||
| Age (years) | −.03 (.03) | −.06 | −.03 (.04) | −0.06 | .02* (.01) | .27*** | 0.02 (.00) | .27*** | −.01 (.01) | −.11 | −.01 (.01) | −.12 |
| Gender | 2.23 (.76) | .20*** | 2.20 (.82) | .19*** | .02 (.12) | .01 | .03 (.12) | .02 | −.46 (.21) | −.17** | −.42 (.21) | −.15** |
| Educational Status | −.28 (−.43) | −.05 | −.48 (−.46) | −0.08 | .10 (.06) | .11 | .11 (.06) | .12 | .07 (.11) | .04 | .05 (.12) | .04 |
| Intimate Partner Violence | 0.21 (.07) | .20*** | 0.27 (.08) | .25*** | 0.03 (.01) | .23*** | 0.03 (.01) | .22** | 0.05 (.02) | .20*** | 0.05 (.02) | .20** |
| Social Support | −2.61 (.57) | −.32* | −.01 (.09) | −.01 | −.41 (.16) | .20** | ||||||
| Communal Mastery | −1.20 (0.84) | −.11 | −.14 (.12) | −.09 | (−.11) (.21) | −.04 | ||||||
| IPV × Social Support | −.19 (−.07) | −.18** | −.01 (.01) | −.04 | .03 (.02) | .10 | ||||||
| IPV × Communal Mastery | −.15 (−.10) | −1.48 | .001 (.02) | .004 | −.03 (.03) | −.11 | ||||||
| R2 | 0.30 | 0.18 | 0.15 | 0.15 | 0.12 | 0.10 | ||||||
| Adjusted R2 | 0.27 | 0.15 | 0.11 | 0.12 | 0.09 | 0.07 | ||||||
p </= .001
p </= .01
p</= .05;
two-tailed tests; B = unstandardized coefficient; β = Beta; SE = standard error
One of the multiplicative interaction effects was significant in the regression models (p < .01). In Model 1, social support moderated the effects of IPV on depressive symptoms and is plotted in Figure 2. As can be seen, depressive symptoms were greatest for those reporting higher levels of IPV and low levels of social support. Regardless of IPV exposure, those participants reporting high levels of social support displayed fewer depressive symptoms than those with lower social support.
Figure 2.
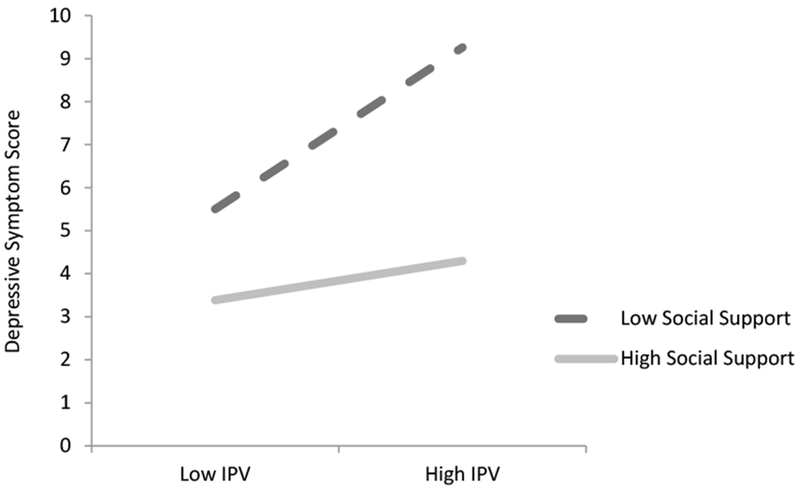
Depressive Symptom Scores by IPV and Social Support Status
Discussion
This is the first study of which we are aware to examine IPV, health outcomes, and social support and communal mastery among a sample of Ojibwe adults. It is one of the few studies of IPV prevalence among AI/AN populations to include men and offers regionally-specific findings that contribute to our knowledge of tribal and regional differences in IPV prevalence and health outcomes. Findings support previous research among non-Ojibwe populations by demonstrating relationships between IPV and adverse health outcomes among Ojibwe women and men. As expected, higher levels of IPV were significantly associated with higher depressive symptoms, more comorbidities and greater drug abuse. Additionally, IPV prevalence was inversely associated with social support and communal mastery. Our hypotheses that social support would moderate relationships between IPV and health outcomes was supported only for the relationship between IPV and depressive symptoms. However, a stratified analysis by social support was beyond the scope of this study. Communal mastery demonstrated no buffering effect in any of the models.
Intimate Partner Violence and Health Outcomes
While variability in sampling strategies and measures warrant caution in comparisons with other studies, a comparison of IPV prevalence reported by participants’ in their current or most recent relationships and lifetime rates of IPV reported by AI/AN women and men in in the latest national survey suggest that participants in this study may be at lower risk of IPV than in other communities (Rosay, 2016). This is also true when compared to community or reservation-based samples – lifetime estimates of IPV in published studies using community-based samples range from 59 – 87% prevalence (Bohn, 2003; Duran et al., 2009; Malcoe, Duran & Montgomery, 2004; Wood & Magen, 2009).
The impact of IPV on AI survivors’ lives has wide reaching implications. Results of this study suggest that IPV, as a traumatic stressor, lessens the quality of life among our population. Increased depression, health conditions associated with type 2 diabetes (cardiovascular, ocular, urinary and circulatory) and drug abuse are indicators that the impact of IPV extends beyond the acts of violence in their lives.
Social Support and Communal Mastery
While communal-mastery implies that one’s ability to confront life challenges and individual efficacy is rooted in involvement with the social group, social support relates to reported attachment to the social group (Hobfoll et al., 2002). Although related, these concepts differ slightly (e.g. an individual can rely heavily on social support from a group while simultaneously reporting low levels of personal efficacy) and may help us understand the differential effects of social support and communal mastery within this population. Lower social support or communal mastery may be found among individuals at higher risk for IPV and experiencing IPV may result in feelings of diminished communal mastery. Individuals may be more likely to draw on social support networks following victimization if those networks are considered available and helpful. Alternately, individuals may avoid or disengage from social networks because of shame, stigma, or perceived unavailability and unhelpfulness.
Another possible explanation for our findings may be related to the social conditions of participants’ communities. As noted in the introduction, AI/AN communities live within a unique sociohistorical context with attendant social and health disadvantages due to ongoing settler colonialism. Previous research has suggested that social support may be mitigated depending on a survivor’s neighborhood context such that survivors in disadvantaged neighborhoods may be more likely to live within a landscape of social isolation and greater tolerance of violence (Wright, 2015). Indeed, Wright (2015) found the effect of social support on IPV was diminished in more disadvantaged neighborhoods and suggests that social support is less relevant in disadvantaged areas. While our findings suggest overall positive relationships between social support and health outcomes, if “disadvantage” is conceptualized as the social and health challenges facing tribal communities due to contemporary disruptions to tribal health behaviors, protective factors, and healing practices, we may see similar effects in this and other tribal populations. Communal mastery was associated with less IPV and fewer depressive symptoms and social support was associated with less IPV and fewer depressive symptoms and drug abuse. These findings suggest that communal mastery and social support may protect individuals from some of the negative health outcomes associated with IPV, but not strengthen or weaken the relationships between IPV and all health outcomes as suggested by moderation effect in the current study.
Limitations
Given that participants were sampled from a group of individuals seeking care for type 2 diabetes, this sample may be (a) skewed toward individuals aware of and seeking to improve their health status or (b) individuals at higher risk for poor negative health outcomes related to living with type 2 diabetes. Furthermore, we cannot be certain that these IPV rates are reflective of other members of these tribal communities. The study sample is limited to Ojibwe reservations in the northern Midwest so national generalizability is limited due to the diversity of tribal communities in the United States. Another potential limitation related to sample size is the inability to examine men and women’s experiences separately beyond bivariate analyses. As with most research on sensitive subjects such as IPV or substance misuse there is a risk of participant unwillingness to be truthful about their experiences or behaviors. This may result in underreporting and underestimation of associations in the current study. Furthermore, because the measure of IPV asked about experiences with a current or most recent partner we cannot capture differential effects on outcomes or relationships to other variables based on if the IPV has occurred in their current relationship or a relationship in the recent or long ago past. We are also unable to assess for frequency or duration of IPV to identify differential effects or associations with outcomes and moderators.
Implications for Services
The development of Post-Traumatic Stress Disorder and other mental health or psychiatric disorders such as depression or anxiety are highly correlated with IPV (Bonomi et al., 2006; Campbell, 2002; Coker et al., 2002a) and with risk factors for developing type 2 diabetes such as cardiovascular disease (Libby, Orton, Novins, Beals, & Manson, 2005). Stress has been associated with both the onset of type 2 diabetes (Surwit, Schneider, & Feinglos, 1992) and worse diabetes-related outcomes including reduced capacity for disease management, increased risk of complications and comorbidities, and reductions in metabolic control and quality of life (Jiang et al., 2008; Walders-Abramson et al., 2014). Among respondents in the national Nurses Health Study II, the experience of physical IPV more than one time was associated with an 18% increase in type 2 diabetes and severe psychological IPV was associated with an almost 80% increased risk in type 2 diabetes (Mason et al, 2013). This study demonstrated a buffering effect of social support on depressive symptoms – therapeutic and interventive services for IPV or diabetes should include efforts to increase social support. Given the disproportionate burden of diabetes in AI/AN communities, medical services should integrate treatment options for IPV to reduce associated health burdens that may complicated diabetes onset and care. Finally, our findings support prior recommendations for increased and better IPV screenings in clinical care settings (Mason et al., 2013).
Directions for Future Research
Future research should examine the interplay of social support and communal mastery to investigate how they converge or diverge on their respective influence on both risk for IPV and the ability to buffer effects of traumatic stressors on health outcomes. Examinations of the various mechanisms whereby social support or communal mastery exert influence are nascent among this population and attention to the unique settler colonial context of AI/AN health should be prioritized in this research. Collective and intergenerational experiences of trauma should be examined in concert with individual or family level violence such as IPV to examine for differential relationships to social support and community mastery. Of particular importance to the population of this study, more research on the mechanisms by which IPV may influence type 2 diabetes risk should be explored as well as research on the long-term effects of IPV on this and other chronic diseases. Given the negative effects of IPV on all health outcomes in this study, the identification of stress buffers other than social support should be investigated in future research to develop more effective IPV services. Due to the lack of significant moderating effects of social support and communal mastery on most health outcomes in the current study, other theoretical perspectives on social connectedness among this population should be explored in future work.
Most research on IPV among AI/AN populations has focused on women, although some studies suggest elevated risk among AI/AN men when compared to the general population (Rosay, 2016). However, findings suggesting gender parity in IPV prevalence has been controversial. While most studies have found that women are more likely to be victimized, injured, and fearful as a result of IPV (Hamberger & Larsen, 2015; Rosay, 2016; Tjaden & Thoennes, 2000), and that men are far more likely to perpetrate violence (Hamby, 2014), others have called for more work on bidirectional violence within intimate relationships (Bates, 2016). Indeed, this study found that although women reported more IPV across types, the only statistically significant gender difference was for physical abuse. Future research should examine gender differences in the prevalence of IPV, consequences of IPV, and roles of social support and communal mastery among this and other AI/AN populations and among those not currently living with type 2 diabetes.
Conclusion
This works builds on a body of work specific to American Indian populations that examines the ways in which individual’s health may be influenced by social connectedness, as measured through social support and communal mastery. Our findings suggest that social support may be protective against negative health outcomes among this population and corroborates previous scientific literature on the negative health outcomes related to IPV. Interventions seeking to increase social support may be an area in which to focus preventive and treatment efforts. Furthermore, preventive and interventive measures should be coordinated across multiple service areas including diabetes care, trauma treatment, and mental health services.
Acknowledgements:
The authors gratefully acknowledge the clinical and community-based members of the Gathering for Health Team: Sidnee Kellar, Rose Barber, Robert Miller, Tweed Shuman, Lorraine Smith, Sandy Zeznanski, Patty Subera, Tracy Martin, Geraldine Whiteman, Lisa Perry, Trisha Prentice, Alexis Mason, Charity Prentice-Pemberton, Kathy Dudley, Romona Nelson, Eileen Miller, Geraldine Brun, Murphy Thomas, Mary Sikora-Petersen, Tina Handeland, GayeAnn Allen, Frances Whitfield, Phillip Chapman, Sr., Sonya Psuik, Hope Williams, Betty Jo Graveen, Daniel Chapman, Jr., Doris Isham, Stan Day, Jane Villebrun, Beverly Steel, Muriel Deegan, Peggy Connor, Michael Connor, Ray E. Villebrun, Sr., Pam Hughes, Cindy McDougall, Melanie McMichael, Robert Thompson, and Sandra Kier.
Funding Information:
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number DK091250 (M. Walls, PI). Research effort support was also provided in part by National Institute of Mental Health under award number T32MH019960. The contents of this manuscript are attributable to the authors and do not necessarily represent the viewpoints of the NIH.
Footnotes
Based on statistical power calculations prior to launching the study suggesting that N = 200 cases were needed to perform more advanced analyses with multiple variables, we believe our sample size is sufficiently powered for these basic regression analyses.
Contributor Information
Katie Schultz, University of Michigan, School of Social Work.
Melissa Walls, University of Minnesota Medical School, Duluth campus.
Sheryl J. Grana, University of Minnesota-Duluth, Department of Anthropology, Sociology and Criminology
References
- Bates EA (2016). Current controversies within intimate partner violence: Overlooking bidirectional violence. Journal of Family Violence, 31(8), 937–940. doi: 10.1007/s10896-016-9862-7 [DOI] [Google Scholar]
- Beeble ML, Bybee D, Sullivan CM, & Adams AE (2009). Main, mediating, and moderating effects of social support on the well-being of survivors of intimate partner violence across two years. Journal of Consulting and Clinical Psychology, 77(4), 718–729. doi: 10.1037/a0016140 [DOI] [PubMed] [Google Scholar]
- Bohn DK (2003). Lifetime physical and sexual abuse, substance abuse, depression, and suicide attempts among Native American women. Issues in Mental Health Nursing, 24, 333–352. [DOI] [PubMed] [Google Scholar]
- Bonomi AE, Thompson RS, Anderson M, Reid RJ, Carrell D, Dimer JA, & Rivara FP (2006). Intimate partner violence and women’s physical, mental, and social functioning. American Journal of Preventive Medicine, 30(6), 458–466. doi: 10.1016/j.amepre.2006.01.015 [DOI] [PubMed] [Google Scholar]
- Branch KA (2008). The role of social support in the use of intimate partner violence: An exploration of the role of social support in heterosexual women’s use of non-lethal intimate partner violence. Saarbrucken, Germany: VDM Verlag Dr. Muller Aktiengesellshaft. [Google Scholar]
- Breiding MJ, Basile KC, Smith SG, Black MC, & Mahendra RR (2015). Intimate partner violence surveillance: Uniform definitions and recommended data elements, version 2.0. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Browning CR (2002). The span of collective efficacy: Extending social disorganization theory to partner violence. Journal of Marriage & Family, 4, 833–850. [Google Scholar]
- Campbell JC (2002). Health consequences of intimate partner violence. Lancet, 359(9314), 1331–1336. doi: 10.1016/s0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- Carlson B, McNutt L, Choi D, & Rose I (2002). Intimate partner abuse and mental health: The role of social support and other protective factors. Violence Against Women, 8, 720–745. [Google Scholar]
- Centers for Disease Control and Prevention. (2008). Adverse health conditions and health risk behaviors associated with intimate partner violence—United States, 2005. Morbidity and Mortality Weekly Report, 57(5), 113–117. [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, & Smith PH (2002). Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine, 23(4), 260–268. [DOI] [PubMed] [Google Scholar]
- Coker A, Watkins K, Smith P, & Brandt H (2003). Social support reduces the impact of partner violence on health: Application of structural equation models. Preventive Medicine, 37, 259–267. [DOI] [PubMed] [Google Scholar]
- Dinges DC, & Joos SK (1988). Stress, coping and health: Models of interaction for Indian and Native populations. American Indian and Alaska Native Mental Health Research, 1, 8–64. [DOI] [PubMed] [Google Scholar]
- Duran B, Oetzel J, Parker T, Malcoe LH, Lucero J, & Yizhou J (2009). Intimate partner violence and alcohol, drug, and mental disorders among American Indian women from Southwest tribes in primary care. American Indian & Alaska Native Mental Health Research: The Journal of the National Center, 16(2), 11–27. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, Grant BF, Hason DS, 2012. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. Journal of Abnormal Psychology, 121(1), 282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Campbell T (2008). Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence, 23(3), 316–338. doi: 10.1177/0886260507312290 [DOI] [PubMed] [Google Scholar]
- Fok CC, Allen J, Henry D, & Mohatt GV (2012). Multicultural mastery scale for youth: Multidimensional assessment of culturally mediated coping strategies. Psychologial Assessment, 24(2), 313–327. doi: 10.1037/a0025505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamberger LK, & Larsen SE (2015). Men’s and women’s experience of intimate partner violence: A review of ten years of comparative studies in clinical samples; part I. Journal of Family Violence, 30(6), 699–717. doi: 10.1007/s10896-015-9732-8 [DOI] [Google Scholar]
- Hamby S (2014). Intimate partner and sexual violence research: Scientific progress, scientific challenges, and gender. Trauma, Violence, & Abuse, 15(3), 149–158. doi: 10.1177/1524838014520723 [DOI] [PubMed] [Google Scholar]
- Hegarty K, Fracgp., Bush R, & Sheehan M. (2005). The composite abuse scale: Further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence and Victims, 20(5), 529–547. doi: 10.1891/vivi.2005.20.5.529 [DOI] [PubMed] [Google Scholar]
- Hill DL (2009). Relationship between sense of belonging as connectedness and suicide in American Indians. Archives of Psychiatric Nursing, 23(1), 65–74. doi: 10.1016/j.apnu.2008.03.003 [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Jackson A, Hobfoll I, Pierce CA, & Young S (2002). The impact of communal-mastery versus self-mastery on emotional outcomes during stressful conditions: A prospective study of Native American women. American Journal of Community Psychology, 30(6), 853–871. doi: 10.1023/a:1020209220214 [DOI] [PubMed] [Google Scholar]
- Jiang L, Roubideaux Y, Beals J, Manson SM, Whitesell NR, & The AI-SUPERPFP Team (2008). Stress burden and diabetes in two American Indian reservation communities. Diabetes Care, 31(3), 427–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamimura A, Parekh A, & Olson LM (2013). Health indicators, social support, and intimate partner violence among women utilizing services at a community organization. Women’s Health Issues, 23(3), e179–e185. doi: 10.1016/j.whi.2013.02.003 [DOI] [PubMed] [Google Scholar]
- Klein RCA, & Milardo RM (2000). The social context of couple conflict: Support and criticism from informal third parties. Journal of Social and Personal Relationships, 17(4–5), 618–637. [Google Scholar]
- Kocot T, & Goodman L (2003). The roles of coping and social support in battered women’s mental health. Violence Against Women, 9, 323–346. [Google Scholar]
- Larance L, & Porter M (2004). Observations from practice: Support group memberships a process of social capital formation among female survivors of domestic violence. Journal of Interpersonal Violence, 19, 676–690. [DOI] [PubMed] [Google Scholar]
- Libby AM, Orton HD, Novins DK, Beals J, & Manson SM (2005). Childhood physical and sexual abuse and subsequent depressive and anxiety disorders for two American Indian tribes. Psychological Medicine, 35 (3), 329–340. [DOI] [PubMed] [Google Scholar]
- Malcoe LH, Duran BM, & Montgomery JM (2004). Socioeconomic disparities in intimate partner violence against Native American women: A cross-sectional study. BMC Medicine, 2(1), 1–14. doi: 10.1186/1741-7015-2-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason SM, Wright RJ, Hibert EN, Spiegelman D, Jun H, Hu FB, & Rich-Edwards JW (2013). Intimate partner violence and incidence of type two diabetes in women. Diabetes Care, 36, 1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mburia-Mwalili A, Clements-Nolle K, Lee W, Shadley M, & Yang W (2010). Intimate partner violence and depression in a population-based sample of women: Can social support help? Journal of Interpersonal Violence, 25(12), 2258–2278. doi: 10.1177/0886260509354879 [DOI] [PubMed] [Google Scholar]
- Mohatt NV, Fok CCT, Burket R, Henry D, & Allen J (2011). Assessment of awareness of connectedness as a culturally-based protective factor for Alaska Native youth. Cultural Diversity & Ethnic Minority Psychology, 17(4), 444–455. doi: 10.1037/a0025456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemeth JM, Bonomi AE, Lu B, Lomax RG, & Wewers ME (2016). Risk factors for smoking in rural women: The role of gender-based sexual and intimate partner violence. Journal of Women’s Health, 25(12), 1282–1291. doi: 10.1089/jwh.2015.5640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oetzel J, Duran B, Jiang Y, & Lucero J (2007). Social support and social undermining as correlates for alcohol, drug, and mental disorders in American Indian women presenting for primary care at an Indian Health Service hospital. Journal of Health Communication, 12(2), 187–206. doi: 10.1080/10810730601152771 [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, & Mullan JT (1981). The stress process. Journal of Health and Social Behavior, 22(4), 337–356. doi: 10.2307/2136676 [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, & Tehranifar P (2010). Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior, 51(1_suppl), S28–S40. [DOI] [PubMed] [Google Scholar]
- Richmond CAM, Ross NA, & Egeland GM (2007). Social support and thriving health: A new approach to understanding the health of Indigenous Canadians. American Journal of Public Health, 97(10), 1827–1833. doi: 10.2105/ajph.2006.096917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosay AB (2016). Violence against American Indian and Alaska Native women and men: 2010 findings from the National Intimate Partner and Sexual Violence Survey. Retrieved from Washington, DC: https://www.ncjrs.gov/pdffiles1/nij/249736.pdf [Google Scholar]
- Schultz K, Cattaneo LB, Sabina C, Brunner L, Jackson S, & Serrata JV (2016). Key roles of community connectedness in healing from trauma. Psychology of Violence, 6(1), 42–48. [Google Scholar]
- Shakespeare-Finch J, & Obst PL (2011). The development of the 2-way social support scale: A measure of giving and receiving emotional ad instrumental support. Journal of Personality Assessment, 93(5), 483–490. doi: 10.1020/00223891.2011.594124 [DOI] [PubMed] [Google Scholar]
- Skinner HA (1982). The drug abuse screening test. Addictive Behaviors, 7(4), 363–371. doi: 10.1016/0306-4603(82)90005-3 [DOI] [PubMed] [Google Scholar]
- Solar O, & Irwin A (2010). A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). Retrieved from http://apps.who.int/iris/bitstream/10665/44489/1/9789241500852_eng.pdf?ua=1&ua=1 [Google Scholar]
- Spitzer RL, Kroenke K, & Williams JB (1999). Validation and utility of a self-report of PRIME-MD: The PHQ primary care study. Primary care Evaluation of mental disorders. Patient health questionnaire. JAMA 282(18), 1737–1744. doi: 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- Surwit RS, Schneider MS, & Feinglos MN (1992) Stress and diabetes mellitus. Diabetes Care, 15(10), 1413–1422. [DOI] [PubMed] [Google Scholar]
- Tehee M, & Esqueda CW (2008). American Indian and European Women’s perceptions of domestic violence. Journal of Family Violence, 23, 25–35. [Google Scholar]
- Tjaden P, & Thoennes N (2000). Extent, nature, and consequences of intimate partner violence: Findings from the National Violence Against Women Survey. NCJ 181867. Washington, DC: National Institute of Justice. [Google Scholar]
- Van Wyk J, Benson ML, Fox GL, & DeMaris AA (2003). Detangling individual-, partner-, and community-level correlates of partner violence. Crime & Delinquency, 49, 412–438. [Google Scholar]
- Walters KL, & Simoni JM (2002). Reconceptualizing Native women’s health: An “indigenist” stress-coping model. American Journal of Public Health, 92(4), 520–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KL, Simoni JM, & Evans-Campbell T (2002). Substance use among American Indians and Alaska Natives: Incorporating culture in an “Indigenist” stress-coping paradigm. Public Health Reports, 117(Suppl 1), S104–S117. [PMC free article] [PubMed] [Google Scholar]
- Walders-Abramson N, Venditti EM, levers-Landis CE, Anderson B, El Ghormli L, Geffner M, … Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) Study Group (2014). Relationships among stressful life events and physiological markers, treatment adherence, and psychosocial functioning among youth with type 2 diabetes. The Journal of Pediatrics, 165(3), 504–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood DS, & Magen RH (2009). Intimate partner violence against Athabaskan women residing in interior Alaska: Results of a victimization survey. Violence Against Women, 15(4), 497–507. doi: 10.1177/1077801208331245 [DOI] [PubMed] [Google Scholar]
- Wright E (2015). The relationship between social support and intimate partner violence in neighborhood context. Crime & Delinquency, 61, 1333–1359 [Google Scholar]


