Key Points
Question
What is the prevalence of therapeutic inertia and its associated factors?
Findings
In this cohort study that included 195 neurologists with expertise in multiple sclerosis, the prevalence and magnitude of therapeutic inertia among a Canadian group were the lowest compared with Argentina, Chile, and Spain. Seeing a higher number of patients per week, years of practice, and participation from Canada were associated with a lower likelihood of therapeutic inertia, whereas aversion to ambiguity was associated with a higher likelihood of therapeutic inertia.
Meaning
Therapeutic inertia is common among practicing neurologists, with practical implications for patients with multiple sclerosis.
This cohort study compares therapeutic inertia, the failure to escalate therapy when goals are unmet, among neurologists across 4 countries (Canada, Argentina, Chile, and Spain) and identifies factors contributing to therapeutic inertia.
Abstract
Importance
There is growing interest in understanding and addressing factors that govern the decision-making process in multiple sclerosis (MS) care. Therapeutic inertia (TI) is the failure to escalate therapy when goals are unmet. Limited data are available on the prevalence of TI and factors affecting therapeutic decisions in the management of patients with MS worldwide.
Objectives
To compare TI across 4 countries (Canada, Argentina, Chile, and Spain) and to identify factors contributing to TI.
Design, Setting, and Participants
Prospective cohort study conducted between July 10, 2017, and May 4, 2018. Participants were exposed to behavioral experiments in which instruments were used to assess their risk preferences (eg, aversion to ambiguity) and therapeutic decisions in 10 simulated MS case scenarios. Mixed-effects linear and logistic regression analyses were performed to determine the association between the participants’ baseline characteristics and TI. The association of unmeasured confounders was assessed by the E-value and a bootstrapping analysis. This multicenter study included neurologists practicing at academic and community centers in Canada, Argentina, Chile, and Spain who make therapeutic decisions for patients with MS.
Main Outcomes and Measures
The primary outcome was the prevalence of TI. The TI score was calculated by dividing the number of case scenarios in which participants showed TI by the number of case scenarios that measured TI. Higher TI scores indicated greater degrees of TI. The secondary outcome was the identification of factors that contributed to TI.
Results
Of 300 neurologists with expertise in MS care who were invited to be part of the study, 226 (75.3%) agreed to participate. Among those who initially showed interest in participating, 195 physicians (86.3%) completed the study, while 31 did not. The mean (SD) age of participants was 43.3 (11.2) years; 52.3% were male. Therapeutic inertia was present in 72.8% (142 of 195) of participants, leading to suboptimal decisions in 20.4% (318 of 1560) of case scenarios. The prevalence of TI among the Canadian group was the lowest compared with the other 3 countries (60.0% [33 of 55] vs 77.9% [109 of 140]; P = .01). For the primary outcome, the TI score in the Canadian group (mean [SD], 0.98 [1.15]) was significantly lower compared with groups from other countries (mean [SD], 1.70 [1.43] for Argentina, 2.24 [1.54] for Chile, and 2.56 [1.64] for Spain) (P = .001). The mixed-effects linear models revealed that participants from Argentina, Chile, and Spain (combined) had higher TI scores compared with their Canadian counterparts (β coefficient, 0.90; 95% CI, 0.52-1.28; P < .001). A higher number of patients with MS per week (OR, 0.44; 95% CI, 0.22-0.88), years of practice (OR, 0.93; 95% CI, 0.86-0.99), and participation from Canada (OR, 0.47; 95% CI, 0.23-0.96) were associated with a lower likelihood of TI. Aversion to ambiguity was associated with a 2-fold higher likelihood of TI (OR, 2.25; 95% CI, 1.02-5.00). All 95% CIs of the β coefficients of covariates were lower than the E-value of 2.35, making it unlikely for the results to be due to the association of unmeasured confounders.
Conclusions and Relevance
This study showed that Canadian participants had the lowest prevalence and magnitude of TI. Higher TI scores were associated with a lower expertise in MS care and with a greater tendency for aversion to ambiguity.
Introduction
Multiple sclerosis (MS) is an evolving field, with an increasing number of proven effective therapies.1,2,3 Given the broad spectrum of disease-modifying therapies (DMTs), neurologists may face therapeutic dilemmas when individualizing decisions regarding the most appropriate DMT for their patients.4,5 It is challenging to decide on an optimal DMT for an individual patient based on the patient’s clinical disease activity, magnetic resonance imaging (MRI) lesion burden, drug availability, adverse effect profile, and patient preferences.1 Despite the recent advances in MS therapeutics, many patients remain undertreated.6 Numerous factors contribute to the suboptimal management, including education gaps in both risk management and decision making among treating physicians.7
The concept of clinical inertia was initially introduced by Phillips et al8 in 2001, who defined it as lack of therapy escalation when it is clinically indicated. The term clinical inertia was substituted with therapeutic inertia (TI) in 2006 by Okonofua et al.9 Therapeutic inertia is prevalent not only among patients with MS but also in other chronic conditions, such as diabetes and hypertension.10,11,12
There is growing interest in understanding and addressing factors that govern the decision-making process13,14 in MS. A particular interest is identifying variables that alter the therapeutic decision making of remaining on the same DMT or escalating to a more effective agent, which can be associated with a possible increase in the risk of serious adverse effects.1,2
Factors contributing to TI remain poorly understood. However, the results of some studies6,15 suggest that physician-associated factors (eg, low tolerance to uncertainty and aversion to ambiguity) may have a role in the decision-making process. In addition, there is limited understanding of country-specific differences with regard to the prevalence of TI. Accordingly, the primary aim of this study was to compare the prevalence of TI among MS-treating physicians in 4 countries (Canada, Argentina, Chile, and Spain). The secondary aim of the study was to identify factors contributing to TI.
Methods
Study Population
This prospective cohort study was conducted between July 10, 2017, and May 4, 2018, and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. Our study population consisted of neurologists who primarily focus their clinical practice on MS care from 4 countries (55 in Canada, 90 in Argentina, 25 in Chile, and 25 in Spain). Participants were invited to take part in the study via email by scientific organizations based in each country (Canadian Consortium of MS Clinics and NeuroSens, Instituto de Neurociencias Buenos Aires [INEBA] and Argentine Neurological Society, Chilean Society of Neurology, and Spanish Neurological Society). Each participant received an email with instructions and a link to start the study. Participants not actively involved in patient care or those who followed up a low volume of patients with MS (<12 patients with MS per year) were excluded.
Informed consent was provided online at the beginning of the study by each participant. Participants received compensation for completing the surveys that is equivalent to US $100. The study was approved by the Research Ethics Board of St Michael’s Hospital, University of Toronto, Toronto, Ontario, Canada.
Data Collection
Participants provided information regarding their clinical practice and expertise and completed behavioral experiments to assess their risk preferences. Thereafter, participants were exposed to 10 simulated MS case scenarios and made therapeutic choices (case scenarios are available in the eAppendix in the Supplement). Case scenarios were designed by team members (M.T. and G.S.) and by MS experts (J.O. and a nonauthor) to reflect current clinical practice. Eight of the cases required escalation of therapy; therefore, the failure to do so by the participant was considered as TI. The other 2 cases were designed to detect overtreatment when treatment escalation was not deemed medically necessary. All participants were exposed to the same case scenarios. Details of behavioral experiments in which instruments were used in the assessment of tolerance to uncertainty and risk aversion are described elsewhere.6,16,17 In brief, participants were asked to choose between 2 options of (1) either winning US $400 or $0 when the probability is 50/50 (represented by a blue/red bar) vs (2) an option of unknown probability (represented by a blue/red bar covered by a gray bar) of the same outcome. Participants who favored the known probability of 50/50 were deemed to have aversion to ambiguity, while other participants were considered as having tolerance to uncertainty. Risk was assessed by asking participants to provide the minimal amount of US dollars (or healthy years) that they would prefer over a 50/50 chance of winning US $400 (or longer survival with adverse effects of a treatment). The degree of risk aversion of each individual corresponded to the difference of the expected value of the risky option (US $200) minus the participant’s response.16
We also evaluated physicians’ tolerance to uncertainty in a patient’s care using the Reaction to Uncertainty Test.17 The test was composed of 5 questions that the respondent rated from 0 to 5, which were summed to give a total score. Higher scores represent a lower tolerance to uncertainty. Low tolerance to uncertainty was defined as values above the median of the total score. Further details of the protocol are published elsewhere.18 Responses from case scenarios were analyzed in light of responses from the behavioral components.
Definitions
Disease activity was defined as a clinical relapse that was associated with the presence of one of the following MRI findings: at least 1 gadolinium-enhancing lesion or 5 or more new brain lesions.19,20 These thresholds were defined based on prior studies demonstrating in patients receiving interferon beta that risk of treatment failure highly correlates with a clinical relapse and MRI lesions as defined above.21 Disease progression in MS was defined as at least 1 point of sustained worsening from baseline in the Expanded Disability Status Scale Score.22
At the time of the study, treatment options for relapsing-remitting MS included first-line therapies (beta interferons, glatiramer acetate, teriflunomide, and dimethyl fumarate), second-line therapy (fingolimod), and third-line therapies (natalizumab and alemtuzumab).4 Given variation in market approval status of some DMTs among the countries in which the study was conducted, ocrelizumab and cladribine were not included in case scenarios. For this analysis, we used the 3-line treatment escalation scheme according to current clinical practice.6,23
Outcome Measures
The primary outcome was the prevalence of TI. As in previous studies,6,24 the TI score was calculated by dividing the number of case scenarios in which participants showed TI by the number of case scenarios that measured TI (n = 8). Higher TI scores indicated greater degrees of TI. The TI score ranged between 0 and 8.
Therapeutic inertia prevalence was defined as the proportion of participants with TI in at least 1 case scenario. The secondary outcome was the identification of factors that contributed to TI.
Statistical Analysis
The primary analysis compared TI between Canada and the other 3 countries combined (ie, Argentina, Chile, and Spain). We included different measures of TI as both continuous and categorical variables to determine the consistency of our results. We used mixed-effects linear and logistic models to assess associations between TI score and TI to determine the association between the participants’ baseline characteristics and the primary outcome of interest after accounting for clustering. We included the following explanatory variables: age, sex, specialty, number of patients with MS seen per week, proportion of time devoted to clinical care, coauthor of a peer-reviewed publication in the last year (yes or no), practice setting (academic vs nonacademic), risk aversion, aversion to ambiguity, and physicians’ reaction to uncertainty (above or below the median).
This multicenter study included neurologists practicing at academic and community centers in Canada, Argentina, Chile, and Spain who make therapeutic decisions for patients with MS. To account for unmeasured confounding, we used an E-value estimate and a bootstrapping analysis to compare the β coefficients in the normal, percentile, bias-corrected, and bias-corrected and accelerated 95% CIs. The E-value is a tool to assess the consequences of unmeasured confounding in observational studies.25 By comparing the upper 95% CI with the 95% CI of covariates included in the models, the E-value provides an estimate of the residual confounding that could explain an observed association if an unmeasured covariate exists.25
All tests were 2 tailed, and P values less than .05 were considered statistically significant. The area under the curve was used to assess the discrimination, and the Hosmer-Lemeshow test was used to assess the calibration of the model.
Results
Of 300 neurologists with expertise in MS care who were invited to be part of the study, 226 (75.3%) agreed to participate. Among those who initially showed interest in participating, 195 physicians (86.3%) completed the study, while 31 did not. The mean (SD) age of participants was 43.3 (11.2) years; 52.3% were male. Eighty-six (44.1%) were MS specialists. Table 1 summarizes baseline characteristics by country.
Table 1. Baseline Characteristics of Participants Between July 10, 2017, and May 4, 2018.
| Characteristic | Total (N = 195) | Canada (n = 55) | Combined (n = 140)a | P Value |
|---|---|---|---|---|
| Age, mean (SD), y | 43.3 (11.2) | 41.8 (12.0) | 43.9 (10.8) | .24 |
| Sex, No. (%) | ||||
| Female | 93 (47.7) | 26 (47.3) | 67 (47.9) | .94 |
| Male | 102 (52.3) | 29 (52.7) | 73 (52.1) | |
| Specialty, No. (%) | ||||
| General neurologist who cares for MS | 109 (55.9) | 24 (43.6) | 85 (60.7) | .03 |
| MS specialist | 86 (44.1) | 31 (56.4) | 55 (39.3) | |
| No. of patients with MS seen/week, mean (SD) | 19.4 (11.6) | 22.2 (14.6) | 18.4 (10.0) | .04 |
| Years of practice, mean (SD) | 16.7 (11.4) | 13.3 (11.2) | 17.9 (12.2) | .01 |
| ≥75% of time devoted to clinical practice, No. (%) | 98 (50.3) | 30 (54.5) | 68 (48.6) | .45 |
| Coauthor of a peer-reviewed publication in the last year, No. (%) | 92 (47.2) | 31 (56.4) | 61 (43.6) | .11 |
Abbreviation: MS, multiple sclerosis.
Combined countries are Argentina, Chile, and Spain.
Overall, the prevalence of TI was 72.8% (142 of 195), leading to suboptimal decisions in 20.4% (318 of 1560) of case scenarios. The mean (SD) TI score for the accountable 8 case scenarios was 1.68 (1.50). For every 10 case scenarios with moderate to high risk of disease progression, this suggested that there would be 2 suboptimal decisions (eg, lack of treatment escalation) when clinical evidence of relapses and radiological evidence of disease activity exist.
Outcome Measures
Comparison of TI Between Canada and Other Countries
For the primary outcome, the TI score in the Canadian group (mean [SD], 0.98 [1.15]) was significantly lower compared with groups from other countries (mean [SD], 1.70 [1.43] for Argentina, 2.24 [1.54] for Chile, and 2.56 [1.64] for Spain) (P = .001). The prevalence of TI among the Canadian group was also the lowest compared with the other 3 countries (60.0% [33 of 55] vs 77.9% [109 of 140], P = .01). Values adjusted for age, specialty, number of patients with MS seen per week, years of practice, and aversion to ambiguity are summarized in Table 2 and Figure 1.
Table 2. Adjusted TI Score and Prevalence of TI by Country.
| Country | TI Score (95% CI)a | Multivariable Analysis for TI Score, β Coefficient (95% CI) | P Valuea | Prevalence of TI, % (95% CI)a |
|---|---|---|---|---|
| Canada | 0.98 (0.63-1.33) | 1 [Reference] | NA | 63.7 (49.4-76.0) |
| Argentina, Chile, and Spain combined | 1.95 (1.73-2.17) | 0.90 (0.52-1.28) | <.001 | 78.0 (70.0-84.2) |
| Argentina | 1.70 (1.42-1.98) | 0.65 (0.24-1.06) | .002 | 72.5 (62.9-82.2) |
| Chile | 2.24 (1.72-2.76) | 0.92 (0.21-1.64) | .01 | 61.7 (39.3-84.1) |
| Spain | 2.56 (2.04-3.08) | 1.74 (1.07-2.42) | <.001 | 96.4 (89.5-100) |
Abbreviations: NA, not applicable; TI, therapeutic inertia.
Adjusted for age, specialty, number of patients with multiple sclerosis seen per week, years of practice, and aversion to ambiguity after accounting for clustering.
Figure 1. Therapeutic Inertia (TI) Score by Country.
Adjusted TI scores are compared across the studied countries. The vertical bars represent 95% CIs. Estimates were derived from linear regression models after adjustment for age, specialty, number of patients with multiple sclerosis seen per week, years of practice, and aversion to ambiguity.
Participant’s risk preferences based on assessments with behavioral instruments are listed in Table 3. Compared with Canada, participants from the other countries were more risk averse and had a lower tolerance to uncertainty (reflected by higher scores) (Table 3). For example, the Canadian group had a lower proportion of participants with values below the certainty equivalence of US $120 (value that identifies participants with risk aversion) compared with their counterparts (20.0% [11 of 55] vs 37.1% [52 of 140], P = .02).
Table 3. Results of Behavioral Experiments Designed to Assess Risk and Aversion to Ambiguitya.
| Country | Risk Financial Domain, Mean (SD) Score | Risk Health Domain, Mean (SD) Score | Aversion to Ambiguity, No./Total No. (%) | Physicians’ Reaction to Uncertainty, Mean (SD) Scoreb |
|---|---|---|---|---|
| Canada | 213.5 (77.2) | 14.9 (3.4) | 41/55 (74.5) | 19.1 (8.6) |
| Argentina, Chile, and Spain combined | 179.5 (97.0)c | 14.3 (4.9) | 93/140 (66.4) | 23.1 (9.3)d |
| Argentina | 159.6 (102.3)e | 12.7 (7.0)c | 54/90 (60.0) | 23.3 (9.3)e |
| Chile | 233.2 (104.0) | 11.2 (5.1)e | 20/25 (80.0) | 23.1 (10.6) |
| Spain | 183.2 (47.9) | 14.9 (3.7) | 19/25 (76.0) | 22.5 (7.9) |
P values are for comparison with Canada (reference group).
Higher scores indicate a lower tolerance to uncertainty.
P = .02.
P = .006.
P < .001.
Participants with an aversion to ambiguity had higher TI scores, although this factor did not reach statistical significance (mean, 1.90 vs 1.57; P = .15). Participants with an aversion to ambiguity also had a significantly higher TI prevalence (82.0% [50 of 61] vs 68.7% [92 of 134], P = .047).
The mixed-effects linear models revealed that participants from Argentina, Chile, and Spain (combined) had higher TI scores compared with their Canadian counterparts (β coefficient, 0.90; 95% CI, 0.52-1.28; P < .001). Similarly, participants from Argentina, Chile, and Spain (combined) had a higher likelihood of TI compared with the Canadian participants (odds ratio [OR], 2.30; 95% CI, 1.10-4.82; P = .03). The observed vs predicted TI scores after adjustment for covariates are shown in the eFigure in the Supplement. Details by country are listed in Table 2.
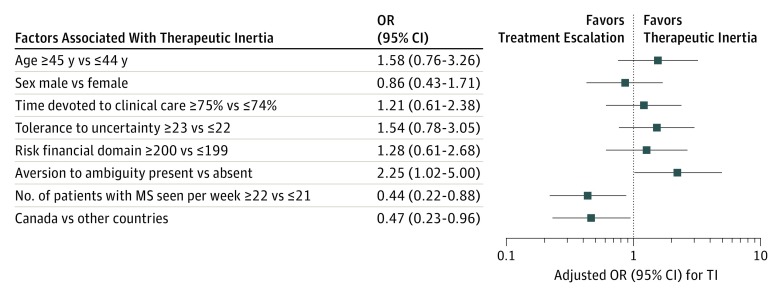
Factors Associated With TI
The multivariable analysis aimed at identifying factors associated with the prevalence of TI revealed that a higher number of patients with MS per week (OR, 0.44; 95% CI, 0.22-0.88), years of practice (OR, 0.93; 95% CI, 0.86-0.99), and participation from Canada (OR, 0.47; 95% CI, 0.23-0.96) were associated with a lower likelihood of TI. Aversion to ambiguity was associated with a 2-fold higher likelihood of TI (OR, 2.25; 95% CI, 1.02-5.00) (Figure 2). The model showed good discrimination (area under the curve, 0.783) and calibration (Hosmer-Lemeshow test P = .90). Participants from Argentina, Chile, and Spain (combined) had 2.40 (95% CI, 1.16-5.06) higher odds of TI.
Figure 2. Factors Associated With Therapeutic Inertia (TI).
Factors associated with TI are shown. A higher number of patients with multiple sclerosis (MS) seen per week and country (ie, Canada) were associated with a lower TI, whereas aversion to ambiguity was associated with a higher TI. OR indicates odds ratio.
Assessment of Unmeasured Confounding
We estimated the E-value using the standardized difference of the mean TI score (point estimate, 0.667; standard error, 0.128; and true association with shift estimate, 0.227). The E-value for the point estimate was 2.35, and the CI was 1.66. All 95% CIs of the β coefficients of covariates were lower than the E-value of 2.35 (eTable 1 in the Supplement), making it unlikely for the results to be due to the association of unmeasured confounders. The bootstrapping analysis showed similarities among the β coefficients within each covariate, suggesting unbiased estimates of the TI scores (eTable 2 in the Supplement).
Discussion
Therapeutic inertia is a well-known phenomenon influencing physicians who manage patients with chronic conditions, including MS.6 Our study showed that neurologists with expertise in MS from 4 different countries exhibited varying degrees of TI. Overall, TI was present in 72.8% (142 of 195) of participants and altered at least 1 in 5 therapeutic decisions. Therapeutic inertia was 2.3-fold more prevalent among neurologists from Argentina, Chile, and Spain (combined) compared with their Canadian counterparts.
The most important factors associated with TI include a lower expertise in MS care (eg, fewer years of experience and a lower number of patients with MS seen per week), country of practice, and a higher aversion to ambiguity. The mixed multivariable analysis supports the contention that aversion to ambiguity was an independent predictor of the prevalence of TI after accounting for demographic factors, level of expertise, and regional variations. We also found that unmeasured confounders were unlikely to have altered our findings.
The country of primary clinical practice was also identified as an independent predictor of TI. The observed differences among countries can be partially explained by variations in adherence to published MS management guidelines,2,26,27 regional differences regarding eligibility and access to DMTs,28 public funding of DMTs, and physician-related factors, such as risk preferences and education in risk management and decision making.
Recognizing the presence of TI and contributing factors is essential in identifying strategies aimed at improving medical education, which could lead to better patient outcomes. For example, the results of recent studies suggest that innovative therapeutic interventions (eg, a traffic light system) may be useful to ameliorate the prevalence and magnitude of TI. In brief, the traffic light system creates a link between a color (representing a risk level) and an action. Red light indicates “high risk” or “stop and think,” yellow light indicates “intermediate risk” or “reassess soon,” and green light indicates “low risk” or “continue the same strategy.” When applied in clinical sittings, this method facilitates the decision-making process.29 A subsequent randomized clinical trial targeting neurologists with MS expertise showed a 70% reduction in TI (OR, 0.30; 95% CI, 0.10-0.89) for the traffic light system educational intervention arm compared with usual care.30
Limitations
Our study has several limitations. The small numbers of participants from Chile and Spain may have altered the accuracy of estimates. As a result, we reported the comparison of TI between Canada and the other 3 countries combined and also analyzed the role of unmeasured confounders. Another limitation is that physicians’ decisions to escalate therapy are influenced by factors like availability of the drug, local policies, drug costs, variations in treatment guidelines in different countries, and other unmeasured variables that can alter the assessment of TI.26,31,32 However, all included countries shared private and government-funded MS drug coverage in the absence of private health insurance.33,34 A previous study35 showed a limited role of costs in explaining therapeutic decisions and TI. In addition, physicians’ performance on case scenarios might not accurately mirror real-life decisions, although such inconsistency would be expected to underestimate the true prevalence of TI among participants. Also, we cannot rule out the possibility of some residual confounding despite a comprehensive adjustment of baseline characteristics.
Conclusions
This study demonstrates the high prevalence of and factors associated with TI even among neurologists with expertise in MS care. To date, our study is the first, to our knowledge, to systematically compare TI using identical case scenarios across countries. This study constitutes a first step in understanding the mechanisms of TI and increases awareness of its high prevalence. Our findings may also lead to the development of further studies that assess strategies to reduce TI, which may result in improved outcomes for patients with MS. We propose larger studies to evaluate the potential benefits of educational interventions to ameliorate TI. If proven effective, these strategies could be included in curricula for undergraduate and postgraduate medical programs to improve the existing education gaps of formal training in risk management and decision-making.
eAppendix. Case Vignette Answered by Participating Physicians
eFigure. Observed vs Predicted TI Score After Adjustment for Covariates
eTable 1. Mixed Linear Regression Model Adjusted for Clustering
eTable 2. Bootstrap Linear Regression to Compare Normal vs Bias-Corrected 95% CI
References
- 1.Montalban X, Gold R, Thompson AJ, et al. ECTRIMS/EAN guideline on the pharmacological treatment of people with multiple sclerosis. Mult Scler. 2018;24(2):-. doi: 10.1177/1352458517751049 [DOI] [PubMed] [Google Scholar]
- 2.Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777-788. doi: 10.1212/WNL.0000000000005347 [DOI] [PubMed] [Google Scholar]
- 3.Giovannoni G. Disease-modifying treatments for early and advanced multiple sclerosis: a new treatment paradigm. Curr Opin Neurol. 2018;31(3):233-243. doi: 10.1097/WCO.0000000000000561 [DOI] [PubMed] [Google Scholar]
- 4.Tramacere I, Del Giovane C, Salanti G, D’Amico R, Filippini G. Immunomodulators and immunosuppressants for relapsing-remitting multiple sclerosis: a network meta-analysis. Cochrane Database Syst Rev. 2015;(9):CD011381. doi: 10.1002/14651858.CD011381.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alping P, Frisell T, Novakova L, et al. Rituximab versus fingolimod after natalizumab in multiple sclerosis patients. Ann Neurol. 2016;79(6):950-958. doi: 10.1002/ana.24651 [DOI] [PubMed] [Google Scholar]
- 6.Saposnik G, Sempere AP, Prefasi D, et al. Decision-making in multiple sclerosis: the role of aversion to ambiguity for therapeutic inertia among neurologists (DIScUTIR MS). Front Neurol. 2017;8:65. doi: 10.3389/fneur.2017.00065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dijkstra IS, Pols J, Remmelts P, Brand PL. Preparedness for practice: a systematic cross-specialty evaluation of the alignment between postgraduate medical education and independent practice. Med Teach. 2015;37(2):153-161. doi: 10.3109/0142159X.2014.929646 [DOI] [PubMed] [Google Scholar]
- 8.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825-834. doi: 10.7326/0003-4819-135-9-200111060-00012 [DOI] [PubMed] [Google Scholar]
- 9.Okonofua EC, Simpson KN, Jesri A, Rehman SU, Durkalski VL, Egan BM. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47(3):345-351. doi: 10.1161/01.HYP.0000200702.76436.4b [DOI] [PubMed] [Google Scholar]
- 10.Khunti K, Gomes MB, Pocock S, et al. Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: a systematic review. Diabetes Obes Metab. 2018;20(2):427-437. doi: 10.1111/dom.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lebeau JP, Cadwallader JS, Vaillant-Roussel H, et al. General practitioners’ justifications for therapeutic inertia in cardiovascular prevention: an empirically grounded typology. BMJ Open. 2016;6(5):e010639. doi: 10.1136/bmjopen-2015-010639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nambam B, DuBose SN, Nathan BM, et al. ; T1D Exchange Clinic Network . Therapeutic inertia: underdiagnosed and undertreated hypertension in children participating in the T1D Exchange Clinic Registry. Pediatr Diabetes. 2016;17(1):15-20. doi: 10.1111/pedi.12231 [DOI] [PubMed] [Google Scholar]
- 13.Edelson MG, Polania R, Ruff CC, Fehr E, Hare TA. Computational and neurobiological foundations of leadership decisions. Science. 2018;361(6401):eaat0036. doi: 10.1126/science.aat0036 [DOI] [PubMed] [Google Scholar]
- 14.Lin H, Vartanian O. A neuroeconomic framework for creative cognition. Perspect Psychol Sci. 2018;13(6):655-677. doi: 10.1177/1745691618794945 [DOI] [PubMed] [Google Scholar]
- 15.Aujoulat I, Jacquemin P, Rietzschel E, et al. Factors associated with clinical inertia: an integrative review. Adv Med Educ Pract. 2014;5:141-147. doi: 10.2147/AMEP.S59022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dohmen T, Falk A, Huffman D, Sunde U, Schupp J, Wagner GG. Individual risk attitudes: measurement, determinants, and behavioral consequences. J Eur Econ Assoc. 2011;9(3):522-550. doi: 10.1111/j.1542-4774.2011.01015.x [DOI] [Google Scholar]
- 17.Gerrity M, White K, DeVellis R, Dittus R. Physicians’ reactions to uncertainty: refining the constructs and scales. Motiv Emot. 1995;19(3):175-191. doi: 10.1007/BF02250510 [DOI] [Google Scholar]
- 18.Saposnik G, Sempere AP, Raptis R, Prefasi D, Selchen D, Maurino J. Decision making under uncertainty, therapeutic inertia, and physicians’ risk preferences in the management of multiple sclerosis (DIScUTIR MS). BMC Neurol. 2016;16(1):58. doi: 10.1186/s12883-016-0577-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prosperini L, Mancinelli CR, De Giglio L, De Angelis F, Barletta V, Pozzilli C. Interferon beta failure predicted by EMA criteria or isolated MRI activity in multiple sclerosis. Mult Scler. 2014;20(5):566-576. doi: 10.1177/1352458513502399 [DOI] [PubMed] [Google Scholar]
- 20.Bermel RA, You X, Foulds P, et al. Predictors of long-term outcome in multiple sclerosis patients treated with interferon beta. Ann Neurol. 2013;73(1):95-103. doi: 10.1002/ana.23758 [DOI] [PubMed] [Google Scholar]
- 21.Sormani MP, Gasperini C, Romeo M, et al. ; MAGNIMS Study Group . Assessing response to interferon-β in a multicenter dataset of patients with MS. Neurology. 2016;87(2):134-140. doi: 10.1212/WNL.0000000000002830 [DOI] [PubMed] [Google Scholar]
- 22.Sormani MP, De Stefano N. Defining and scoring response to IFN-β in multiple sclerosis. Nat Rev Neurol. 2013;9(9):504-512. doi: 10.1038/nrneurol.2013.146 [DOI] [PubMed] [Google Scholar]
- 23.Prosperini L, Giannì C, Leonardi L, et al. Escalation to natalizumab or switching among immunomodulators in relapsing multiple sclerosis. Mult Scler. 2012;18(1):64-71. doi: 10.1177/1352458511417481 [DOI] [PubMed] [Google Scholar]
- 24.Saposnik G, Montalban X, Selchen D, et al. Therapeutic inertia in multiple sclerosis care: a study of Canadian neurologists. Front Neurol. 2018;9:781. doi: 10.3389/fneur.2018.00781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haneuse S, VanderWeele TJ, Arterburn D. Using the E-value to assess the potential effect of unmeasured confounding in observational studies. JAMA. 2019;321(6):602-603. doi: 10.1001/jama.2018.21554 [DOI] [PubMed] [Google Scholar]
- 26.García Merino A, Ramón Ara Callizo J, Fernández Fernández O, Landete Pascual L, Moral Torres E, Rodríguez-Antigüedad Zarrantz A. Consensus statement on the treatment of multiple sclerosis by the Spanish Society of Neurology in 2016 [in Spanish]. Neurologia. 2017;32(2):113-119. doi: 10.1016/j.nrl.2016.02.026 [DOI] [PubMed] [Google Scholar]
- 27.Cristiano E, Alonso R, Alvez Pinheiro A, et al. Argentinean recommendations on the identification of treatment failure in relapsing remitting multiple sclerosis patients. J Neurol Sci. 2018;385:217-224. doi: 10.1016/j.jns.2018.01.004 [DOI] [PubMed] [Google Scholar]
- 28.Kaplan WA, Wirtz VJ, Stephens P. The market dynamics of generic medicines in the private sector of 19 low and middle income countries between 2001 and 2011: a descriptive time series analysis. PLoS One. 2013;8(9):e74399. doi: 10.1371/journal.pone.0074399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saposnik G, Maurino J, Sempere AP, et al. Overcoming therapeutic inertia in multiple sclerosis care: a pilot randomized trial applying the traffic light system in medical education. Front Neurol. 2017;8:430. doi: 10.3389/fneur.2017.00430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saposnik G, Mamdani M, Montalban X, et al. Traffic lights intervention reduces therapeutic inertia: a randomized controlled trial in multiple sclerosis care. MDM P&P. In press. doi: 10.1177/2381468319855642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Regulatory process in the United States of America, Europe, China, and Japan. In: Shahzad A, ed. Translational Medicine : Tools and Techniques. Boston, MA: Academic Press; 2016:chap 5. [Google Scholar]
- 32.Garcia R, Araujo DV. The regulation of biosimilars in Latin America. Curr Rheumatol Rep. 2016;18(3):16. doi: 10.1007/s11926-016-0564-1 [DOI] [PubMed] [Google Scholar]
- 33.Ernstsson O, Gyllensten H, Alexanderson K, Tinghög P, Friberg E, Norlund A. Cost of illness of multiple sclerosis: a systematic review. PLoS One. 2016;11(7):e0159129-e0159129. doi: 10.1371/journal.pone.0159129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hartung DM, Bourdette DN, Ahmed SM, Whitham RH. The cost of multiple sclerosis drugs in the US and the pharmaceutical industry: too big to fail? Neurology. 2015;84(21):2185-2192. doi: 10.1212/WNL.0000000000001608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saposnik G, Mamdani M, Terzaghi M, et al. The role of prescribing generic (non-proprietary) drugs in the prevalence of therapeutic inertia in multiple sclerosis care. Front Neurol. 2018;9:835. doi: 10.3389/fneur.2018.00835 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Case Vignette Answered by Participating Physicians
eFigure. Observed vs Predicted TI Score After Adjustment for Covariates
eTable 1. Mixed Linear Regression Model Adjusted for Clustering
eTable 2. Bootstrap Linear Regression to Compare Normal vs Bias-Corrected 95% CI