Abstract
Background
The aim of this systematic review and meta-analysis was to evaluate the clinical use of MRI for the evaluation of acute appendicitis during pregnancy.
Methods
The searches were conducted by two independent researchers (MK, MS) to find the relevant studies published from 1/1/2009 until end of 30/12/2018. We searched for published literature in the English language in MEDLINE via PubMed, EMBASETM via Ovid, The Cochrane Library, and Trip database. For literature published in other languages, we searched national databases (Magiran and SID), KoreaMed, and LILACS. The keywords used in the search strategy are Pregnancy [MeSH], Pregnant [MeSH] OR—Magnetic resonance imaging [MeSH] OR—Appendicitis [MeSH] OR—Ultrasound, [MeSH] OR, imaging, MRI [MeSH] OR"،" and Right lower quadrant pain [MeSH]. The risk of bias of every article was evaluated by using QUADAS-2. On the basis of the results from the 2 × 2 tables, pooled measures for sensitivity, specificity, diagnostic odds ratio (DOR), and area under the curves (AUC) along with their 95% confidence intervals (CIs) were calculated using the DerSimonian Lair methodology.
Results
As many as 1164 studies were selected. After analyzing the correspondence of the studies with the required criteria, 19 studies were selected for the final review. For appendicitis in pregnancy, the MRI sensitivity was 91.8% at the 95% confidence interval of (95% CI 87.7–94.9%). At the confidence interval of 95%, the specificity was 97.9% (95% CI 0.97.2–100%). The risk of bias in the studies conducted was measured using the QUADAS-2 tool.
Conclusion
MRI has high sensitivity and specificity (91.8%, 97.9% respectively) for the diagnosis of acute appendicitis in pregnant patients with clinically suspected appendicitis. It is an excellent imaging technique in many instances, which does not expose a fetus, or the mother, to ionizing radiation, making it an excellent option for pregnant patients with suspected acute appendicitis.
Keywords: Pregnancy, Acute appendicitis, Magnetic resonance imaging (MRI)
Background
Approach to acute pain in the right lower quadrant in pregnancy is a challenge; It has various causes including digestive, gynecological and obstetrical, and renal causes. The possibility of acute appendicitis must be specifically ruled out, since it is the most common cause of surgical intervention in pregnancy requires immediate management [1–7]. The incidence rate of acute appendicitis in pregnancy has been reported to be 1:1250 and 1:1500 [8–15]. The possibility of acute appendicitis is higher in the second and third decades of life which are the fertility years [16–18]. Accurate diagnosis is difficult because the typical diagnostic clinical images are not present in all of the cases [19–25]. As the gestational age increases, the accuracy of the diagnosis decreases and the likelihood of appendical perforation and other complications will increase [26–29]. The negative laparotomy rate of suspected appendicitis is 25–50% in obstetric cases and 15–35% in general surgical cases [30–36]. Imaging in combination with physical examination will reduce the negative results of appendectomies [37–40]. Previous studies have indicated that CT (computed tomography) scan has better sensitivity and efficiency in comparison to US (ultrasound) [41–43]. Moreover, these studies have shown the high failure rate of US in diagnosing the disease even in patients whose appendicitis had been already confirmed by other imaging techniques [44–47]. The common usage of CT has been confirmed for evaluating patients suspected of appendicitis with reports on reduced healthcare costs for each patient and reduced rate of unnecessary appendectomy [48–52]. However, the fact that CT is applying ionizing radiation is worrying for both fetuses and pregnant women during the imaging process. Moreover, intravenous contrast is applied for increasing the diagnosis accuracy of CT, and it is associated with increased allergic reactions and contrast-inducted nephropathy. The changes made into the CT protocol can reduce exposure to fetal radiation less than 3 mGy, which is lower than the doses inducing adverse fetal effects [15, 53] mGy for the risk of carcinogenesis, 50 mGy for deterministic effects) [16, 54, 55]. However, CT is recommended in cases when inclusive clinical findings and ultrasound results are obtained or in situations in which MRI is not accessible. Thus, following the initial negative result of US, the American College of Radiology has introduced MRI (magnetic resonance imaging) as the recommended treatment [15, 16]. Therefore, the present systematic review and meta-analysis has been conducted to investigate the sensitivity,specificity, and diagnostic accuracy of MRI in diagnosing acute appendicitis in pregnant women.
Methods
Presenting a systematic review and meta-analysis based on PRISMA [26] principles.
Search methods for eligible studies
Searching for the eligible studies was conducted from 1/1/2009 to the end of 30/12/2018 by using the following searching strategy:
The searches were conducted by two independent researchers (MK, MS) to find the relevant studies published from 1/1/2009 to the end of 30/12/2018. We searched for published literature in the English language in MEDLINE via PubMed and EMBASETM via Ovid, The Cochrane Library, and Trip database. For literature published in other languages, we searched national databases (Magiran and SID), KoreaMed, and LILACS. To ensure literature saturation, the list of the included research references or the relevant reviews found by searching was studied (FP). The special search strategies were created using the Health Sciences Librarian website with specialization in systematic review searches using the MESH phrases and open phrases in accordance with the PRESS standards. After finalizing the MEDLINE strategy, the results were compared with searches from other databases (MS, FP). Similarly, PROSPERO was searched to find recent or ongoing systematic reviews. The keywords used in the search strategy were Pregnancy [MeSH], Pregnant [MeSH] OR—Magnetic resonance imaging [MeSH] OR—Appendicitis [MeSH] OR—Ultrasound, [MeSH] OR, imaging, MRI [MeSH] OR"،" , and Right lower quadrant pain [MeSH]. The list of previous study resources and systematic reviews were also searched for identifying the published studies (MK, MS). In addition, it was attempted to contact the authors of all studies that met the inclusion criteria and request unpublished data and abstracts (FP).
Eligibility criteria
The inclusion criteria we used to select articles are as follows: (a) original retrospective and prospective blinded studies investigating the performance of MRI for appendicitis diagnosis in suspected pregnant women presenting with right lower quadrant pain; (b) using laparaoscopy open surgery or histopathologic examination as the standard reference, (c) containing a 2 × 2 table or included data that allowed the construction of a 2 × 2 table, (d) Described the diagnostic criteria for appendicitis on MRI in clear details, and (e) met quality standards, as assessed by the 14-item Quality Assessment of Diagnostic Accuracy Studies (QUADAS2) tool.
Data extraction and risk of bias evaluation
The data were extracted for evaluating the characteristics of the participants. The index test included characteristics including special equipment, reference standard (executor of the tests and the interval between tests). The information related to diagnosis accuracy was also extracted. The first reader extracted the data (MS). The second reader confirmed the data (MK), and he would have completed them if they were incomplete.
The risk of bias of every article was evaluated using QUADAS-2 (a revised tool for quality assessment of diagnostic accuracy studies); four possible domains of bias results are evaluated. The first domain is patient selection (selecting the participants based on sequence or random). The participants of the present study are required to have the test conditions. Thus, the risk of bias is high in the studies; only participants suspected of appendicitis were selected. The second domain is the index test (wrong interpretation of the index test, accurate explanation of detection threshold). The third domain is the reference standard or “golden standard” (99% accuracy, the interpretation without considering the results of the index test). The last domain is the flow and timing (describing the patients receiving the index test, the time interval between index tests, and reference standard). Two reviewers evaluated the article independently with QUADAS-2 criteria (MS, FP). After independent evaluations, the reviewers discussed the article. Each domain was discussed to achieve a single view. The reliability of the reviewers for each domain was measured by using κ-statistic.
Statistical analysis
On the basis of the results from the 2 × 2 tables, pooled measures for sensitivity, specificity, diagnostic odds ratio (DOR), and area under the curves (AUC) along with their 95% confidence intervals (CIs) were calculated using the DerSimonian Lair methodology [56]. Based on the pooled DOR of each index, test summary receiver–operator curves (sROC) were reconstructed using Moses–Shapiro–Littenberg methodology [57]. The DOR reflects the ability of a test to detect, in this case, appendicitis. A DOR of 1 indicates that the test has no discriminative power. The higher the DOR, the better the diagnostic ability of the imaging modality. To evaluate heterogeneity between studies, a Cochran Q statistic and the I2 index was used. A substantial I2 index indicates heterogeneity beyond sampling variation. A meta-regression analysis was performed to identify pre-defined sources of heterogeneity. We constructed the forest plots with the freeware Meta-DiSc, version 1.4, software (http://www.hrc.es/investigacion/ metadisc-en.htm; Ramon y Cajal Hospital; Madrid, Spain) [58]. The data related to the diagnostic accuracy of ultrasound were collected for providing a complete analysis. Then, for each of the categories, some studies were meta-analyzed; these studies had high and low risk of bias of participant selection (based on QUADAS-2 criteria). Sensitivity, specificity, and positive and negative likelihood ratios (LRs) were computed based on the true-positive, true-negative, false-positive, and false-negative rates for each study. Both LRs are independent from prevalence rates, and there is a consensus that a positive LR > 10 and a negative LR < 0.1 provide reliable evidence of satisfactory diagnostic performance [59]. The ratio of positive LR to negative LR was combined in a single global accuracy measure, the diagnostic odds ratio [60]. Summary sensitivity and specificity, positive and negative LRs, and diagnostic odds ratios were estimated by using a bivariate random effects model. This approach assumes bivariate normal distributions for the logit transformations of sensitivity and specificity from individual studies [61, 62]. In addition, the hierarchical summary receiver–operating characteristic (ROC) curve presenting the point estimates for each study, the joint ROC curve, and the pooled characteristics, including the 95% confidence region and the 95% prediction region, was constructed [63].
Results
Study selection
Based on the searching strategy, as many as 1164 studies were selected. After analyzing the correspondence of the studies with the required criteria, 19 studies were selected for the final review (Fig. 1).
Fig. 1.
PRISMA flow diagram
Characteristics of the studies
The required characteristics of each selected study are indicated in Table 1. In total, 2400 patients (2400 pregnant women suspected of appendicitis presenting with right lower quadrant pain) were investigated in 19 studies. From these 19 studies, as many as 17 studies (94.7%) were retrospectives studies, and 2 studies (5.2%) were prospective studies. The investigated population were pregnant women suspected of appendicitis. The patients’ age ranged from 16 to 47 years. Seventeen studies applied 1.5-T MRI. Other studies have applied lower MRI field strength, and some have not reported it. From 2400 patients, 996 patients were evaluated with a magnetic strength of larger than 1 T. The MRI images obtained from all of the studies have been analyzed by an experienced radiologist which in most of the cases was a fellowship-trained attending radiologist.
Table 1.
Summary of included studies
| Author | Year | Country/province | Sampling method | Study design | Study duration | Setting | Mode of data collection | Participants | Age mean ± SD or range | Study population | Image interpretation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Theileu [64] | 2014 | USA | Convenience | Retrospective | 2007–2012 | Hospital | Interview | 171 | – | Pregnant women with suspected appendicitis | Board-certified attending |
| Ramaling am [65] | 2015 | USA | Convenience | Retropprospective | 2007–2012 | Hospital | Interview | 102 | 16–41 | Pregnant patients with acute abdominal pain | Fellowship radiologist trained in body MRI |
| Bichard [66] | 2005 | USA | Prospective | 2002–2004 | Hospital | Interview | 29 | – | Pregnant patients with acute abdominal pain | Fellowship radiologist trained in body MRI | |
| Fonseca [67] | 2014 | USA | Convenience | Retrospective | 2000–2011 | Hospital | Interview | 31 | – | Pregnant women suspected for appendicitis | Attending radiologist |
| Isra [68] | 2008 | USA | Convenience | Retroprospective | 2004–2006 | Hospital | Interview | 33 | 18–36 | Pregnant women suspected for appendicitis | Attending radiologist |
| Rap [69] | 2013 | USA | Convenience | Retroprospective | 1996–2011 | Hospital | Interview | 212 | – | Pregnant patients with acute abdominal pain | Trained abdominal radiologist |
| Jang [70] | 2011 | South Korea | Convenience | Retroprospesctive | 2008–2010 | Hospital | Interview | 18 | – | Pregnant patients with acute appendicitis | Experienced gastrointestinal radiologist |
| Masselli [71] | 2011 | Italy | purposive | prospective | 2006-2010 | Hospital | Interview | 40 | 20-35 | pregnant patients with acute Abdominal and pelvic pain | Experienced radiologist in body MRI |
| Vu [72] | 2009 | Canada | Purposive | Retroprospective | 2004–2008 | Hospital | Interview | 19 | 22–39 | Pregnant patients with acute abdominal pain | Radiologist reponsible for reviewing abdominal MRI |
| Pedrosu [73] | 2009 | USA | Purposive | Retropresctive | 2002–2007 | Hospital | Medical records | 148 | 15–42 | Pregnant patients with acute abdominal pain | Fellowship trained attending radiologist |
| Oto [74] | 2009 | USA | Purposive | Retropresctive | 2001–2007 | Hospital | Hospital | 118 | 18–40 | Pregnant patients with acute abdominal and pelvic pain | Radiologist with subspecialty in abdominal MRI |
| Cobben [75] | 2004 | The Netherlands | Purposive | Presctive | 2000–2003 | Hospital | Interview | 12 | 18–34 | Pregnant patients with acute abdominal pain | Radiologist experienced in abdominal MRI |
| Aguilera [76] | 2016 | USA | Purposive | Retropresctive | 2000–2011 | Hospital | Interview | 52 | – | Pregnant patients with acute abdominal pain | Attending radiologist |
| Konrad [77] | 2015 | USA | Convenience | Retrospective | 2009–2011 | Hospital | Interview | 140 | – | Pregnant patients with suspected acute appendicitis | Attending radiologist |
| Sungah [78] | 2016 | South Korea | Convenience | Retrospective | 2014-2016 | Hospital | Interview | 125 | – | Pregnant patients with acute abdominal pain | Experienced radiologist |
| Kereshi [79] | 2017 | USA | Convenience | Retrospective | 2010–2015 | Hospital | Interview | 204 | 17–47 | Pregnant women with suspected appendicitis | Radiology fellow or abdominal imaging attend |
| Lauren M [80] | 2015 | USA | Convenience | Retrospective | 2009–2014 | Hospital | Interview | 709 | 16–46 | Pregnant patients with acute abdominal pain | Board-certified fellowship-trained abdominal radiologist |
| Richard [81] | 2017 | USA | Convenience | Retrospective | 2007–2012 | Hospital | Interview | 223 | – | Pregnant patients with acute abdominal pain | MRI fellows on any given day |
| Darshan [82] | 2017 | Canada | Purposive | Retrospective | 2008–2015 | Hospital | Interview | 42 | 17–39 | Pregnant patients with acute abdominal pain | Fellowship trained in body MRI |
Risk of bias
The findings of QUADAS-2 assessment have been indicated in Figs. 2 and 3; they indicate that only one parameter has a low risk of bias in the assessment. The studies have two or some specific limitations (Figs. 2 and 3).
Fig. 2.

The risk of bias in the studies conducted was measured by using the QUADAS-2 tool. The risk of bias shown in Eq. 2 of the above image model (MRI) of each diagram indicate the number and percentage of studies with high (red), medium (yellow), and low (green) risk of bias in the four groups of the QUADAS-2 tool
Fig. 3.
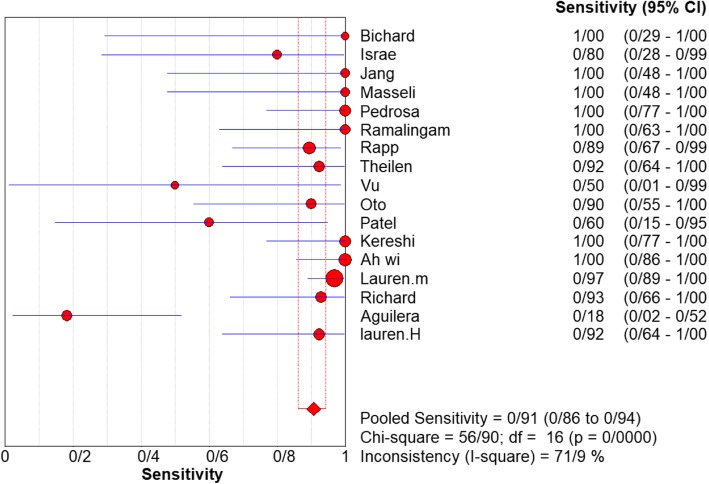
Sensitivity of MRI for diagnosing appendicitis in studies that included pregnant patients only. Forest plot of sensitivity reported in each study. Each study is identified by name of first author and year of publication, with circles representing individual study point estimates, size of each circle indicating relative contribution to data pooling (inverse variance weighting), horizontal lines indicating 95% CIs, and dashed vertical lines representing 95% CIs for pooled sensitivity and specificity
Overall meta-analysis
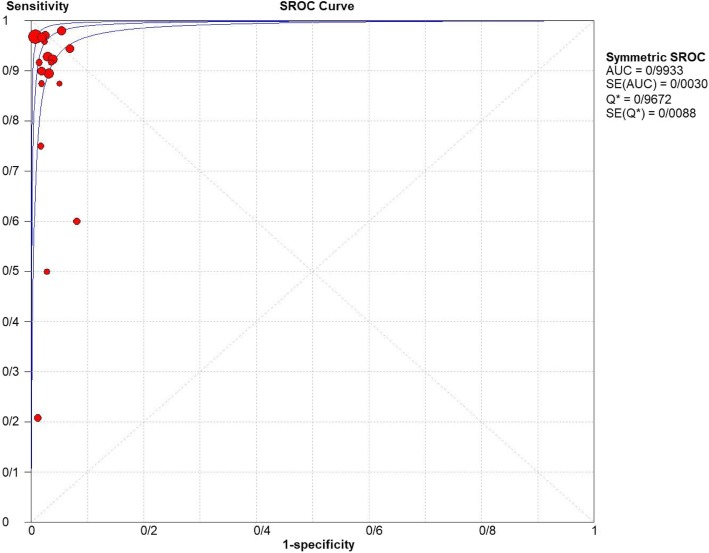
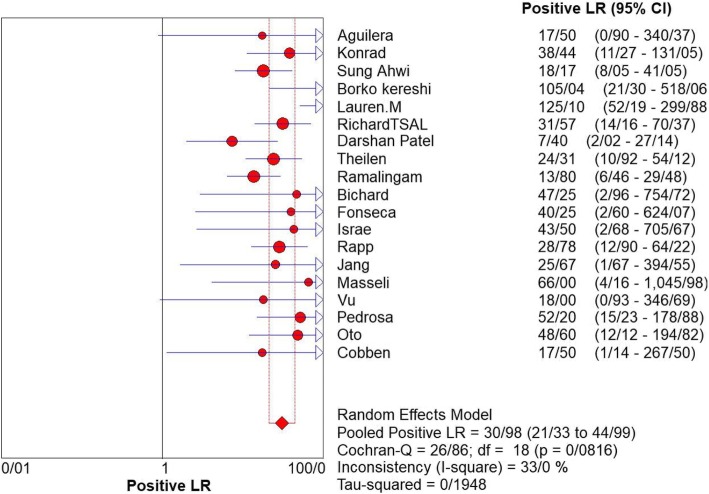
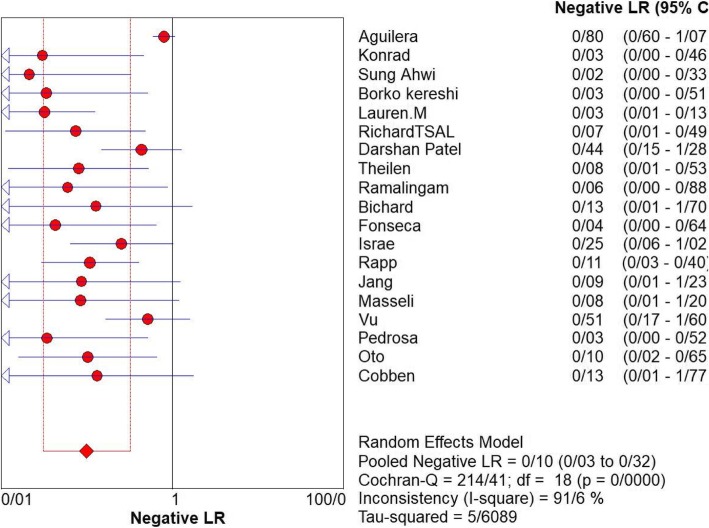
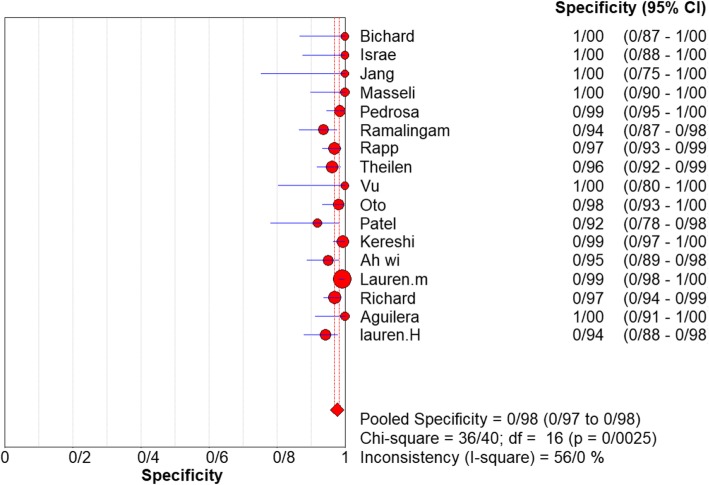
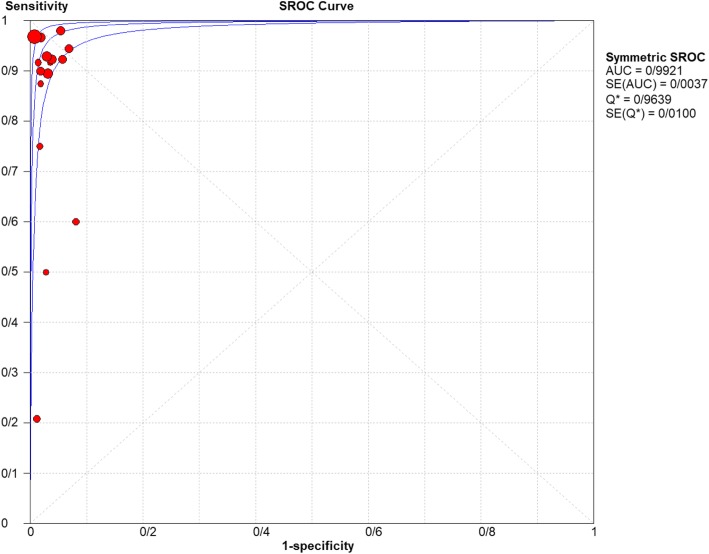
For appendicitis in pregnancy, the MRI sensitivity was 91.8% at the confidence interval of 95 percent (95% CI 87.7–94.9%). At the confidence interval of 95%, the specificity was 97.9% (95% CI 97.2–100%). The diagnostic odds ratio was 177.60 (95% CI 35.012–900.91) showing a high accuracy of MRI in diagnosing appendicitis in pregnant women (Table 2). The SROC plot showed a summary of estimated sensitivity and specificity and the area under the SROC curve of MRI in diagnosing appendicitis in pregnant women (Figs. 3, 4, and 5). The positive and negative LRs for MRI in diagnosing appendicitis in pregnant women were 30.98(21.33 to 44.99) and 0.10(0.03 to 0.32) respectively (Figs. 6 and 7).
Table 2.
Accuracy of individual studies MRI in characterization of acute appendicitis during pregnancy
| Study | Year | Participants | TP | FP | FN | TN | Sensitivity(95% CI) | Specificity(95% CI) | Accuracy | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% | Low | Up | 95% | Low | Up | ||||||||
| Theilen | 2014 | 171 | 12 | 6 | 1 | 152 | 0.923 | 0.640 | 0.998 | 0.962 | 0.919 | 0.986 | 92% |
| Ramalingam | 2015 | 102 | 8 | 6 | 0 | 88 | 1.000 | 0.631 | 1.000 | 0.936 | 0.866 | 0.976 | 100% |
| Bichard | 2005 | 29 | 3 | 0 | 0 | 26 | 1.000 | 0.292 | 1.000 | 1.000 | 0.868 | 1.000 | 100% |
| Fonseca | 2014 | 31 | 11 | 0 | 0 | 20 | 1.000 | 0.715 | 1.000 | 1.000 | 0.832 | 1.000 | 100% |
| Isra | 2008 | 33 | 4 | 0 | 1 | 28 | 0.800 | 0.284 | 0.995 | 1.000 | 0.877 | 1.000 | 80% |
| Rap | 2013 | 212 | 17 | 6 | 2 | 187 | 0.895 | 0.669 | 0.987 | 0.969 | 0.934 | 0.989 | 89% |
| Jang | 2011 | 18 | 5 | 0 | 0 | 13 | 1.000 | 0.478 | 1.000 | 1.000 | 0.753 | 1.000 | 100% |
| Masselli | 2011 | 40 | 5 | 0 | 0 | 35 | 1.000 | 0.478 | 1.000 | 1.000 | 0.753 | 1.000 | 100% |
| Vu | 2009 | 19 | 1 | 0 | 1 | 17 | 0.500 | 0.013 | 0.987 | 1.000 | 0.805 | 1.000 | 50% |
| Pedrosu | 2009 | 148 | 14 | 2 | 0 | 132 | 1.000 | 0.768 | 1.000 | 0.985 | 0.947 | 0.998 | 100% |
| Ato | 2009 | 118 | 9 | 2 | 1 | 106 | 0.900 | 0.555 | 0.997 | 0.981 | 0.935 | 1.000 | 50% |
| Cobben | 2004 | 12 | 3 | 0 | 0 | 9 | 1.000 | 0.292 | 1.000 | 1.000 | 0.664 | 1.000 | 100% |
| Aguilera | 2016 | 52 | 2 | 0 | 9 | 41 | 0.182 | 0.023 | 0.518 | 1.000 | 0.914 | 1.000 | 18% |
| Konrad | 2015 | 140 | 16 | 2 | 0 | 96 | 1.000 | 0.794 | 1.000 | 0.980 | 0.928 | 0.998 | 100% |
| Sungah | 2016 | 125 | 24 | 5 | 0 | 96 | 1.000 | 0.858 | 1.000 | 0.950 | 0.888 | 0.984 | 100% |
| Borkokereshi | 2017 | 176 | 14 | 1 | 0 | 161 | 1.000 | 0.768 | 1.000 | 0.994 | 0.982 | 1.000 | 100% |
| Lauren M | 2015 | 709 | 61 | 5 | 2 | 641 | 0.968 | 0.890 | 0.996 | 0.992 | 0.982 | 0.997 | 96% |
| Richard | 2017 | 223 | 13 | 6 | 1 | 198 | 0.929 | 0.661 | 0.998 | 0.971 | 0.937 | 0.989 | 92% |
| Darshan | 2017 | 42 | 3 | 3 | 2 | 34 | 0.600 | 0.147 | 0.947 | 0.919 | 0.781 | 0.983 | 60% |
| Pooled sensitivity and specificity | – | 2400 | 135 | 44 | 110 | 2080 | 0.918 | 0.877 | 0.949 | 0.979 | 0.972 | 1.000 | – |
TP, true positive; FP, false positive; FN, false negative; TN, true negative; 95% CI, 95% confidence interval
Fig. 4.
Specificity of MRI (≥ 1.5 T) for diagnosing appendicitis in studies that included pregnant patients only. Forest plots of specificity reported in each study. Each study is identified by name of first author and year of publication, with circles representing individual study point estimates, size of each circle indicating relative contribution to data pooling (inverse variance weighting), horizontal lines indicating 95% CIs, and dashed vertical lines representing 95% CIs for pooled specificity
Fig. 5.
Summary-ROC (SROC) curve for diagnostic accuracy of MRI in diagnosing appendicitis. Size of each circle on graph represents sample size of included study. SE = standard error; Q* index = point at which sensitivity and specificity are equal or point closest to ideal top-left corner of SROC space
Fig. 6.
Positive LR of MRI for diagnosing appendicitis in studies that included pregnant patients only. Forest plot of positive LR reported in each study. Each study is identified by name of first author and year of publication, with circles representing individual study point estimates, size of each circle indicating relative contribution to data pooling (inverse variance weighting), horizontal lines indicating 95% CIs, and dashed vertical lines representing 95% CIs for pooled positive LR
Fig. 7.
Negative LR of MRI for diagnosing appendicitis in studies that included pregnant patients only. Forest plot of negative LR reported in each study. Each study is identified by name of first author and year of publication, with circles representing individual study point estimates, size of each circle indicating relative contribution to data pooling (inverse variance weighting), horizontal lines indicating 95% CIs, and dashed vertical lines representing 95% CIs for pooled Negative LR
Meta-regression
Meta-regression indicated that the mean field strength of MRI was intervening (p = 0.0017) (Table 3).
Table 3.
The quality of the articles that is calculated using a checklist which includes 5 criteria
| First Author | Country | Year | Tesla | Sample size | Mean age | Accuracy | NPV | PPV |
|---|---|---|---|---|---|---|---|---|
| Birchard | USA | 2005 | 1.5 | √ | √ | * | * | * |
| Cobben | - | 2004 | 1 | √ | √ | * | * | * |
| Fonseca | USA | 2014 | N/A | √ | * | * | * | * |
| Israel | USA | 2008 | 1.5 | √ | √ | √ | √ | √ |
| Jang | Korea | 2011 | 1.5 | √ | √ | * | * | * |
| Masselli | Italy | 2009 | 1.5 | √ | * | * | √ | √ |
| Pedrosa | USA | 2009 | 1.5 | √ | √ | * | √ | √ |
| Ramalingam | USA | 2014 | 1.5 | √ | √ | * | √ | √ |
| Rapp | USA | 2013 | 1.5 | √ | √ | * | √ | √ |
| Theilen | USA | 2014 | 1.5 | √ | √ | * | √ | √ |
| Vu | Canada | 2009 | 1.5 | √ | √ | √ | √ | √ |
| Oto | USA | 2008 | 1.5 | √ | √ | √ | √ | √ |
| Patel | Canada | 2017 | 1.5 | √ | √ | √ | √ | √ |
| Kereshi | USA | 2017 | 1.5 | √ | √ | * | √ | √ |
| Ah Wi | Korea | 2018 | 1.5 | √ | √ | √ | √ | √ |
| Burke | USA | 2015 | 1.5 | √ | √ | √ | √ | √ |
| Konrad | USA | 2015 | 1.5 | √ | * | * | √ | √ |
| Aguilera | USA | 2018 | 1.5 | √ | √ | * | √ | √ |
| Theilen | USA | 2014 | 1.5 | √ | * | * | √ | √ |
Based on these 5 criteria, articles were scored and then classified to three different quality including good quality (score more than 4), average quality (score 3–4), and weak quality (score below 3). Six studies had good quality
Subgroup analysis of MRI field of strength
Analyzing studies with the field strength of ≥ 1.5 T indicated that sensitivity was 0.94% (95% CI 88–0.98%) and specificity was 0.92% (at the confidence interval of 95% CI 0.64–100%). DOR was 325.74 (at the confidence interval of 95%) showing a very high accuracy of MRI with field strength of ≥ 1.5 T in diagnosing appendicitis in pregnant women. and inconsistency was 56%. The SROC plot. The SROC plot showed a summary of estimated sensitivity and specificity and the area under the SROC curve of MRI with a field strength of ≥ 1.5 T in diagnosing appendicitis in pregnant women (Figs. 6, 7, and 8).
Fig. 8.
Specifity of MRI (≥ 1.5 T) for diagnosing appendicitis in studies that included pregnant patients only. Forest plot of sensitivity reported in each study. Each study is identified by name of first author and year of publication, with circles representing individual study point estimates, size of each circle indicating relative contribution to data pooling (inverse variance weighting), horizontal lines indicating 95% CIs, and dashed vertical lines representing 95% CIs for pooled sensitivity and specificity
Country
Analyzing 13 studies conducted in USA [64–69, 73, 74, 76, 77, 79–81] indicated a pooled sensitivity of 91.5% (95% CI 86.8–95%) and a pooled specificity of 98.1%(95% CI 97.4–98.7%) and a DOR of 559.41 (95% CI 262.40–1192.6) (Figs. 9 and 10). the sensitivity, specificity, and DOR of MRI in diagnosis of appendicitis in pregnant women in South Korea based on 2 included articles [70, 78] were 100% (95% CI 88.1–100%), 95.6% (95% CI 90.1–98.6%), 596.36 (95% CI 55.640–6391.9) respectively. The sensitivity, specificity, and DOR of MRI in diagnosis of appendicitis in pregnant women in Canada based on 2 included articles [72, 82] were 57.1% (95% CI 18.4–90.1%), 94.4% (95% CI 84.6–98.8%), 20.523 (95% CI 3.250–129.61) respectively (Fig. 11).
Fig. 9.
Sensivity of MRI (≥ 1.5 T) for diagnosing appendicitis in studies that included pregnant patients only. Forest plots of specificity reported in each study. Each study is identified by name of first author and year of publication, with circles representing individual study point estimates, size of each circle indicating relative contribution to data pooling (inverse variance weighting), horizontal lines indicating 95% CIs, and dashed vertical lines representing 95% CIs for pooled specificity
Fig. 10.
Summary-ROC (SROC) curve for diagnostic accuracy of MRI (≥ 1.5 T) in diagnosing appendicitis. Size of each circle on graph represents sample size of included study. SE = standard error; Q* index = point at which sensitivity and specificity are equal or point closest to ideal top-left corner of SROC space
Fig. 11.
Pooled sensitivity and specificity of MRI in diagnosis of appendicitis in pregnancy by countries
Discussion
Many investigators have previously shown that MRI for the workup of acute appendicitis in pregnancy is highly reliable and useful. In this systematic review and meta-analysis, we calculated a 91.8% sensitivity and a 97.9% specificity of MRI for the diagnosis of appendicitis in pregnant women. We were able to include 7 more studies than the most recent published meta-analysis by Eugene Duke et al [83] included, which reviewed 12 studies between 2004 and 2015 comprising 933 pregnant women and calculated a pooled sensitivity of 94% (95% CI 87–98%), and specificity of 97% (95% CI 96–98%) and a DOR of 309.8 (95% CI 140.5–711). Also, analyzing studies with the field strength of ≥ 1.5 T (which was the field strength used in most of the studies included) indicated that sensitivity was 0.94% (95% CI 88–0.98%) and specificity was 0.92% (at the confidence interval of 95% CI 0.64–100%). DOR was 325.74 (at the confidence interval of 95%) which is indicative of the better accuracy of MRI with a field strength of ≥ 1.5 T in diagnosing appendicitis in pregnant women. Our calculated sensitivity and specificity was lower than what Blumenfeld YJ et al. [84] reported in their meta-analysis (specificity of 99.9% and sensitivity of 95.0%). Due to the high number of included studies which were conducted in the USA [64–69, 73, 74, 76, 77, 79–81], we decided to perform a subgroup meta-analysis based on the country which was indicative of a pooled sensitivity of 91.5% (95% CI 86.8–95%) and a pooled specificity of 98.1% (95% CI 97.4–98.7%) and a DOR of 559.41 (95% CI 262.40–1192.6) for MRI in diagnosis of appendicitis in pregnant women. The sensitivity, specificity, and DOR of MRI in diagnosis of appendicitis in pregnant women in South Korea based on 2 included articles [70, 78] were 100% (95% CI 88.1–100%), 95.6% (95% CI 90.1–98.6%), and 596.36 (95% CI 55.640–6391.9) respectively. Mahesh K et al. [85] in a 5-year study on 39 pregnant women reported that the sensitivity of CT in the diagnosis of appendicitis in pregnant women was 100%; they also reported a sensitivity of 46.1% for ultrasound, but on the other hand, Kevin A et al. [86] in their meta-analysis presented a sensitivity of 89.9% and a specificity of 93.6% for CT scan in diagnosing the acute appendicitis in adults including pregnant women which is quite close and even in some countries like South Korea, The Netherlands, and Italy, less than what we calculated as the sensitivity and specificity of MRI in diagnosing acute appendicitis in pregnant women. The SAGES guidelines do not recommend the employment of CT scan as the initial imaging technique for pregnant patients, except in cases where urgent information is needed for trauma or acute abdominal pain [87–90]. Given the effectiveness of ultrasound and MRI, CT should be used only in emergency cases or in situations where MRI is inaccessible or cannot be used [91, 92]. When ionizing radiation imaging is required, specific techniques can be employed in accordance with as low as reasonably achievable (ALARA) principle [93]. MR imaging can be performed without using intravenous gadolinium for pregnant women. MRI is favored compared with CT scan to diagnose non-obstetric abdominal pain in gravid patients, as the former makes it possible to take excellent soft tissue images without using ionizing radiation and is safer when applied to pregnant patients [67, 94, 95].
The maternal and fetal outcomes can be improved if abdominal conditions during pregnancy are diagnosed accurately and timely. Diagnostic laparoscopy is a preferred choice for cases where available resources prevent prompt imaging for diagnosis or when imaging is inconclusive. The risks of delayed diagnosis should be compared with possible risks associated with possible negative laparoscopy. The conditions diagnosed at laparoscopy should be treated by the surgeon as soon as possible [96].
The results of this study indicate that although there is a small difference between CT scan and MRI sensitivity in diagnosing appendicitis in pregnancy due to multiple complications of CT scan in pregnancy including exposure of patients to ionizing radiation, which is of special concern in pediatric and obstetric populations [87], MRI seems to be a more reasonable imaging modality than CT scan in cases of suspected appendicitis in pregnancy, especially in tertiary care centers that have access to specialized radiologists.
Limitations of this meta-analysis mostly relate to the available data and the heterogeneity of design, interpretation of results, and reporting of data in primary studies. Our study is also limited by the fact that most of the studies were retrospective case series. The number of patients enrolled ranged from 12 to 709, which in some cases led to inconsistencies in the results, especially in the calculated accuracies of MRI. and most studies did not include the overall appendicitis rates in their respective institutions, and thus, we were unable to calculate prevalence-adjusted positive and negative predictive values. Also, the studies varied by their inclusion criteria.
Conclusion
MRI has high sensitivity and specificity (91.8% and 97.9% respectively) for the diagnosis of acute appendicitis in pregnant patients with clinically suspected appendicitis. It is an excellent imaging technique in many instances, which does not expose a fetus, or the mother, to ionizing radiation, making it an excellent option for pregnant patients with suspected acute appendicitis. It can be performed at any stage of pregnancy, with no evidence of adverse effects on fetal outcomes, as it is currently being used. As radiologists become increasingly comfortable with interpreting abdominal and pelvic MRI, and as it becomes more widely available as an emergent procedure, its utility will continue to increase in the future.
Acknowledgements
Not applicable.
Abbreviations
- CT
Computed tomography
- DOR
Diagnostic odds ratio
- LR
Likelihood ratio
- MRI
Magnetic resonance imaging
- SROC
Summary receiver–operator curves
- US
Ultrasound
Authors’ contributions
MK participated in conception and design of the study, library searches and assembling relevant literature, critical review of the paper, supervising and writing of the paper, and database management. FP participated in data collection, library searches and assembling relevant literature, writing the paper, and critical review of the paper. MS participated in data collection, library searches and assembling relevant literature, writing the paper, analysis of the data, and critical review of the paper. All authors read and approved the final manuscript.
Funding
Not applicable
Availability of data and materials
Please contact the authors for data requests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mania Kave, Email: zhn.search@gmail.com.
Fateme Parooie, Email: tahghighatt3@gmail.com.
Morteza Salarzaei, Email: mr.mortezasalar@gmail.com.
References
- 1.Ueberrueck T, Koch A, Meyer L, et al. Ninety-four appendectomies for suspected acute appendicitis during pregnancy. World J Surg. 2004;28(5):508–511. doi: 10.1007/s00268-004-7157-2. [DOI] [PubMed] [Google Scholar]
- 2.Andersson Roland EB, Lambe Mats. Incidence of appendicitis during pregnancy. International Journal of Epidemiology. 2001;30(6):1281–1285. doi: 10.1093/ije/30.6.1281. [DOI] [PubMed] [Google Scholar]
- 3.Şimşek Deniz, Turan Özgür Deniz, Ergenoğlu Ahmet Mete, Demir Halit Batuhan, Sezer Taylan Özgür, Şahin Çağdaş. Pregnancy Outcomes and Surgical Management of Pregnancy Complicated By Appendicitis: Obstetrician View. Meandros Medical and Dental Journal. 2015;16(2):43–49. doi: 10.4274/meandros.2401. [DOI] [Google Scholar]
- 4.Apandisit AP. Acute perforated appendicitis as a cause of fetal tachycardia at term pregnancy. Cukurova Med J. 2015;40(2):336–339. doi: 10.17826/cutf.83967. [DOI] [Google Scholar]
- 5.Aydın S, Fatihoğlu E. Perfore Apandisit: Ultrasonografik Bir Tanısal Zorluk. Ankara Eğitim ve Araştırma Hastanesi Tıp Dergisi. 51(2):110–5.
- 6.Gök AF, Soytaş Y, Bayraktar A, Emirikçi S, İlhan M, Koltka AK, Günay MK. Laparoscopic versus open appendectomy in pregnancy: a single center experience. Ulusal Travma Acil Cerrahi Derg. 2018;24(6):552–556. doi: 10.5505/tjtes.2018.26357. [DOI] [PubMed] [Google Scholar]
- 7.Hatipoglu S, Hatipoglu F, Akbulut S, Abdullayev R. Management of acute appendicitis in pregnancy: Early diagno.
- 8.Ucuncu MZ, Ucuncu MM. Left sided acute appendicitis in pregnant woman: a case report/Sol Yerlesimli Gebe Akut Apandisit: Olgu Sunumu. Turk J Color Dis. 2016;26(4):136–139. [Google Scholar]
- 9.Demir MK, Savas Y, Furuncuoglu Y, Cevher T, Demiral S, Tabandeh B, Aslan M. Imaging findings of the unusual presentations, associations and clinical mimics of acute appendicitis. Eurasian J Med. 2017;49(3):198. doi: 10.5152/eurasianjmed.2017.17218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Çınar H, Aygün A, Derebey M, Tarım İA, Akalın Ç, Büyükakıncak S, Erzurumlu K. Significance of hemogram on diagnosis of acute appendicitis during pregnancy. Ulus Travma Acil Cerrahi Derg. 2018;24(5):423–428. doi: 10.5505/tjtes.2018.62753. [DOI] [PubMed] [Google Scholar]
- 11.Mir SA, Wani M, Tak SA, Shiekh SH, Moheen HA. Feasibility of early surgical intervention for acute appendicitis in gravid patients. Saudi Surg J. 2017;5(3):111. doi: 10.4103/ssj.ssj_25_17. [DOI] [Google Scholar]
- 12.Pastore P. A., Loomis D. M., Sauret J. Appendicitis in Pregnancy. The Journal of the American Board of Family Medicine. 2006;19(6):621–626. doi: 10.3122/jabfm.19.6.621. [DOI] [PubMed] [Google Scholar]
- 13.Eryilmaz Ramazan, Şahin Mustafa, Baş Gürhan, Alimoglu Orhan, Kaya Bülent. Acute Appendicitis during Pregnancy. Digestive Surgery. 2002;19(1):40–44. doi: 10.1159/000052004. [DOI] [PubMed] [Google Scholar]
- 14.Beyazal M, Özkaçmaz S, Ünal Ö, Yavuz A, Bora A. Necrotizing Brucella epididymoorchitis: magnetic resonance imaging findings. Prevalence. 2014;19:24. [Google Scholar]
- 15.Oto Aytekin, Ernst Randy D., Ghulmiyyah Labib M., Nishino Thomas K., Hughes Douglas, Chaljub Gregory, Saade George. MR imaging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdominal Imaging. 2008;34(2):243–250. doi: 10.1007/s00261-008-9381-y. [DOI] [PubMed] [Google Scholar]
- 16.De Wilde JP, Rivers AW, Price DL. A review of the current use of magnetic resonance imaging in pregnancy and safety implications for the fetus. Prog Biophys Mol Biol. 2005;87(2–3):335–53. [DOI] [PubMed]
- 17.Mourad Jamal, Elliott John P., Erickson Laurie, Lisboa Luis. Appendicitis in pregnancy: New information that contradicts long-held clinical beliefs. American Journal of Obstetrics and Gynecology. 2000;182(5):1027–1029. doi: 10.1067/mob.2000.105396. [DOI] [PubMed] [Google Scholar]
- 18.Dewhurst C, Beddy P, Pedrosa I. MRI evaluation of acute appendicitis in pregnancy. J Magn Reson Imaging. 2013;37(3):566–575. doi: 10.1002/jmri.23765. [DOI] [PubMed] [Google Scholar]
- 19.Tamir IL, Bongard FS, Klein SR. Acute appendicitis in the pregnant patient. Am J Surg. 1990;160(6):571–576. doi: 10.1016/S0002-9610(05)80748-2. [DOI] [PubMed] [Google Scholar]
- 20.Chen Morie M., Coakley Fergus V., Kaimal Anjali, Laros Russell K. Guidelines for Computed Tomography and Magnetic Resonance Imaging Use During Pregnancy and Lactation. Obstetrics & Gynecology. 2008;112(2, Part 1):333–340. doi: 10.1097/AOG.0b013e318180a505. [DOI] [PubMed] [Google Scholar]
- 21.Vu L, Ambrose D, Vos P, Tiwari P, Rosengarten M, Wiseman S. Evaluation of MRI for the diagnosis of appendicitis during pregnancy when ultrasound is inconclusive. J Surg Res. 2009;156(1):145–149. doi: 10.1016/j.jss.2009.03.044. [DOI] [PubMed] [Google Scholar]
- 22.Colletti PM, Sylvestre PB. Magnetic resonance imaging in pregnancy. Magnetic resonance imaging clinics of North America. 1994;2(2):291–307. [PubMed]
- 23.Tremblay Emilie, Thérasse Eric, Thomassin-Naggara Isabelle, Trop Isabelle. Quality Initiatives: Guidelines for Use of Medical Imaging during Pregnancy and Lactation. RadioGraphics. 2012;32(3):897–911. doi: 10.1148/rg.323115120. [DOI] [PubMed] [Google Scholar]
- 24.Rooholamini S A, Au A H, Hansen G C, Kioumehr F, Dadsetan M R, Chow P P, Kurzel R B, Mikhail G. Imaging of pregnancy-related complications. RadioGraphics. 1993;13(4):753–770. doi: 10.1148/radiographics.13.4.8356266. [DOI] [PubMed] [Google Scholar]
- 25.Rosen MP, Ding A, Blake MA, Baker ME, Cash BD, Fidler JL, Grant TH, Greene FL, Jones B, Katz DS, Lalani T. ACR Appropriateness Criteria® right lower quadrant pain—suspected appendicitis. J Am College Radiol. 2011;8(11):749–755. doi: 10.1016/j.jacr.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Nunnelee JD, Musselman R, Spaner SD. Appendectomy in pregnancy and postpartum: analysis of data from a large private hospital. Clin Excell Nurse Pract. 1999;3(5):298–301. [PubMed: 10763629].. [PubMed]
- 27.Ito K, Ito H, Whang EE, Tavakkolizadeh A. Appendectomy in pregnancy: evaluation of the risks of a negative appendectomy. Am J Surg. 2012;203(2):145–150. doi: 10.1016/j.amjsurg.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 28.Wallace CA, Petrov MS, Soybel DI, Ferzoco SJ, Ashley SW, Tavakkolizadeh A. Influence of imaging on the negative appendectomy rate in pregnancy. J Gastrointest Surg. 2008;12(1):46–50. doi: 10.1007/s11605-007-0377-7. [DOI] [PubMed] [Google Scholar]
- 29.Baysinger CL. Imaging during pregnancy. Anesthesia & Analgesia. 2010;110(3):863–7. [DOI] [PubMed]
- 30.Jung Seung Eun, Byun Jae Young, Lee Jae Mun, Rha Sung Eun, Kim Hyun, Choi Byung Gil, Hahn Seong Tai. MR Imaging of Maternal Diseases in Pregnancy. American Journal of Roentgenology. 2001;177(6):1293–1300. doi: 10.2214/ajr.177.6.1771293. [DOI] [PubMed] [Google Scholar]
- 31.Yilmaz Hatice Gulsen, Akgun Yilmaz, Bac Bilsel, Celik Yusuf. Acute appendicitis in pregnancy — risk factors associated with principal outcomes: A case control study. International Journal of Surgery. 2007;5(3):192–197. doi: 10.1016/j.ijsu.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 32.McGory Marcia L., Zingmond David S., Tillou Areti, Hiatt Jonathan R., Ko Clifford Y., Cryer Henry M. Negative Appendectomy in Pregnant Women Is Associated with a Substantial Risk of Fetal Loss. Journal of the American College of Surgeons. 2007;205(4):534–540. doi: 10.1016/j.jamcollsurg.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 33.Ramalingam V, LeBedis C, Kelly JR, Uyeda J, Soto JA, Anderson SW. Evaluation of a sequential multi-modality imaging algorithm for the diagnosis of acute appendicitis in the pregnant female. Emerg Radiol. 2015;22(2):125–132. doi: 10.1007/s10140-014-1260-y. [DOI] [PubMed] [Google Scholar]
- 34.Aggenbach L, Zeeman GG, Cantineau AE, Gordijn SJ, Hofker HS. Impact of appendicitis during pregnancy: no delay in accurate diagnosis and treatment. Int J Surg. 2015;15:84–89. doi: 10.1016/j.ijsu.2015.01.025. [DOI] [PubMed] [Google Scholar]
- 35.Thompson MM, Kudla AU, Chisholm CB. Appendicitis during pregnancy with a normal MRI. West J Emerg Med. 2014;15(6):652. doi: 10.5811/westjem.2014.7.22988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baron KT, Arleo EK, Robinson C, Sanelli PC. Comparing the diagnostic performance of MRI versus CT in the evaluation of acute nontraumatic abdominal pain during pregnancy. Emerg Radiol. 2012;19(6):519–525. doi: 10.1007/s10140-012-1066-8. [DOI] [PubMed] [Google Scholar]
- 37.SCOAP Collaborative. Cuschieri J, Florence M, et al. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg. 2008;248(4):557–563. doi: 10.1097/SLA.0b013e318187aeca. [DOI] [PubMed] [Google Scholar]
- 38.Babaknia A, Parsa H, Woodruff JD. Appendicitis during pregnancy. Obstet Gynecol. 1977;50(1):40–1. [PubMed]
- 39.Leeuwenburgh MM, Jensch S, Gratama JW, Spilt A, Wiarda BM, Van Es HW, Cobben LP, Bossuyt PM, Boermeester MA, Stoker J, OPTIMAP Study Group MRI features associated with acute appendicitis. Eur Radiol. 2014;24(1):214–222. doi: 10.1007/s00330-013-3001-0. [DOI] [PubMed] [Google Scholar]
- 40.Repplinger MD, Levy JF, Peethumnongsin E, Gussick ME, Svenson JE, Golden SK, Ehlenbach WJ, Westergaard RP, Reeder SB, Vanness DJ. Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J Magn Reson Imaging. 2016;43(6):1346–1354. doi: 10.1002/jmri.25115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hiersch L, Yogev Y, Ashwal E, From A, Ben-Haroush A, Peled Y. The impact of pregnancy on the accuracy and delay in diagnosis of acute appendicitis. J Matern Fetal Neonatal Med. 2014;27(13):1357–1360. doi: 10.3109/14767058.2013.858321. [DOI] [PubMed] [Google Scholar]
- 42.van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA. Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology. 2008;249(1):97–106. doi: 10.1148/radiol.2483071652. [DOI] [PubMed] [Google Scholar]
- 43.Leeuwenburgh MM, Wiarda BM, Jensch S, van Es HW, Stockmann HB, Gratama JW, Cobben LP, Bossuyt PM, Boermeester MA, Stoker J. OPTIMAP Study group. Accuracy and interobserver agreement between MR-non-expert radiologists and MR-experts in reading MRI for suspected appendicitis. Eur J Radiol. 2014;83(1):103–110. doi: 10.1016/j.ejrad.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 44.Debnath J, Sharma P, Maurya V. Diagnosing appendicitis during pregnancy: which study when? Am J Obstet Gynecol. 2016;214(1):135–136. doi: 10.1016/j.ajog.2015.09.064. [DOI] [PubMed] [Google Scholar]
- 45.Kapan S, Bozkurt MA, Turhan AN, Gönenç M, Alış H. Management of acute appendicitis in pregnancy. Ulus Travma Acil Cerrahi Derg. 2013;19(1):20–24. doi: 10.5505/tjtes.2013.81889. [DOI] [PubMed] [Google Scholar]
- 46.Affleck David G, Handrahan Diana L, Egger Marlene J, Price Raymond R. The laparoscopic management of appendicitis and cholelithiasis during pregnancy. The American Journal of Surgery. 1999;178(6):523–528. doi: 10.1016/S0002-9610(99)00244-5. [DOI] [PubMed] [Google Scholar]
- 47.Theilen LH, Mellnick VM, Shanks AL, Tuuli MG, Odibo AO, Macones GA, Cahill AG. Acute appendicitis in pregnancy: predictive clinical factors and pregnancy outcomes. Am J Perinatol. 2017;34(06):523–528. doi: 10.1055/s-0036-1593764. [DOI] [PubMed] [Google Scholar]
- 48.Kinner S, Repplinger MD, Pickhardt PJ, Reeder SB. Contrast-enhanced abdominal MRI for suspected appendicitis: how we do it. Am J Roentgenol. 2016;207(1):49–57. doi: 10.2214/AJR.15.15948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kereshi Borko, Lee Karen S., Siewert Bettina, Mortele Koenraad J. Clinical utility of magnetic resonance imaging in the evaluation of pregnant females with suspected acute appendicitis. Abdominal Radiology. 2017;43(6):1446–1455. doi: 10.1007/s00261-017-1300-7. [DOI] [PubMed] [Google Scholar]
- 50.Coursey CA, Nelson RC, Patel MB, et al. Making the diagnosis of acute appendicitis: do more preoperative CT scans mean fewer negative appendectomies? A 10-year study. Radiology. 2010;254:460–468. doi: 10.1148/radiol.09082298. [DOI] [PubMed] [Google Scholar]
- 51.Morse BC, Roettger RH, Kalbaugh CA, Blackhurst DW, Hines WB. Abdominal CT scanning in reproductive-age women with right lower quadrant abdominal pain: does its use reduce negative appendectomy rates and healthcare costs? Am Surg. 2007;73:580–584. [PubMed] [Google Scholar]
- 52.Raja AS, Wright C, Sodickson AD, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology. 2010;256:460–465. doi: 10.1148/radiol.10091570. [DOI] [PubMed] [Google Scholar]
- 53.Pedrosa I, Levine D, Eyvazzadeh AD, Siewert B, Ngo L, Rofsky NM. MR imaging evaluation of acute appendicitis in pregnancy. Radiology. 2006;238(3):891–899. doi: 10.1148/radiol.2383050146. [DOI] [PubMed] [Google Scholar]
- 54.Long SS, Long C, Lai H, Macura KJ. Imaging strategies for right lowerquadrant pain in pregnancy. AJR Am J Roentgenol. 2011;196(1):4–12. doi: 10.2214/AJR.10.4323. [DOI] [PubMed] [Google Scholar]
- 55.Hurwitz LM, Yoshizumi T, Reiman RE, Goodman PC, Paulson EK, Frush DP, et al. Radiation dose to the fetus from body MDCT during early gestation. AJR Am J Roentgenol. 2006;186(3):871–876. doi: 10.2214/AJR.04.1915. [DOI] [PubMed] [Google Scholar]
- 56.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 57.Moses LE, Shapiro D, Littenberg B. Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med. 1993;12:1293–1316. doi: 10.1002/sim.4780121403. [DOI] [PubMed] [Google Scholar]
- 58.Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A. Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol. 2006;6:31. doi: 10.1186/1471-2288-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Deville WL, Buntinx F, Bouter LM, et al. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol. 2002;2:9. doi: 10.1186/1471-2288-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56:1129–1135. doi: 10.1016/S0895-4356(03)00177-X. [DOI] [PubMed] [Google Scholar]
- 61.Arends LR, Hamza TH, van Houwelingen JC, Heijenbrok-Kal MH, Hunink MG, Stijnen T. Bivariate random effects meta-analysis of ROC curves. Med Decis Making. 2008;28:621–638. doi: 10.1177/0272989X08319957. [DOI] [PubMed] [Google Scholar]
- 62.Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–990. doi: 10.1016/j.jclinepi.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 63.Rutter CM, Gatsonis CA. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Statist Med. 2001;20:2865–2884. doi: 10.1002/sim.942. [DOI] [PubMed] [Google Scholar]
- 64.Theilen LH, Mellnick VM, Longman RE, Tuuli MG, Odibo AO, Macones GA, Cahill AG. Utility of magnetic resonance imaging for suspected appendicitis in pregnant women. Am J Obstet Gynecol. 2015;212(3):345–3e1. doi: 10.1016/j.ajog.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 65.Ramalingam V, LeBedis C, Kelly JR, Uyeda J, Soto JA, Anderson SW. Evaluation of sequential multi-modality imaging algorithm for the diagnosis of acute appendicitis in the pregnant female. Emerg Radiol. 2015;22:125–132. doi: 10.1007/s10140-014-1260-y. [DOI] [PubMed] [Google Scholar]
- 66.Birchard KR, Brown MA, Hyslop WB, Firat Z, Semelka RC. MRI of acute abdominal and pelvic pain in pregnant patients. AJR. 2005;184:452–458. doi: 10.2214/ajr.184.2.01840452. [DOI] [PubMed] [Google Scholar]
- 67.Fonseca AL, Schuster KM, Kaplan LJ, Maung AA, Lui FY, Davis KA. The use of magnetic resonance imaging in the diagnosis of suspected appendicitis in pregnancy: shortened length of stay without increase in hospital charges. JAMA Surg. 2014;149:687–693. doi: 10.1001/jamasurg.2013.4658. [DOI] [PubMed] [Google Scholar]
- 68.Israel GM, Malguria N, McCarthy S, Copel J, Weinreb J. MRI vs. ultrasound for suspected appendicitis during pregnancy. J Magn Reson Imaging. 2008;28:428–433. doi: 10.1002/jmri.21456. [DOI] [PubMed] [Google Scholar]
- 69.Rapp EJ, Naim F, Kadivar K, Davarpanah A, Cornfeld D. Integrating MR imaging into the clinical workup of pregnant patients suspected of having appendicitis is associated with a lower negative laparotomy rate: single-institution study. Radiology. 2013;267:137–144. doi: 10.1148/radiol.12121027. [DOI] [PubMed] [Google Scholar]
- 70.Jang KM, Kim SH, Choi D, Lee SJ, Rhim H, Park MJ. The value of 3D T1-weighted gradient-echo MR imaging for evaluation of the appendix during pregnancy: preliminary results. Acta Radiol. 2011;52:825–828. doi: 10.1258/ar.2011.110116. [DOI] [PubMed] [Google Scholar]
- 71.Masselli G, Brunelli R, Casciani E, et al. Acute abdominal and pelvic pain in pregnancy: MR imaging as a valuable adjunct to ultrasound? Abdom Imaging. 2011;36:596–603. doi: 10.1007/s00261-010-9654-0. [DOI] [PubMed] [Google Scholar]
- 72.Vu L, Ambrose D, Vos P, Tiwari P, Rosengarten M, Wiseman S. Evaluation of MRI for the diagnosis of appendicitis during pregnancy when ultrasound is inconclusive. J Surg Res. 2009;156:145–149. doi: 10.1016/j.jss.2009.03.044. [DOI] [PubMed] [Google Scholar]
- 73.Pedrosa I, Lafornara M, Pandharipande PV, Goldsmith JD, Rofsky NM. Pregnant patients suspected of having acute appendicitis: effect of MR imaging on negative laparotomy rate and appendiceal perforation rate. Radiology. 2009;250:749–757. doi: 10.1148/radiol.2503081078. [DOI] [PubMed] [Google Scholar]
- 74.Oto A, Ernst RD, Ghulmiyyah LM, et al. MR im- aging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdom Imaging. 2009;34:243–250. doi: 10.1007/s00261-008-9381-y. [DOI] [PubMed] [Google Scholar]
- 75.Cobben LP, Groot I, Haans L, Blickman JG, Puylaert J. MRI for clinically suspected appendicitis during pregnancy. AJR. 2004;183:671–675. doi: 10.2214/ajr.183.3.1830671. [DOI] [PubMed] [Google Scholar]
- 76.Aguilera F, Gilchrist BF, Farkas DT. Accuracy of MRI in Diagnosing Appendicitis during Pregnancy. Am Surg. 2018;84(8):1326–1328. [PubMed] [Google Scholar]
- 77.Konrad J, Grand D, Lourenco A. MRI: first-line imaging modality for pregnant patients with suspected appendicitis. Abdom Imaging. 2015;40(8):3359–3364. doi: 10.1007/s00261-015-0540-7. [DOI] [PubMed] [Google Scholar]
- 78.Wi SA, Kim DJ, Cho ES, Kim KA. Diagnostic performance of MRI for pregnant patients with clinically suspected appendicitis. Abdom Radiol. 2018;43(12):3456–3461. doi: 10.1007/s00261-018-1654-5. [DOI] [PubMed] [Google Scholar]
- 79.Kereshi B, Lee KS, Siewert B, Mortele KJ. Clinical utility of magnetic resonance imaging in the evaluation of pregnant females with suspected acute appendicitis. Radiology. 2017:1-0. [DOI] [PubMed]
- 80.Burke LM, Bashir MR, Miller FH, Siegelman ES, Brown M, Alobaidy M, Jaffe TA, Hussain SM, Palmer SL, Garon BL, Oto A. Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multiinstitutional study. Am J Obstet Gynecol. 2015;213(5):693–6e1. doi: 10.1016/j.ajog.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 81.Tsai R, Raptis C, Fowler KJ, Owen JW, Mellnick VM. MRI of suspected appendicitis during pregnancy: interradiologist agreement, indeterminate interpretation and the meaning of non-visualization of the appendix. Br J Radiol. 2017;90(1079):20170383. doi: 10.1259/bjr.20170383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Patel D, Fingard J, Winters S, Low G. Clinical use of MRI for the evaluation of acute appendicitis during pregnancy. Abdom Radiol. 2017;42(7):1857–1863. doi: 10.1007/s00261-017-1078-7. [DOI] [PubMed] [Google Scholar]
- 83.Duke E, Kalb B, Arif-Tiwari H, Daye ZJ, Gilbertson-Dahdal D, Keim SM, Martin DR. A systematic review and meta-analysis of diagnostic performance of MRI for evaluation of acute appendicitis. Am J Roentgenol. 2016;206(3):508–517. doi: 10.2214/AJR.15.14544. [DOI] [PubMed] [Google Scholar]
- 84.Blumenfeld YJ, Wong AE, Jafari A, Barth RA, El-Sayed YY. MR imaging in cases of antenatal suspected appendicitis–a meta-analysis. J Matern Fetal Neonatal Med. 2011;24(3):485–488. doi: 10.3109/14767058.2010.506227. [DOI] [PubMed] [Google Scholar]
- 85.Shetty Mahesh K., Garrett Nan M., Carpenter Wendy S., Shah Yogesh P., Roberts Candace. Abdominal Computed Tomography During Pregnancy for Suspected Appendicitis: A 5-Year Experience at a Maternity Hospital. Seminars in Ultrasound, CT and MRI. 2010;31(1):8–13. doi: 10.1053/j.sult.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 86.Eng KA, Abadeh A, Ligocki C, Lee YK, Moineddin R, Adams-Webber T, Schuh S, Doria AS. Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology. 2018;288(3):717–727. doi: 10.1148/radiol.2018180318. [DOI] [PubMed] [Google Scholar]
- 87.Smith MP, Katz DS, Lalani T, et al. ACR appropriateness Criteria® right lower quadrant pain--suspected appendicitis. Ultrasound Q. 2015;31(2):85–91. doi: 10.1097/RUQ.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 88.Groen RS, Bae JY, Lim KJ. Fear of the unknown: ionizing radiation exposure during pregnancy. Am J Obstet Gynecol. 2012;206:456–462. doi: 10.1016/j.ajog.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 89.Masselli G, Derchi L, McHugo J, Rockall A, Vock P, Weston M, Spencer J, Subcommittee EFPI Acute abdominal and pelvic pain in pregnancy: ESUR recommendations. Eur Radiol. 2013;23:3485–3500. doi: 10.1007/s00330-013-2987-7. [DOI] [PubMed] [Google Scholar]
- 90.Katz DS, Khalid M, Coronel EE, Mazzie JP. Computed tomography imaging of the acute pelvis in females. Can Assoc Radiol J. 2013;64:108–118. doi: 10.1016/j.carj.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 91.Masselli G, Derme M, Laghi F, Framarino-dei-Malatesta M, Gualdi G. Evaluating the acute abdomen in the pregnant patient. Radiol Clin North Am. 2015;53:1309–1325. doi: 10.1016/j.rcl.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 92.Karamat MI. Strategies and scientific basis of dose reduction on state-of-the-art multirow detector X-Ray CT systems. Crit Rev Biomed Eng. 2015;43:33–59. doi: 10.1615/CritRevBiomedEng.2015013977. [DOI] [PubMed] [Google Scholar]
- 93.Masselli G, Brunelli R, Monti R, Guida M, Laghi F, Casciani E, Polettini E, Gualdi G. Imaging for acute pelvic pain in pregnancy. Insights Imaging. 2014;5:165–181. doi: 10.1007/s13244-014-0314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Furey EA, Bailey AA, Pedrosa I. Magnetic resonance imaging of acute abdominal and pelvic pain in pregnancy. Top Magn Reson Imaging. 2014;23:225–224. doi: 10.1097/RMR.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 95.Karul M, Berliner C, Keller S, Tsui TY, Yamamura J. Imaging of appendicitis in adults. Rofo. 2014;186:551–558. doi: 10.1055/s-0034-1372825. [DOI] [PubMed] [Google Scholar]
- 96.Pearl JP, Price RR, Tonkin AE, Richardson WS, Stefanidis D. SAGES guidelines for the use of laparoscopy during pregnancy. Surg Endosc. 2017;31(10):3767–3782. doi: 10.1007/s00464-017-5637-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Please contact the authors for data requests.