Abstract
Hematological abnormalities and altered vascular permeability are frequently encountered in Dengue virus infected patients, but the mechanisms that alter platelet–endothelium interactions remain incompletely understood. The DENV NS1 protein has been implicated in adverse disease outcomes. In the present study the role of NS1 protein in affecting the expression of vWF and platelet adhesion properties of endothelial cells was studied in vitro. The results suggest that vWF is down regulated in cultured endothelial cells 6 and 24 h after exposure with increase in vWF levels in culture supernatants at corresponding time points. Ultrastructural studies showed distinct evidence of endothelial cell activation morphology and degranulation of Weibel-Palade bodies in NS1 exposed cells that also showed increased platelet activation physiology. The findings suggest that changes in vWF production and secretion may be induced in endothelial cells exposed to DENV NS1 protein; and play a role in bleeding complications of severe DENV disease.
Keywords: Endothelial cells, Dengue virus, von Willebrand factor, NS1
Dengue virus (DENV) is a mosquito borne Flavivirus of significant public health importance with approximately 390 million infections, 500,000 hospitalizations and 25,000 deaths attributed to the infection; as per recent global disease burden projections. In India, 7.5–32.5 million new infections are estimated to be occuring every year [1]. The clinical presentation of DENV can range from mild self-limiting febrile illness to severe life threatening forms with hemorrhage and shock termed Dengue Hemorrhagic Fever and Shock Syndrome (DHF/DSS) in a subset of cases. While hematological abnormalities like leucopenia and thrombocytopenia are frequently associated with DENV infection, the pathophysiology of vascular abnormalities remains incompletely understood. However, injury to the endothelium directly by virus infection or through indirect disease pathology has been suggested [2, 3]. Von Willebrand factor (vWF) is a high molecular weight protein synthesized and secreted by endothelial cells, platelets and megakaryocytes and is crucial for maintaining the normal hemostasis. The secreted vWF is prothrombotic and is responsible for platelet-endothelial interactions at sites of injury [4]. The high molecular weight form of vWF normally is cleaved to a circulating low molecular weight form by an enzyme; a disintegrin and metalloproteinase with a thrombospondin type motif 1, member13 (ADAMTS13). Changes in vWF homeostasis can adversely affect vascular and coagulation functions [5]. While abnormal variation in vWF have been reported in patients with DHF/DSS there is no clear evidence till date on the exact role of DENV in affecting endothelial cell vWF homeostasis.
The DENV non-structural protein-1 (NS1), in its soluble secreted hexameric form (sNS1) is found in sera of patients during acute illness; and high levels in sera correlate with disease severity. The protein has been found to increase endothelial permeability in vitro [6, 7]; but its effect on altering platelet–endothelium homeostasis is not known. In the present study we examined in vitro the effect of DENV-2 NS1 protein on endothelial cell vWF physiology.
To study the effect of DENV-2 NS1 exposure on endothelial cells; Human Umbilical vein endothelial cells (HUVEC, Lonza, USA) were cultured in endothelial cell growth medium-2 (EBM-2, Lonza, USA) and supplemented with SingleQuots™ growth factor kit (Lonza USA) as per manufacturer’s instructions. The cells were treated with recombinant DENV-2 NS1 protein expressed in HEK cells (Abcam, UK) at a concentration of 5 μg/ml [7]. Cell culture supernatants were harvested to measure vWF released by HUVECs using a quantitative ELISA test (Abcam, UK) as per the manufacturer’s instructions. Cell-lysates at corresponding time-points were harvested for immuno-blotting studies. Immuno-blotting was performed by a method described earlier [8]; and either anti-vWF rabbit polyclonal antibody (Abcam, UK), or anti-β-Actin rabbit polyclonal antibody (Sigma, USA) were used to detect vWF or β-Actin. To study the distribution and expression of vWF in HUVECs treated with DENV-2 NS1, immuno-fluorescence assay was performed as described earlier [9] with a rabbit polyclonal anti-vWF antibody (Abcam, UK). To elucidate the ultrastructure, HUVEC cells exposed to DENV 2 NS1 protein were harvested and fixed, dehydrated, embedded in EPON 812 blocks, sectioned and imaged under a 100 kV operating voltage Trans mission Electron microscope as described earlier [10]. Adhesion of platelets to DENV-2 NS1 exposed HUVEC was assayed by a method previously described [11], and areas of adhesion were counted microscopically.
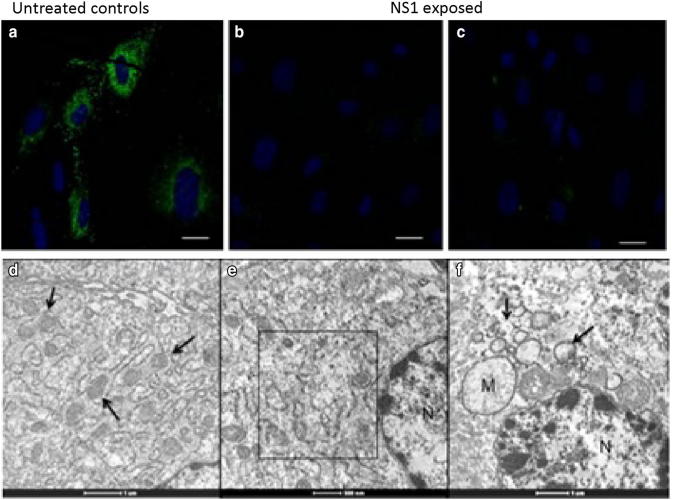
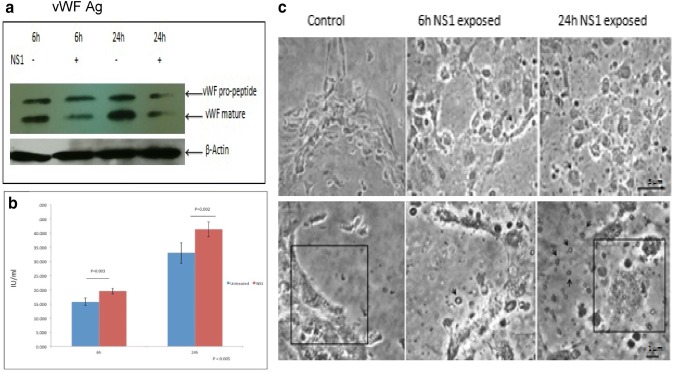
Exposure of the HUVECs to DENV-2 NS1 protein did not show any cytopathic effect on the cells. Immunofluorescence labeling of the cells for vWF antigen showed the typical appearance in most of the cells (Fig. 1a) while in cells exposed to the DENV 2 NS1 protein there was a marked reduction in the detectable vWF fluorescence (Fig. 1b, c) suggesting down-regulation. Assays of cell lysates by western blotting showed a similar change where cell associated vWF antigen showed a relative lower expression compared with the controls at 6 and 24 h post exposure (Fig. 2a). Both pro-vWF and mature vWF levels were found to be lower in DENV-2 NS1 treated cells compared to untreated controls. In comparison, the levels of soluble vWF from cell-culture media, showed a marked increase in cells treated with DENV-2 NS1 as compared to controls, at 6 and 24 h after exposure (Fig. 2b).
Fig. 1.
Effect of DENV 2 NS1 exposure on HUVEC vWF expression and ultrastructure. Representative micrographs showing typical appearance of vWF (arrows) in uninfected HUVEC cells (a) by IFA; and detectable reduction in vWF expression after 6 h (b) and 24 h (c) post NS1 exposure. Ultrastructure of cytoplasm in uninfected HUVEC showing presence of Wiebel-Palade bodies (arrows) that store vWF (d) and significant reduction in Wiebel-Palade bodies (e) as shown in box with evidence of cytoplasmic vacuolation (arrows) and mitochondrial swelling (M) (f) after 24 h of NS1 exposure. Magnification bars are built into the micrographs
Fig. 2.
Post exposure effect of DENV 2 NS1 shows a comparative reduction of the in vWF antigen in cell lysates (a) and statistically significant increase in the supernatant (b). In platelet-endothelial adhesion assays (c) there was a significant increase in presence of activated platelets both at 6 and 24 h post-exposure with increased adhesion when compared with the uninfected controls. Top panel shows low magnification images whereas bottom panel shows high magnification (c). Magnification bars are built into the micrographs
Endothelial cells have a well-defined ultrastructure that has been reported to show characteristic changes due to a variety of physiological and pathologic stimuli [12, 13]. A typical feature of these cells is the presence of elongated electron dense structures called Wiebel-Palade bodies (WPB) that store von Willebrand factor (Fig. 1d). There were distinct changes in the WPB morphology in the NS1 exposed cells along with cytoplasmic vacuolations and mitochondrial hypertrophy (Fig. 1e, f).
There was no evidence of either platelets attaching to HUVECs in abundance in the unexposed controls or presence of activated platelets (Fig. 2c). In contrast at both 6 and 24 h (Fig. 2c) post exposure time-points there was a significant increase in platelet adhesion and presence of morphologically activated platelets in the fields scanned.
Hematological abnormalities are frequent clinical presentation in dengue virus infection and in severe disease like DHF/DSS it can be fatal without timely clinical intervention. While thrombocytopenia and leucopenia are most common, hemorrhage, coagulopathies and capillary leakage with shock occurs in severe disease. Much of the pathophysiology of the dengue associated bleeding disorders remains incompletely understood. While the evidence for direct infection of endothelium by DENV is still evolving indirect injury to endothelial cells by immuno-pathogenic mechanisms of DENV disease pathology is the most relevant cause [14]. The findings from autopsy studies of DHF cases are interesting in this context [15, 16].
The changes in circulating plasma vWF in DENV infected patients have shown variable findings. In Dengue virus infected pediatric cases the elevation of vWF [17] and decrease in ADAMTS13 activity have been reported [18]. Elevated level of vWF was also reported in a small number of cases of Sudan virus infection [19] and cases of Hantavirus infection [20].
The role of DENV non structural protein NS1 has been associated with severe disease outcomes. This protein can be detected in the early stages of infection, is present as a hexamer with a lipid core and has also been shown to have multifaceted effects with immune and endothelial cells [21]. In our studies we exposed the endothelial cells to physiological doses of NS1 as described earlier and studied the vWF expression at post-exposure time points reported to be most effective with binding [7]. The dramatic reduction of detectable vWF in the exposed cells after 6 and 24 h was consistent with the ultrastructural observations. While in control cells, the vWF organization in Weibel Palade bodies was well defined; cells with NS1 exposure showed evidence of degranulation, cytoplasmic vacuolation and mitochondrial hypertrophy that suggests endothelial cell activation. This is an important observation as DENV NS1 has been reported to bind toll like receptors (TLR) on immune and endothelial cells activating signaling pathways that could affect barrier physiology [22]. The reduction in endothelial vWF with concomitant release in the media would also suggest possible engagement of signaling pathways linked to hemostatic function of these cells. This is consistent with the recent study of Puerta-Guardo et al. [7] that demonstrated exogenous exposure of DENV NS1 can alter endothelial cell permeability specifically by altering glycocalyx and expression of heparanase and sialidases.
The observation of enhanced platelet adhesion on NS1 exposed endothelial cells also suggests the physiological activation of these cells similar to earlier reports but the difference is that the earlier studies had shown this with virus-infected cells [11]. So if NS1 can directly induce a similar effect, its potential role in the in vivo disease biology and vascular injury acquires prominence. The screening for vWF levels in laboratory confirmed DENV cases might be of significant value as an additional hematological marker for disease severity.
In summary, regulation of endothelial cell vWF by DENV NS1 protein could be a fundamental event in the multifactorial etiology of endothelial injury in severe DHF/DSS and more focused studies on the analysis of in vitro cellular and molecular pathways underlying this effect can provide knowledge towards therapeutic interventions.
Acknowledgements
This work was supported by a Dengue Task Force grant from Department of Biotechnology-India. Nitali Tadkalkar is a graduate student supported by a Council for Scientific and Industrial Research Junior Research Fellowship.
Compliance with Ethical Standards
Ethical Statement
Platelets were obtained from healthy donors after obtaining written informed consent. The study was approved by the Institutional Ethics committee of the National Institute of Virology, Pune.
References
- 1.Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, et al. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dalrymple NA, Mackow ER. Endothelial cells elicit immune-enhancing responses to dengue virus infection. J Virol. 2012;86(12):6408–6415. doi: 10.1128/JVI.00213-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hottz ED, Lopes JF, Freitas C, Valls-de-Souza R, Oliveira MF, et al. Platelets mediate increased endothelium permeability in dengue through NLRP3-inflammasome activation. Blood. 2013;122(20):3405–3414. doi: 10.1182/blood-2013-05-504449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gragnano F, Sperlongano S, Golia A, Natale F, Bianchi R, et al. The role of von Willebrand factor in vascular inflammation: from pathogenesis to targeted therapy. Mediat Inflamm. 2017;2017:5620314. doi: 10.1155/2017/5620314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.South K, Lane DA. ADAMTS-13 and von Willebrand factor: a dynamic duo. J Thromb Haemost. 2018;16(1):6–18. doi: 10.1111/jth.13898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beatty PR, Puerta-Guardo H, Killingbeck SS, Glasner DR, Hopkins K, Harris E. Dengue virus NS1 triggers endothelial permeability and vascular leak that is prevented by NS1 vaccination. Sci Transl Med. 2015;7(304):304ra141. doi: 10.1126/scitranslmed.aaa3787. [DOI] [PubMed] [Google Scholar]
- 7.Puerta-Guardo H, Glasner DR, Harris E. Dengue virus NS1 disrupts the endothelial glycocalyx, leading to hyperpermeability. PLoS Pathog. 2016;12(7):e1005738. doi: 10.1371/journal.ppat.1005738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X, Sun H, Li Z, Zhang H, Yang W, et al. Gastric cancer-associated enhancement of von Willebrand factor is regulated by vascular endothelial growth factor and related to disease severity. BMC Cancer. 2015;15:80. doi: 10.1186/s12885-015-1083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Montali M, Panvini FM, Barachini S, Ronca F, Carnicelli V, et al. Human adult mesangiogenic progenitor cells reveal an early angiogenic potential, which is lost after mesengenic differentiation. Stem Cell Res Ther. 2017;8:106. doi: 10.1186/s13287-017-0562-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gangodkar S, Jain P, Dixit N, Ghosh K, Basu A. Dengue virus-induced autophagosomes and changes in endomembrane ultrastructure imaged by electron tomography and whole-mount grid-cell culture techniques. J Electron Microsc (Tokyo) 2010;59(6):503–511. doi: 10.1093/jmicro/dfq063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krishnamurti C, Peat RA, Cutting MA, Rothwell SW. Platelet adhesion to dengue-2 virus-infected endothelial cells. Am J Trop Med Hyg. 2002;66(4):435–441. doi: 10.4269/ajtmh.2002.66.435. [DOI] [PubMed] [Google Scholar]
- 12.Warhol MJ, Sweet JM. The ultrastructural localization of von Willebrand factor in endothelial cells. Am J Pathol. 1984;117:310–315. [PMC free article] [PubMed] [Google Scholar]
- 13.Mourik MJ, Faas FG, Valentijn KM, Valentijn JA, Eikenboom JC, Koster AJ. Correlative light microscopy and electron tomography to study von Willebrand factor exocytosis from vascular endothelial cells. Methods Cell Biol. 2014;124:71–92. doi: 10.1016/B978-0-12-801075-4.00004-5. [DOI] [PubMed] [Google Scholar]
- 14.Tadkalkar N, Ganti K, Ghosh K, Basu A. Pathogenesis of dengue associated haematological dysfunction. Dengue Bull. 2016;39:32–39. [Google Scholar]
- 15.Aye KS, Charngkaew K, Win N, Wai KZ, Moe K, et al. Pathologic highlights of dengue hemorrhagic fever in 13 autopsy cases from Myanmar. Hum Pathol. 2014;45(6):1221–1233. doi: 10.1016/j.humpath.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 16.Povoa TF, Alves AM, Oliveira CA, Nuovo GJ, Chagas VL, Paes MV. The pathology of severe dengue in multiple organs of human fatal cases: histopathology, ultrastructure and virus replication. PLoS ONE. 2014;9(4):e83386. doi: 10.1371/journal.pone.0083386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basuki PS. A glance at the von Willebrand factor in dengue virus infection. Southeast Asian J Trop Med Public Health. 2003;34(3):559–563. [PubMed] [Google Scholar]
- 18.Djamiatun K, van der Ven AJAM, de Groot PG, Faradz SMH, Hapsari D, et al. Severe dengue is associated with consumption of von Willebrand factor and its cleaving enzyme ADAMTS-13. PLoS Negl Trop Dis. 2012;6(5):e1628. doi: 10.1371/journal.pntd.0001628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McElroy AK, Erickson BR, Flietstra TD, Rollin PE, Towner JS, et al. Von Willebrand factor is elevated in individuals infected with Sudan virus and is associated with adverse clinical outcomes. Viral Immunol. 2015;28(1):71–73. doi: 10.1089/vim.2014.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laine O, Makela S, Mustonen J, Helminen M, Vaheri A, et al. Platelet ligands and ADAMTS13 during Puumala hantavirus infection and associated thrombocytopenia. Blood Coagul Fibrinolysis. 2011;22(6):468–472. doi: 10.1097/MBC.0b013e328346a420. [DOI] [PubMed] [Google Scholar]
- 21.Muller DA, Young PR. The flavivirus NS1 protein: molecular and structural biology, immunology, role in pathogenesis and application as a diagnostic biomarker. Antiviral Res. 2013;98(2):192–208. doi: 10.1016/j.antiviral.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 22.Modhiran N, Watterson D, Muller DA, Panetta AK, Sester DP, et al. Dengue virus NS1 protein activates cells via Toll-like receptor 4 and disrupts endothelial cell monolayer integrity. Sci Trans Med. 2015;7(304):304ra142. doi: 10.1126/scitranslmed.aaa3863. [DOI] [PubMed] [Google Scholar]