Abstract
Background:
Chronic arsenic exposure is associated with increased risk for arsenical skin lesions, cancer, and other adverse health outcomes. One potential mechanism of arsenic toxicity is telomere dysfunction. However, prior epidemiological studies of arsenic exposure, telomere length (TL), and skin lesion are small and cross-sectional. We investigated the associations between arsenic exposure and TL and between baseline TL and incident skin lesion risk among individuals participating in the Health Effects of Arsenic Longitudinal Study in Bangladesh (2000–2009).
Methods:
Quantitative PCR was used to measure the average TL of peripheral blood DNA collected at baseline. The association between baseline arsenic exposure (well water and urine) and TL was estimated in a randomly- selected subcohort (n = 1469). A nested case-control study (466 cases and 464 age- and sex-matched controls) was used to estimate the association between baseline TL and incident skin lesion risk (diagnosed < 8 years after baseline).
Results:
No association was observed between arsenic exposure (water or urine) and TL. Among incident skin lesion cases and matched controls, we observed higher skin lesion risk among individuals with shorter TL (Ptrend = 1.5 × 10−5) with odds ratios of 2.60, 1.59, and 1.10 for the first (shortest), second, and third TL quartiles compared to the fourth (longest).
Conclusions:
Arsenic exposure was not associated with TL among Bangladeshi adults, suggesting that leukocyte TL may not reflect a primary mode of action for arsenic’s toxicity. However, short TL was associated with increased skin lesion risk, and may be a biomarker of arsenic susceptibility modifying arsenic’s effect on skin lesion risk.
Keywords: Arsenic, Bangladesh, Drinking water, Skin lesion, Telomere length
1. Introduction
More than 100 million people worldwide experience chronic arsenic exposure through naturally contaminated drinking water (World Health Organization, 2001), including approximately 20–45 million in Bangladesh (Flanagan et al., 2012). Arsenic exposure has been reported to increase the risk of various adverse health outcomes including mortality (Sohel et al., 2009), neurological conditions (Vahidnia et al., 2007), cardiovascular diseases (States et al., 2009), as well as malignancies such as cancers of the skin, bladder, kidney, liver, and lung (Celik et al., 2008; Hopenhayn-Rich et al., 1998; Liu and Waalkes, 2008; Mink et al., 2008; Yu et al., 2006). An early and common sign of arsenic toxicity is the appearance of skin lesions, which can reflect susceptibility to arsenic-related diseases, including cancers (Yu et al., 2006; Cuzick et al., 1982, 1992; Hsu et al., 2013; Arsenic in Drinking Water, 2001).
The mechanism of arsenic’s toxicity and carcinogenicity may be related in part to telomere length and dysfunction. Telomeres are the repeating six-nucleotide sequence binding protein complexes at the end of human chromosomes that protect DNA ends from damage. The telomerase enzyme elongates telomeres in stem and progenitor cells (Shawi and Autexier, 2008). Telomere length (TL) shortening occurs with cell division and has been investigated as a biomarker of aging and susceptibility for age-related health conditions, including cardiovascular diseases, neurocognitive diseases, cancers, and overall mortality (Cawthon et al., 2003; Martin-Ruiz et al., 2006; Sanders and Newman, 2013; Serrano and Andrés, 2004; Willeit et al., 2010), all of which have also been linked with chronic arsenic exposure. In vitro studies of human cord blood cells and human cell lines have shown that arsenic exposure can both increase and decrease TL and telomerase activity depending on dose (Ferrario et al., 2009; Zhang et al., 2003). Acceleration of TL shortening has been attributed in part to oxidative stress and inflammation (Jenny, 2012; O’Donovan et al., 2011; Von Zglinicki, 2002), two processes that are also potential causes of arsenic toxicity (Ahmed et al., 2011; Kitchin, 2001; Liu et al., 2003).
Recent epidemiologic studies linked arsenic exposure to longer TL in peripheral blood and saliva (Chatterjee et al., 2015; Fillman et al., 2016; Gao et al., 2015; Li et al., 2012; Ameer et al., 2016) and altered peripheral blood expression of genes involved in telomere maintenance (Gao et al., 2015; Li et al., 2012; Mo et al., 2009). However, the few published studies of the association between arsenic exposure and TL tend to be small, and only one study to date has investigated the association between TL and arsenical skin lesions—a cross-sectional study that found longer TL in skin lesion subjects (Chatterjee et al., 2015). The goal of this paper was to characterize the role of TL in the arsenic-skin lesion association by answering two questions: 1) whether arsenic exposure is associated with TL; and 2) whether TL is associated with skin lesion risk. Addressing these questions will allow us to determine whether TL is a mediator or modifier of the association between arsenic and skin lesion. In animal models, shorter telomere length has been associated with skin lesions including ulcerations with epidermal hyperplasia and hyperkeratosis (Rudolph et al., 1999; Varela et al., 2016). UV radiation-induced short TL has previously been linked to actinic keratosis in human subjects, suggesting that TL may play a role in the biology of skin lesions independent of any arsenic exposure (Ikeda et al., 2014). Furthermore, given that age is a risk factor for skin lesion (Ahsan et al., 2006), and TL is related to multiple diseases of aging (Haycock et al., 2017), we additionally hypothesize that TL may independently affect skin lesion risk. Prospective studies assessing the association between baseline TL and risk of subsequent arsenic-related skin lesions are needed to establish the temporal relationship between TL and skin lesion risk, allowing for the evaluation of TL as a biomarker for susceptibility to arsenic-related skin lesions in exposed populations.
In this study, we assessed the associations between arsenic exposure and TL and between baseline TL and subsequent skin lesions among Bangladeshi individuals with a wide range of arsenic exposure through drinking water.
2. Methods
2.1. Study participants
The Health Effects of Arsenic Longitudinal Study (HEALS) in Araihazar, Bangladesh is a prospective cohort study designed to assess the effects of exposure to arsenic through drinking water on health. Details of the participant selection, study design, and study methods have been described previously (Ahsan et al., 2005). In brief, 11,746 male and female participants were recruited between 2000 and 2002 in Araihazar, Bangladesh. The study location is in a rural area with relatively homogeneous sociocultural characteristics. The cohort has been expanded in subsequent years but the current study is conducted among this original cohort. Demographic and lifestyle data as well as blood (from which TL is measured) and urine samples were collected at baseline. In-person visits were conducted every two years following the baseline visit and each visit included a physical examination and collection of urine. All subjects in the study received basic medical care through the study clinic. Informed consent was obtained from all study participants, and the study protocol was approved by the Institutional Review Boards of the University of Chicago, Columbia University, and the ethical committee of the Bangladesh Medical Research Council.
2.2. Skin lesion status
During the baseline interview as well as three biennial follow-ups, participants were examined by trained physicians for the presence of arsenical skin lesions according to a structured protocol. The physicians, who were blinded to the participants’ arsenic exposure status, recorded the presence of melanosis (hyperpigmentation), leucomelanosis (hypopigmentation), or keratosis (thickening of the skin on palms and soles). For this study, skin lesion status was defined as the presence or absence of any type of the aforementioned skin lesions. Over the course of the three biennial follow-ups after baseline, 866 individuals developed incident skin lesions among the 10,182 skin lesion-free individuals at baseline (Argos et al., 2011).
2.3. Selection of the subcohort
A random subset of the baseline HEALS cohort was selected (n = 1469), including participants with prevalent (i.e. pre-existing) skin lesions at baseline (Ahsan et al., 2006; Argos et al., 2011). Although we have arsenic exposure measurements for a larger sample of subjects from the Bangladesh Vitamin E and Selenium Trial (BEST) (n = 1825) and the expansion of the HEALS cohort (ACE) (n = 1047), only HEALS subjects were included in the analysis in order to avoid any issues of exposure misclassification. HEALS subjects’ baseline exposure reflects historical exposure as participants were not aware of the arsenic exposure status at baseline (Chen et al., 2007), whereas many BEST and ACE participants may have been aware of their exposure status at baseline and have had the opportunity to change their exposure in response to arsenic mitigation efforts. We chose to conduct this analysis in a randomly-selected subcohort rather than in a selected group of skin-lesion cases and/or controls in order to avoid collider bias (_Cole et al., 2010). Collider bias is a form of selection bias in which a spurious association is induced between two variables when the analysis is conditioned on a common outcome (e.g. conditioning on skin lesion status, a potential common effect of both arsenic exposure and TL). TL measures were not obtained for the full cohort due to limited resources.
2.4. Nested case-control study selection
To assess associations between TL and skin lesion status, we conducted a nested case-control study of 516 individuals with incident skin lesions who were frequency matched by sex and 5-year age intervals with 516 individuals who remained skin lesion-free during the study. Subjects selected for the nested case-control study partially overlap with the random subcohort, but also include additional individuals from the parent HEALS study. We chose to perform age- and sex-matching for this analysis because age and sex are well-described correlates of TL (Sanders and Newman, 2013), which may confound the association between TL and skin lesion status. Among the subjects selected for the nested case-control study, samples for 92 subjects were excluded from the analysis due to TL assay quality control measures as detailed below, resulting in 466 cases and 464 controls. Fig. 1 shows a flowchart of the selection of participants for the nested case-control study. Characteristics of subjects excluded due to insufficient DNA and TL assay quality control are shown in Supplementary Tables 1 and 2, respectively.
Fig. 1.
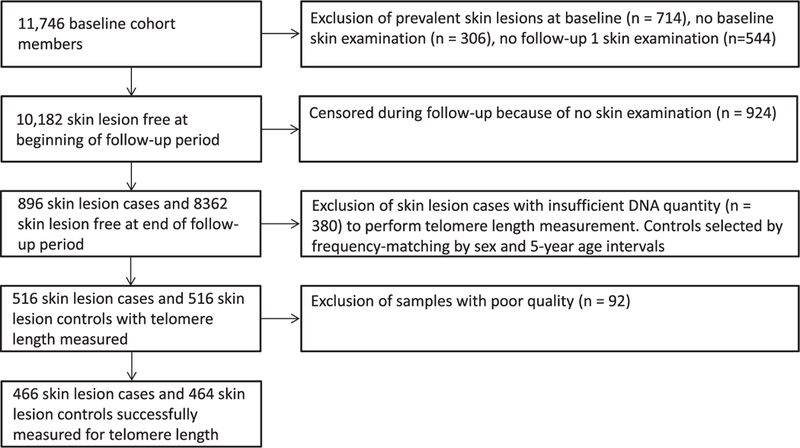
Selection of samples for nested case-control study, Health Effects of Arsenic Longitudinal Study, Bangladesh, 2000–2009.
2.5. Exposure assessment
Ascertainment of arsenic exposure through well water has previously been described (Ahsan et al., 2005; Cheng et al., 2004; Nixon et al., 1991). In brief, arsenic concentrations of water samples were measured from the wells identified by participants as their primary source of drinking water. Urinary total arsenic concentration and urinary creatinine were measured by methods previously described (Nixon et al., 1991; Heinegård and Tiderstrom, 1973). A creatinine-adjusted urinary total arsenic concentration, expressed as μg/g of creatinine, was calculated by dividing urinary total arsenic by creatinine (Nermell et al., 2008). Daily arsenic intake (μg/day) was calculated by multiplying the primary well water arsenic concentration (μg/L) by the self-reported daily water volume consumed from that well (L/day) with secondary well information also incorporated in the calculation (Argos et al., 2011). Water arsenic exposure was modeled as four levels with the first two cut points defined according to the WHO’s guideline for arsenic in drinking water (≤ 10μg/L) and Bangladesh’s national standard for arsenic in drinking water (≤50 μg/L) (corresponding approximately to the first and second quartiles). The third cut point was selected based on the upper third and fourth quartiles of water arsenic exposure. Creatinine-adjusted urinary arsenic concentration and daily arsenic intake were categorized by quartiles based on the distribution of each measure in the randomly-selected subcohort. Although arsenic exposure was assessed during follow-up visits, only the first baseline arsenic exposure was used for the association analyses in this study, representative of long-term arsenic exposure prior to arsenic mitigation efforts.
To further investigate the potential impact of arsenic exposure on TL, we assessed the association between TL and the single nucleotide polymorphism (SNP) rs9527 located in the 10q24.32 region. This variant was previously shown to be associated with percentages of arsenic metabolites monomethylarsonic acid and dimethylarsinic acid (Pierce et al., 2012, 2013) and is likely to reflect the efficiency with which arsenic is cleared from the body and excreted in urine. Furthermore, rs9527 is associated with skin lesion risk through its interaction with arsenic exposure, indicating that genetic variation for arsenic metabolism can lead to differential “effective” arsenic exposure that affects arsenical skin lesion risk. Because this SNP represents genetic variation affecting the internal dose of arsenic, an analysis of its association with TL serves to confirm findings from the analysis of the association between arsenic exposure and TL. Genotyping data was obtained based on procedures previously described (Pierce et al., 2012, 2013).
2.6. TL measurement
The method of TL measurement is similar to that of prior studies (Ehrlenbach et al., 2009; Cawthon, 2002). In summary, quantitative polymerase chain reaction (PCR) was used to compare the abundance of the telomere repeat sequence to that of a single-copy gene, RPLP0, calculated as a ratio proportional to the average relative TL of a sample (T/S ratio). Inter-plate coefficient of variation of 37 randomly selected samples repeated on different days was 11.7% for one assessment of the reproducibility of the assay and 9.8% for a second assessment of reproducibility by measuring a reference sample across 31 plates. Additional details are provided in the Supplementary Materials, Supplementary Fig. 1, and Supplementary Fig. 2.
2.7. Covariates
The following variables measured at baseline were included as covariates in all analyses: age, sex, years of formal education (0, 1–5, 6–16 years), body mass index (BMI) (< 18.5, 18.5–24.9, > 25), smoking (never, former, current), and TV and land ownership (measures of socioeconomic status). Covariates were selected a priori based on previously described correlates of arsenic exposure or TL (Sanders and Newman, 2013; Ahsan et al., 2006; Argos et al., 2010; Zhang et al., 2016). TL quartiles were created based on the distribution of TL in the random subcohort.
2.8. Statistical analyses
We assessed the association between baseline arsenic exposure and TL in the randomly-selected subcohort using linear regression (n = 1469). To remove the variation in TL due to PCR plate position (accounting for 5–9% of the variation) or plate number (accounting for 13–25% of the variation), we first obtained the position- and plate- adjusted residual TL measure for each plate design using a mixed-effects model with continuous TL as the outcome, position as a fixed effect, and plate as a random effect. The position- and plate-adjusted residual TL was then used as the outcome in minimally-adjusted linear regression models with TL as the outcome and arsenic exposure as the predictor, accounting for continuous age, sex, plate design type, and DNA extraction batch (a study design variable). Fully-adjusted models additionally included socioeconomic factors, smoking, and BMI as covariates. Analyses were repeated using water arsenic, urinary arsenic, and daily arsenic dose (modeled as quartiles) as the arsenic exposure measure. P-trend was obtained by regressing TL on an ordinal coding of arsenic exposure. We also modeled arsenic exposure as a log-transformed continuous measure, compared the TL of subjects with the top decile of arsenic exposure to those with the bottom decile exposure, and compared the TL of subjects with the top decile of arsenic exposure to all other subjects with lower arsenic exposure for all three arsenic measures.
In the analysis of the arsenic metabolism SNP and TL, the association with rs9527 (coded as 0, 1 or 2 minor alleles) was performed in a sample of 5019 individuals with both SNP and TL data. This SNP-TL analysis was performed in a combined dataset of HEALS, BEST, and ACE. Although BEST and ACE differ from HEALS with respect to historic arsenic exposure, these samples were being analyzed for genetic variation in arsenic metabolism, which is randomly assigned at birth and does not vary over time or exposure. Therefore, we were able to leverage the larger sample size of all genotyped subjects with measured TL.
Next, we calculated the odds ratios (ORs) for the risk of skin lesions by quartile TL (and repeated with continuous TL) using conditional logistic regression accounting for case-control matching based on sex- and age-defined strata (i.e., n to n matching). We again adjusted for plate position, plate number, and DNA extraction batch in minimally-adjusted conditional logistic regression models and included socio-economic factors, smoking, BMI, and baseline arsenic exposure as covariates in fully-adjusted models. The analyses of the association between arsenic and TL and between TL and skin lesion were repeated after stratifying by sex and median age of skin lesion cases (< = 45, > 45), and tests of multiplicative interaction were performed by evaluating the Wald statistic for the cross-product interaction term from the regression model. We also investigated whether TL was an effect modifier of the association between arsenic and skin lesion with tests of multiplicative interaction assessing the P value of the cross-product term of the ordinal exposure variable (arsenic quartiles) and the ordinal effect modifier (TL quartiles) in the conditional logistic regression. The relative excess risk due to interaction (RERI) measure of additive interaction was calculated for each interaction assessed (Knol et al., 2007). We chose to investigate the arsenic-TL interaction effect on skin lesion risk based on a prior study observing that risk factors of skin lesion (i.e. metabolism profile) can vary by the level of arsenic exposure (Jansen et al., 2015). Age and sex were chosen for effect modification analyses based on prior studies that observed males and older participants were more susceptible to arsenic effects on skin lesions (Chen et al., 2009), suggesting that some risk factors of skin lesion vary by age and sex. A summary of all associations and potential interaction being investigated is depicted in Supplementary Fig. 3.
All analyses were conducted using Stata (version 14, StataCorp, College Station, TX).
3. Results
3.1. Subject characteristics
The baseline characteristics, arsenic exposure, and TL measures of the age- and sex- matched skin lesion cases (n = 466) and controls (n = 464) used for the nested case-control study are shown in Table 1 along with characteristics of the random subcohort (n = 1469) used for the arsenic-TL association analysis. Among the subjects in the random subcohort, 40 had prevalent skin lesions at baseline and 74 developed skin lesions during the study follow-up. Baseline statistics of the sub-cohort subjects are summarized in Supplementary Table 3 and displayed as histograms in Supplementary Fig. 4. TL was inversely associated with age within the random subcohort (P = 1.1 × 10−14) (Supplementary Fig. 5), the case group (P = 0.002), and the control group (P = 0.02).
Table 1.
Baseline characteristics of incident skin lesions cases, matched controls, and a random sample of the HEALS cohort, Health Effects of Arsenic Longitudinal Study, Bangladesh, 2000–2009.a
| Characteristicsb | Skin lesion cases | Matched skin lesion controls | Random subcohort | |
|---|---|---|---|---|
| n | 466 | 464 | 1469 | |
| Sex | Male | 325 (69.7%) | 314 (67.7%) | 541 (36.8%) |
| Female | 141 (30.3%) | 150 (32.3%) | 928 (63.2%) | |
| Age | Years | 44.8 (9.2) | 44.8 (9.1) | 35.1 (9.1) |
| Education | 0 | 227 (48.8%) | 191 (41.2%) | 603 (41.0%) |
| 1–5 | 129 (27.7%) | 138 (29.7%) | 465 (31.7%) | |
| 6–16 | 109 (23.4%) | 135 (29.1%) | 401 (27.3%) | |
| BMI | < 18.5 | 195 (42.3%) | 191 (41.2%) | 525 (35.9%) |
| 18.5–24.9 | 246 (53.4%) | 239 (51.5%) | 822 (56.2%) | |
| > 25 | 20 (4.3%) | 34 (7.3%) | 116 (7.9%) | |
| Smoking | Never | 185 (39.7%) | 198 (42.6%) | 1014 (69.0%) |
| Former | 70 (15.0%) | 57 (12.3%) | 67 (4.6%) | |
| Current | 211 (45.3%) | 209 (45.0%) | 388 (26.4%) | |
| Own TV | Yes | 145(31.1%) | 183 (39.4%) | 505 (34.4%) |
| Own land | Yes | 264 (56.7%) | 277 (59.7%) | 758 (51.6%) |
| Water arsenic (μg/L) | 0.1–10 | 72 (15.5%) | 148 (31.9%) | 362 (24.6%) |
| 10.1–50 | 61 (13.1%) | 111 (23.9%) | 342 (23.3%) | |
| 50.1–150 | 133 (28.5%) | 132 (28.4%) | 449 (30.6%) | |
| 150.1+ | 200 (42.9%) | 73 (15.7%) | 316 (21.5%) | |
| Creatinine-adjusted urinary arsenic (μg/g) | < 105 | 82 (18.2%) | 143 (31.0%) | 366 (24.9%) |
| 105- < 194 | 82 (18.2%) | 138 (29.9%) | 358 (24.4%) | |
| 194- < 329 | 116 (25.7%) | 96 (20.8%) | 363 (24.7%) | |
| 329+ | 171 (37.9%) | 85 (18.4%) | 382 (26.0%) | |
| Daily arsenic dose (μg/day) | < 30.4 | 71 (15.3%) | 147 (31.7%) | 366 (24.9%) |
| 30.4- < 147 | 75 (16.2%) | 125 (26.9%) | 363 (24.7%) | |
| 147- < 376 | 128 (27.6%) | 92 (19.8%) | 368 (25.1%) | |
| 376+ | 190 (40.9%) | 100 (21.6%) | 372 (25.3%) | |
| T/S ratio | 0.771 (0.167) | 0.802 (0.161) | 0.804 (0.167) | |
| T/S quartiles | < 0.69 | 171 (36.7%) | 119 (25.6%) | 368 (25.1%) |
| 0.69- < 0.78 | 104 (22.3%) | 110 (23.7%) | 367 (25.0%) | |
| 0.78- < 0.90 | 110 (23.6%) | 127 (27.4%) | 367 (25.0%) | |
| 0.90+ | 81 (17.4%) | 108 (23.3%) | 367 (25.0%) | |
Categorical variables are shown in counts and percentages; continuous variables in mean (standard deviation).
bNote that some variables have missing values, with a maximum of 15 subjects missing any 1 variable
3.2. Association between arsenic and TL
Arsenic exposure was not associated with TL in the random sub-cohort for either minimally-adjusted or fully-adjusted models assessing water arsenic (beta = –0.002; 95% CI –0.022–0.019; P = 0.86; comparing the highest quartile to the lowest), urinary arsenic (beta = 0.007; 95% CI — 0.013–0.027; P = 0.49), and daily dose arsenic (beta= 0.010; 95% CI –0.010–0.029; P = 0.32) (Table 2). Estimates were also null using log-transformed continuous measures of arsenic exposure (Table 2), comparing TL in subjects with the top decile of arsenic exposure to the bottom decile, and in subjects with the top decile of arsenic exposure to all other subjects with lower exposure for all three arsenic measures (not shown). SNP rs9527, a variant previously shown to be associated with arsenic metabolism efficiency, was also not associated with TL (beta = 0.002; 95% CI – 0.007, 0.010; P= 0.70).
Table 2.
Association between baseline arsenic exposure and telomere length, Health Effects of Arsenic Longitudinal Study, Bangladesh, 2000–2009 (n = 1469).
| Arsenic exposure type | Sample sizea | Minimally-adjusted modelb | Covariate-adjusted modelc | ||||
|---|---|---|---|---|---|---|---|
| β | CI | P | β | CI | P | ||
| Water Arsenic (μg/L) | |||||||
| Continuousd | 1461 | 0.000 | − 0.003,0.004 | 0.78 | 0.000 | − 0.003,0.004 | 0.89 |
| Categorical | |||||||
| 0.1–10 | 359 | 0.000 | Ref. | Ref. | 0.000 | Ref. | Ref. |
| 10.1–50 | 339 | − 0.017 | − 0.037,0.003 | 0.10 | − 0.018 | − 0.038,0.002 | 0.081 |
| 50.1–150 | 447 | 0.006 | − 0.012,0.025 | 0.51 | 0.005 | − 0.014,0.024 | 0.60 |
| 150.1+ | 316 | − 0.001 | − 0.021,0.020 | 0.96 | − 0.002 | − 0.022,0.019 | 0.86 |
| Ptrend = 0.47 | Ptrend = 0.55 | ||||||
| Creatinine-Adjusted Urinary Arsenic (μg/g) | |||||||
| Continuousd | 1461 | 0.001 | − 0.007,0.009 | 0.77 | 0.000 | − 0.008,0.009 | 0.92 |
| Categorical | |||||||
| < 105 | 363 | 0.000 | Ref. | Ref. | 0.000 | Ref. | Ref. |
| 105- < 194 | 354 | 0.000 | − 0.020,0.019 | 0.98 | 0.000 | − 0.020,0.019 | 0.98 |
| 194- < 329 | 363 | − 0.004 | − 0.024,0.015 | 0.68 | − 0.005 | − 0.025,0.015 | 0.61 |
| 329+ | 381 | 0.008 | − 0.011,0.028 | 0.39 | 0.007 | − 0.013,0.027 | 0.49 |
| Ptrend = 0.48 | Ptrend = 0.60 | ||||||
| Daily arsenic dose (μg/day) | |||||||
| Continuousd | 1461 | 0.001 | − 0.002,0.005 | 0.51 | 0.001 | − 0.003,0.005 | 0.58 |
| Categorical | |||||||
| < 30.4 | 362 | 0.000 | Ref. | Ref. | 0.000 | Ref. | Ref. |
| 30.4- < 147 | 361 | − 0.008 | − 0.027,0.012 | 0.44 | − 0.008 | − 0.028,0.012 | 0.43 |
| 147- < 376 | 366 | 0.006 | − 0.014,0.025 | 0.57 | 0.005 | − 0.015,0.024 | 0.64 |
| 376+ | 372 | 0.011 | − 0.009,0.030 | 0.28 | 0.010 | − 0.010,0.029 | 0.32 |
| Ptrend = 0.15 | Ptrend = 0.18 | ||||||
Sample sizes of subjects without missing data for the covariate-adjusted model.
Adjusting for age, sex, and laboratory batch variables.
Additionally adjusting for BMI, education, smoking status, TV ownership, and land ownership.
Log-transformed.
3.3. Association between arsenic and skin lesion
In the nested case-control study, the odds ratios for incident skin lesions comparing the second, third, and fourth quartiles with the lowest quartile of well water arsenic exposure were OR = 1.23; 95% CI 0.75–2.03; OR = 2.16; 95% CI 1.38–3.39; and OR = 4.88; 95% CI 3.07–7.77, respectively. This is consistent with the arsenic-skin lesion association described previously in a prospective study of the entire cohort of 10,182 subjects (Argos et al., 2011).
3.4. Association between TL and skin lesion
Short TL was associated with increased skin lesion incidence in a dose-dependent manner with similar estimates for a minimally-adjusted model (OR = 2.60; 95% CI 1.61–4.19; P = 1.5 × 10 −5 comparing the shortest TL quartile to the longest), and a fully-adjusted model with water arsenic exposure included as a covariate (OR = 2.86; 95% CI 1.72–4.75; P = 2.2 × 10 −5). Similar estimates were also observed when adjusting for urinary arsenic or daily dose of arsenic, and when analyses were repeated using a continuous measure of TL (Table 3). Stratified analyses by skin lesion subtype (melanosis, leucomelanosis, or keratosis) showed similar estimates (Supplementary Table 4). Furthermore, there was suggestive evidence that subjects with shorter TL were more likely to be diagnosed at an earlier follow-up, although estimates were unstable due to small sample sizes (results not shown).
Table 3.
Odds ratios for the associations between baseline telomere length and incident skin lesions, Health Effects of Arsenic Longitudinal Study, Bangladesh, 2000–2009.
| Model | Telomere length | Case/controla | ORb | 95% CI | P |
|---|---|---|---|---|---|
| Minimally-adjustedc | Continuous | 466/464 | 1.47 | 1.23,1.75 | 2.0 × 10−4 |
| Categorical | |||||
| 4 (longest) | 80/116 | 1.00 | Ref. | Ref. | |
| 3 | 100/116 | 1.10 | 0.68,1.78 | 0.70 | |
| 2 | 122/116 | 1.59 | 0.99,2.55 | 0.057 | |
| 1 | 164/116 | 2.60 | 1.61,4.19 | 9.4 × 10−5 | |
| Ptrend = 1.5 × 10−5 | |||||
| Water arsenic-adjustedd | Continuous | 460/464 | 1.51 | 1.25,1.82 | 1.6 × 10−5 |
| Categorical | |||||
| 4 (longest) | 80/116 | 1.00 | Ref. | Ref. | |
| 3 | 97/116 | 1.33 | 0.80,2.19 | 0.27 | |
| 2 | 119/116 | 1.70 | 1.03,2.81 | 0.039 | |
| 1 | 164/116 | 2.86 | 1.72,4.75 | 5.2 × 10 −5 | |
| Ptrend = 2.2 × 10−5 | |||||
| Creatinine-adjusted urinary arsenic adjustede | Continuous | 446/462 | 1.50 | 1.25,1.81 | 1.8 × 10−5 |
| Categorical | |||||
| 4 (longest) | 77/115 | 1.00 | Ref. | Ref. | |
| 3 | 93/116 | 1.14 | 0.69,1.87 | 0.61 | |
| 2 | 117/115 | 1.70 | 1.03,2.79 | 0.038 | |
| 1 | 159/116 | 2.79 | 1.68,4.64 | 7.4 × 10−5 | |
| Ptrend = 1.2 × 10−5 | |||||
| Daily arsenic dose-adjustede | Continuous | 458/464 | 1.52 | 1.26,1.83 | 8.1 × 10−6 |
| Quartiles | |||||
| 4 (longest) | 78/116 | 1.00 | Ref. | Ref. | |
| 3 | 97/116 | 1.31 | 0.79,2.15 | 0.29 | |
| 2 | 119/116 | 1.71 | 1.04,2.82 | 0.035 | |
| 1 | 164/116 | 2.95 | 1.78,4.88 | 3.0 × 10−5 | |
| Ptrend = 2.5 × 10−5 | |||||
Reduced sample sizes reflect missing covariate data.
Odds ratio for each unit decrease in standardized telomere length.
Adjusting for age, sex, and laboratory batch variables.
Water arsenic exposure modeled as four levels with the first two cut points defined according to the WHO’s guideline for arsenic in drinking water (≤ 10 μg/L) and Bangladesh’s national standard for arsenic in drinking water (≤ 50 μg/L), and the third cut point selected based on the upper third and fourth quartiles of water arsenic exposure, and additionally adjusting for BMI, education, smoking status, TV ownership, and land ownership.
Arsenic measures coded as quartiles, and additionally adjusting for BMI, education, smoking status, TV ownership, and land ownership.
3.5. Interaction analyses
We observed suggestive evidence that TL showed a positive association with arsenic (P = 0.04) in younger subjects (≤ 45 years old) and negative association with arsenic (P = 0.04) among older subjects (> 45), although estimates were unstable due to small samples sizes (results not shown). No effect modification by sex was observed in the association between arsenic exposure and TL (results not shown). Tests for additive interaction suggest the presence of effect modification by TL on the arsenic-skin lesion association for the three arsenic exposures (Pinteraction = 0.046–0.059), but this was not observed for tests for multiplicative interaction (Pinteraction = 0.093–0.41). Odds ratios of skin lesion risk according to strata of arsenic exposure and TL quartiles compared to a common reference group of low arsenic exposure and long TL are presented in Table 4. The additive interaction tests corresponded to interaction estimates of RERI = 0.52, 95% CI: – 0.02, 1.05 for water arsenic, RERI = 0.26, 95% CI: 0.00, 0.51 for creatinine-adjusted urinary arsenic, and RERI = 0.33, 95% CI: 0.00, 0.65 for daily arsenic exposure. On the additive scale, the interpretation is that with every category increase in arsenic exposure and quartile decrease in TL, the odds ratio of skin lesion ranges from 0.26 to 0.52 more than if there were no interaction for the three arsenic exposures. A different presentation of interaction effects showing the odds ratios of skin lesion due to increasing arsenic exposure, stratified by TL quartile (with four reference groups), are also presented in Supplementary Table 5. In analyses stratified by sex, the association between TL and skin lesion risk appeared substantially larger for women than men, i.e. short TL was associated with larger increased risk in skin lesions among female subjects. However, this analysis was not well-powered, and the P value for interaction term was not significant (Pinteraction = 0.48; Supplementary Table 6). No differences by age were observed in the stratified analyses (results not shown).
Table 4:
Odds ratios and 95% confidence intervalsa for skin lesion risk among HEALS participants, according to strata of arsenic exposure and telomere length quartiles, Araihazar, Bangladesh, 2000–2009.
| Telomere length | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 4th quartile (longest) |
3rd quartile | 2nd quartile | 1st quartile (shortest) |
||||||
| Case/Control | OR (95% CI) | Case/Control | OR (95% CI) | Case/Control | OR (95% CI) | Case/Control | OR (95% CI) | ||
| Water Arsenic (μg/L) | 0.1–10 | 11/37 | 1.00 (REF) | 3/28 | 1.04 (0.38, 2.86) | 26/33 | 1.04 (0.36, 3.00) | 40/18 | 4.97 (1.76, 14.0) |
| 10.1–50 | 17/42 | 0.33 (0.07, 1.59) | 20/30 | 1.81 (0.64, 5.14) | 33/28 | 2.89 (1.00, 8.38) | 27/16 | 2.97 (1.06, 8.32) | |
| 50.1–150 | 14/44 | 2.33 (0.85, 6.39) | 16/24 | 3.08 (1.14, 8.30) | 33/32 | 3.09 (1.11, 8.56) | 56/16 | 5.20 (1.95, 13.8) | |
| 150.1 + | 27/25 | 5.88 (2.10, 16.4) | 22/29 | 5.24 (1.74, 15.8) | 40/39 | 9.46 (3.42, 26.1) | 75/23 | 10.2 (3.77, 27.4) | |
| Multiplicative Pinteractionb = 0.093 | |||||||||
| Additive Pinteractionc = 0.059 | |||||||||
| Creatinine-adjusted Urinary Arsenic (μg/g) | < 105 | 15/37 | 1.00 (REF) | 4/35 | 1.35 (0.52, 3.49) | 28/19 | 0.99 (0.37, 2.64) | 30/24 | 3.74 (1.42, 9.80) |
| 105- < 194 | 21/34 | 0.48 (0.13, 1.76) | 17/38 | 1.01 (0.38, 2.68) | 26/22 | 2.59 (0.97, 6.95) | 29/22 | 3.84 (1.53, 9.60) | |
| 194- < 329 | 16/43 | 3.76 (1.34, 10.5) | 21/28 | 2.85 (1.07, 7.58) | 31/27 | 4.13 (1.59, 10.7) | 49/17 | 2.98 (1.15, 7.74) | |
| 329 + | 29/29 | 2.9 (1.10, 7.66) | 37/37 | 3.02 (1.12, 8.17) | 31/28 | 5.89 (2.22, 15.7) | 62/22 | 9.08 (3.49, 23.6) | |
| Multiplicative Pinteractionb = 0.41 | |||||||||
| Additive Pinteractionc = 0.046 | |||||||||
| Daily arsenic dose (μg/day) | < 30.4 | 10/38 | 1.00 (REF) | 6/28 | 1.38 (0.50, 3.83) | 23/21 | 1.08 (0.35, 3.27) | 39/29 | 5.21 (1.83, 14.8) |
| 30.4- <147 | 19/40 | 0.84 (0.23, 2.99) | 22/36 | 1.82 (0.65, 5.09) | 27/16 | 3.31 (1.17, 9.36) | 29/24 | 3.84 (1.39, 10.6) | |
| 147- < 376 | 12/42 | 4.49 (1.50, 13.4) | 20/29 | 5.29 (1.77, 15.8) | 34/22 | 4.65 (1.61, 13.5) | 53/23 | 7.27 (2.68, 19.8) | |
| 376 + | 28/27 | 3.79 (1.39, 10.3) | 26/32 | 3.91 (1.35, 11.4) | 43/33 | 7.75 (2.84, 21.1) | 67/24 | 10.3 (3.69, 28.4) | |
| Multiplicative Pinteractionb= 0.32 | |||||||||
| Additive Pinteractionc = 0.047 | |||||||||
Abbreviations: CI, confidence interval, HEALS, Health Effects of Arsenic Longitudinal Study; OR, odds ratio.
Multivariable-adjusted model including age, sex, laboratory batch variables, BMI, education, smoking status, TV ownership, and land ownership.
Multiplicative Pinteraction term generated by multiplying well water arsenic exposure category (i.e. 1–4) by telomere length quartiles.
Additive P value for the relative excess risk to due interaction (RERI).
4. Discussion
In this cohort-based study of Bangladeshi adult men and women, we found no association between baseline arsenic exposure and baseline TL. However, we observed an association between short baseline TL and increased risk of subsequent arsenical skin lesions.
Our observation of a lack of association between arsenic exposure and TL was additionally supported by a lack of association between a genetic variant associated with arsenic metabolism efficiency (and therefore effective dose of arsenic) and TL. The observed lack of association between arsenic exposure and TL in this study differed from four prior epidemiologic studies, three of which suggested a positive association between arsenic exposure and TL (Gao et al., 2015; Li et al., 2012; Ameer et al., 2016), and one which suggested an inverse association (Borghini et al., 2016). However, it is important to note that all four prior studies were limited by small sample sizes (n < 400) and generally reported modest associations. A fifth study observed a positive association between high arsenic exposure and longer TL among subjects with skin lesions (Chatterjee et al., 2015), although this association is potentially susceptible to collider-stratification bias due to stratifying on skin lesion status, a potential common outcome of both arsenic exposure and TL (Cole et al., 2010). Furthermore, studies by both Chatterjee et al. and Li et al. were limited to comparing TL in high arsenic exposed subjects from one region to low arsenic exposed subjects from a different region – a design susceptible to potential biases due to confounding by other local factors. Another study by Fillman et al. was not susceptible to this potential issue as all subjects were from the same district, and notably, the positive association observed between arsenic exposure and TL was not statistically significant (Ptrend = 0.11) (Fillman et al., 2016). The assessment of arsenic exposure among prior studies were generally comparable to the current study with measurements of urinary arsenic having medians of 230 μg/L (Li et al., 2012), 80 μg/L (Ameer et al., 2016), and 196 μg/L (Ameer et al., 2016), and a creatinine adjusted urinary arsenic median of 196.0 ± 301.1 μg/g (mean ± standard deviation) (Fillman et al., 2016). The exception was one study assessing TL only in subjects with high water arsenic exposure, 153 ± 65.5 μg/L (Chatterjee et al., 2015).
Previous in vitro studies of arsenic exposure on cell cultures suggest a bimodal effect of arsenic on TL in which low doses either maintain or lengthen TL, while high doses shorten TL (Ferrario et al., 2009; Zhang et al., 2003; Liu et al., 2003). However, it is unclear if the range of arsenic concentrations tested in vitro in these studies corresponds to the same range of exposures experienced by human hematopoietic cells in vivo via arsenic-contaminated drinking water. Furthermore, in vitro studies performed over hours, days, or even weeks may not be suitable for extrapolating effects corresponding to years of chronic arsenic exposure in humans.
The observation that TL is positively associated with arsenic exposure among younger subjects (< 45 years old) and negatively associated in older subjects (≥ 45 years old) suggests that the window or length of exposure may determine the nature of the arsenic-TL association. Furthermore, the opposing directions of associations of the age strata may have masked each other, resulting in the null association observed in the subcohort analysis among all ages. Differential response to arsenic exposure by age was previously observed for skin lesion incidence, possibly due to biologic factors associated with aging, or a longer exposure time (Ahsan et al., 2006). Children and adolescents have been observed to more efficiently methylate arsenic than adults (Lindberg et al., 2008; Löveborn et al., 2016), which suggests that they may experience a lower “effective” arsenic dose compared to adults. However, the current analysis was underpowered for estimating this interaction, and additional studies of larger sample sizes are necessary to further elucidate any effect modification of age on the arsenic-TL association.
Our observation of increased skin lesion risk associated with short TL stands in contrast to the only other epidemiologic study on TL and arsenical skin lesions (Chatterjee et al., 2015), which found increased skin lesion risk for individuals with longer TL. However, unlike our prospective study design, these findings were based on a cross-sectional study design and potentially susceptible to issues of reverse causality.
There is no prior literature regarding the effect modification we observed, i.e. a stronger association between arsenic exposure and skin lesion risk in subjects with shorter TL. However, previous studies have described effect modification on the additive scale of arsenic-induced skin lesions by smoking and fertilizer use, suggesting that some risk factors of skin lesions interact with arsenic exposure to further increase skin lesion risk (Chen et al., 2006; Melkonian et al., 2011). Further-more, a previous in vitro study on apoptosis in human cell-lines showed that treatment with a telomerase inhibitor (thereby disrupting TL maintenance) enhances arsenic-induced apoptosis. Although the exact biological mechanism underlying this observation remains unclear, this study suggests a potential synergism between effects of arsenic exposure and an altered telomere state on the cell cycle. Additional investigations to replicate and elucidate this observed differential arsenic susceptibility are necessary.
Generalizability of our findings to other populations likely depend on the arsenic exposure levels and the distribution of TL in those populations. Given the interaction effect between arsenic and TL on skin lesion risk observed in this study, different magnitudes of association between TL and skin lesion risk may be observed in other populations exposed to higher or lower levels of arsenic. Differences in average leukocyte TL between populations (e.g. shorter TL in individuals of European ancestry compared to individuals of African ancestry (Sanders and Newman, 2013)) may also contribute to differences from the described associations in other populations, although no study to date has assessed leukocyte TL of Bangladeshi individuals relative to other race/ethnicities.
This study has several key strengths. For estimating the arsenic-TL association, we used a randomly-selected subset from the HEALS population-based cohort, which is representative of the local population, thus reducing the risk of selection bias. Both the arsenic-TL and the TL-skin lesion analyses had much larger sample sizes than prior studies, providing superior statistical power. Our analyses involved comprehensive adjustment of potential confounders as covariates. Subjects in this study have a wide range of arsenic exposure levels with multiple types of arsenic exposure measurements collected. Our study of TL and skin lesion risk is prospective in design with controls selected from the same cohort as the cases, and TL measured prior to skin lesion ascertainment, thus reducing potential issues of reverse causality and selection bias.
Prior research indicates high correlation between TL measured in leukocyte and skin (r = 0.83) (Daniali et al., 2013). Thus, TL measures obtained from peripheral blood cells are likely to be proxies for TL in skin, suggesting a biological mechanism underlying the association we observe between TL and skin lesion risk. However, not all tissues in the body accumulate arsenic equally, with studies in both human and mice models showing higher accumulation of arsenic in skin than in blood (due in part to arsenic’s affinity to keratin in skin) (Hughes et al., 2003; Hughes et al., 2009; Saha et al., 1999). Thus, it is possible that chronic arsenic exposure affects TL in skin cells (or other tissues), but not the blood-based TL measures analyzed in this study. Future analyses examining arsenic levels and TL from biopsied skin samples may be necessary to clarify this issue.
Due to limitations in resources and DNA availability, our analyses were restricted to a random subset of 1469 rather than the full HEALS cohort and to 516 cases in the nest case-control study rather than all 896 skin lesion incident cases. Arsenic exposure levels were somewhat higher for the skin lesion cases that were measured for TL compared to skin lesion cases that were excluded (Supplementary Table 1); such variability could potentially bias the estimates of the association between TL and skin lesion, although we believe this is unlikely due to the lack of association observed between arsenic and TL, i.e. arsenic is unlikely to be a confounder. Another limitation of this study is the use of qPCR to measure TL, a method which exhibits greater variability in measurements than the “gold standard” Southern blot method (Aviv et al., 2011). Such non-differential measurement error may result in association estimates biased towards the null. Another potential limitation of the arsenic-TL association analysis is that arsenic measures may not represent cumulative lifetime exposure. However, participants selected into HEALS were required to be residents of the study area for at least 5 years and primarily drinking water from one of the study wells for at least 3 years (Ahsan et al., 2005), so the baseline exposure estimates are likely to represent stable long-term arsenic exposure through drinking water. Prior studies have shown that well-switching is not frequent when arsenic-status of wells are not known (Madajewicz et al., 2007; Schoenfeld, 2005). For this reason, well-switching before baseline is not a likely confounder as HEALS participants were not aware of the arsenic statuses of wells, which were measured and made known just after baseline. Nevertheless, future studies of the impact of different exposure windows on the association between arsenic and TL are worthwhile, particularly in children and/or adolescents who may be more susceptible to chronic arsenic exposure. Furthermore, longitudinal studies with repeated arsenic and TL measures would allow for more rigorous estimation of the association between lifetime arsenic exposure and TL, as well as clarify when best to measure TL as a predictive biomarker for subsequent health outcomes.
5. Conclusions
Our findings suggest a lack of association between arsenic exposure and blood TL in adults. However, our observation that short TL is associated with risk for subsequent arsenical skin lesions has potential implications for elucidating the biological mechanisms linking arsenic exposure to skin lesions, predicting individual susceptibility to arsenic-induced skin lesions, as well as future investigations of other arsenic-related health conditions.
Supplementary Material
Acknowledgements
This work was supported by the National Institutes of Health (T32AG000243 and P30AG012857 training grant support to C.Z., P42 ES 10349 to J.G., R01 CA 107431 to H.A., and R01 ES020506 and U01 HG007601 to B.L.P.).
Footnotes
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.envres.2018.03.005.
References
- Ahmed S, Mahabbat-e Khoda S, Rekha RS, Gardner RM, Ameer SS, Moore S, et al. 2011. Arsenic-associated oxidative stress, inflammation, and immune disruption in human placenta and cord blood. Environ et al. Health Perspect. 119, 258–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahsan H, Chen Y, Parvez F, Argos M, Hussain AI, Momotaj H, et al. , 2005. Health effects of arsenic longitudinal study (HEALS): description of a multidisciplinary epidemiologic investigation. J. Expo. Sci. Environ. Epidemiol. 16, 191–205. [DOI] [PubMed] [Google Scholar]
- Ahsan H, Chen Y, Parvez F, Zablotska L, Argos M, Hussain I, et al. , 2006. Arsenic exposure from drinking water and risk of premalignant skin lesions in Bangladesh: baseline results from the health effects of arsenic longitudinal study. Am. J. Epidemiol. 163, 1138–1148. [DOI] [PubMed] [Google Scholar]
- Ameer SS, Xu Y, Engstrom K, Li H, Tallving P, Nermell B, et al. , 2016. Exposure to inorganic arsenic is associated with increased mitochondrial DNA copy number and longer telomere length in peripheral blood. Front. Cell Dev. Biol. 4, 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Argos M, Kalra T, Rathouz PJ, Chen Y, Pierce B, Parvez F, 2010. Arsenic exposure from drinking water, and all-cause and chronic-disease mortalities in Bangladesh (HEALS): a prospective cohort study. Lancet 376, 252–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Argos M, Kalra T, Pierce BL, Chen Y, Parvez F, Islam T, et al. , 2011. A Prospective study of arsenic exposure from drinking water and incidence of skin lesions in Bangladesh. Am. J. Epidemiol. 174, 185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arsenic in Drinking Water: 2001 Update, 2001. National Academies Press (US), Washington (DC: ). [PubMed] [Google Scholar]
- Aviv A, Hunt SC, Lin J, Cao X, Kimura M, Blackburn E, 2011. Impartial comparative analysis of measurement of leukocyte telomere length/DNA content by Southern blots and qPCR. Nucleic Acids Res. 39 (e134–e134). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borghini A, Faita F, Mercuri A, Minichilli F, Bustaffa E, Bianchi F, et al. , 2016. Arsenic exposure, genetic susceptibility and leukocyte telomere length in an Italian young adult population. Mutagenesis 31, 539–546. [DOI] [PubMed] [Google Scholar]
- Cawthon RM, 2002. Telomere measurement by quantitative PCR. Nucleic Acids Res. 30 (e47–e47). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawthon RM, Smith KR, O’Brien E, Sivatchenko A, Kerber RA, 2003. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet 361, 393–395. [DOI] [PubMed] [Google Scholar]
- Celik I, Gallicchio L, Boyd K, Lam TK, Matanoski G, Tao X, et al. , 2008. Arsenic in drinking water and lung cancer: a systematic review. Environ. Res. 108, 48–55. [DOI] [PubMed] [Google Scholar]
- Chatterjee D, Bhattacharjee P, Sau TJ, Das JK, Sarma N, Bandyopadhyay AK, et al. , 2015. Arsenic exposure through drinking water leads to senescence and alteration of telomere length in humans: a case-control study in West Bengal, India. Mol. Carcinog. 54, 800–809. [DOI] [PubMed] [Google Scholar]
- Chen Y, Graziano JH, Parvez F, Hussain I, Momotaj H, van Geen A, et al. , 2006. Modification of risk of arsenic-induced skin lesions by sunlight exposure, smoking, and occupational exposures in Bangladesh. Epidemiol. Camb. Mass. 17, 459–467. [DOI] [PubMed] [Google Scholar]
- Chen Y, van Geen A, Graziano JH, Pfaff A, Madajewicz M, Parvez F, et al. , 2007. Reduction in urinary arsenic levels in response to arsenic mitigation efforts in Araihazar, Bangladesh. Environ. Health Perspect. 115, 917–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Parvez F, Gamble M, Islam T, Ahmed A, Argos M, et al. , 2009. Arsenic exposure at low-to-moderate levels and skin lesions, arsenic metabolism, neurological functions, and biomarkers for respiratory and cardiovascular diseases: review of Recent findings from the health effects of arsenic longitudinal study (HEALS) in Bangladesh. Toxicol. Appl. Pharmacol. 239, 184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Z, Zheng Y, Mortlock R, van Geen A, 2004. Rapid multi-element analysis of groundwater by high-resolution inductively coupled plasma mass spectrometry. Anal. Bioanal. Chem. 379, 512–518. [DOI] [PubMed] [Google Scholar]
- Cole SR, Platt RW, Schisterman EF, Chu H, Westreich D, Richardson D, et al. , 2010. Illustrating bias due to conditioning on a collider. Int. J. Epidemiol. 39, 417–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuzick J, Evans S, Gillman M, Price Evans DA, 1982. Medicinal arsenic and internal malignancies. Br. J. Cancer 45, 904–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuzick J, Sasieni P, Evans S, 1992. Ingested arsenic, keratoses, and bladder cancer. Am. J. Epidemiol. 136, 417–421. [DOI] [PubMed] [Google Scholar]
- Daniali L, Benetos A, Susser E, Kark JD, Labat C, Kimura M, et al. , 2013. Telomeres shorten at equivalent rates in somatic tissues of adults. Nat. Commun. 4, 1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlenbach S, Willeit P, Kiechl S, Willeit J, Reindl M, Schanda K, et al. , 2009. Influences on the reduction of relative telomere length over 10 years in the population-based Bruneck Study: introduction of a well-controlled high-throughput assay. Int. J. Epidemiol. 38, 1725–1734. [DOI] [PubMed] [Google Scholar]
- Ferrario D, Collotta A, Carfi M, Bowe G, Vahter M, Hartung T, et al. , 2009. Arsenic induces telomerase expression and maintains telomere length in human cord blood cells. Toxicology 260, 132–141. [DOI] [PubMed] [Google Scholar]
- Fillman T, Shimizu-Furusawa H, Ng CFS, Parajuli RP, Watanabe C, 2016. Association of cadmium and arsenic exposure with salivary telomere length in adolescents in Terai, Nepal. Environ. Res. 149, 8–14. [DOI] [PubMed] [Google Scholar]
- Flanagan SV, Johnston RB, Zhenga Yan, 2012. Arsenic in tube well water in Bangladesh: health and economic impacts and implications for arsenic mitigation. Bull. World Health Organ. 90, 839–846 (8p). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J, Roy S, Tong L, Argos M, Jasmine F, Rahaman R, et al. , 2015. Arsenic exposure, telomere length, and expression of telomere-related genes among Bangladeshi individuals. Environ. Res. 136, 462–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haycock PC, Burgess S, Nounu A, Zheng J, Okoli GN, Bowden J, et al. , 2017. Association between telomere length and risk of cancer and non-neoplastic diseases: a mendelian randomization study. JAMA Oncol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinegård D, Tiderstrom G, 1973. Determination of serum creatinine by a direct colorimetric method. Clin. Chim. Acta 43, 305–310. [DOI] [PubMed] [Google Scholar]
- Hopenhayn-Rich C, Biggs ML, Smith AH, 1998. Lung and kidney cancer mortality associated with arsenic in drinking water in Córdoba, Argentina. Int. J. Epidemiol. 27, 561–569. [DOI] [PubMed] [Google Scholar]
- Hsu L-I, Chen G-S, Lee C-H, Yang T-Y, Chen Y-H, Wang Y-H, et al. , 2013. Use of arsenic-induced palmoplantar hyperkeratosis and skin cancers to predict risk of subsequent internal malignancy. Am. J. Epidemiol. [Internet] (Available from). <http://aje.oxfordjournals.org/content/early/2013/01/07/aje.kws369.abstract>. [DOI] [PubMed] [Google Scholar]
- Hughes MF, Kenyon EM, Edwards BC, Mitchell CT, Razo LMD, Thomas DJ, 2003. Accumulation and metabolism of arsenic in mice after repeated oral administration of arsenate. Toxicol. Appl. Pharmacol. 191, 202–210. [DOI] [PubMed] [Google Scholar]
- Hughes MF, Thomas DJ, Kenyon EM, 2009. Toxicology and Epidemiology of Arsenic and its Compounds, in Arsenic: Environmental Chemistry, Health Threats and Waste Treatment (ed Henke K). John Wiley & Sons, Ltd, Chichester, UK, pp. 237–275. 10.1002/9780470741122.ch4. [DOI] [Google Scholar]
- Ikeda H, Aida J, Hatamochi A, Hamasaki Y, Izumiyama-Shimomura N, Nakamura K, et al. , 2014. Quantitative fluorescence in situ hybridization measurement of telomere length in skin with/without sun exposure or actinic keratosis. Hum. Pathol. 45, 473–480. [DOI] [PubMed] [Google Scholar]
- Jansen RJ, Argos M, Tong L, Li J, Rakibuz-Zaman M, Islam MT, et al. , 2015. Determinants and consequences of arsenic metabolism efficiency among 4,794 individuals: demographics, lifestyle, genetics, and toxicity. Cancer Epidemiol. Biomark. Prev. [Internet] (Available from). <http://cebp.aacrjournals.org/content/early/2015/12/16/1055-9965.EPI-15-0718.abstract>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenny NS, 2012. Inflammation in aging: cause, effect, or both? Discov. Med. 13, 451–460. [PubMed] [Google Scholar]
- Kitchin KT, 2001. Recent advances in arsenic carcinogenesis: modes of action, animal model systems, and methylated arsenic metabolites. Toxicol. Appl. Pharmacol. 172, 249–261. [DOI] [PubMed] [Google Scholar]
- Knol MJ, van der Tweel I, Grobbee DE, Numans ME, Geerlings MI, 2007. Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int. J. Epidemiol. 36, 1111–1118. [DOI] [PubMed] [Google Scholar]
- Li H, Engstrom K, Vahter M, Broberg K, 2012. Arsenic exposure through drinking water is associated with longer telomeres in peripheral blood. Chem. Res. Toxicol. 25, 2333–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindberg A-L, Ekström E-C, Nermell B, Rahman M, Lönnerdal B, Persson L-Å, et al. , 2008. Gender and age differences in the metabolism of inorganic arsenic in a highly exposed population in Bangladesh. Environ. Res. 106, 110–120. [DOI] [PubMed] [Google Scholar]
- Liu J, Waalkes MP, 2008. Liver is a target of arsenic carcinogenesis. Toxicol. Sci. 105, 24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Trimarchi JR, Navarro P, Blasco MA, Keefe DL, 2003. Oxidative stress contributes to arsenic-induced telomere attrition, chromosome instability, and apoptosis. J. Biol. Chem. 278, 31998–32004. [DOI] [PubMed] [Google Scholar]
- Löveborn HS, Kippler M, Lu Y, Ahmed S, Kuehnelt D, Raqib R, et al. , 2016. Arsenic metabolism in children differs from that in adults. Toxicol. Sci. 152, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madajewicz M, Pfaff A, van Geen A, Graziano J, Hussein I, Momotaj H, et al. , 2007. Can information alone change behavior? Response to arsenic contamination of groundwater in Bangladesh. J. Dev. Econ. 84, 731–754. [Google Scholar]
- Martin-Ruiz C, Dickinson HO, Keys B, Rowan E, Kenny RA, Von Zglinicki T, 2006. Telomere length predicts poststroke mortality, dementia, and cognitive decline. Ann. Neurol. 60, 174–180. [DOI] [PubMed] [Google Scholar]
- Melkonian S, Argos M, Pierce BL, Chen Y, Islam T, Ahmed A, et al. , 2011. A prospective study of the synergistic effects of arsenic exposure and smoking, sun exposure, fertilizer use, and pesticide use on risk of premalignant skin lesions in Bangladeshi men. Am. J. Epidemiol. 173, 183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mink PJ, Alexander DD, Barraj LM, Kelsh MA, Tsuji JS, 2008. Low-level arsenic exposure in drinking water and bladder cancer: a review and meta-analysis. Regul. Toxicol. Pharmacol. 52, 299–310. [DOI] [PubMed] [Google Scholar]
- Mo J, Xia Y, Ning Z, Wade TJ, Mumford JL, 2009. Elevated human telomerase reverse transcriptase gene expression in blood cells associated with chronic arsenic exposure in Inner Mongolia, China. Environ. Health Perspect. 117, 354–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nermell B, Lindberg A-L, Rahman M, Berglund M, Persson LÁ, El Arifeen S, et al. , 2008. Urinary arsenic concentration adjustment factors and malnutrition. Environ. Res. 106, 212–218. [DOI] [PubMed] [Google Scholar]
- Nixon DE, Mussmann GV, Eckdahl SJ, Moyer TP, 1991. Total arsenic in urine: palladium-persulfate vs nickel as a matrix modifier for graphite furnace atomic absorption spectrophotometry. Clin. Chem. 37, 1575–1579. [PubMed] [Google Scholar]
- O’Donovan A, Pantell MS, Puterman E, Dhabhar FS, Blackburn EH, Yaffe K, et al. , 2011. Cumulative inflammatory load is associated with short leukocyte telomere length in the health, aging and body composition study. PLoS One 6, e19687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce BL, Kibriya MG, Tong L, Jasmine F, Argos M, Roy S, et al. , 2012. Genomewide association study identifies chromosome 10q24.32 variants associated with arsenic metabolism and toxicity phenotypes in Bangladesh. PLoS Genet. 8, e1002522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce BL, Tong L, Argos M, Gao J, Jasmine F, Roy S, et al. , 2013. Arsenic metabolism efficiency has a causal role in arsenic toxicity: mendelian randomization and gene-environment interaction. Int. J. Epidemiol. 42, 1862–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KL, Chang S, Lee H-W, Blasco M, Gottlieb GJ, Greider C, et al. , 1999. Longevity, stress response, and cancer in aging telomerase-deficient mice. Cell 96, 701–712. [DOI] [PubMed] [Google Scholar]
- Saha JC, Dikshit AK, Bandyopadhyay M, Saha KC, 1999. A review of arsenic poisoning and its effects on human health. Crit. Rev. Environ. Sci. Technol. 29, 281–313. [Google Scholar]
- Sanders JL, Newman AB, 2013. Telomere length in epidemiology: a biomarker of aging, age-related disease, both, or neither? Epidemiol. Rev. 35, 112–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenfeld A, 2005. Area, village, and household response to arsenic testing and labeling of tubewells in Araihazar. Bangladesh. [Google Scholar]
- Serrano AL, Andrés V, 2004. Telomeres and cardiovascular disease: does size matter? Circ. Res. 94, 575–584. [DOI] [PubMed] [Google Scholar]
- Shawi M, Autexier C, 2008. Telomerase, senescence and ageing. Mech. Ageing Dev. 129, 3–10. [DOI] [PubMed] [Google Scholar]
- Sohel N, Persson LÅ, Rahman M, Streatfield PK, Yunus M, Ekstrom E-C, et al. ,2009. Arsenic in drinking water and adult mortality: a population-based cohort study in rural Bangladesh. Epidemiology 20, 824–830. [DOI] [PubMed] [Google Scholar]
- States JC, Srivastava S, Chen Y, Barchowsky A, 2009. Arsenic and cardiovascular disease. Toxicol. Sci. 107, 312–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahidnia A, van der Voet GB, de Wolff FA, 2007. Arsenic neurotoxicity — a review. Hum. Exp. Toxicol. 26, 823–832. [DOI] [PubMed] [Google Scholar]
- Varela E, Muñoz-Lorente MA, Tejera AM, Ortega S, Blasco MA, 2016. Generation of mice with longer and better preserved telomeres in the absence of genetic manipulations. Nat. Commun. 7, 11739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Zglinicki T, 2002. Oxidative stress shortens telomeres. Trends Biochem. Sci. 27, 339–344. [DOI] [PubMed] [Google Scholar]
- Willeit P, Willeit J, Mayr A, Weger S, Oberhollenzer F, Brandstatter A, et al. , 2010. Telomere length and risk of incident cancer and cancer mortality. J. Am. Med. Assoc. 304, 69–75. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2001. United Nations Synthesis Report on Arsenic in Drinking Water. WHO, Geneva. [Google Scholar]
- Yu H-S, Liao W-T, Chai C-Y, 2006. Arsenic carcinogenesis in the skin. J. Biomed. Sci. 13, 657–666. [DOI] [PubMed] [Google Scholar]
- Zhang C, Lauderdale DS, Pierce BL, 2016. Sex-specific and time-varying associations between cigarette smoking and telomere length among older adults. Am. J. Epidemiol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T-C, Schmitt MT, Mumford JL, 2003. Effects of arsenic on telomerase and telomeres in relation to cell proliferation and apoptosis in human keratinocytes and leukemia cells in vitro. Carcinogenesis 24, 1811–1817. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


