Abstract
Background
Social and legal acceptance of long-term same-sex partnerships in the United States has increased over the past decade which may impact sexual partnering among men who have sex with men (MSM). Identifying whether and how partnering trends have evolved at a national level could improve understanding of HIV transmission and prevention among MSM partnerships.
Methods
We used Centers for Disease Control and Prevention’s National HIV Behavioral Surveillance data (2008, 2011, and 2014) to study trends in the number and partner type composition (main/casual) of male sex partners among US MSM. Changes over time were assessed in Poisson regression models with the link function tailored to the count and binary outcomes.
Results
The mean total number of partners in the past year increased, while the mean number of main partners remained stable. The percentage of MSM with both main and casual partners increased, and we observed a shift from having ≥1 main and 0 casual partners to having ≥1 main and ≥2 casual partners. Condomless anal sex in the past year increased regardless of partner composition.
Discussion
Findings suggest casual partnering among MSM has increased in recent years, including among those with ≥1 main partners. Both partner-based and individual prevention programs remain critical to reaching MSM.
Keywords: HIV, MSM, partner type, partner number, condomless anal sex, trends
INTRODUCTION
Gay, bisexual, and other men who have sex with men (collectively referred to as MSM) are disproportionately affected by HIV and accounted for 70% of new HIV diagnoses in the United States in 2016.1 Estimates of HIV transmission among MSM have varied by main and casual partner type. For example, deterministic models have estimated that 68%–78% of HIV transmissions in MSM arise from main partnerships, likely driven by more condomless anal sex and higher sex frequency in main partnerships compared to casual partnerships.2,3 As a result, partner-based prevention interventions such as couples’ HIV testing and counseling (CHTC) have been introduced to help reduce HIV infections among MSM.4,5 Yet, sexual network models typically attribute most HIV transmissions to casual partners, perhaps because these models are able to capture increased concurrency with casual partners, supporting individual-based interventions for MSM in casual partnerships.6,7
Although the underlying drivers of HIV transmission among MSM may vary based on main and casual partner types, little is known about how the number and composition of sex partner types has changed nationally in recent history, and, thus, which relationship contexts should be prioritized for HIV prevention. Over the past 20 years, significant progress has been made in the acceptance of long-term same-sex partnerships in the United States, culminating in the Supreme Court decision to legalize same-sex marriage in 2015. According to the General Social Survey, from 1991 to 2010, public acceptance of “homosexual behavior” has increased by 27% and “same-sex marriage” by 35%.8 These recent social and legal changes over the past 2 decades could be leading to changes in sexual partnering among MSM, with possible implications for HIV transmission and prevention. For example, one hypothesis is that, on average, MSM may be more likely to form main partnerships during this period and reduce their number of total partners. A second hypothesis is that MSM on average may maintain the same total number of partners, but shift the composition of these partnerships toward having more main partners. Similar trends in condomless anal sex may be occurring. Previous research has shown that condomless anal sex among MSM in the United States has increased since 2005, but it is unknown whether this could be the result of an increasing number of main partnerships, within which MSM are more likely to engage in condomless anal sex.9,10
We sought to evaluate recent changes in the number and composition of sex partners among MSM to identify whether and how sexual partnering has changed in an era of increasing social and legal acceptance of long-term same-sex partnerships in the United States. Identifying and describing these changes could provide critical information for understanding HIV transmission among MSM and for determining the relationship contexts in which HIV prevention efforts should be focused.
METHODS
The Centers for Disease Control and Prevention’s National HIV Behavioral Surveillance (NHBS) collects data on HIV risk and prevention behaviors among 3 populations: MSM, persons who inject drugs, and heterosexuals at increased risk of HIV infection.11 Cross-sectional data reported in this analysis were collected among MSM in 3 survey “rounds” (2008, 2011, and 2014). NHBS sampling procedures have been previously published and are summarized briefly here.12 MSM were recruited through venue-based, time-space sampling and, if eligible, were offered a behavioral survey and HIV testing. Eligible men included those who were male sex at birth and self-identified as male, had ever had sex with another man, were aged 18 years or older, currently resided in a participating metropolitan statistical area, had not previously participated in NHBS during that year’s survey, and were able to complete the survey in English or Spanish. For this analysis, eligible men also had to have at least 1 male sex partner in the past 12 months. NHBS activities were approved by local institutional review boards in each of the 21 participating metropolitan statistical areas (listed in Table 1).
TABLE 1.
Sample Characteristics of MSM Participating in NHBS, 21 Cities, United States, 2008–2014
| 2008, n (%) | 2011, n (%) | 2014, n (%) | Total Combined, n (%) | |
|---|---|---|---|---|
| Age (yrs) | ||||
| 18–24 | 2069 (22.4) | 2347 (25.4) | 1952 (20.4) | 6368 (22.7) |
| 25–29 | 1710 (18.5) | 1746 (18.9) | 2094 (21.9) | 5550 (19.8) |
| 30–39 | 2561 (27.7) | 2182 (23.6) | 2470 (25.8) | 7213 (25.7) |
| ≥40 | 2907 (31.4) | 2954 (32.0) | 3069 (32.0) | 8930 (31.8) |
| Race/ethnicity | ||||
| Black/African American | 2188 (23.7) | 2485 (26.9) | 2652 (27.7) | 7325 (26.1) |
| Hispanic/Latino* | 2232 (24.1) | 2407 (26.1) | 2523 (26.3) | 7162 (25.5) |
| White | 4024 (43.5) | 3665 (39.7) | 3668 (38.3) | 11357 (40.5) |
| Other† | 803 (8.7) | 672 (7.3) | 742 (7.7) | 2217 (7.9) |
| Education | ||||
| High school graduate or less | 2712 (29.3) | 2714 (29.4) | 2489 (26.0) | 2489 (26.0) |
| Some college or technical college | 3021 (32.7) | 3128 (33.9) | 3072 (32.1) | 3072 (32.1) |
| College or higher education | 3513 (38.0) | 3386 (36.7) | 4023 (42.0) | 4023 (42.0) |
| Sexual identity | ||||
| Homosexual | 7499 (81.2) | 7555 (82.1) | 7794 (81.6) | 22848 (81.6) |
| Bisexual/heterosexual | 1735 (18.8) | 1646 (17.9) | 1761 (18.4) | 5142 (18.4) |
| Self-reported HIV status | ||||
| HIV-negative | 7044 (76.2) | 7114 (77.1) | 7381 (77.0) | 21539 (76.8) |
| HIV-positive | 1101 (11.9) | 1239 (13.4) | 1581 (16.5) | 3921 (14.0) |
| Unknown | 1102 (11.9) | 876 (9.5) | 623 (6.5) | 2601 (9.3) |
| City‡ | ||||
| Atlanta, GA | 347 (3.8) | 556 (6.0) | 505 (5.3) | 1408 (5.0) |
| Baltimore, MD | 501 (5.4) | 451 (4.9) | 496 (5.2) | 1448 (5.2) |
| Boston, MA | 281 (3.0) | 415 (4.5) | 301 (3.1) | 1123 (3.6) |
| Chicago, IL | 566 (6.1) | 500 (5.4) | 517 (5.4) | 1583 (5.6) |
| Dallas, TX | 509 (5.5) | 471 (5.1) | 500 (5.2) | 1480 (5.3) |
| Denver, CO | 544 (5.9) | 546 (5.9) | 513 (5.4) | 1603 (5.7) |
| Detroit, MI | 388 (4.2) | 460 (5.0) | 508 (5.3) | 1356 (4.8) |
| Houston, TX | 448 (4.8) | 509 (5.5) | 508 (5.3) | 1465 (5.2) |
| Los Angeles, CA | 537 (5.8) | 519 (5.6) | 522 (5.5) | 1578 (5.6) |
| Miami, FL | 529 (5.7) | 503 (5.5) | 530 (5.5) | 1562 (5.6) |
| Nassau-Suffolk, NY | 281 (3.0) | 337 (3.7) | 337 (3.5) | 955 (3.4) |
| New Orleans, LA | 478 (5.2) | 484 (5.2) | 515 (5.4) | 1477 (5.3) |
| New York, NY | 554 (6.0) | 519 (5.6) | 497 (5.2) | 1570 (5.6) |
| Newark, NJ | 98 (1.1) | 248 (2.7) | 245 (2.6) | 591 (2.1) |
| Philadelphia, PA | 562 (6.1) | 545 (5.9) | 649 (6.8) | 1756 (6.3) |
| St. Louis, MO | 372 (4.0) | — | — | 372 (1.3) |
| San Diego, CA | 549 (5.9) | 470 (5.1) | 536 (5.6) | 1555 (5.5) |
| San Francisco, CA | 486 (5.3) | 464 (5.0) | 386 (4.0) | 1336 (4.8) |
| San Juan, PR | 355 (3.8) | 363 (3.9) | 515 (5.4) | 1233 (4.4) |
| Seattle, WA | 361 (3.9) | 369 (4.0) | 498 (5.2) | 1228 (4.4) |
| Washington, DC | 501 (5.4) | 500 (5.4) | 507 (5.3) | 1508 (5.4) |
| Total | 9247 (33.0) | 9229 (32.9) | 9585 (34.2) | 28061 (100.0) |
Hispanics/Latinos can be of any race.
Other races include American Indian, Alaska Native, Asian, Native Hawaiian, other Pacific Islander, and mixed race.
All cities were included in the 2008 survey. All cities except St. Louis, MO, were included in the 2011 and 2014 surveys.
Partner count outcomes included the number of total male sex partners in the past 12 months and the number of main male sex partners in the past 12 months. We estimated the adjusted mean partner counts overall and by key demographic characteristics. Total partner counts above 50 (2.1%) were set to 50, and main partner counts above 10 (0.3%) were set to 10 to avoid the influence of outliers on trends in mean counts. We used identity-linked Poisson regression to evaluate trends in the count outcomes and measured the mean change in partner count per 3-year increase in time. Descriptive statistics are reported for the binary outcomes of having 1 main partner only (and 0 casual partners) in the past year, having both main and casual partners in the past year, and having condomless anal sex in the past year among (a) men with 1 main partner only (and 0 casual partners) and (b) men with both main and casual partners. Main partners referred to “men with whom the participant has had sex and feels committed to above anyone else,” and casual partners referred to “men with whom the participant has had sex yet does not feel committed to or does not know very well.”13 Because the odds ratio can overestimate the prevalence ratio for common binary outcomes in cross-sectional studies, we used log-linked Poisson regression with robust standard errors to obtain estimated “round” percent changes (ERPCs), which represent the mean relative percent change in the outcome per 3-year increase in time.14
All models included year as the main, continuous term of interest; age, race/ethnicity, and self-reported HIV status as covariates of interest; and all 2-way interaction terms between year and age, race, and HIV status to evaluate changes overall and by key characteristics. Because each model contained multiple interaction terms with year, when estimating the effect of year by 1 covariate of interest, we specified the distribution of the other 2 variables from the combined sample across all 3 survey years. This allowed for standardizing the year effects to the sample distribution of the other 2 variables in the model. City was also included in models to account for potential confounding, and all models accounted for clustering by venue recruitment event. All analyses were conducted in SAS 9.4 and figures were created using R’s ggplot2 package.
RESULTS
For this analysis, we included 28,061 men across the 3 NHBS-MSM rounds who consented to participate, provided complete, valid survey responses, reported having at least 1 male sex partner in the past year, and provided information on the key covariates of interest. Characteristics of the sample by NHBS round are described in Table 1.
Partner Count Outcomes
Overall, the adjusted mean total number of male sex partners in the past year increased among MSM from 7.1 in 2008 to 7.7 in 2014 (Table 2; see Figure A, Supplemental Digital Content, http://links.lww.com/QAI/B299). We found significant differences by age and race. On average, MSM younger than 40 years experienced an increase of between 0.43 and 0.60 total partners per 3-year increase in time, while MSM aged 40 years and older experienced stable total partner numbers. Black and Hispanic MSM, and MSM of other race/ethnicities apart from white, had stable trends in total partner counts; yet, white MSM had a significant increase of 0.67 total partners per 3-year increase. Total number of partners increased significantly among both HIV-negative and HIV-positive MSM.
TABLE 2.
Trends in Number of Total and Main Partners Among MSM—NHBS, 21 Cities, United States, 2008–2014
|
No. of Total Partners |
|||||||||||||
|
2008 |
2011 |
2014 |
Overall (N = 28061) |
||||||||||
| n | Adj. Mean | 95% CI | n | Adj. Mean | 95% CI | n | Adj. Mean | 95% CI | Estimated Round Mean Change*† | 95% CI | P | Inter.‡ P | |
| Age (yrs) | 0.02 | ||||||||||||
| 18–24 | 2069 | 6.4 | 6.1 to 6.7 | 2347 | 6.7 | 6.4 to 7.0 | 1952 | 7.3 | 7.0 to 7.7 | 0.60 | 0.31 to 0.88 | <0.01 | |
| 25–29 | 1710 | 7.2 | 6.8 to 7.5 | 1746 | 7.1 | 6.8 to 7.5 | 2094 | 8.1 | 7.7 to 8.4 | 0.52 | 0.18 to 0.86 | <0.01 | |
| 30–39 | 2561 | 7.4 | 7.1 to 7.7 | 2182 | 7.6 | 7.3 to 8.0 | 2470 | 8.2 | 7.9 to 8.5 | 0.43 | 0.14 to 0.73 | <0.01 | |
| ≥40 | 2907 | 7.2 | 6.9 to 7.5 | 2954 | 7.2 | 6.9 to 7.5 | 3069 | 7.3 | 7.0 to 7.6 | 0.01 | −0.29 to 0.31 | 0.95 | |
| Race/ethnicity | 0.01 | ||||||||||||
| Black/African American | 2188 | 6.0 | 5.7 to 6.3 | 2485 | 6.0 | 5.7 to 6.3 | 2652 | 6.1 | 5.8 to 6.4 | 0.02 | −0.24 to 0.27 | 0.90 | |
| Hispanic/Latino∥ | 2232 | 6.9 | 6.6 to 7.3 | 2407 | 7.0 | 6.7 to 7.4 | 2523 | 7.4 | 7.1 to 7.7 | 0.17 | −0.14 to 0.49 | 0.29 | |
| White | 4024 | 7.8 | 7.6 to 8.1 | 3665 | 8.0 | 7.7 to 8.3 | 3668 | 9.1 | 8.8 to 9.4 | 0.67 | 0.38 to 0.96 | <0.01 | |
| Other¶ | 803 | 6.7 | 6.2 to 7.3 | 672 | 7.0 | 6.4 to 7.7 | 742 | 7.7 | 7.1 to 8.3 | 0.42 | −0.10 to 0.94 | 0.11 | |
| Self-reported HIV status | 0.22 | ||||||||||||
| HIV-negative | 7044 | 6.8 | 6.6 to 7.0 | 7114 | 7.1 | 6.9 to 7.3 | 7381 | 7.5 | 7.3 to 7.7 | 0.36 | 0.18 to 0.54 | <0.01 | |
| HIV-positive | 1101 | 8.7 | 8.2 to 9.2 | 1239 | 8.5 | 8.1 to 9.0 | 1581 | 9.6 | 9.1 to 10.0 | 0.54 | 0.03 to 1.04 | 0.04 | |
| Unknown | 1102 | 6.5 | 6.1 to 7.0 | 876 | 6.1 | 5.7 to 6.5 | 623 | 6.5 | 6.0 to 7.1 | 0.03 | −0.42 to 0.47 | 0.90 | |
| Total | 9247 | 7.1 | 6.9 to 7.2 | 9229 | 7.2 | 7.0 to 7.4 | 9585 | 7.7 | 7.5 to 7.9 | 0.35 | 0.18 to 0.52 | <0.01 | |
|
No. of Main§ Partners |
|||||||||||||
|
2008 |
2011 |
2014 |
Overall (N = 28053) |
||||||||||
| n | Adj. Mean | 95% CI | n | Adj. Mean | 95% CI | n | Adj. Mean | 95% CI | Estimated Round Mean Change*† | 95% CI | P | Inter.‡P | |
| Age (yrs) | 0.03 | ||||||||||||
| 18–24 | 2069 | 1.3 | 1.3 to 1.4 | 2347 | 1.3 | 1.3 to 1.4 | 1950 | 1.2 | 1.2 to 1.3 | −0.05 | −0.09 to −0.01 | 0.02 | |
| 25–29 | 1709 | 1.1 | 1.0 to 1.2 | 1746 | 1.1 | 1.0 to 1.1 | 2093 | 1.1 | 1.1 to 1.2 | 0.02 | −0.02 to 0.06 | 0.45 | |
| 30–39 | 2561 | 0.9 | 0.9 to 1.0 | 2181 | 1.0 | 0.9, 1.0 | 2470 | 0.9 | 0.9 to 1.0 | 0.01 | −0.02, 0.04 | 0.57 | |
| ≥40 | 2907 | 0.8 | 0.7 to 0.8 | 2951 | 0.8 | 0.7 to 0.8 | 3069 | 0.7 | 0.7 to 0.8 | −0.04 | −0.07 to −0.01 | 0.02 | |
| Race/ethnicity | 0.20 | ||||||||||||
| Black/African American | 2187 | 1.0 | 1.0 to 1.1 | 2484 | 1.1 | 1.0 to 1.1 | 2651 | 1.0 | 0.9 to 1.0 | −0.03 | −0.07 to 0.01 | 0.14 | |
| Hispanic/Latino∥ | 2232 | 1.0 | 1.0 to 1.1 | 2406 | 1.0 | 1.0 to 1.1 | 2523 | 0.9 | 0.9 to 1.0 | −0.04 | −0.08 to −0.01 | 0.01 | |
| White | 4024 | 1.0 | 1.0 to 1.0 | 3663 | 1.0 | 0.9 to 1.0 | 3667 | 1.0 | 0.9 to 1.0 | 0.00 | −0.03 to 0.03 | 0.95 | |
| Other¶ | 803 | 1.0 | 0.9 to 1.0 | 672 | 1.0 | 0.9 to 1.1 | 741 | 1.0 | 0.9 to 1.1 | 0.01 | −0.05 to 0.07 | 0.69 | |
| Self-reported HIV status | <0.01 | ||||||||||||
| HIV-negative | 7043 | 1.0 | 1.0 to 1.1 | 7112 | 1.0 | 1.0 to 1.0 | 7379 | 1.0 | 0.9 to 1.0 | −0.03 | −0.05 to −0.01 | <0.01 | |
| HIV-positive | 1101 | 1.0 | 0.9 to 1.0 | 1239 | 1.1 | 1.0 to 1.1 | 1581 | 1.1 | 1.1 to 1.2 | 0.07 | 0.02 to 0.11 | <0.01 | |
| Unknown | 1102 | 0.9 | 0.8 to 1.0 | 874 | 0.8 | 0.8 to 0.9 | 622 | 0.8 | 0.8 to 0.9 | −0.02 | −0.09 to 0.04 | 0.47 | |
| Total | 9246 | 1.0 | 1.0 to 1.0 | 9225 | 1.0 | 1.0 to 1.0 | 9582 | 1.0 | 1.0 to 1.0 | −0.02 | −0.04 to 0.00 | 0.05 | |
Estimated round mean change = estimated 3-year mean change outcome.
Adjusted for age, race, HIV status, and city and accounted for clustering by recruitment event.
Interaction P value.
Main partners refer to “men with whom the participant has had sex and feels committed to above anyone else.”
Hispanics/Latinos can be of any race.
Other races include American Indian, Alaska Native, Asian, Native Hawaiian, other Pacific Islander, and mixed race.
Partner type was missing for 8 observations; hence, 28,053 participants were included in analyses of the main partner count outcome (Table 2; see Figure A, Supplemental Digital Content, http://links.lww.com/QAI/B299). The mean number of main male sex partners among MSM overall was stable from 2008 to 2014 at about 1 main partner per year. There were significant differences by age and HIV status. MSM aged 18–24 and 40 years and older and HIV-negative MSM experienced small decreases in the number of main partners, while HIV-positive MSM experienced a slight increase.
Partner Type Composition and Condomless Anal Sex Outcomes
The proportion of MSM having 1 main partner only in the past 12 months significantly declined from 19.9% in 2008 to 15.1% in 2014 overall. This represented a relative percent decline of 13.5% per 3 years during this period (ERPC = −13.5%, P < 0.01; Table 3 and see Figure B, Supplemental Digital Content, http://links.lww.com/QAI/B299). Significant interactions were found by age and race. Although the decline in the proportion having 1 main partner only occurred across all age, race, and HIV status groups, the greatest decreases were in younger MSM aged 18–24, 25–29, and 30–39 years, white MSM, black MSM, and HIV-negative MSM.
TABLE 3.
Trends in Partner Type Composition Amona MSM—NHBS, 21 Cities, United States, 2008–2014
|
One Main§
Partner Only∥
in Past 12 Months |
|||||||
|
2008 (N = 9246) |
2011 (N = 9225) |
2014 (N = 9582) |
Overall (N = 28053) |
||||
| n (%) | n (%) | n (%) | Estimated Round Percent Change*† | 95% CI | P | Inter.‡ P | |
| Age (yrs) | 0.045 | ||||||
| 18–24 | 378 (18.3) | 328 (14.0) | 253 (13.0) | −18.8 | −4.9 to −12.3 | <0.01 | |
| 25–29 | 331 (19.4) | 280 (16.0) | 289 (13.8) | −16.2 | −22.0 to −9.9 | <0.01 | |
| 30–39 | 523 (20.4) | 401 (18.4) | 371 (15.0) | −13.3 | −18.5 to −7.8 | <0.01 | |
| ≥40 | 610 (21.0) | 600 (20.3) | 535 (17.4) | −7.8 | −12.9 to −2.4 | <0.01 | |
| Race/ethnicity | 0.01 | ||||||
| Black/African American | 448 (20.5) | 501 (20.2) | 393 (14.8) | −15.0 | −20.1 to 9.6 | <0.01 | |
| Hispanic/Latino# | 396 (17.7) | 409 (17.0) | 421 (16.7) | −5.1 | −11.2 to 1.4 | 0.12 | |
| White | 849 (21.1) | 597 (16.3) | 519 (14.2) | −18.1 | −22.4 to −13.5 | <0.01 | |
| Other** | 149 (18.6) | 102 (15.2) | 115 (15.5) | −9.4 | −19.5 to 1.9 | 0.10 | |
| Self-reported HIV status | 0.09 | ||||||
| HIV-negative | 1415 (20.1) | 1228 (17.3) | 1086 (14.7) | −15.1 | −18.4 to −11.7 | <0.01 | |
| HIV-positive | 203 (18.4) | 222 (17.9) | 259 (16.4) | −7.9 | −15.4 to 0.3 | 0.06 | |
| Unknown | 224 (20.3) | 159 (18.2) | 103 (16.6) | −7.7 | −16.9 to 2.4 | 0.13 | |
| Total | 1842 (19.9) | 1609 (17.4) | 1448 (15.1) | −13.5 | −16.5 to −10.4 | <0.01 | |
|
Both Main§
and Casual¶
Partners in Past 12 Months |
|||||||
|
2008 |
2011 |
2014 |
Overall |
||||
| n (%) | n (%) | n (%) | Estimated Round Percent Change*† | 95% CI | P | Inter.‡ P | |
| Age (yrs) | 0.95 | ||||||
| 18–24 | 899 (43.5) | 1206 (51.4) | 1015 (52.1) | 9.7 | 6.2 to 13.4 | <0.01 | |
| 25–29 | 750 (43.9) | 834 (47.8) | 1074 (51.3) | 8.2 | 4.5 to 12.1 | <0.01 | |
| 30–39 | 954 (37.3) | 935 (42.9) | 1112 (45.0) | 9.2 | 5.6 to 12.9 | <0.01 | |
| ≥40 | 805 (27.7) | 971 (32.9) | 1024 (33.4) | 9.2 | 4.9 to 13.7 | <0.01 | |
| Race/ethnicity | 0.09 | ||||||
| Black/African American | 739 (33.8) | 1004 (40.4) | 1110 (41.9) | 10.4 | 6.2 to 14.8 | <0.01 | |
| Hispanic/Latino# | 889 (39.8) | 1071 (44.5) | 1113 (44.1) | 5.0 | 1.5 to 8.7 | <0.01 | |
| White | 1472 (36.6) | 1568 (42.8) | 1656 (45.2) | 10.5 | 7.5 to 13.7 | <0.01 | |
| Other** | 308 (38.4) | 303 (45.1) | 346 (46.7) | 11.0 | 4.8 to 17.6 | <0.01 | |
| Self-reported HIV status | 0.67 | ||||||
| HIV-negative | 2657 (37.7) | 3112 (43.8) | 3300 (44.7) | 9.6 | 7.2 to 12.0 | <0.01 | |
| HIV-positive | 423 (38.4) | 535 (43.2) | 704 (44.5) | 7.1 | 2.3 to 12.2 | <0.01 | |
| Unknown | 328 (29.8) | 299 (34.2) | 221 (35.5) | 8.4 | 1.0 to 16.3 | 0.02 | |
| Total | 3408 (36.9) | 3946 (42.8) | 4225 (44.1) | 9.1 | 7.0 to 11.3 | <0.01 | |
Estimated Round Percent Change (ERPC) = estimated 3-year percent change in number of partners.
ERPC is adjusted for age, race, HIV status, and city and accounted for clustering by recruitment event.
Interaction P value.
Main partners refer to “men with whom the participant has had sex and feels committed to above anyone else.”
One main partner only refers to “MSM reporting only 1 main partner and 0 casual partners in the past year.”
Casual partners refer to “men with whom the participant has had sex yet does not feel committed to or does not know very well.”
Hispanics/Latinos can be of any race.
Other races include American Indian, Alaska Native, Asian, Native Hawaiian, other Pacific Islander, and mixed race.
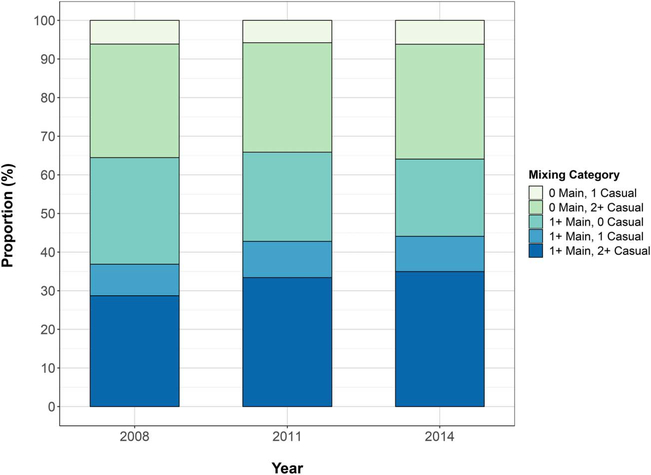
The proportion of MSM having both main and casual partners in the past 12 months significantly increased overall from 36.9% in 2008 to 44.1% in 2014. This represented a relative percent increase of 9.1% per 3 years (ERPC = 9.1%; P < 0.01; Table 3 and see Figure B, Supplemental Digital Content, http://links.lww.com/QAI/B299). This significant increase was observed at a similar magnitude across all age, race, and HIV status groups, and we found no significant interactions for this outcome. When comparing the number and composition of partner types over time, the proportion of men who reported having 1 or more main partners and 0 casual partners decreased by 7.6% (percentage points) from 2008 to 2014 while the proportion of men who reported having 1 or more main partners and 2 or more casual partners increased by 6.3% (percentage points). All other composition types (0 main and 1 casual, 0 main and 2 or more casual, and 1 or more main and 1 casual) remained stable (Fig. 1).
FIGURE 1.
Trends in partner type number and composition in the past 12 months among MSM—NHBS, 21 cities, United States, 2008–2014.
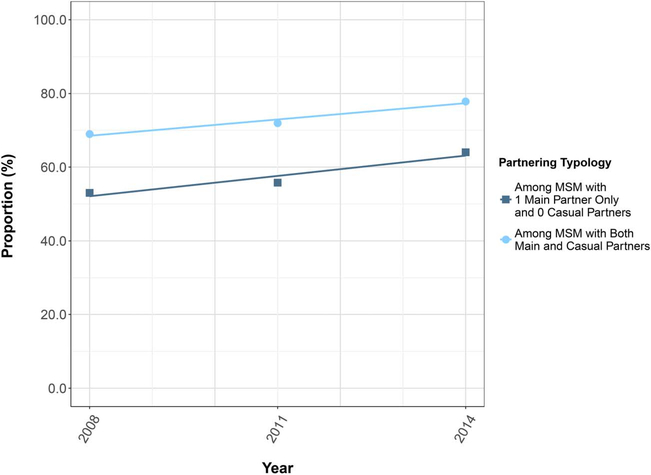
Of those who had 1 main partner only in the past year, 2 did not report on condom use (n = 4897); of those who had both main and casual partners in the past year, 13 did not report on condom use (n = 11,566). Condomless anal sex among men with 1 main partner only in the past 12 months increased significantly from 53.0% in 2008 to 64.0% in 2014 (Fig. 2 and see Table A, Supplemental Digital Content, http://links.lww.com/QAI/B299). Condomless anal sex among men with both main and casual partners in the past 12 months was higher and also significantly increased from 69.0% in 2008 to 77.8% in 2014. We found no significant interactions for either outcome.
FIGURE 2.
Trends in condomless anal sex in the past 12 months among MSM, by partner type composition—NHBS, 21 cities, United States, 2008–2014.
Post Hoc Subanalysis
Given our results above did not support our original hypotheses, we decided to conduct a limited post hoc analysis. A recent study demonstrated associations between frequent Internet use and higher number of casual partners in cross-sectional data from 2014.15 Therefore, we sought to examine the role of Internet use on changes in sexual partnering using our 2011 and 2014 data. We found that when controlling for Internet use to meet or socialize with men in the past 12 months (ever vs. never), the increasing trend in total partner counts slightly attenuated (0.34 increase in total partners per 3 years; P = 0.03) and the trend in the proportion with both main and casual partners became stable (ERPC = 1.6%; P = 0.36). We further stratified our sample by Internet use frequency (weekly or more often vs. a few times a month or less frequent vs. never) and found that, among MSM who frequently (ie, weekly or more often) used the Internet to meet or socialize with men, the mean total partner counts increased by 1.1 partners per 3 years (P < 0.01) and the proportion of MSM with both main and casual partners increased by 5.7% per 3 years (P = 0.02), whereas MSM with occasional use or no use in the past 12 months had stable partner outcomes.
DISCUSSION
From 2008 to 2014, the mean number of total partners in the past year among MSM significantly increased overall, driven mostly by white MSM and MSM younger than 40 years, while the mean number of main partners remained stable. During the same period, the proportion of MSM engaged in 1 main partnership only in the past year decreased and the proportion with both main and casual partners increased. Partnering changes were characterized by decreases in MSM reporting 1 or more main partners and 0 casual partners and increases in MSM reporting 1 or more main partners and 2 or more casual partners. Condomless anal sex in the past year increased significantly regardless of partner type composition.
Although we expected that growing social acceptance of long-term same-sex partnerships could contribute to MSM being more likely to pair with main partners or have 1 main partner only in the past year, we did not observe this trend. Our overall findings suggest that MSM have been increasingly engaging in sex with additional casual partners. These results could serve to generate new hypotheses for future research. One explanation for our results may be that increasing social acceptance of same-sex relationships in general has led MSM to experience less stigma about same-sex behaviors and be more open to meet new casual sex partners in recent years. Another hypothesis is that the Internet boom and accessibility to smartphones, dating apps, and other online tools during the past decade has profoundly changed how men seek partners, and increasing use of the Internet may contribute to an increasing number of sex partners or a shift toward casual partners who may be easier to find online.16 A recent analysis of MSM found that Internet use to meet men has increased since 2008 and that frequent Internet use was associated with greater partner counts in 2014.15 Our post hoc subanalysis further demonstrated that the increasing trend in total partner counts became slightly attenuated and the trend in the proportion of MSM with both main and casual partners became stable after controlling for Internet use to meet men. When stratified, only men using the Internet most frequently (ie, weekly or more often) experienced significant increases in total partner counts and in the proportion having both main and casual partners. These findings suggest that partnering trends may differ by Internet use. Future studies should consider trends in Internet use to meet partners and associated risk behaviors by partner type and compare behaviors between online and offline partners by partner type. Although occurring during a period of stable overall HIV incidence for MSM, these hypotheses and proposed behavioral patterns are consistent with our results as well as the recent increases in condomless anal sex and sexually transmitted infections (STIs) among MSM in the United States and parts of Europe.9,17–19
The increases in total partners and the proportion of MSM with both main and casual partners in the past year raise an important concern that these may be concurrent main and casual partnerships and that concurrency may be increasing among MSM. Concurrency, or “the overlapping of sexual partnerships where sexual intercourse with 1 partner occurs between 2 acts of intercourse with another partner,” can contribute to the spread of infection through partners’ indirect exposure to one another.20–23 Concurrency can be more common within casual partnerships, as these tend to be shorter, and MSM may have multiple casual partners allowing for potential overlap in sexual acts.24,25 Yet, main partnerships tend to be longer in duration and have a higher frequency of sex acts and condomless anal sex than casual partnerships.2,25 If the main and casual partnerships MSM report are not serially monogamous, it is possible that men may be having sex with additional casual partners while in a longer-duration main partnership, resulting in concurrency and increasing a main partner’s risk of acquiring HIV. This may warrant increased attention to prevent transmissions to main partners who are exposed to condomless anal sex more frequently. Unfortunately, we were not able to examine timing of partnerships and therefore whether concurrency may be increasing among MSM; yet, this should be considered in future studies. Finally, we believed that previous findings of increasing condomless anal sex among MSM could be explained by an increasing number of main partnerships that are more likely to practice condomless anal sex; however, our results do not support this, and further analyses to explain increasing condomless anal sex trends are needed.
We observed heterogeneity in partner outcomes by age, race, and HIV status. Black and Hispanic MSM had stable total partner counts and either stable or slightly declining main partner counts, yet both groups still experienced a significant increase in the proportion of MSM with both main and casual partners. These results indicate that although total partner counts were constant on average, there was still a shift in partner composition toward having both main and casual partners. This could suggest that there may have only been a certain number of sex partners that black and Hispanic MSM had over a year’s time, but that a similar change toward casual partnering was occurring among black and Hispanic MSM as observed for other races. Young MSM aged 18–24 years had the largest increase in total partners and the greatest declines in main partner counts and the proportion with 1 main partner only. One explanation for these results could be that population-level exposure to technology and online dating apps is unequally distributed or unequally increasing by age, such that young MSM are more likely to use these media to seek sex partners than their older counterparts were, exposing them to more casual partners.26 Alternative explanations could be that young MSM in recent years may be more open about sexuality and seeking partners or are coming of age and exploring sexuality earlier than when young MSM in previous years were, such that young MSM in recent years may have a greater number of partners or may be less likely to engage in main partnerships. This may be supported by other literature that has suggested declines in age of sexual debut and increases in sexual risk taking among younger birth cohorts.27 MSM with a known HIV-positive status had increasing total partner counts and increasing main partner counts; however, the magnitude of the increase in main partners was not enough to account for the total increase. Therefore, additional casual partners were still largely contributing to the total partner increase in HIV-positive MSM. The proportion with both main and casual partners was also increasing in this subgroup and could indicate increasing concurrency. Although HIV transmission risk from known, nonrecently infected HIV-positive MSM to concurrent HIV-negative partners confers no additional risk over having the same number of serially monogamous HIV-negative partners, increased concurrency would still be relevant to these partners’ risk of acquiring other STIs.
Our findings regarding increasing casual partners and a shift toward casual partnering suggest that individual interventions for HIV prevention should continue to receive high priority for funding resources. Men with multiple partners may need individual interventions where they can be regularly tested and identified as candidates for treatment or pre-exposure prophylaxis (PrEP). These individual interventions should emphasize multiple options for reducing risk, including partner reduction and condom use. Yet, because the increase in casual partners did not occur alone, but in addition to having main partners, partner-based interventions that target main partnerships are still warranted for MSM. Existing partner-based interventions such as CHTC are not commonly offered as part of routine HIV testing, but these interventions can facilitate testing together, discussion about HIV status, and negotiation of sexual agreements such as whether partners can have outside partners and what type of sex can occur within the relationship and/or with outside partners.28–31 Partner-based interventions including HIV prevention programs geared toward couples can also help to identify positive partners and either start or reengage them on treatment, or identify candidates for PrEP and support uptake and retention on PrEP, to reduce potential transmission not only within the partnership but with outside casual partners. Increasing financial support and capacity building for CHTC and other partner-based interventions in facilities that already provide HIV testing could maximize the impact of testing services and prevent transmissions among men in both main and casual partnerships.
This study is subject to several limitations. First, it is possible that insufficient time has accrued since recent social and legal acceptance of long-term same-sex partnerships to be able to observe and interpret the impact of social trends on sexual partnering norms; analyses could be revised once more data are available. Second, these data were collected using venue-based sampling and therefore are not generalizable to non-venue-attending MSM. Furthermore, it is important to note that our sample consisted of men who visit venues such as gay-oriented bars and restaurants, and it may be that men in committed, main partnerships are less likely to attend these venues. This may result in an underestimation of men with main partners or 1 main partner only in the past year. However, we did not expect this proportion of men in committed main partnerships who do not visit venues to change substantially over time, and therefore, we did not anticipate this to affect our estimates. Because we focused on self-reported sexual behavior outcomes, it is possible that social desirability may bias our estimates, underestimating partner counts and condomless anal sex. Although difficult to assess how social desirability bias may have changed over time without more objective measures of behavior, MSM may be more open to sharing information and less likely to misreport sex behaviors in recent years. In future NHBS rounds with MSM, additional biological measures such as STIs are planned and may be able to capture the magnitude of potential biases in self-reported sexual behavior data. Finally, we were not able to account for possible changes in men’s perceptions of partner type over time, but the objective definitions of partner types used in NHBS interviews did not change.
CONCLUSIONS
We found that total partner counts were increasing or stable across MSM subgroups, while main partner counts remained stable across most all groups. An increasing proportion of MSM had both main and casual partnerships in the past year, characterized by having more casual partners in addition to 1 or more main partners. In light of these behavioral trends, prevention efforts that use knowledge about partners are needed. Main partnerships can provide opportunities for routine couples’ HIV testing and identification of partners who need to enter or re-enter HIV care or initiate PrEP. Individual interventions for men with multiple casual partners should continue to encourage at least annual HIV testing, condom use, and partner reduction. Future research should study potential increases in concurrency by partner type and examine post hoc hypotheses including how increasing use of the Internet and dating apps may contribute to additional casual partnering in recent years.
Supplementary Material
Footnotes
The authors have no conflicts of interest to disclose.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Use of trade names is for identification only and does not imply endorsement by the US Department of Health and Human Services, the Public Health Service, or the Centers for Disease Control and Prevention.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jaids.com).
REFERENCES
- 1.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas-2016. HIV Surveill Rep. 2017; 26:17. [Google Scholar]
- 2.Sullivan PS, Salazar L, Buchbinder S, et al. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–1162. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg ES, Grey JA, Paz-Bailey G, et al. Estimating the Number and Characteristics of Male-Male HIV Transmissions in the USA. Conference on Retroviruses and Opportunistic Infections, 2015. Seattle, WA Abstract #1115. [Google Scholar]
- 4.Sullivan PS, Stephenson R, Grazter B, et al. Adaptation of the African couples HIV testing and counseling model for men who have sex with men in the United States: an application of the ADAPT-ITT framework. Springerplus. 2014;3:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Guidance on Couples HIV Testing and Counselling Including Antiretroviral Therapy for Treatment and Prevention in Serodiscordant Couples: Recommendations for a Public Health Approach. Geneva, Switzerland: WHO Press; 2012. [PubMed] [Google Scholar]
- 6.Chapin-Bardales J, Jenness SM, Rosenberg ES, et al. Distribution of HIV Transmission by Network and Clinical Factors Among US MSM. Conference on Retroviruses and Opportunistic Infections, 2017. Seattle, WA Abstract #1024. [Google Scholar]
- 7.Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS One. 2012;7:e50522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith TW. Public Attitudes Toward Homosexuality. Chicago, IL: National Opinion Research Center, University of Chicago; 2011. [Google Scholar]
- 9.Paz-Bailey G, Mendoza M, Finlayson T, et al. Trends in condom use among men who have sex with men in the United States: the role of antiretroviral therapy and sero-adaptive strategies. AIDS. 2016;30: 1985–1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paz-Bailey G, Hall IH, Wolitski RJ, et al. HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men—United States. MMWR Morb Mortal Wkly Rep. 2013;62:958–962. [PMC free article] [PubMed] [Google Scholar]
- 11.Paz-Bailey G, Raymond HF, Lansky A, et al. Using the national HIV behavioral surveillance system to inform HIV prevention efforts in the United States. AIDS Behav. 2014;18(suppl 3):S233–S236. [DOI] [PubMed] [Google Scholar]
- 12.Finlayson TJ, Le B, Smith A, et al. HIV risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance System, 21 U.S. cities, United States, 2008. MMWR Surveill Summ. 2011;60:1–34. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. HIV Infection Risk, Prevention, and Testing Behaviors Among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 20 U.S. Cities, 2014. HIV Surveillance Special Report 15. 2016. Available at: http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-hssr-nhbs-msm-2014.dfp. Accessed May 16, 2016.
- 14.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paz-Bailey G, Hoots BE, Xia M, et al. Trends in internet use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2017;75:S288–S295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grov C, Breslow AS, Newcomb ME, et al. Gay and bisexual men’s use of the Internet: research from the 1990s through 2013. J Sex Res. 2014; 51:390–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kouyos RD, Hasse B, Calmy A, et al. Increases in condomless sex in the Swiss HIV cohort study. Open Forum Infect Dis. 2015;2:ofv077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hess KL, Crepaz N, Rose C, et al. Trends in sexual behavior among men who have sex with men (MSM) in high-income countries, 1990–2013: a systematic review. AIDS Behav. 2017;21:2811–2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2016. Atlanta, GA: U.S. Department of Health and Human Services; 2017. [Google Scholar]
- 20.UNAIDS Reference Group on Estimates Modelling and Projections. Consultation on Concurrent Sexual Partnerships: Recommendations From a Meeting of the UNAIDS Reference Group on Estimates; 2009. [Google Scholar]
- 21.Morris M, Goodreau SM, Moody J. Sexual networks, concurrency, and STD/HIV In: Holmes KK, Sparling PF, Stamm WE, et al. , eds. Sexually Transmitted Diseases. New York, NY: McGraw Hill; 2008. [Google Scholar]
- 22.Eaton JW, Hallett TB, Garnett GP. Concurrent sexual partnerships and primary HIV infection: a critical interaction. AIDS Behav. 2011;15:687–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenberg ES, Rothenberg RB, Kleinbaum DG, et al. The implications of respondent concurrency on sex partner risk in a national, web-based study of men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2013;63:514–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenberg ES, Sullivan PS, Dinenno EA, et al. Number of casual male sexual partners and associated factors among men who have sex with men: results from the National HIV Behavioral Surveillance system. BMC Public Health. 2011;11:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wall KM, Stephenson R, Sullivan PS. Frequency of sexual activity with most recent male partner among young, Internet-using men who have sex with men in the United States. J Homosex. 2013;60:1520–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pew Research Center. 15% ofAmerican Adults Have Used Online Dating Sites or Mobile Dating Apps. Washington, DC: Pew Research Center; 2016. [Google Scholar]
- 27.Nelson KM, Gamarel KE, Pantalone DW, et al. Sexual debut and HIV-related sexual risk-taking by birth cohort among men who have sex with men in the United States. AIDS Behav. 2016;20:2286–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stephenson R, Sullivan PS, Salazar LF, et al. Attitudes towards couples-based HIV testing among MSM in three US cities. AIDS Behav. 2011; 15(suppl 1):S80–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sullivan PS, White D, Rosenberg ES, et al. Safety and acceptability of couples HIV testing and counseling for US men who have sex with men: a randomized prevention study. JInt Assoc Provid AIDS Care. 2014;13:135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Testing together. 2017. Available at: https://effectiveinterventions.cdc.gov/en/HighImpactPrevention/PublicHealthStrategies/testing-together. Accessed November 8, 2017.
- 31.Hoff CC, Beougher SC. Sexual agreements among gay male couples. Arch Sex Behav. 2010;39:774–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.