Abstract
OBJECTIVE
To examine the effects of two Mediterranean eating plans (Med-EatPlans) versus a low-fat eating plan on the need for glucose-lowering medications.
RESEARCH DESIGN AND METHODS
From the Prevención con Dieta Mediterránea (PREDIMED) trial, we selected 3,230 participants with type 2 diabetes at baseline. These participants were randomly assigned to one of three eating plans: Med-EatPlan supplemented with extra-virgin olive oil (EVOO), Med-EatPlan supplemented with mixed nuts, or a low-fat eating plan (control). In a subgroup (15%), the allocation was done in small clusters instead of using individual randomization, and the clustering effect was taken into account in the statistical analysis. In multivariable time-to-event survival models, we assessed two outcomes: 1) introduction of the first glucose-lowering medication (oral or injectable) among participants on lifestyle management at enrollment and 2) insulin initiation.
RESULTS
After a median follow-up of 3.2 years, in multivariable analyses adjusting for baseline characteristics and propensity scores, the hazard ratios (HRs) of starting a first glucose-lowering medication were 0.78 (95% CI 0.62–0.98) for Med-EatPlan + EVOO and 0.89 (0.71–1.12) for Med-EatPlan + nuts, compared with the control eating plan. After a median follow-up of 5.1 years, the adjusted HRs of starting insulin treatment were 0.87 (0.68–1.11) for Med-EatPlan + EVOO and 0.89 (0.69–1.14) for Med-EatPlan + nuts compared with the control eating plan.
CONCLUSIONS
Among participants with type 2 diabetes, a Med-EatPlan + EVOO may delay the introduction of new-onset glucose-lowering medications. The Med-EatPlan did not result in a significantly lower need for insulin.
Introduction
Diabetes has reached epidemic proportions, and this disease is at the forefront of public health problems, affecting 451 million people worldwide in 2017 (1). More than 90% of patients with diabetes have type 2 diabetes (2). The attainment and maintenance of good glycemic control reduces the risk of long-term complications of type 2 diabetes (3). However, glucose levels increase over the natural history of type 2 diabetes (4,5), and this progressive nature of the disease usually requires the sequential addition of glucose-lowering medications (5).
A healthful eating pattern, such as the Mediterranean eating plan (Med-EatPlan), is a key component of type 2 diabetes management (6,7). The traditional Mediterranean pattern is characterized by a high intake of olive oil, fruits, vegetables, nuts, and cereals; a moderate intake of fish and poultry; a low intake of red meat, whole-fat diary, and sweet desserts; and wine consumption with meals is allowed in moderation (8). Well-conducted and analyzed prospective cohorts (9,10) have consistently supported the effectiveness of the Med-EatPlan for reducing the incidence of type 2 diabetes, and a large intervention study, the Prevención con Dieta Mediterránea (PREDIMED) trial, showed that a Med-EatPlan supplemented with either extra-virgin olive oil (EVOO) or mixed nuts was superior to a low-fat diet for the prevention of type 2 diabetes (11,12). Previously, a trial conducted in patients with newly diagnosed type 2 diabetes found that compared with a low-fat diet, an energy-restricted Med-EatPlan allows for better glycemic control and delays the need for new-onset glucose-lowering medications (13). However, the potential preventive role of the Med-EatPlan for delaying the progression of type 2 diabetes, without energy restriction, weight loss, or other lifestyle interventions, has not been assessed in a clinical trial.
In this subgroup analysis of the PREDIMED trial, we tested the effect of the two supplemented Med-EatPlans on the need for a first glucose-lowering medication (either oral or injectable) compared with a low-fat (control) eating plan among trial participants with type 2 diabetes who did not require glucose-lowering medication at enrollment. In addition, we separately assessed the initiation of insulin treatment as a second outcome.
Research Design and Methods
The PREDIMED study was designed as a parallel-group, multicenter, randomized trial. It was conducted in Spain to assess the effects of two Med-EatPlans versus a low-fat control eating plan on the primary prevention of cardiovascular disease in adults at high risk but without previously documented cardiovascular disease at baseline. Detailed methods of the trial have been published previously (14,15) and are available at www.predimed.es.
The trial was conducted in 11 recruiting centers affiliated with 11 Spanish university hospitals. A total of 7,447 participants underwent randomization from October 2003 through June 2009. Eligible participants were men (55–80 years of age) and women (60–80 years of age) free of cardiovascular disease at enrollment who had either type 2 diabetes or at least three of the following major cardiovascular risk factors: current smoking, hypertension, elevated LDL cholesterol levels, low HDL cholesterol levels, overweight or obesity, or a family history of premature coronary heart disease. Detailed enrollment criteria have been published previously (14,15). The protocol was approved by the institutional review boards at all study locations. All participants provided written informed consent.
The protocol specified that participants were to be randomized in a 1:1:1 ratio to one of three dietary interventions: a Med-EatPlan supplemented with EVOO (Med-EatPlan + EVOO), a Med-EatPlan supplemented with mixed nuts (Med-EatPlan + nuts), or a control eating plan that consisted of advice to reduce intake of all types of fat. Allocation concealment was achieved by using closed envelopes during part of the pilot phase of the study, but envelopes were not used for the rest of the study. A computer-generated random number sequence provided randomization tables for 11 study sites, which included 169 clinics. These tables had four strata (women <70 years of age, women ≥70 years of age, men <70 years of age, and men ≥70 years of age). In a subset of participants (15% of the participants with type 2 diabetes), there were deviations from the randomization procedures as reported in detail elsewhere (15). To summarize, participants who lived in the same household of previously randomized participants (usually their spouses) were assigned to the same intervention (since enrollment) as their spouses already in the trial. In addition, a subgroup of 311 participants of 1 of the 11 participating sites (site D) were not individually randomized but, instead, were assigned in small clusters according to the clinic where they belonged (i.e., all adults in the same clinic received the same intervention).
Participants assigned to the Med-EatPlan + EVOO received 1 L of EVOO per week for free, and they were recommended to meet the goal of consuming at least 4 tablespoons/day. Participants allocated to the Med-EatPlan + nuts received 30 g/day of mixed nuts (15 g walnuts, 7.5 g hazelnuts, and 7.5 g almonds), also at no cost. Participants in the control group received small nonfood gifts. Neither energy restriction nor increased physical activity was promoted for any of the study groups.
A general medical questionnaire, a 137-item validated food frequency questionnaire (16), and the validated Spanish version of the Minnesota Leisure Time Physical Activity Questionnaire were administered at randomization and yearly thereafter (14). Information from the food frequency questionnaire was used to calculate energy and nutrient intake. Weight, height, and waist circumference were directly measured (17).
For participants in the two Med-EatPlan groups, dietitians ran individual and group dietary training sessions at the baseline visit and quarterly thereafter. In each session, a validated 14-item dietary questionnaire was used to estimate adherence to either of the Med-EatPlans (18). The answers to these questionnaires were used as a tool to tailor the intervention for each participant and to negotiate changes to upgrade participants’ adherence. Participants in the control group also received dietary training at the baseline visit and completed the 14-item dietary questionnaire used to examine baseline adherence to Med-EatPlan. Through October 2006, participants in the control group received only a leaflet describing the low-fat eating plan. Thereafter, participants assigned to the control eating plan also received personalized advice and were invited to group sessions with the same frequency and intensity as those in the Med-EatPlan groups. A separate nine-item dietary questionnaire was used to assess adherence to the control eating plan. During follow-up, scores on the 14-item Med-EatPlan questionnaire increased for the participants randomized to the two Med-EatPlan groups (15,19). Biomarkers also showed that the intervention changed the overall dietary pattern of participants. Specifically, adherence to the Med-EatPlan + EVOO intervention was examined by measuring urinary hydroxytyrosol (a biomarker of EVOO consumption), and adherence to the Med-EatPlan + nuts intervention was examined by measuring the plasma proportion of α-linolenic acid (a fatty acid characteristic of walnuts). The blood and urine samples were taken at 1, 3, and 5 years of follow-up in random subsamples of participants (15).
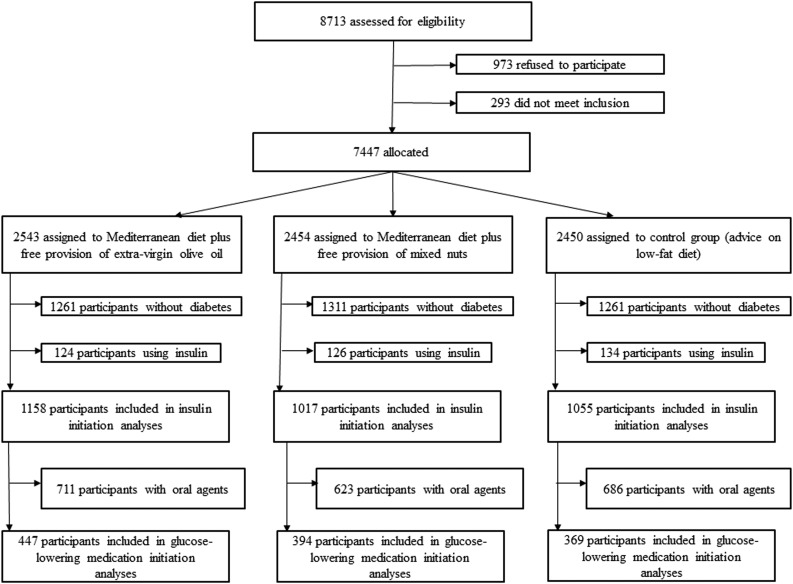
Among the initial 7,447 participants of the total PREDIMED trial, we excluded those without diabetes at baseline (n = 3,833). We also excluded participants who received insulin at enrollment (n = 384). Finally, the current study included data only on participants with type 2 diabetes and not using insulin at baseline (n = 3,230). Among these 3,230 participants, 2,020 were receiving at least one oral agent at baseline and were excluded in the analyses of new-onset glucose-lowering medications (Fig. 1).
Figure 1.
Study flowchart.
In the time-to-event analyses, we assessed two outcomes: 1) introduction of the first glucose-lowering medication (oral or injectable) among participants on only lifestyle management at enrollment and 2) insulin initiation. During the trial, participants’ physicians adjusted glucose-lowering medications at their discretion to achieve individually appropriate glycemic targets. Glucose-lowering medications were obtained from the questionnaires completed by the participants at baseline and yearly thereafter. Nurses and research assistants who collected this information were blinded with respect to the hypotheses of the current study. Other investigators assessing the outcomes were also blinded to these hypotheses.
Statistical Analysis
All analyses were performed on an intention-to-treat basis. We assessed the effect of the intervention on the need for glucose-lowering medications fitting Cox proportional hazard regression models. Hazard ratios (HRs) and their 95% CIs were calculated, considering the control group as the reference. Person-years of follow-up were calculated from baseline to the earliest event (glucose-lowering medication), loss to follow-up, or end of follow-up (December 1, 2010). We repeated the analyses using insulin initiation as the dependent variable.
To address the small departures from individual randomization in a subset of participants, we conducted analyses that did not assume that all the participants were randomly allocated and that randomization would distribute baseline characteristics of the participants equally across intervention groups. Thus, in addition to the crude model, in a subsequent multivariable model, we stratified by sex, age (deciles), recruiting center, and educational level (five categories) and adjusted for propensity scores that used 30 baseline variables to estimate the probability of assignment to each of the intervention groups. The model was also adjusted for hypertension (yes/no), dyslipidemia (yes/no), smoking status (never smoked, former smoker, or current smoker), BMI (continuous), waist-to-height ratio (continuous), leisure time physical activity (continuous), and total energy intake (continuous). For the assessment of the second outcome, namely insulin initiation, the models were also adjusted for baseline oral agents (yes/no). Robust variance estimators were used to account for intracluster correlation in Cox models, considering as clusters the members of the same household and the participants in the same clinic of site D allocated in clusters. As a sensitivity analysis, we removed participants whose randomization procedures had deviated from protocol: second members of the same household and all participants from site D. We repeated all analyses after merging the two Med-EatPlan groups and assessed their effect compared with the control group. We used the Kaplan-Meier method to describe the probability of remaining free of glucose-lowering medications and Nelson-Aalen incidence curves to estimate the probability of requiring insulin therapy during follow-up.
All P values are two-tailed at the <0.05 level. We used Stata version 12.0 statistical software.
Results
We assessed 1,158, 1,017, and 1,055 participants from the Med-EatPlan + EVOO, the Med-EatPlan + nuts, and the control eating plan, respectively. These 3,230 participants had type 2 diabetes and were not treated with insulin at enrollment. Baseline characteristics were well balanced in the three study groups without any clinically significant between-group differences (Table 1). Perhaps the only exception was the lower proportion of women (absolute difference 6%) in the Med-EatPlan + nuts group compared with the control group. In any case, we always adjusted for sex.
Table 1.
Baseline characteristics of participants according to intervention arm
| Variable | Med-EatPlan + EVOO (n = 1,158) | Med-EatPlan + nuts (n = 1,017) | Control eating plan (n = 1,055) |
|---|---|---|---|
| Age (years), mean (SD) | 67.5 (6.2) | 67.1 (6.1) | 67.7 (6.5) |
| Female sex, n (%) | 635 (54.8) | 481 (47.3) | 562 (53.3) |
| BMI (kg/m2) | |||
| Mean (SD) | 29.7 (3.8) | 29.7 (3.9) | 30.2 (4.3) |
| <25, n (%) | 116 (10.0) | 105 (10.3) | 92 (8.7) |
| 25–30, n (%) | 519 (44.8) | 448 (44.1) | 454 (43.0) |
| >30, n (%) | 523 (45.2) | 464 (45.6) | 509 (48.3) |
| Body weight (kg), mean (SD) | 76.3 (11.8) | 77.1 (12.0) | 77.2 (12.7) |
| Married, n (%) | 921 (79.5) | 783 (77.0) | 790 (74.9) |
| Smoking status, n (%) | |||
| Never | 714 (61.7) | 581 (57.1) | 646 (61.2) |
| Former | 301 (26.0) | 308 (30.3) | 280 (26.5) |
| Current | 143 (12.4) | 128 (12.6) | 129 (12.2) |
| Waist circumference (cm), mean (SD) | 101 (10) | 101 (10) | 102 (11) |
| Waist-to-height ratio, mean (SD) | 0.63 (0.06) | 0.63 (0.06) | 0.64 (0.07) |
| Hypertension, n (%) | 847 (73.1) | 722 (71.0) | 793 (75.2) |
| Dyslipidemia, n (%) | 685 (59.2) | 600 (59.0) | 621 (58.9) |
| Medication use, n (%) | |||
| Oral glucose-lowering medications | 711 (61.4) | 623 (61.3) | 686 (65.0) |
| Lipid-lowering drugs | 545 (47.1) | 456 (44.8) | 495 (46.9) |
| Antihypertensive agents | 774 (66.8) | 651 (64.0) | 708 (67.1) |
| Leisure time physical activity level (MET min/day), mean (SD) | 233 (236) | 257 (258) | 226 (261) |
Data are mean ± SD or n (%). BMI is weight in kilograms divided by the square of height in meters. The waist-to-height ratio is waist circumference divided by height. Hypertension was defined as a systolic blood pressure of ≥140 mmHg, a diastolic blood pressure of ≥90 mmHg, or the use of antihypertensive therapy. Dyslipidemia was defined as an LDL cholesterol level >160 mg/dL (4.1 mmol/L), an HDL cholesterol level of ≤40 mg/dL (1.0 mmol/L) in men or ≤50 mg/dL (1.3 mmol/L) in women, or the use of lipid-lowering therapy.
During follow-up, the mean scores on the 14-item Med-EatPlan questionnaire increased in both Med-EatPlan groups and were higher than in the control group (Supplementary Fig. 1). Supplementary Table 1 shows the mean nutrient changes in the three groups.
After a median follow-up of 3.2 years, 686 participants with only lifestyle management at baseline started glucose-lowering medications (576 participants started an oral agent, 37 participants started long-term insulin, and 73 participants started both an oral agent and insulin at the same time). After a median follow-up of 5.1 years, a total of 407 insulin-naïve participants at baseline started long-term insulin therapy.
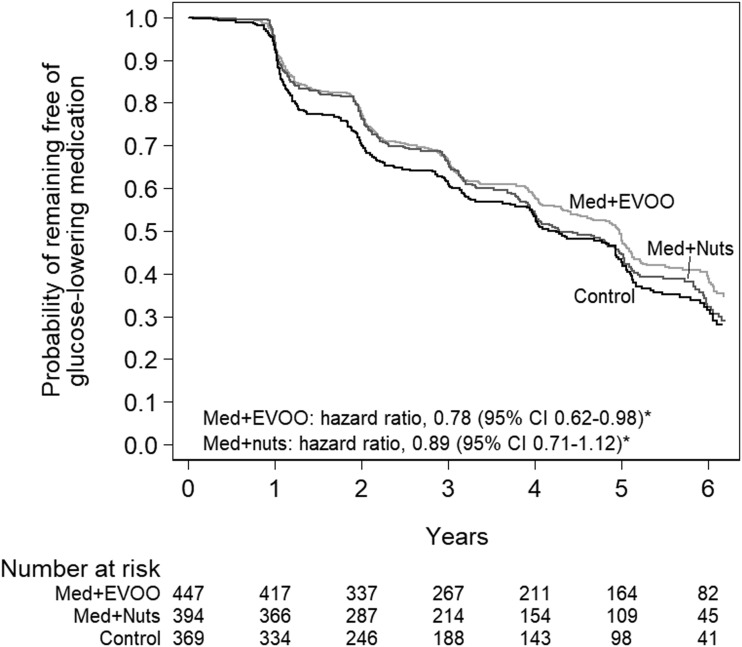
Figure 2 shows the probability of remaining free of glucose-lowering medications in the three groups. The unadjusted HRs of starting glucose-lowering medications were 0.83 (95% CI 0.69–0.99) for a Med-EatPlan + EVOO and 0.92 (0.76–1.11) for a Med-EatPlan + nuts compared with the control eating plan. When we assessed the two Med-EatPlan groups together, the HR of starting glucose-lowering medication was 0.87 (0.74–1.02). The multivariable-adjusted HRs, including adjustments for propensity scores, of starting glucose-lowering medications were 0.78 (0.62–0.98) for Med-EatPlan + EVOO and 0.89 (0.71–1.12) for Med-EatPlan + nuts compared with the control eating plan. When both Med-EatPlan groups were merged together, we found an HR of 0.83 (0.68–1.02). In a sensitivity analysis, when we excluded second members of the same household (56 participants) and all participants from site D (141 participants), the results with 1,013 individuals aligned with the findings of the adjusted model. The adjusted HR for both Med-EatPlan groups merged together was 0.85 (0.69–1.05). After 1-year follow-up, a 1-unit increase in the score on the 14-item Med-EatPlan questionnaire was associated thereafter with an adjusted HR of starting glucose-lowering medication of 0.98 (0.92–1.05).
Figure 2.
Kaplan-Meier estimate of the probability of remaining free of glucose-lowering medications. *The Cox model was stratified according to sex, age (deciles), recruiting center, and educational level (five categories) and adjusted for propensity scores that used 30 baseline variables to estimate the probability of assignment to each of the intervention groups. The model was also adjusted for hypertension (yes/no), dyslipidemia (yes/no), smoking status (never smoked, former smoker, or current smoker), BMI (continuous), waist-to-height ratio (continuous), leisure time physical activity (continuous), and total energy intake (continuous). Robust SEs to account for intracluster correlations were used. Med, Med-EatPlan.
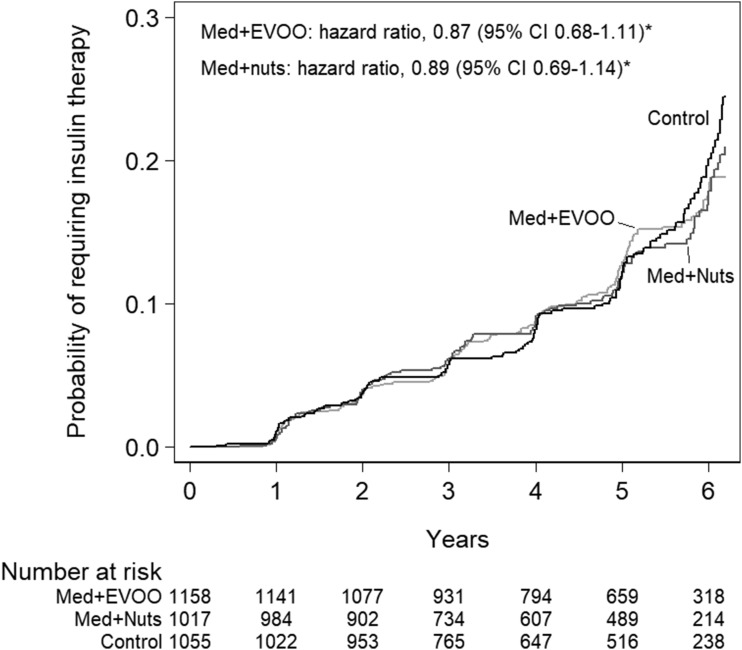
Figure 3 shows the probability of remaining free of insulin in the three groups. The unadjusted HRs of starting long-term insulin treatment were 0.90 (95% CI 0.72–1.14) for Med-EatPlan + EVOO and 0.91 (0.71–1.16) for Med-EatPlan + nuts compared with the control eating plan. When we assessed the two Med-EatPlan groups together, the HR of starting glucose-lowering medication was 0.91 (0.74–1.11). The propensity score and multivariable-adjusted HRs of starting long-term insulin treatment were 0.87 (0.68–1.11) for Med-EatPlan + EVOO and 0.89 (0.69–1.14) for Med-EatPlan + nuts, using the control eating plan as the reference. The adjusted HR for the Med-EatPlan groups (both groups merged vs. the control group) was 0.88 (0.71–1.09). After excluding second members of the same household and all participants from site D (165 and 311, respectively), the analysis with 2,754 individuals showed an adjusted HR, for both Med-EatPlan combined versus the control eating plan group, of 0.92 (0.73–1.16). After 1-year follow-up, a 1-unit increase in the score on the 14-item Med-EatPlan questionnaire was associated thereafter with an adjusted HR of starting insulin of 0.95 (0.88–1.01). The mean fasting blood glucose level was 145 ± 40 mg/dL at baseline and 143 ± 42 mg/dL after 5 years in the Med-EatPlan + EVOO group, 144 ± 42 mg/dL at baseline and 140 ± 37 mg/dL after 5 years in the Med-EatPlan + nuts, and 147 ± 43 mg/dL at baseline and 146 ± 46 mg/dL after 5 years in the control group.
Figure 3.
Nelson-Aalen estimate of the probability of requiring insulin therapy. *The Cox model was stratified according to sex, age (deciles), recruiting center, and educational level (five categories) and adjusted for propensity scores that used 30 baseline variables to estimate the probability of assignment to each of the intervention groups. The model was also adjusted for hypertension (yes/no), dyslipidemia (yes/no), smoking status (never smoked, former smoker, or current smoker), BMI (continuous), waist-to-height ratio (continuous), leisure-time physical activity (continuous), total energy intake (continuous), and oral agents (yes/no). Robust SEs to account for intracluster correlations were used. Med, Med-EatPlan.
Conclusions
In this trial, a Med-EatPlan supplemented with EVOO without any caloric restriction or weight-loss goals, but not a Med-EatPlan supplemented with nuts, significantly decreased the need of new-onset pharmacologic interventions, compared with a control eating plan, in participants with type 2 diabetes and no cardiovascular disease at enrollment after a median follow-up of 3.2 years. A Med-EatPlan + EVOO or nuts did not result in a lower rate of insulin initiation after a median follow-up of 5.1 years.
The lower need of starting a first glucose-lowering medication (either oral or injectable) with the Med-EatPlan + EVOO probably reflects the better glycemic control of this group during the long follow-up of the PREDIMED study, and for this reason, a first treatment was prescribed less often to achieve or maintain glycemic goals. The favorable effect was likely due to the overall composition of the dietary pattern and not to decreased caloric intake, increased physical activity, or weight loss because such lifestyle interventions were not part of the PREDIMED trial, and there were no notable between-group differences in these characteristics at baseline or during follow-up (20). In particular, after adjustment for propensity scores and use of robust variance estimators, the average difference in body weight change at 5 years in the Med-EatPlan + EVOO group was −0.41 kg (95% CI −0.83 to 0.01 kg), and in the Med-EatPlan + nuts group, it was −0.02 kg (−0.45 to 0.42 kg) compared with the control group (20). In addition, no between-group difference in body weight was found in participants with baseline diabetes (20).
Previously, the PREDIMED trial reported a significant reduction in the risk of type 2 diabetes among participants without diabetes at baseline (11,12,21). In a meta-analysis of prospective studies published between 2007 and 2014, including eight prospective cohort studies (122,810 subjects) and one randomized controlled trial (PREDIMED), greater adherence to a Med-EatPlan was associated with a significant 19% lower risk of type 2 diabetes (9). In agreement with these results, the initial 3-month assessment in 772 participants of the PREDIMED study found an improved fasting glucose in the Med-EatPlan groups in the absence of weight loss (22). In addition, two randomized trials also reported an improvement in glycemic control of the Med-EatPlan combined with other lifestyle strategies, such as exercise or calorie-restricted diets (23,24). In a 4-year trial (the longest to date), Esposito et al. (13) randomized 215 patients with newly diagnosed type 2 diabetes to a low-carbohydrate Mediterranean-style diet or a low-fat diet. At the end of the trial, 44% of patients in the Mediterranean-style diet group and 70% in the low-fat group required glucose-lowering medications. Participants randomized to the Med-EatPlan lost more weight. Finally, in a 12-month trial, Elhayany et al. (25) randomly assigned 259 patients with type 2 diabetes to one of three diets: low-carbohydrate Mediterranean, traditional Mediterranean, and the 2003 American Diabetes Association diet. The mean weight loss for the three diets was 10.1, 7.4, and 7.7 kg, respectively. Using as a reference the American Diabetes Association diet, Elhayany et al. reported greater reductions in HbA1c levels in participants allocated to the low-carbohydrate Mediterranean diet and the traditional Mediterranean diet (average difference changes of 0.4% and 0.2%, respectively). In a subset of the PREDIMED trial, better adherence to the Med-EatPlan was associated with lower HbA1c levels, although the observed differences were statistically nonsignificant (26). These previous results provide support to the benefits of the Med-EatPlan + EVOO that we have observed.
Med-EatPlan + nuts was also associated with a lower need of antihyperglycemic drug therapy in the point estimate, but the CIs were wider, and the upper limit was compatible with a 12% higher risk. This finding contrasts with that in the Med-EatPlan + EVOO group. The difference in the effects of the two interventions using the same Med-EatPlan as the background diet might be related to several factors. It is possible that there are differences between EVOO and nuts. A meta-analysis in patients with type 2 diabetes reported that EVOO supplementation resulted in a change in HbA1c of −0.27% (95% CI −0.37 to −0.17%) (27). Nuts have been associated with a lower risk of type 2 diabetes (28). However, the glycemic effect of nut-enriched meals may be lower in people with diabetes than in people without diabetes (29). In addition, at the end of PREDIMED, 22% of total calories in the Med-EatPlan + EVOO group were from EVOO, whereas only 8% of calories in the Med-EatPlan + nuts group were from nuts. However, the CIs for both estimates were widely overlapping.
Our results suggest a 12% lower rate of initiation of insulin in the point estimate. Nonetheless, a 30% lower risk and a 10% higher risk are also reasonably compatible with our data. This highlights possible differences among participants of PREDIMED because participants who initiated insulin therapy usually had a longer duration of diabetes and a higher HbA1c than those on lifestyle management. Differences between participants who initiated insulin and those included in diabetes prevention analyses of PREDIMED are even greater (11,12). However, other lifestyle interventions have shown a lower need of insulin in participants with diabetes. Participants randomized to intensive lifestyle intervention, focusing on weight loss, in the Look AHEAD (Action for Health in Diabetes) trial had a lower use of insulin than participants in the control group (30).
Our study has certain limitations. First, the need for glucose-lowering medications was not a prespecified end point in the PREDIMED trial. Thus, these analyses are exploratory. In addition, the analyses of this study were conducted in the subgroup of participants with type 2 diabetes. However, there is no reason to suspect that the randomization would not have worked in such a large number of participants. Second, we recruited white adults (55–80 years of age) without previously documented cardiovascular disease at baseline. Thus, the results cannot be generalized to all subjects with type 2 diabetes. Third, inherent to the design of a dietary intervention trial using a whole dietary pattern, the trial could not be double blind. In any case, participants and staff members involved in the intervention and data collection were unaware of the hypotheses of the present report. The strengths of the PREDIMED trial include the large sample size, long follow-up period, breadth of included participants with type 2 diabetes, and adjustment for a wide array of potential confounders in multivariable analyses.
In summary, our study results show that PREDIMED participants with type 2 diabetes who underwent an intervention with an energy-unrestricted Med-EatPlan + EVOO had significantly lower rates of initiation of glucose-lowering medications. Our results are compatible not only with a benefit of a Med-EatPlan + nuts in the rates of initiation of glucose-lowering medications and with a benefit of a Med-EatPlan + EVOO or nuts in the need of insulin but also with a slightly higher risk.
Supplementary Material
Article Information
Acknowledgments. The authors thank the participants for involvement in the trial, the PREDIMED personnel, and the personnel of all affiliated primary care centers.
Funding. The supplemental foods used in the study were donated by Patrimonio Comunal Olivarero and Hojiblanca, Madrid, Spain (EVOO); the California Walnut Commission, Sacramento, CA (walnuts); and Borges SA (almonds) and La Morella Nuts (hazelnuts), Reus, Spain. The PREDIMED trial was supported by Instituto de Salud Carlos III, the official funding agency for biomedical research of the Spanish government, through grants provided to research networks specifically developed for the trial (RTIC RD 06/0045 [coordinator: M.A.M.-G.] and RTIC G03/140 [coordinator: R.E.]). All investigators of the PREDIMED trial belong to CIBER, an initiative of Instituto de Salud Carlos III. The authors also acknowledge grants from the National Institutes of Health Clinical Center (1R01-HL-118264-01 and 1R01-DK-102896), Fondo de Investigación Sanitaria–Fondo Europeo de Desarrollo Regional (PI04/0233, PI05/0976, PI07/0240, PI10/01407, PI10/02658, PI11/00049, PI11/02505, and AGL2010-22319-C03-03), Consejería de Salud Junta de Andalucía (PI0105/2007), and the Generalitat Valenciana, Valencia, Spain (ACOMP/2013/165 and COMP/2013/159).
Duality of Interest. E.R. reports grants, nonfinancial support, and other fees from the California Walnut Commission; grants, personal fees, nonfinancial support, and other fees from Merck Sharp & Dohme, Alexion, and Ferrer International; personal fees, nonfinancial support, and other fees from Aegerion, Amarin, and Danone; grants and personal fees from Sanofi; and grants from Amgen and Pfizer outside of the submitted work. R.E. reports serving on the board of and receiving lecture fees from the Research Foundation on Wine and Nutrition; serving on the boards of the Beer and Health Foundation and the European Foundation for Alcohol Research; receiving lecture fees from Instituto Cerventes, Fundación Dieta Mediterránea, Cerveceros de España, Lilly Laboratories, AstraZeneca, and Sanofi; receiving consultancy fees from KAO Coorporation; and receiving grant support through his institution from Novartis, Amgen, Bicentury, and Grand Fountaine. L.S.-M. reports serving on the boards of the Mediterranean Diet Foundation and the Beer and Health Foundation. X.P. reports serving on the board of and receiving grant support through his institution from the Residual Risk Reduction Initiative Foundation; serving on the board of Omegafort; serving on the board of and receiving payment for the development of educational presentations as well as grant support through his institution from Ferrer International; receiving consulting fees from Abbott Laboratories; receiving lecture fees as well as grant support through his institution from Merck and Roche; receiving lecture fees from Danone and Esteve; receiving payment for the development of educational presentations from Menarini, Mylan, LACER, and Rubio Laboratories; and receiving grant support through his institution from Sanofi, Kowa, Unilever, Boehringer Ingelheim, and Karo Bio. F.A. reports receiving grants from Instituto de Salud Carlos III, Fondo de Investigación Sanitario (FIS), and CIBEROBN during the conduct of the study and personal fees from payment for the development of educational presentations outside the submitted work. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. F.J.B.-G., M.R.-C., M.A.M.-G., N.B., J.V.S., M.Fit., E.R., E.G.-G., M.Fio., J.L., R.E., L.S.-M., X.P., J.I.G., M.B., O.C., Á.A.-G., L.F., and F.A. revised the manuscript for important intellectual content and read and approved the final manuscript. F.J.B.-G., M.R.-C., M.A.M.-G., M.Fit., E.R., E.G.-G., M.Fio., J.L., R.E., L.S.-M., X.P., L.F., and F.A. acquired, analyzed, or interpreted data. F.J.B.-G., M.A.M.-G., and F.A. drafted the manuscript. M.A.M.-G., M.Fit., E.R., E.G.-G., M.Fio., R.E., L.S.-M., and F.A. conceived the study concept and design. M.A.M.-G., E.R., J.L., R.E., and L.S.-M. obtained funding. F.J.B.-G., M.A.M.-G., and F.A. are the guarantors of this work and, as such, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc18-2475/-/DC1.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.Cho NH, Shaw JE, Karuranga S, et al. . IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 2018;138:271–281 [DOI] [PubMed] [Google Scholar]
- 2.Xu G, Liu B, Sun Y, et al. . Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ 2018;362:k1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 4.Kahn SE, Haffner SM, Heise MA, et al.; ADOPT Study Group . Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med 2006;355:2427–2443 [DOI] [PubMed] [Google Scholar]
- 5.Turner RC, Cull CA, Frighi V, Holman RR; UK Prospective Diabetes Study (UKPDS) Group . Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). JAMA 1999;281:2005–2012 [DOI] [PubMed] [Google Scholar]
- 6.Evert AB, Boucher JL, Cypress M, et al. . Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014;37(Suppl. 1):S120–S143 [DOI] [PubMed] [Google Scholar]
- 7.Davies MJ, D’Alessio DA, Fradkin J, et al. . Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018;41:2669–2701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willett WC, Sacks F, Trichopoulou A, et al. . Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 1995;61(Suppl.):1402S–1406S [DOI] [PubMed] [Google Scholar]
- 9.Schwingshackl L, Missbach B, König J, Hoffmann G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr 2015;18:1292–1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koloverou E, Esposito K, Giugliano D, Panagiotakos D. The effect of Mediterranean diet on the development of type 2 diabetes mellitus: a meta-analysis of 10 prospective studies and 136,846 participants. Metabolism 2014;63:903–911 [DOI] [PubMed] [Google Scholar]
- 11.Salas-Salvadó J, Bulló M, Babio N, et al.; PREDIMED Study Investigators . Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2011;34:14–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salas-Salvadó J, Bulló M, Estruch R, et al. . Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Intern Med 2014;160:1–10 [DOI] [PubMed] [Google Scholar]
- 13.Esposito K, Maiorino MI, Ciotola M, et al. . Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med 2009;151:306–314 [DOI] [PubMed] [Google Scholar]
- 14.Martínez-González MÁ, Corella D, Salas-Salvadó J, et al.; PREDIMED Study Investigators . Cohort profile: design and methods of the PREDIMED study. Int J Epidemiol 2012;41:377–385 [DOI] [PubMed] [Google Scholar]
- 15.Estruch R, Ros E, Salas-Salvadó J, et al.; PREDIMED Study Investigators . Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med 2018;378:e34 [DOI] [PubMed] [Google Scholar]
- 16.Fernández-Ballart JD, Piñol JL, Zazpe I, et al. . Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr 2010;103:1808–1816 [DOI] [PubMed] [Google Scholar]
- 17.Salas-Salvadó J, Fernández-Ballart J, Ros E, et al.; PREDIMED Study Investigators . Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: one-year results of the PREDIMED randomized trial. Arch Intern Med 2008;168:2449–2458 [DOI] [PubMed] [Google Scholar]
- 18.Schröder H, Fitó M, Estruch R, et al. . A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 2011;141:1140–1145 [DOI] [PubMed] [Google Scholar]
- 19.Zazpe I, Sanchez-Tainta A, Estruch R, et al. . A large randomized individual and group intervention conducted by registered dietitians increased adherence to Mediterranean-type diets: the PREDIMED study. J Am Diet Assoc 2008;108:1134–1144; discussion 1145 [DOI] [PubMed] [Google Scholar]
- 20.Estruch R, Martínez-González MA, Corella D, et al.; PREDIMED Study Investigators . Effect of a high-fat Mediterranean diet on bodyweight and waist circumference: a prespecified secondary outcomes analysis of the PREDIMED randomised controlled trial. Lancet Diabetes Endocrinol 2019;7:e6–e17 [DOI] [PubMed] [Google Scholar]
- 21.Martínez-González MA, Salas-Salvadó J, Estruch R, Corella D, Fitó M, Ros E; PREDIMED Investigators . Benefits of the Mediterranean diet: insights from the PREDIMED study. Prog Cardiovasc Dis 2015;58:50–60 [DOI] [PubMed] [Google Scholar]
- 22.Estruch R, Martínez-González MA, Corella D, et al.; PREDIMED Study Investigators . Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med 2006;145:1–11 [DOI] [PubMed] [Google Scholar]
- 23.Toobert DJ, Glasgow RE, Strycker LA, et al. . Biologic and quality-of-life outcomes from the Mediterranean Lifestyle Program: a randomized clinical trial. Diabetes Care 2003;26:2288–2293 [DOI] [PubMed] [Google Scholar]
- 24.Shai I, Schwarzfuchs D, Henkin Y, et al.; Dietary Intervention Randomized Controlled Trial (DIRECT) Group . Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008;359:229–241 [DOI] [PubMed] [Google Scholar]
- 25.Elhayany A, Lustman A, Abel R, Attal-Singer J, Vinker S. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1-year prospective randomized intervention study. Diabetes Obes Metab 2010;12:204–209 [DOI] [PubMed] [Google Scholar]
- 26.Díez-Espino J, Buil-Cosiales P, Serrano-Martínez M, Toledo E, Salas-Salvadó J, Martínez-González MÁ. Adherence to the Mediterranean diet in patients with type 2 diabetes mellitus and HbA1c level. Ann Nutr Metab 2011;58:74–78 [DOI] [PubMed] [Google Scholar]
- 27.Schwingshackl L, Lampousi AM, Portillo MP, Romaguera D, Hoffmann G, Boeing H. Olive oil in the prevention and management of type 2 diabetes mellitus: a systematic review and meta-analysis of cohort studies and intervention trials. Nutr Diabetes 2017;7:e262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang R, Manson JE, Stampfer MJ, Liu S, Willett WC, Hu FB. Nut and peanut butter consumption and risk of type 2 diabetes in women. JAMA 2002;288:2554–2560 [DOI] [PubMed] [Google Scholar]
- 29.Kendall CW, Esfahani A, Josse AR, Augustin LS, Vidgen E, Jenkins DJ. The glycemic effect of nut-enriched meals in healthy and diabetic subjects. Nutr Metab Cardiovasc Dis 2011;21(Suppl. 1):S34–S39 [DOI] [PubMed] [Google Scholar]
- 30.Wing RR, Bolin P, Brancati FL, et al.; Look AHEAD Research Group . Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes [published correction appears in N Engl J Med 2014;370:1866]. N Engl J Med 2013;369:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.