Abstract
Background
Primary intraosseous meningioma is a subset of extradural meningioma that arises in the bone, and only a few cases have been reported to date.
Case presentation
An 80-year-old man presented with decreased hearing on the right side accompanied by a disturbance of balance 10 months prior to admission. Magnetic resonance imaging revealed an 8 × 7 cm osteolytic mass in the right posterior fossa related to the petrous bone, with extension to the cervical region. During surgery, the tumor was found to be located extradurally, with no invasion of the dura. The tumor was removed entirely, apart from a small portion around the jugular foramen to avoid lower cranial nerve injury.
Conclusion
The final diagnosis was primary intraosseous osteolytic meningioma with atypical pathology. Here, we report a rare case of an osteolytic skull lesion in the skull base not invading the dura and with extensive bone destruction.
Electronic supplementary material
The online version of this article (10.1186/s12883-019-1392-5) contains supplementary material, which is available to authorized users.
Keywords: Intraosseous, Meningioma, Osteolysis
Background
Meningiomas are common intradural lesions that arise from the arachnoid cap cells of the arachnoid layer. In contrast, primary extradural meningioma is a relatively rare entity, accounting for less than 2% of all meningiomas [1, 2]. They may arise from other locations, such as the skin, orbit, nasopharynx, and neck [3–5]. Primary intraosseous meningioma, which arises in the bone, is a subset of primary extradural meningioma, and only a few cases have been reported [1, 3]. Here, we report a recent case of primary intraosseous osteolytic meningioma with extension to the cervical region which was successfully removed.
Case presentation
An 80-year-old man presented with a progressive decrease in hearing on the right side accompanied by dizziness and disturbance of balance 10 months prior to admission. The neurological examination revealed right hypoglossal nerve palsy. Audiometry documented complete sensorineural hearing loss on the right side.
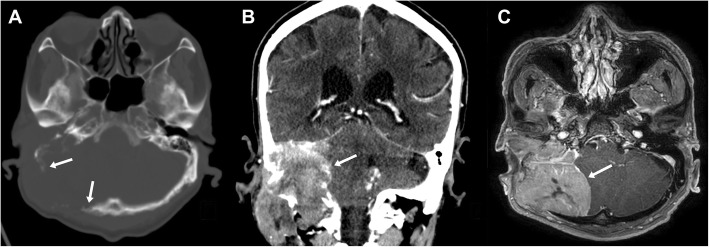
Skull x-ray and cranial computed tomography (CT) scans showed a large osteolytic lesion with bone destruction, including the temporal bone, occipital bone, clivus, jugular foramen, and hypoglossal canal (Fig. 1a and b). Magnetic resonance imaging (MRI) revealed an 8 × 7 cm homogeneous enhancing mass in the right posterior fossa related to the petrous part of the temporal bone, with extension to the cervical region (Fig. 1c). The cerebellum was displaced, and definite brain invasion was not seen. The preoperative diagnosis was a temporal bone origin malignancy such as squamous cell carcinoma or meningioma with invasion of the petrous bone.
Fig. 1.
Preoperative imaging. Axial computed tomography (CT) scan with bone window (a) shows a destructive osteolytic mass lesion in the right temporal-posterior fossa region. Coronal CT scan (b) and magnetic resonance imaging (c) revealed an 8 × 7 cm homogenous mass extending to the cervical region
The patient underwent surgery to obtain a pathological diagnosis and for complete removal of the mass. A C-shaped postauricular skin incision was made that extended to the neck. The scalp was reflected anteriorly, and the mass infiltrating the subcutaneous tissue was exposed. The lesion appeared as a firm gray mass that had destroyed the temporal and occipital bones. The dura was intact with no invasion, and the lesion was easily peeled off. For the cervical part of the tumor, the major vessels were secured inferiorly, and the mass was removed up to the skull base. The tumor was removed entirely, except for a small portion around the jugular foramen to avoid lower cranial nerve injury. Finally, the large empty space was filled with a sternocleidomastoid muscle flap (Fig. 2). There were no neurological deficits after surgery.
Fig. 2.
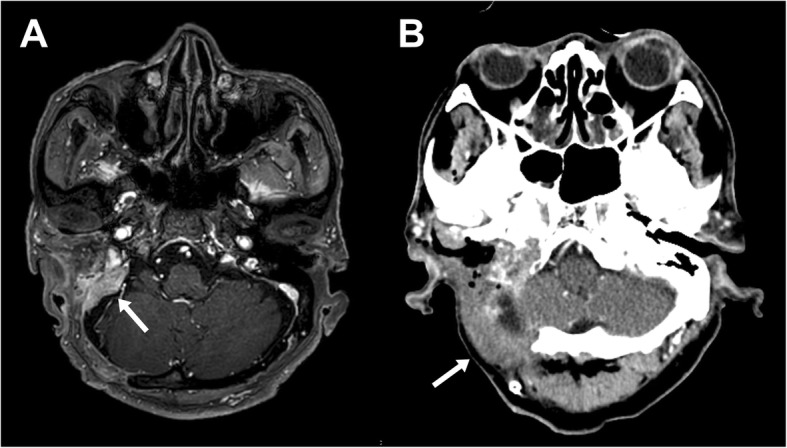
Postoperative magnetic resonance imaging (a) shows a small residual tumor around the jugular foramen, and computed tomography scan (b) demonstrates the sternocleidomastoid muscle which fills the tumor removal space
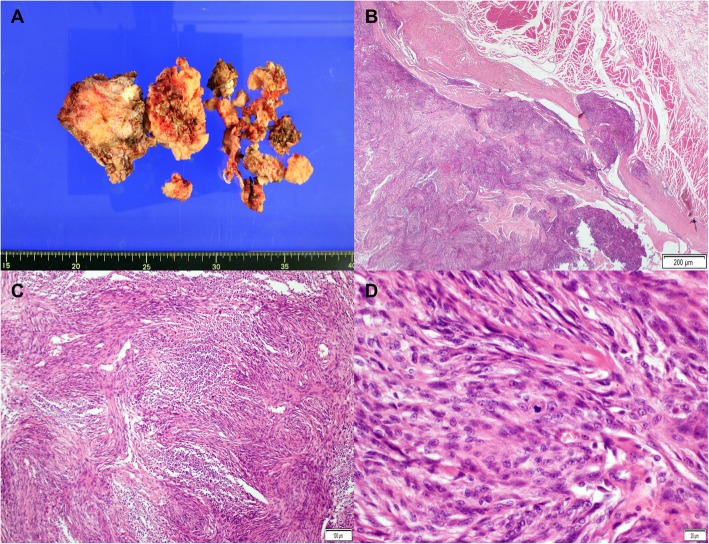
Histopathological studies confirmed a WHO (World Health Organization) grade II atypical meningioma with up to 6 mitoses per 10 high-power fields (Fig. 3). The Ki-67 proliferation index was 15%. The results of immunohistochemical staining are provided in Additional file 1: Figure S1.
Fig. 3.
Histopathologic findings of atypical meningioma. The fragmented specimen (a) is seen as grayish-white solid masses. On microscopic examination, the tumor infiltrated the adjacent soft tissue (b, hematoxylin and eosin [H&E] stain, × 20, scale bar = 200 μm) and showed a whorled appearance and multifocal necrosis (c, H&E stain, × 100, scale bar = 100 μm). The tumor cells are composed of spindle cells with prominent nucleoli and ill-defined cytoplasm. Many mitoses are visible (d, H&E stain, × 400, scale bar = 20 μm)
Discussion and conclusions
Primary intraosseous meningiomas are rare cranial lesions that arise from the bone, and they represent the most common type of primary extradural meningiomas [1–3]. The majority of intraosseous meningiomas are osteoblastic and cause hyperostosis, which may mimic fibrous dysplasia. In contrast, and more rarely, they may present as an osteolytic skull lesion [6, 7]. Reportedly, less than 20% of intraosseous meningiomas are osteolytic [8].
Primary extradural meningiomas are most commonly found in skull convexities, the paranasal sinus, and the middle ear but rarely in the skull base. Liu et al. reported 170 cases of extradural meningiomas in the head, and only 5.8% were located in the skull base [9]. Notably, there are few reports of osteolytic intraosseous meningiomas in the skull base. To date, 50 cases of osteolytic subtypes (including the present case) have been reported in the English literature (Table 1). Of these, only seven were located in the skull base, and all but two originated from the petrous bone.
Table 1.
Reports of primary intraosseous osteolytic meningiomas
| Reference, year | Sex/age | Location | Type | Pathology |
|---|---|---|---|---|
| Klein et al., 1975 [10] | F/66 | Parietal | IIIC | Meningothelial |
| McWhorter et al., 1976 [11] | M/42 | Temporal | IIC | Benign |
| Palma et al., 1977 [12] | M/18 | Frontal | IIIC | Fibroblastic |
| Pearl et al., 1979 [13] | F/44 | Frontal | IIC | Meningothelial |
| Ohaegbulam et al., 1979 [14] | M/31 | Frontal | IIIC | Fibroblastic |
| Young et al., 1983 [15] | M/71 | Frontal | IIC | Benign |
| Kaneko et al., 1988 [16] | F/71 | Frontoparietal | IIIC | Fibroblastic |
| Lee et al., 1988 [17] | F/71 | Frontoparietal | IIC | Malignant |
| Oka et al., 1989 [18] | F/79 | Frontoparietal | IIIC | Transitional |
| Ammirati et al., 1990 [19] | M/21 | Petrous | IIIB | Benign |
| Kulali et al., 1991 [20] | M/50 | Occipital | IIIC | Transitional |
| Ito et al., 1992 [21] | F/72 | Frontoparietal | IIC | Meningothelial |
| Fujita et al., 1993 [22] | M/42 | Petrous | IIIB | Malignant |
| Ghobashy and Tobler, 1994 [23] | F/65 | Frontal | IIC | Transitional |
| Parington et al., 1995 [24] | F/84 | Frontotemporal | IIIC | Atypical |
| Levin et al., 1995 [25] | N/A | Calvaria | N/A | N/A |
| Kuzeyli et al., 1996 [26] | M/6 | Temporal | IIC | Meningothelial |
| Changhong et al., 1997 [27] | F/42 | Occipital | IIC | Malignant |
| Muthukumar et al., 1997 [28] | M/55 | Parietal | IIIC | Meningothelial |
| M/50 | Temporoparietal | IIC | Meningothelial | |
| M/60 | Frontal | IIIC | Meningothelial | |
| Kudo et al., 1998 [29] | F/56 | Parietooccipital | IIIC | Meningothelial |
| Okamoto et al., 2000 [30] | F/78 | Parietal | IIC | Microcystic |
| Yamazaki et al., 2001 [31] | M/62 | Occipital | IIIB | Meningothelial |
| Rosahl et al., 2004 [32] | M/38 | Petrous | IIB | Meningothelial |
| Tokgoz et al., 2005 [33] | M/44 | Frontoparietal | IIIC | Chordoid |
| Bassiouni et al., 2006 [34] | M/47 | Parietal | IIIC | Benign |
| F/46 | Temporal | IIC | Meningothelial | |
| F/57 | Parietal | IIC | Fibroblastic | |
| F/62 | Frontal | IIC | Atypical | |
| M/34 | temporal | IIIC | Meningothelial | |
| Al-Khawaja et al., 2007 [35] | M/50 | Parietal | IIC | Meningothelial |
| Sheikhrezaie et al., 2009 [36] | M/62 | Frontoparietal | IIIC | Benign |
| Yener et al., 2009 [37] | M/78 | Parietal | IIC | Meningothelial |
| Hong et al., 2010 [38] | M/52 | Parietal | N/A | Benign |
| M/73 | Occipital | N/A | Anaplastic | |
| Kim et al., 2012 [39] | M/68 | Parietal | IIIC | Atypical |
| F/74 | Frontal | IIIC | Papillary | |
| Akhaddar and Ennouali, 2014 [40] | F/37 | Frontal | IIC | Meningothelial |
| Tang et al., 2014 [41] | F/82 | Parietal | IIC | Meningothelial |
| Yun and Lee, 2014 [42] | F/65 | Frontal | IIIC | Atypical |
| Kim et al., 2014 [43] | F/44 | Sphenoid | IIIB | Transitional |
| Bujok and Bienioszek, 2014 [44] | F/59 | Frontal | IIC | Microcystic |
| Kwon et al., 2015 [45] | M/69 | Parietal | IIIC | Meningothelial |
| Hong et al., 2015 [46] | M/61 | Frontoparietal | IIC | Benign |
| Ben Nsir et al., 2016 [47] | M/42 | Petrous | IIIB | Clear cell |
| Bohara et al., 2016 [48] | M/38 | Parietal | IIIC | Atypical |
| Mouri et al., 2017 [49] | F/76 | Frontal | IIIC | Transitional |
| Richardson et al., 2017 [50] | M/23 | Frontal | IIC | Benign |
| Present case | M/80 | Petrous | IIIB | Atypical |
The exact origin of extradural meningiomas is unclear, but several theories have been proposed. Their unusual locations are assumed to be the result of the aberrant differentiation or misplacement of undifferentiated mesenchymal stem cells [51]. Alternatively, extradural meningiomas may arise from differentiated arachnoid cap cells associated with blood vessels or nerves traversing the skull [52, 53]. Another theory proposes that they originate from arachnoid cap cells that get trapped in the cranial sutures during embryogenesis or molding of the cranium at birth [20, 21, 54]. Trauma with skull fracture has also been proposed as a causative factor of some extradural meningiomas, suggesting direct dural entrapment within bone fragments at the time of trauma [55].
The osteolytic subtype of intraosseous meningiomas is often misdiagnosed as a primary or secondary bone tumor due to its radiological appearance. The differential diagnosis of a solitary osteolytic skull lesion includes hemangioma, chondroma, chondrosarcoma, eosinophilic granuloma, epidermoid cyst, giant cell tumor, myeloma, and metastatic skull tumor [6, 23, 33].
Primary extradural meningiomas were practically classified according to their location by Lang and colleagues (Table 2) [3]. Therefore, intraosseous meningiomas could be considered Type II or Type III extradural meningiomas. Based on this classification, the present case falls into the type IIIB category due to the presence of extracalvarial extension. This classification is helpful in predicting the risk of tumor recurrence. The IIC and IIIC subtypes rarely recur after complete resection, whereas the IIB and IIIB subtypes have a reported lifetime risk of recurrence of 26% [3].
Table 2.
Primary extradural meningioma classification by Lang et al. 2000 [3]
| Type | Description | Subtype |
|---|---|---|
| I | Purely extracalvarial with no bony attachment | |
| II | Purely calvarial | B (skull base) |
| C (convexity) | ||
| III | Calvarial with extracalvarial extension | B (skull base) |
| C (convexity) |
Histopathological features are also important factors affecting tumor recurrence and prognosis. Recurrence was noted in 22% of benign intraosseous meningiomas in the literature, while it was reportedly 33% in cases of tumors with atypical or malignant pathology. In addition, aggressive atypical or malignant meningiomas had a significantly higher mortality of 29% compared to tumors with benign features (4.8%) [3]. Osteolytic meningiomas may have a higher incidence of atypical or malignant features [6]. In previous reports, benign features were reported in 87–89% of all extradural meningiomas, whereas in our literature review of osteolytic intraosseous meningiomas, 26% of cases were WHO grade II or III [3, 8].
Wide surgical excision is the main treatment for extradural meningiomas, and it is potentially curative if complete resection is achieved [6, 7]. In the present case, a small portion of the tumor near the jugular foramen could not be removed due to the possibility of cranial nerve injury. In the case of skull base lesions that cannot be totally resected, decompression of vital neural structures is performed.
In conclusion, we performed surgical treatment for a rare case of primary osteolytic intraosseous meningioma in the skull base with extension to the cervical area. The histopathologic diagnosis was atypical meningioma. If possible, complete resection is the treatment of choice, and serial follow-up should be done to confirm recurrence or progression.
Additional file
Figure S1. Immunohistochemical staining results. The tumor showed a wild-type p53 pattern (A, × 200) and exhibited strong cytoplasmic expression of β-catenin (B, × 200). Some tumor cells exhibited weak membranous expression of EGFR (C, × 200). The tumor was negative for Bcl-2 (D, × 200). The tumor shows membrane and cytoplasmic immunopositivity for EMA (E, × 200) and negative for S-100 protein (F, × 200). Vimentin is diffusely expressed in the cytoplasm of tumor cells (G, × 200). The Ki-67 proliferation index is estimated to be approximately 15% (H, × 200). Scale bar = 100 μm. (DOCX 8214 kb)
Acknowledgements
Not applicable.
Abbreviations
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- WHO
World Health Organization
Authors’ contributions
SMK collected data and drafted the manuscript. YK critically revised the manuscript and supervised the study. SSB performed the pathological analysis. All authors revised the manuscript and approved the final version.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
This study was approved by the institutional review board of Hanyang University Medical Center.
Consent for publication
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. A copy of the signed consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sae Min Kwon, Email: kwonsaemin@hanmail.net.
Yong Ko, Phone: +82-2-2290-8492, Email: koy8497@hanyang.ac.kr.
Seong Sik Bang, Email: grypony@naver.com.
References
- 1.Agrawal V, Ludwig N, Agrawal A, Bulsara KR. Intraosseous Intracranial Meningioma. Am J Neuroradiol. 2007;28:314–315. [PMC free article] [PubMed] [Google Scholar]
- 2.Muzumdar DP, Vengsarkar US, Bhatjiwale MG, Goel A. Diffuse calvarial meningioma: a case report. J Postgrad Med. 2001;47:116. [PubMed] [Google Scholar]
- 3.Lang FF, Macdonald OK, Fuller GN, DeMonte F. Primary extradural meningiomas: a report on nine cases and review of the literature from the era of computerized tomography scanning. J Neurosurg. 2000;93:940–950. doi: 10.3171/jns.2000.93.6.0940. [DOI] [PubMed] [Google Scholar]
- 4.Nicolay S, De Foer B, Bernaerts A, Van Dinther J, Parizel PM. A case of a temporal bone meningioma presenting as a serous otitis media. Acta Radiol Short Rep. 2014;3:2047981614555048. doi: 10.1177/2047981614555048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoye SJ, Hoar CS, Murray JE. Extracranial meningioma presenting as a tumor of the neck. Am J Surg. 1960;100:486–489. doi: 10.1016/0002-9610(60)90394-9. [DOI] [PubMed] [Google Scholar]
- 6.Elder JB, Atkinson R, Zee C-S, Chen TC. Primary intraosseous meningioma. Neurosurg Focus. 2007;23:E13. doi: 10.3171/FOC-07/10/E13. [DOI] [PubMed] [Google Scholar]
- 7.Crawford TS, Kleinschmidt-DeMasters BK, Lillehei KO. Primary intraosseous meningioma. Case report. J Neurosurg. 1995;83:912–915. doi: 10.3171/jns.1995.83.5.0912. [DOI] [PubMed] [Google Scholar]
- 8.Mattox A, Hughes B, Oleson J, Reardon D, McLendon R, Adamson C. Treatment recommendations for primary extradural meningiomas. Cancer. 2011;117:24–38. doi: 10.1002/cncr.25384. [DOI] [PubMed] [Google Scholar]
- 9.Liu Y, Wang H, Shao H, Wang C. Primary extradural meningiomas in head: a report of 19 cases and review of literature. Int J Clin Exp Pathol. 2015;8:5624. [PMC free article] [PubMed] [Google Scholar]
- 10.Klein EW, Farhat SM, Hoskins PA, Colvin JT. Radionuclide cerebral angiographic evaluation of a diploic extracranial meningioma: case report. J Nucl Med Off Publ Soc Nucl Med. 1975;16:833–834. [PubMed] [Google Scholar]
- 11.McWhorter JM, Ghatak NR, Kelly DL. Extracranial meningioma presenting as lytic skull lesion. Surg Neurol. 1976;5:223–224. [PubMed] [Google Scholar]
- 12.Palma L, Mercuri S, Ferrante L. Epidural calvarial meningioma. Surg Neurol. 1977;8:315–318. [PubMed] [Google Scholar]
- 13.Pearl GS, Takei Y, Parent AD, Boehm WM. Primary intraosseous meningioma presenting as a solitary osteolytic skull lesion: case report. Neurosurgery. 1979;4:269–270. doi: 10.1227/00006123-197903000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Ohaegbulam SC. Ectopic epidural calvarial meningioma. Surg Neurol. 1979;12:33–35. [PubMed] [Google Scholar]
- 15.Young PH. Solitary subcutaneous meningioma appearing as an osteolytic skull defect. South Med J. 1983;76:1039–1040. doi: 10.1097/00007611-198308000-00027. [DOI] [PubMed] [Google Scholar]
- 16.Kaneko F, Takase K, Nishiyama K, Kusaka K, Morizumi H, Matsumoto K. Report of a case of intraosseous meningioma. No Shinkei Geka. 1988;16:197–202. [PubMed] [Google Scholar]
- 17.Lee WH, Tu YC, Liu MY. Primary intraosseous malignant meningioma of the skull: case report. Neurosurgery. 1988;23:505–508. doi: 10.1227/00006123-198810000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Oka K, Hirakawa K, Yoshida S, Tomonaga M. Primary calvarial meningiomas. Surg Neurol. 1989;32:304–310. doi: 10.1016/0090-3019(89)90235-8. [DOI] [PubMed] [Google Scholar]
- 19.Ammirati M, Mirzai S, Samii M. Primary intraosseous meningiomas of the skull base. Acta Neurochir (Wien). 1990;107:56–60. doi: 10.1007/BF01402613. [DOI] [PubMed] [Google Scholar]
- 20.Kulali A, Ilçayto R, Rahmanli O. Primary calvarial ectopic meningiomas. Neurochirurgia (Stuttg). 1991;34:174–177. doi: 10.1055/s-2008-1052084. [DOI] [PubMed] [Google Scholar]
- 21.Ito H, Takagi H, Kawano N, Yada K. Primary intraosseous meningioma: case report. J Neurooncol. 1992;13:57–61. doi: 10.1007/BF00172946. [DOI] [PubMed] [Google Scholar]
- 22.Fujita T, Nakagawa H, Tsuruzono K, Izumoto S, Kadota T, Wada A. Extradural temporal meningioma directly extended to cervical bone--case report. Neurol Med Chir (Tokyo). 1993;33:458–462. doi: 10.2176/nmc.33.458. [DOI] [PubMed] [Google Scholar]
- 23.Ghobashy A, Tobler W. Intraosseous calvarial meningioma of the skull presenting as a solitary osteolytic skull lesion: case report and review of the literature. Acta Neurochir (Wien). 1994;129:105–108. doi: 10.1007/BF01400883. [DOI] [PubMed] [Google Scholar]
- 24.Partington MD, Scheithauer BW, Piepgras DG. Carcinoembryonic antigen production associated with an osteolytic meningioma. Case report. J Neurosurg. 1995;82:489–492. doi: 10.3171/jns.1995.82.3.0489. [DOI] [PubMed] [Google Scholar]
- 25.Levin M, Wertheim SE, Klein E, Lowry J. Unusual lytic intraosseous meningioma. J Neuroimaging Off J Am Soc Neuroimaging. 1995;5:247–248. doi: 10.1111/jon199554247. [DOI] [PubMed] [Google Scholar]
- 26.Kuzeyli K, Duru S, Baykal S, Usul H, Ceylan S, Aktürk F. Primary intraosseous meningioma of the temporal bone in an infant. A case report. Neurosurg Rev. 1996;19:197–199. doi: 10.1007/BF00512053. [DOI] [PubMed] [Google Scholar]
- 27.Changhong L, Naiyin C, Yuehuan G, Lianzhong Z. Primary intraosseous meningiomas of the skull. Clin Radiol. 1997;52:546–549. doi: 10.1016/S0009-9260(97)80333-9. [DOI] [PubMed] [Google Scholar]
- 28.Muthukumar N. Primary calvarial meningiomas. Br J Neurosurg. 1997;11:388–392. doi: 10.1080/02688699745862. [DOI] [PubMed] [Google Scholar]
- 29.Kudo H, Maeda S, Takamoto T, Tamaki N. Intraosseous meningioma with a dural defect. Neurol Med Chir (Tokyo). 1998;38:229–231. doi: 10.2176/nmc.38.229. [DOI] [PubMed] [Google Scholar]
- 30.Okamoto S, Hisaoka M, Aoki T, Kadoya C, Kobanawa S, Hashimoto H. Intraosseous microcystic meningioma. Skeletal Radiol. 2000;29:354–357. doi: 10.1007/s002560000217. [DOI] [PubMed] [Google Scholar]
- 31.Yamazaki T, Tsukada A, Uemura K, Satou H, Tsuboi K, Nose T. Intraosseous meningioma of the posterior fossa--Case report. Neurol Med Chir (Tokyo). 2001;41:149–153. doi: 10.2176/nmc.41.149. [DOI] [PubMed] [Google Scholar]
- 32.Rosahl SK, Mirzayan M-J, Samii M. Osteolytic intra-osseous meningiomas: illustrated review. Acta Neurochir (Wien). 2004;146:1245–1249. doi: 10.1007/s00701-004-0380-7. [DOI] [PubMed] [Google Scholar]
- 33.Tokgoz N, Oner YA, Kaymaz M, Ucar M, Yilmaz G, Tali TE. Primary intraosseous meningioma: CT and MRI appearance. AJNR Am J Neuroradiol. 2005;26:2053–2056. [PMC free article] [PubMed] [Google Scholar]
- 34.Bassiouni H, Asgari S, Hübschen U, König H-J, Stolke D. Dural involvement in primary extradural meningiomas of the cranial vault. J Neurosurg. 2006;105:51–59. doi: 10.3171/jns.2006.105.1.51. [DOI] [PubMed] [Google Scholar]
- 35.Al-Khawaja D, Murali R, Sindler P. Primary calvarial meningioma. J Clin Neurosci Off J Neurosurg Soc Australas. 2007;14:1235–1239. doi: 10.1016/j.jocn.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 36.Sheikhrezaie A, Meybodi AT, Hashemi M, Shafiee S. Primary intraosseous osteolytic meningioma of the skull: a case report. Cases J. 2009;2:7413. doi: 10.1186/1757-1626-0002-0000007413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yener U, Bayrakli F, Vardereli E, Sav A, Peker S. Intradiploic meningioma mimicking calvarial metastasis: case report. Turk Neurosurg. 2009;19:297–301. [PubMed] [Google Scholar]
- 38.Hong B, Hermann EJ, Klein R, Krauss JK, Nakamura M. Surgical resection of osteolytic calvarial lesions: clinicopathological features. Clin Neurol Neurosurg. 2010;112:865–869. doi: 10.1016/j.clineuro.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 39.Kim H, Jung T-Y, Kim I-Y, Lee J-K. Two cases of primary osteolytic intraosseous meningioma of the skull metastasizing to whole skull and the spine. J Korean Neurosurg Soc. 2012;51:151–154. doi: 10.3340/jkns.2012.51.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akhaddar A, Ennouali H. Intraosseous extradural meningioma of the frontal bone. Pan Afr Med J. 2014;17:69. doi: 10.11604/pamj.2014.17.69.3844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tang V, Lam M, Lai A. Intraosseous meningioma mimicking a metastasis. BMJ Case Rep. 2014;2014. [DOI] [PMC free article] [PubMed]
- 42.Yun J-H, Lee S-K. Primary osteolytic intraosseous atypical meningioma with soft tissue and dural invasion: report of a case and review of literatures. J Korean Neurosurg Soc. 2014;56:509–512. doi: 10.3340/jkns.2014.56.6.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim HS, Kim SH, Kim HJ, Kang SW, Kim SJ, Lee JH, et al. Primary Benign Intraosseous Meningioma on (18)F-FDG PET/CT Mimicking Malignancy. Nucl Med Mol Imaging. 2014;48:153–156. doi: 10.1007/s13139-013-0259-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bujok J, Bienioszek M. Microcystic variant of an intraosseous meningioma in the frontal area: a case report. Case Rep Neurol Med. 2014;2014:527267. doi: 10.1155/2014/527267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon SY, Shin HS, Kim TH, Kim HJ. Primary Intraosseous Osteolytic Meningioma of the Skull Mimicking Scalp Mass: A Case Report and Review of Literature. Brain Tumor Res Treat. 2015;3:151–155. doi: 10.14791/btrt.2015.3.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hong SC, Woon K, O’Keeffe B. Brain mushroom: A case of osteolytic intraosseous meningioma with transcalvaria herniation. Br J Neurosurg. 2015;29:876–878. doi: 10.3109/02688697.2015.1029432. [DOI] [PubMed] [Google Scholar]
- 47.Ben Nsir A, Ben Hamouda K, Hammedi F, Kilani M, Hattab N. Osteolytic clear cell meningioma of the petrous bone occurring 36 years after posterior cranial fossa irradiation: Case report. Neurol Neurochir Pol. 2016;50:297–302. doi: 10.1016/j.pjnns.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 48.Bohara S, Agarwal S, Khurana N, Pandey PN. Primary intraosseous atypical inflammatory meningioma presenting as a lytic skull lesion: Case report with review of literature. Indian J Pathol Microbiol. 2016;59:386–388. doi: 10.4103/0377-4929.188131. [DOI] [PubMed] [Google Scholar]
- 49.Mouri G, Suzuki H, Hatazaki S, Matsubara T, Taki W. Skull Meningioma Associated with Intradural Cyst: A Case Report. Clin Med Insights Case Rep. 2017;10:1179547617738231. doi: 10.1177/1179547617738231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richardson TE, Georgescu M-M, Kapur P, Hwang H, Barnett SL, Raisanen JM, et al. Unusual skull tumors with psammomatoid bodies: a diagnostic challenge. Clin Neuropathol. 2017;36(2017):114–120. doi: 10.5414/NP300997. [DOI] [PubMed] [Google Scholar]
- 51.Shuangshoti S, Netsky MG, Fitz-Hugh GS. Parapharyngeal meningioma with special reference to cell of origin. Ann Otol Rhinol Laryngol. 1971;80:464–473. doi: 10.1177/000348947108000327. [DOI] [PubMed] [Google Scholar]
- 52.Perzin KH, Pushparaj N. Nonepithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx. A clinicopathologic study. XIII: Meningiomas. Cancer. 1984;54:1860–1869. doi: 10.1002/1097-0142(19841101)54:9<1860::AID-CNCR2820540916>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 53.Pompili A, Caroli F, Cattani F, Iachetti M. Intradiploic meningioma of the orbital roof. Neurosurgery. 1983;12:565–568. doi: 10.1227/00006123-198305000-00016. [DOI] [PubMed] [Google Scholar]
- 54.Azar-Kia B, Sarwar M, Marc JA, Schechter MM. Intraosseous meningioma. Neuroradiology. 1974;6:246–253. doi: 10.1007/BF00345784. [DOI] [PubMed] [Google Scholar]
- 55.Turner OA, Laird AT. Meningioma with traumatic etiology. Report of a case. J Neurosurg. 1966;24:96–98. doi: 10.3171/jns.1966.24.1.0096. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Immunohistochemical staining results. The tumor showed a wild-type p53 pattern (A, × 200) and exhibited strong cytoplasmic expression of β-catenin (B, × 200). Some tumor cells exhibited weak membranous expression of EGFR (C, × 200). The tumor was negative for Bcl-2 (D, × 200). The tumor shows membrane and cytoplasmic immunopositivity for EMA (E, × 200) and negative for S-100 protein (F, × 200). Vimentin is diffusely expressed in the cytoplasm of tumor cells (G, × 200). The Ki-67 proliferation index is estimated to be approximately 15% (H, × 200). Scale bar = 100 μm. (DOCX 8214 kb)
Data Availability Statement
Not applicable.