Key Points
Question
Are objective measures of surgeon effort and surgical specialty associated with the assigned work relative value units of procedures?
Findings
In this cross-sectional study of 628 unique Current Procedural Terminology codes from 1 239 991 patient observations, 80% of the variations in assigned work relative value units were associated with procedures’ operative time, length of stay, and readmission and reoperation rates. Statistically significant differences remained, however, across surgical specialties despite controlling for these measures.
Meaning
Incorporating objective data from a surgical registry may improve the relative value unit assignment and update processes, including reducing the differences across specialties.
Abstract
Importance
The primary data sources used to generate and update work relative value units (RVUs) are surveys of small groups of specialists who are asked to estimate the time and intensity needed to perform surgical procedures. Because these surveys are conducted by specialty societies and rely on subjective data, these sources have been challenged as potentially biased.
Objective
To assess whether objective work measures are associated with a surgical procedure’s assigned work RVUs and whether differences exist by surgical specialty.
Design, Setting, and Participants
This cross-sectional study obtained data from the 2016 and 2017 participant use files of the American College of Surgeons National Surgical Quality Improvement Program. The 2017 physician fee schedule of the Centers for Medicare & Medicaid Services was a secondary data source. Procedures were included if they had at least 100 patient-level observations over the 2-year period. Data were analyzed from August 29, 2018, to April 2, 2019.
Main Outcomes and Measures
The dependent variable was a procedure’s assigned work RVU. Independent variables of work RVUs were 4 procedure-level work measures (median operative time, median postoperative length of stay, all-cause 30-day readmission rate, and all-cause 30-day reoperation rate) and surgeon specialty (10-level category using general surgery as the reference).
Results
The data set included 628 unique Current Procedural Terminology (CPT) codes and 726 CPT-specialty combinations from 1 239 991 patient observations. Statistically significant associations were found between each work measure and assigned work RVU, as follows: median operative time (R2 = 0.74; 95% CI, 0.71-0.78), postoperative length of stay (R2 = 0.42; 95% CI, 0.36-0.48), rate of readmission (R2 = 0.18; 95% CI, 0.13-0.23), and rate of reoperation (R2 = 0.15; 95% CI, 0.10-0.20). Including all 4 measures explained 80.2% (95% CI, 77.3%-83.1%) of the variation. Adding the surgical specialty improved the overall fit of the model (likelihood ratio test χ2 = 231.27; P < .001). Cardiac (7.78; 95% CI, 4.25-11.31; P < .001) and neurosurgery (2.46; 95% CI, 1.08-3.83; P < .001) had higher work RVUs compared with general surgery, whereas orthopedics (–1.53; 95% CI, –2.48 to –0.59; P = .002), urology (–1.58; 95% CI, –2.88 to –0.29; P = .02), plastics (–2.70; 95% CI, –4.39 to –1.01; P = .002), and otolaryngology (–3.05; 95% CI, –4.69 to –1.42; P < .001) had lower work RVUs compared with general surgery.
Conclusions and Relevance
Objective work measures appeared to be associated with assigned work RVUs, predominantly with operative time; registry data can be used to augment and inform the generation and updating processes of the work RVUs.
This cross-sectional study evaluates the current system for generating and updating the data used to quantify the relative value unit of a surgeon’s work for each surgical procedure.
Introduction
In 1992, Medicare transitioned physician compensation from a fee-based system to the resource-based relative value scale.1 Private insurers followed suit.2 Under the resource-based relative value scale, physician payments are determined by 3 components, the largest of which is physician work (51%) followed by practice expense (45%) and professional lability insurance (4%).3 Each component is assigned a numeric relative value unit (RVU), which is multiplied by a geographic practice cost index and a monetary conversion factor (in 2018, the factor was $36). The sum of these 3 components is the overall reimbursement for a given Current Procedural Terminology (CPT) code.3,4
The initial work RVUs were generated in the 1980s and 1990s using the results of a national survey to assess the relative time and complexity of each CPT code.5 Since then, adjustments to the work RVU have relied on the recommendations of the Relative Value Scale Update Committee (RUC) of the American Medical Association. The primary data used by the RUC to generate recommendations are responses from surveys of surgeons, who provide estimates of the time and the intensity required of a given procedure. A national effort by the Society of Thoracic Surgeons in the mid-2000s led to the incorporation of objective data into the assignment of some cardiothoracic RVUs.6 The other surgical specialties rely on survey data, a system that has been heavily criticized.3,7,8
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) reports data that could be used to guide work RVU assignment across surgical specialties. The present study aimed to assess whether objective measures of surgeon effort (ie, work measures), such as operative time, are associated with assigned work RVU and whether differences by surgical specialty exist after controlling for these work measures.
Methods
The primary data sources for this cross-sectional study were the 2016 and 2017 essential participant use files of the ACS NSQIP. A secondary data source was the 2017 physician fee schedule of the Centers for Medicare & Medicaid Services (CMS).9 Data from the ACS NSQIP and the participating hospitals have not been verified, and these sources are not responsible for the statistical validity of this data analysis or the conclusions derived. Data were analyzed from August 29, 2018, to April 2, 2019. Because no patient identifiers were included in the ACS NSQIP or the CMS files, the University of California, Los Angeles (UCLA) Institutional Review Board determined that this study did not meet the definition of human participant research. This article was prepared following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.10
The 2 aims of the study were to assess (1) whether objective work measures of surgeons from a national registry are associated with assigned work RVUs and (2) whether surgical specialty is associated with assigned work RVUs after controlling for available work measures.
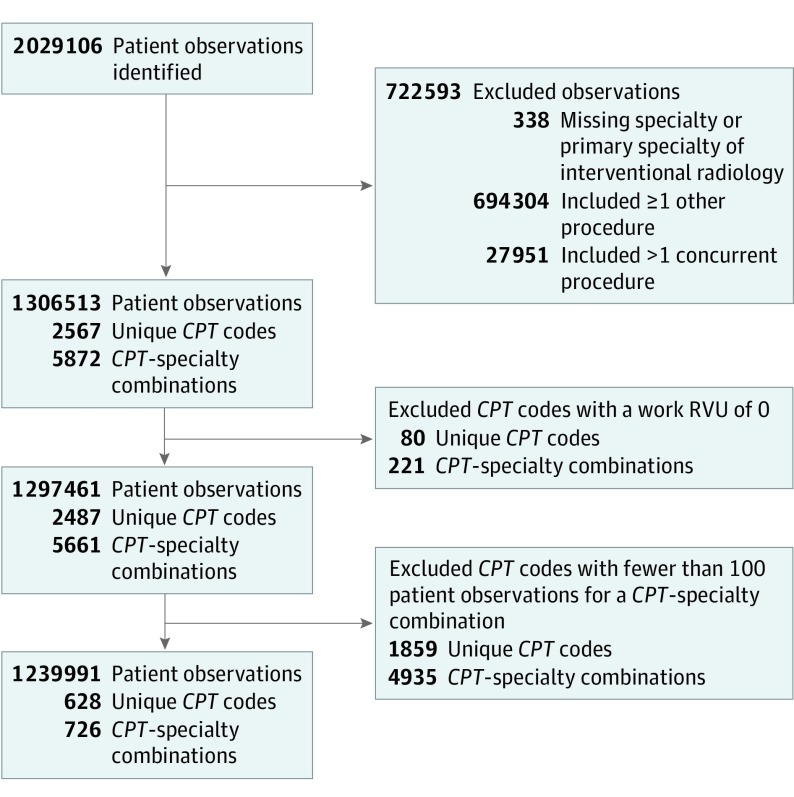
Figure 1 shows the flow diagram for the analytic sample, which comprised 3 units: (1) patient observations used to generate procedure-level measures, (2) unique CPT codes, and (3) CPT-specialty combinations. Because multiple specialties can perform a procedure but may have different work measures (eg, the procedure time for a gynecologist performing a lysis of adhesions may vary from that of a general surgeon), the unit of analysis was the CPT-specialty combination.
Figure 1. Flow Diagram of the Study Sample.
CPT indicates Current Procedural Terminology.
We started with all patient observations from the combined 2016 and 2017 files of the ACS NSQIP. Observations with missing specialty or with a primary specialty of interventional radiology were excluded. Similarly, observations with more than 1 operation, either performed by the same surgical team (other) or a separate surgical team (concurrent), were excluded. After these exclusions, the file was collapsed to the procedure level: The analytic sample included 1 procedure-level observation for orthopedic surgeons performing total knee arthroplasty, instead of 100 000 individual total knee arthroplasty observations. Next, we excluded CPT codes with an assigned work RVU of 0. These primarily represented CPT codes that are not specific enough for CMS to reimburse, such as CPT 37799 (vascular surgical procedure). We limited the analysis to procedures with at least 100 underlying patient-level observations. This limit was imposed to focus the analysis on high-volume CPT codes and to allow precise estimation of procedure-level variables. Because this number was selected subjectively, the analyses were repeated using both higher (n = 250) and lower (n = 50) thresholds.
The dependent variable was the procedure’s assigned work RVU. Work RVU is provided for every observation in the ACS NSQIP file on the basis of primary CPT code. However, to externally verify the work RVUs in the ACS NSQIP file, we compared the CMS file with the ACS NSQIP file. The work RVUs available in the ACS NSQIP file were correct more than 99% of the time. For the few discrepancies, we used the CMS value.
Independent variables of work RVUs included 4 work measures and surgeon specialty. The 4 work measures were (1) median operative time, defined from procedure start to procedure end, in minutes; (2) median postoperative length of stay (LOS) in days; (3) all-cause 30-day readmission rate; and (4) all-cause 30-day reoperation rate. These 4 measures were included because they were the only measures in the ACS NSQIP file that directly reflected actual surgeon effort (eg, time in the operating room for primary operation or repeated operation, or time spent on patient rounds during index or subsequent admissions). We recognized that repeated operations would generate a new CPT code and therefore did not anticipate an association between reoperation rates and work RVUs, but nevertheless we included reoperation rate as it may also reflect operation complexity. We explored alternative measures of complexity, such as a procedure’s mean mortality or adverse event rates, but we generally found no association and did not include them in multivariate models because of collinearity. Surgeon specialty was a 10-level categorical variable included in the ACS NSQIP file. The included procedures had no missing data.
Statistical Analysis
All analyses were conducted using Stata, version 15.1 (StataCorp LLC) with statistical significance determined using 2-sided tests and an α = .05. Two statistical tests were used: a likelihood ratio test for comparing nested models, and a Wald test for evaluating the significance of a coefficient in a linear regression model.
To address study aim 1, bivariate and subsequent multivariate linear regression models were fit using assigned work RVU as the dependent variable and work measures as covariates. Multiple models were fit to account for possible nonlinear associations and interactions (eTables 1-3 in the Supplement). Collinearity was addressed by de-meaning variables and was assessed using variance inflation factors. Model fit was compared using Akaike information criterion. From the final model, we generated estimated work RVUs. Residuals were calculated as the estimated work RVU minus the actual RVU and were standardized to identify outliers (>2 standard residuals).
To address study aim 2, we added surgeon specialty to the model and evaluated the overall effect on model fit as well as the individual coefficients for each specialty. The general surgery specialty was used as the reference category because it included the largest number of CPT codes. We ran several sensitivity checks, including using different volume thresholds, and because of a slight skew in the work RVU distribution, we repeated our analysis using negative binomial regression.
Results
The final data set included 628 unique CPT codes and 726 CPT-specialty combinations derived from 1 239 991 patient observations (Figure 1). Of the 628 unique CPT codes, 543 (86.5%) were performed by 1 specialty, 76 (12.1%) by 2 specialties, 5 (0.8%) by 3 specialties, and 4 (0.6%) by 4 specialties. An example of a procedure performed by more than 1 specialty is CPT 11041 (debridement of subcutaneous tissue), which is undertaken by general, orthopedic, plastic, and vascular surgeons. The median (interquartile range [IQR]) number of patient observations used to generate procedure-level statistics was 334 (170-931), with a range from 100 to 112 095.
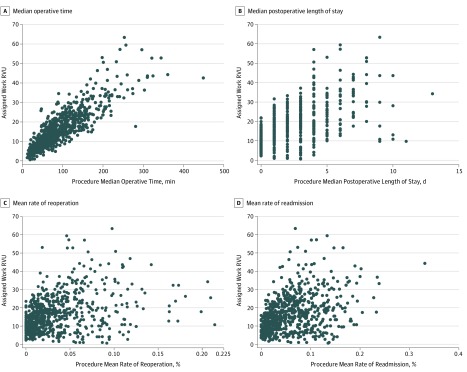
Scatterplots illustrating the unadjusted association between each work measure and assigned work RVU are shown in Figure 2. Each dot represents a CPT-specialty combination. Statistically significant associations were observed between each work measure and assigned work RVU: median operative time (R2 = 0.74; 95% CI, 0.71-0.78), postoperative LOS (R2 = 0.42; 95% CI, 0.36-0.48), rate of readmission (R2 = 0.18; 95% CI, 0.13-0.23), and rate of reoperation (R2 = 0.15; 95% CI, 0.10-0.20). Assuming linear associations, mean work RVUs increased by 0.14 (95% CI, 0.14-0.15) per minute of operative time, by 2.76 (95% CI, 2.51-3.00) per postoperative day, by 0.84 (95% CI, 0.71-0.98) per percentage risk of readmission, and by 0.96 (95% CI, 0.77-1.15) per percentage risk of reoperation.
Figure 2. Bivariate Associations Between Procedure-Level Surgeon Work Measures and Assigned Work Relative Value Units (RVUs).
Because more than 1 specialty may perform a given surgical procedure, some Current Procedural Terminology (CPT) codes are duplicated. These CPT codes have the same assigned work RVUs but may have different work measures, depending on a specialty’s specific work measures.
The final model included all 4 work measures and explained 80.2% (95% CI, 77.3%-83.1%) of the variation in the procedure’s assigned work RVU (eTable 2 in the Supplement). Estimated work RVUs were generated for each CPT-specialty combination (eTable 4 in the Supplement). Table 1 includes high and low outliers. An example of a potentially overvalued CPT code is 33410 (open replacement of the aortic valve), which had an estimated work RVU of 32.87 (actual RVU, 46.41) based on a 186-minute median operative time, 6-day LOS, 7.5% rate of reoperation, and 5.6% rate of readmission. An example of a potentially undervalued CPT code is 27 882 (guillotine amputation through the tibia and fibula), which had an estimated work RVU of 18.64 (actual RVU, 9.79) based on a 27-minute median operative time, 11-day LOS, 12.5% rate of reoperation, and 15.7% rate of readmission.
Table 1. Procedures With Outlier Assigned Work Relative Value Units.
| CPT Code | CPT Description | Specialty | Median | Rate, % | Actual Work RVU | Estimated Work RVU | Difference (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|
| Operative Time, min | Postoperative LOS, d | Reoperation | Readmission | ||||||
| Potentially Overvalued Procedures | |||||||||
| 33410 | Replacement of aortic valve—open | Cardiac surgery | 186 | 6 | 7.5 | 5.6 | 46.41 | 32.87 | 13.54 (4.82 to 22.26) |
| 33430 | Replacement of mitral valve | Cardiac surgery | 233 | 8 | 10.2 | 9.0 | 50.93 | 40.11 | 10.82 (2.13 to 19.50) |
| 33361 | Replacement of aortic valve—percutaneous | Cardiac surgery | 78.5 | 2 | 4.2 | 10.2 | 25.13 | 15.19 | 9.94 (1.17 to 18.70) |
| 47125 | Partial removal of liver—total left lobectomy | General | 198 | 5 | 1.8 | 7.4 | 53.04 | 33.39 | 19.65 (10.92 to 28.38) |
| 47122 | Extensive removal of liver—trisegmentectomy | General | 257 | 6 | 4.6 | 13.3 | 59.48 | 40.02 | 19.46 (10.76 to 28.16) |
| 47130 | Partial removal of liver—total right lobectomy | General | 242 | 6 | 4.9 | 11.2 | 57.19 | 38.86 | 18.33 (9.60 to 27.05) |
| 49020 | Drainage of abdominal abscess—open | General | 47 | 6 | 9.7 | 12.4 | 26.67 | 14.71 | 11.96 (3.23 to 20.69) |
| 47120 | Partial removal of liver—partial lobectomy | General | 160 | 4 | 1.6 | 7.4 | 39.01 | 27.94 | 11.07 (2.33 to 19.81) |
| 43848 | Revision of gastroplasty | General | 134 | 3 | 4.7 | 11.6 | 32.75 | 23.42 | 9.33 (0.57 to 18.08) |
| 61697 | Brain aneurysm repair—complex | Neurosurgery | 253 | 9 | 9.8 | 6.9 | 63.40 | 43.64 | 19.76 (11.16 to 28.37) |
| 61700 | Brain aneurysm repair—simple | Neurosurgery | 201 | 4 | 7.1 | 5.9 | 50.62 | 31.80 | 18.82 (10.09 to 27.54) |
| 61520 | Removal of brain lesion—cerebellopontine angle tumor | Neurosurgery | 296.5 | 4 | 6.6 | 10.2 | 57.09 | 40.44 | 16.65 (8.04 to 25.27) |
| 61521 | Removal of brain lesion—midline tumor at base of skull | Neurosurgery | 211 | 4 | 11.8 | 12.7 | 46.99 | 31.46 | 15.53 (6.81 to 24.24) |
| 22857 | Lumbar artificial discectomy | Neurosurgery | 99 | 1 | 0.7 | 1.5 | 27.13 | 16.22 | 10.91 (2.14 to 19.67) |
| 61518 | Removal of brain lesion—infratentorial or posterior fossa | Neurosurgery | 182 | 4 | 7.8 | 14.2 | 39.89 | 29.41 | 10.48 (1.74 to 19.23) |
| 61312 | Opening of skull for drainage | Neurosurgery | 88 | 7 | 13.2 | 10.0 | 30.17 | 20.96 | 9.21 (0.51 to 17.91) |
| 63056 | Decompression of spinal cord—lumbar | Orthopedics | 62.5 | 0 | 1.4 | 0.9 | 21.86 | 10.14 | 11.72 (2.96 to 20.49) |
| 22856 | Cervical artificial discectomy | Orthopedics | 87 | 1 | 0.6 | 0.9 | 24.05 | 14.49 | 9.56 (0.79 to 18.32) |
| 50947 | Laparoscopic ureteroneocystectomy with cystoscopy and ureteral stent placement | Urology | 46 | 1 | 2.9 | 4.9 | 25.78 | 9.37 | 16.41 (7.64 to 25.18) |
| 33880 | Endovascular repair of descending thoracic aorta with coverage of left subclavian artery origin | Vascular | 90 | 3 | 6.4 | 8.3 | 34.58 | 17.66 | 16.92 (8.16 to 25.68) |
| 33881 | Endovascular repair of descending thoracic aorta without coverage of left subclavian artery origin | Vascular | 89 | 3 | 5.6 | 8.1 | 29.58 | 17.64 | 11.94 (3.18 to 20.71) |
| 35082 | Repair of artery—ruptured aorta | Vascular | 169 | 7 | 11.0 | 3.8 | 42.09 | 31.39 | 10.70 (2.05 to 19.35) |
| Potentially Undervalued Procedures | |||||||||
| 45111 | Partial removal of rectum | General | 172 | 5 | 10.2 | 13.1 | 18.01 | 29.18 | −11.17 (−19.91 to −2.42) |
| 49568 | Implantation of mesh for open incisional or ventral hernia repair or closure of debridement for necrotizing soft tissue infection | General | 82 | 1 | 3.6 | 5.4 | 4.88 | 14.49 | −9.61 (−18.38 to −0.84) |
| 11006 | Debridement of genitalia, perineum, and abdominal wall | General | 51 | 10 | 8.5 | 7.8 | 13.10 | 22.22 | −9.12 (−17.63 to −0.62) |
| 24546 | Treatment of humerus fracture | Orthopedics | 171.5 | 1 | 1.9 | 6.5 | 14.91 | 25.70 | −10.79 (−19.53 to −2.05) |
| 24435 | Repair of humerus with graft | Orthopedics | 163 | 1 | 2.5 | 5.9 | 14.99 | 24.70 | −9.71 (−18.46 to −0.96) |
| 38780 | Removal of abdominal lymph nodes | Urology | 281 | 4 | 0.0 | 7.7 | 17.70 | 39.58 | −21.88 (−30.45 to −13.32) |
| 21705 | Revision of neck muscle/rib | Vascular | 117 | 2 | 3.6 | 3.6 | 9.92 | 19.96 | −10.04 (−18.80 to −1.28) |
| 27882 | Guillotine amputation through tibia and fibular | Vascular | 27 | 11 | 12.5 | 15.7 | 9.79 | 18.64 | −8.85 (−17.17 to −0.53) |
Abbreviations: CPT, Current Procedural Terminology; LOS, length of stay, RVU, relative value unit.
The distribution of potentially overvalued and undervalued procedures was not balanced between specialties (Table 2). At the extremes, cardiac had 1 procedure with lower-than-expected RVUs and 5 procedures with higher-than-expected RVUs, compared with otolaryngology, which had 28 of 35 procedures with lower-than-expected RVUs and 7 of 35 procedures with higher-than-expected RVUs.
Table 2. Proportion of Surgical Procedures Within a Specialty With Lower-Than-Expected Work Relative Value Units .
| Specialty | Procedures Evaluated, No. | Procedures With Lower-Than-Expected Work RVUs, No. (%) |
|---|---|---|
| Cardiac surgery | 6 | 1 (17) |
| Neurosurgery | 50 | 16 (32) |
| General | 215 | 101 (47) |
| Gynecology | 69 | 34 (49) |
| Orthopedics | 166 | 97 (58) |
| Urology | 56 | 33 (59) |
| Vascular | 78 | 49 (63) |
| Thoracic | 19 | 13 (68) |
| Plastics | 32 | 23 (72) |
| Otolaryngology | 35 | 28 (80) |
Abbreviation: RVU, relative value unit.
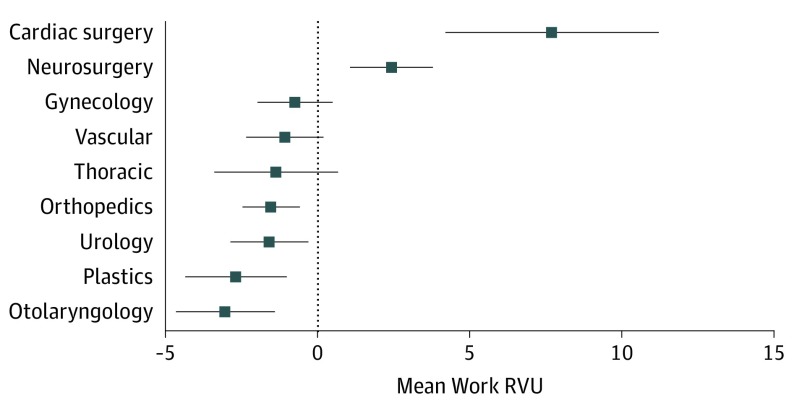
Adding the surgical specialty improved the overall fit of the regression model (likelihood ratio test χ2 = 231.27; P < .001). The association of individual specialties with assigned work RVU, using general surgery as the reference, is included in Figure 3. Cardiac (7.78; 95% CI, 4.25-11.31; P < .001) and neurosurgery (2.46; 95% CI, 1.08-3.83; P < .001) had higher assigned work RVUs compared with general surgery (reference). Orthopedics (–1.53; 95% CI, –2.48 to –0.59; P = .002), urology (–1.58; 95% CI, –2.88 to –0.29; P = .02), plastics (–2.70; 95% CI, –4.39 to –1.01; P = .002), and otolaryngology (–3.05; 95% CI, –4.69 to –1.42; P < .001) had lower work RVUs compared with general surgery, after controlling for the available work measures. These findings remained largely the same on sensitivity analyses (eFigures 1 and 2 in the Supplement).
Figure 3. Association of Surgeon Specialty With Assigned Work Relative Value Units (RVUs) .
Shown is a linear regression model with the assigned work RVU as the dependent variable with a 10-level categorical variable for specialty (reference: general surgery) as the primary independent variable. Covariates included the specialty-specific procedure median operative time; median postoperative length of stay; reoperation rate; and readmission rate, including quadratic terms when appropriate (full model is included in eTable 2 in the Supplement). Error bars represent the 95% CI around the point estimate. A specialty with an error bar completely to the right of the dotted vertical line may be interpreted as, after controlling for the available surgeon work measures, having higher mean work RVU values compared with general surgery. A specialty with an error bar entirely to the left of the dotted vertical line may be interpreted as, after controlling for the available surgeon work measures, having lower mean work RVU values compared with general surgery.
Eighty-five CPT codes were performed by more than 1 specialty. Estimated work RVUs were within 10% of each other for 46 CPT codes, within 20% for 66 CPT codes, and within 50% for 80 CPT codes.
Discussion
Four objective surgeon work measures (operative time, postoperative LOS, rate of readmission, and rate of reoperation) collectively explain 80% of the variation in a procedure’s assigned work RVU. However, certain specialties perform procedures that may be undervalued or overvalued according to these objective data.
Understanding the implications for these findings requires a detailed evaluation of the status quo. In the initial physician surveys to generate work RVUs, work was broken into 4 components, known as the building blocks of the work RVU: (1) preservice, (2) intraservice (ie, skin-to-skin time), (3) immediate postservice (eg, talking to family), and (4) postoperative evaluation and management.11,12 Each component was assigned an RVU that reflected the multiple of time spent and intensity (work = time × intensity). Because physicians confounded time and intensity, they were asked to estimate work as 1 combined variable instead of 2 separate measures. Although this system may appear to be comprehensive, it was found by a RAND analysis to have a number of nonsensical patterns.11 For example, for CPT code 33322 (suture repair of the aorta), the RVU calculated for the postoperative evaluation and management building block was higher than the total work RVU. Furthermore, reverse-calculating the intraservice intensity values (intensity = work / time) found that nearly 16% of values were illogical (either negative or obvious outliers). The reason for these idiosyncrasies lay in the surveying and updating processes.
For more than 20 years, updates have fallen under the purview of the RUC, which develops recommendations with specialty societies and passes them to CMS, which, more often than not, accepts these recommendations without modification.7 The RUC is a 31-member group, in which surgeons permanently occupy 9 seats. The primary data sources used by the RUC are the results from physician surveys conducted by the specialty societies. The specialty society surveys approximately 30 practicing surgeons, asking them to estimate the time and total work involved for a procedure. This system has been heavily criticized. First, specialty societies are typically given the right of first refusal about whether to reevaluate an assigned RVU. As expected, most codes that are reevaluated are believed to be undervalued instead of overvalued. Second, the surveys have a low response rate and small sample, limiting precision, and several studies have found that physician time measures (eg, procedure time) are uniformly overestimated in this process.13,14 One strategy used by the RUC is to use the 25th percentile from the survey responses, recognizing that overestimation is common. Third, the process cannot keep up with the rapid gains in efficiency. Measures from the 1980s likely do not reflect today’s practice.11 The RUC has adopted a number of changes over the past decade, such as increasing the number of survey respondents for high-volume CPT codes (>100 000 per year) and increasing the frequency with which they identify and review misvalued codes, but the primary dependence on survey data continues. Despite the ready availability of objective data in the ACS NSQIP file, we are not aware of its use in any formal capacity to inform RUC recommendations.
How do we reconcile the measures and analytic approach used in this study with the existing work RVU assignment process? The building block method requires 8 measures, separate time and intensity measures for each component. No database exists that can provide time measures for all 4 components, let alone measures of intensity. Even if a prospective database were generated to objectively track measures across all surgical CPT codes, surgeons would not likely agree on measures that fully capture a procedure’s intensity. There are differences in the technical skill and mental stress that a procedure requires, but measuring these elements in a reliable fashion across specialties seems unlikely.
This study adopted a different approach. We included 4 measures readily available in the ACS NSQIP file (operative time, postoperative LOS, readmission rate, and reoperation rate). Operative time measures intraservice time and is directly analogous to the measure employed by CMS. We do not have time measures of the preservice, immediate postservice, and postoperative evaluation and management, nor do we have objective measures of intensity for any component. However, the 3 measures we did use (LOS and rates of readmission and reoperation) may represent objective and reliable proxies. It seems reasonable that more complex procedures should manifest, in some way, in one of these measures. Adding readmission and reoperation rates did not improve the fit of our model dramatically, suggesting that operative time and LOS alone may be strong proxies for complexity. Ultimately, we believe the question becomes that of measurement. A survey system may be able to capture the nuanced differences in technical skill or mental stress, but do we believe a system that relies on small surveys conducted by specialty societies to more accurately and unbiasedly capture the full effort of surgeons than a system that relies on objective measures, even if these objective measures are incomplete?
The model presented in this study could not and should not be used to assign work RVUs. If the underlying data on which the model rests (assigned work RVUs) are biased, then this would be counterintuitive. However, this analysis does have a number of potential uses. First, analyses like these can help identify outlier procedures. Second, as CPT codes are re-reviewed, ACS NSQIP statistics can be provided to survey respondents, the specialty society, and the RUC as they develop their recommendations. Third, the current model, one that weights operative time most heavily, does not have to continue. Should measures such as readmission and reoperation rates be equally or more important? Conversely, if lower readmission rates are a sign of improved quality, should RVUs be inversely associated with these quality measures? What additional measures, either reflecting time or intensity, could be captured by the ACS NSQIP that would improve work RVU assignment, such as preoperative and postoperative clinic visits, intensive care unit time, amount of time spent at the bedside, or measures of mental stress? Fourth, efforts are needed to understand the disparities identified across specialties. This analysis found systematic differences in assigned work RVUs across specialties, and although most variations were small, that for cardiac was notable. This deviation in cardiac procedures likely reflects the effort by the Society of Thoracic Surgeons that resulted in an increase in cardiothoracic work RVUs in 2007. The society accomplished this outcome by using objective data from its database for procedure time and LOS, performing a national survey to estimate intensity, and substantial political maneuvering with the RUC and CMS. A report of the society’s effort concluded that other specialties should generate databases to inform their own work RVU estimates.6 The ACS NSQIP and other registries could replicate this process for all surgical specialties.
Limitations
This study has a number of limitations. First, the ACS NSQIP data were skewed toward inpatient procedures with higher work RVUs and therefore were not useful for evaluating many outpatient-based procedures. The National Survey of Ambulatory Surgery historically provided comprehensive clinical data for outpatient procedures but was discontinued and last performed in 2006, so an alternative data source is needed. Second, the ACS NSQIP data were provided by a biased sample of participating hospitals with work measures that may not be generalizable to all hospitals. Third, the inability to model intrasurgeon and intrahospital variations may have resulted in inaccurate CIs. Fourth, we focused on surgical CPT codes. We did not address the concerns associated with the disparities between evaluation and management codes and procedural codes or between medical and surgical practitioners.15
Conclusions
Objective work measures appeared to be associated with assigned work RVUs, predominantly with median operative time. However, differences remain across surgical specialties despite controlling for these work measures. Registry data can be used to inform the generation and updating processes of the work RVUs.
eTable 1. Bivariate Associations
eTable 2. Building Multivariate Model Including Variable Transformations
eTable 3. Testing Potential Interactions
eTable 4. Full List of Included Procedures With Actual and Predicted Work Relative Value Units
eFigure 1. Changing the Sample Size Threshold Required to Include a Procedure in the Regression Model
eFigure 2. Negative Binomial Regression
References
- 1.American Medical Association An introduction to the RUC. https://www.ama-assn.org/rvs-update-committee-ruc. Accessed November 28, 2018.
- 2.McCormack LA, Burge RT. Diffusion of Medicare’s RBRVS and related physician payment policies. Health Care Financ Rev. 1994;16(2):159-173. [PMC free article] [PubMed] [Google Scholar]
- 3.American Medical Association The RVS update process booklet. https://www.ama-assn.org/rvs-update-committee-ruc. Accessed November 28, 2018.
- 4.American Medical Association Medicare physician payment schedules. https://www.ama-assn.org/practice-management/medicare-physician-payment-schedules. Accessed November 28, 2018.
- 5.Hsiao WC, Braun P, Yntema D, Becker ER. Estimating physicians’ work for a resource-based relative-value scale. N Engl J Med. 1988;319(13):835-841. [DOI] [PubMed] [Google Scholar]
- 6.Smith PK, Mayer JE Jr, Kanter KR, et al. ; STS/AATS Workforce on Nomenclature and Coding . Physician payment for 2007: a description of the process by which major changes in valuation of cardiothoracic surgical procedures occurred. Ann Thorac Surg. 2007;83(1):12-20. [DOI] [PubMed] [Google Scholar]
- 7.Laugesen MJ, Wada R, Chen EM. In setting doctors’ Medicare fees, CMS almost always accepts the relative value update panel’s advice on work values. Health Aff (Millwood). 2012;31(5):965-972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klepper B. The RUC, health care finance’s star chamber, remains untouchable. Health Affairs Blog. doi: 10.1377/hblog20130201.027753. Published February 1, 2013. Accessed November 20, 2018. [DOI]
- 9.Centers for Medicare & Medicaid Services PFS relative value files. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html. Accessed November 21, 2018
- 10.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. [DOI] [PubMed] [Google Scholar]
- 11.Wynn BO, Burgette LF, Mulcahy AW, et al. Development of a model for the validation of work relative value units for the Medicare physician fee schedule. Rand Health Q. 2015;5(1):5. [PMC free article] [PubMed] [Google Scholar]
- 12.Mabry CD, McCann BC, Harris JA, et al. The use of intraservice work per unit of time (IWPUT) and the building block method (BBM) for the calculation of surgical work. Ann Surg. 2005;241(6):929-938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burgette LF, Mulcahy AW, Mehrotra A, Ruder T, Wynn BO. Estimating surgical procedure times using anesthesia billing data and operating room records. Health Serv Res. 2017;52(1):74-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCall N, Cromwell J, Braun P. Validation of physician survey estimates of surgical time using operating room logs. Med Care Res Rev. 2006;63(6):764-777. [DOI] [PubMed] [Google Scholar]
- 15.Sinsky CA, Dugdale DC. Medicare payment for cognitive vs procedural care: minding the gap. JAMA Intern Med. 2013;173(18):1733-1737. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Bivariate Associations
eTable 2. Building Multivariate Model Including Variable Transformations
eTable 3. Testing Potential Interactions
eTable 4. Full List of Included Procedures With Actual and Predicted Work Relative Value Units
eFigure 1. Changing the Sample Size Threshold Required to Include a Procedure in the Regression Model
eFigure 2. Negative Binomial Regression