Abstract
Objectives
This study aims to examine the abuse and addiction of gabapentinoids in penal institutions.
Patients and methods
Between September 2014 and November 2014, a total of 1,639 participants were administered an electronic questionnaire investigating the drug use and addiction. The questionnaire was requested to be asked and filled by the officers in charge for all voluntary convicts and prisoners in all penitentiaries throughout Turkey.
Results
The rate of answering the questions varied between 20.5% and 100%. It was found that 2% of the participants used pregabalin and gabapentin simultaneously, while 25.2% of them used multiple drugs. The usage rate of pregabalin and gabapentin was higher in some penitentiaries, compared to the normal population. There was a significant positive correlation between the use of gabapentinoids and multiple drugs and alcohol and drug addiction, various withdrawal symptoms, the number of going to the infirmary, and the number of referral to the hospital (p<0.05).
Conclusion
Although gabapentinoids seem to be used in the treatment of addiction, and are proved effective treatment agents. With a definite diagnosis, appropriate follow-up, and timely completion of the treatment, it is necessary to strictly control their use due to the probability of abuse and addiction.
Keywords: Abuse, addiction, gabapentin, gabapentinoid, pregabalin
Introduction
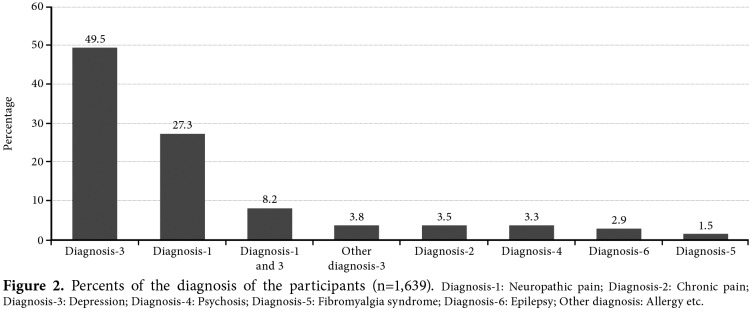
Gabapentinoids (gabapentin and pregabalin) are antiepileptic drugs used in the treatment of primary focal and secondary generalized epilepsy, the former of which makes N-type calcium channel modulation and is eliminated from the body 100% by kidneys and the latter of which acts by binding to α2δ subunit of the voltage-gated calcium channel and is eliminated from the body 95% by kidneys. Pregabalin has a six times stronger binding affinity to this subunit of the calcium channels than gabapentin.[1-5] As a result of calcium release from the nerve endings, it reduces the release of various neurotransmitters such as glutamate, norepinephrine, and substance P.[6-8] Pregabalin does not act through the gamma-aminobutyric acid (GABA) receptors, and does not change the GABA uptake and degradation.[9,10] Neither drug binds to the plasma proteins, and interacts with liver enzymes and other drugs.[11] The well-known side effects of gabapentin are somnolence, dizziness, ataxia, fatigue, nystagmus, weight gain, and behavior disorders in children and side effects of pregabalin are mild temporary elevations in the liver enzymes, somnolence, fatigue, dizziness, and weight gain.[1] Pregabalin is primarily used in the treatment of epilepsy and neuropathic pain, and also in the treatment of addiction of alcohol and benzodiazepine.[12] Similarly, based on the central mechanisms in the etiopathogenesis of fibromyalgia syndrome, antiepileptics are considered to be tested in the treatment. Pregabalin is the first agent to be deemed suitable for the treatment of fibromyalgia syndrome by the United States Food and Drug Administration.[13] In regard to the use of gabapentin in fibromyalgia, a randomized placebo-controlled study is available in the literature.[14] According to the data obtained by examining the commercial records (provided by the drug companies in Turkey), the use and institutional costs of these drugs have been gradually increasing worldwide (Figure 1). While the quantity of gabapentin sold in Turkey in 2011 was 3,725,927 boxes, this number increased up to 4,621,100 boxes in 2014. The quantity of pregabalin sold was 896,744 boxes in 2011, while this number was 2,997,515 boxes in 2014. The money spent for pregabalin was 13,130,220 US Dollars in 2011, while it was 23,433,991 US Dollars in 2014.
Figure 1. The population ratio of the sold pillbox numbers and institutional costs of pregabalin and gabapentin in US Dollars in the markets of USA, Europe and Turkey in 2011, 2012, 2013 and 2014.
Gabapentin has been shown to be associated with euphoria as a side effect in 1 to 10% of patients.[15] Also, there are case reports of probable addiction of gabapentinoids.[16,17] Although they are considered as effective drugs, they are also regarded as the drugs potentially developing clinical abuse.[15-18] In the present study, we aimed to examine the abuse and addiction of gabapentinoids which have been becoming more widespread around the world, in penal institutions where the probability of addiction is estimated to be higher, in terms of improving the health and training of the convicts and prisoners in the penal institutions, and developing the drug policies of the institutions.[19]
Patients and Methods
Upon receiving the official and ethical approval of Turkish Republic Ministry of Justice General Directorate of Penitentiary and Detention Institutions, dated 25/08/2014 and numbered 57292265-204.06.03-1445/134224, a questionnaire investigating the drug use and addiction was prepared in the electronic environment, and it was requested to be asked and filled by officers in charge for all the convicts and prisoners who accepted to participate in the study and signed the written consent in all penitentiaries throughout Turkey. The study was conducted in accordance with the principles of the Declaration of Helsinki. By conforming to the privacy, it was ensured that the questionnaires were collected in a pool in electronic environment which can only be reached by the researchers. The data obtained was subjected to statistical analysis by an expert statistician. The results of this project were allowed to be published with the approval of Turkish Republic Ministry of Justice, dated 24/12/2015 and numbered 57292265- 204.06.03-E.2013/188853. Statistical analysis Statistical analysis was performed using the PASW version 17.0 statistical software (SPSS Inc., Chicago, IL, USA). Descriptive statistics were expressed in median (min-max) values and number and percentage. The chi-square and Cramer’s V tests were used to assess the correlations. A p value of <0.05 was considered statistically significant.
Results
A total of 1,639 participants attended to the questionnaire study. The response rate of the participants differed for each question, as it was based on volunteering (range, 20.5 to 100%; Table 1). According to the numbers of the individuals using pregabalin and gabapentin in each penal institution, it was found that the total number of the individuals using pregabalin and gabapentin was above the number of the participants in some institutions (e.g., Adana/Kozan and Nigde E type), which was due to the fact that some of the participants used pregabalin and gabapentin simultaneously (Table 2).
Table 1. Number and percent of the participants to each question (n=1,639).
| Question | Number of the participants | Percent of the participants (%) |
| Usage of pregabalin? | 1567 | 95,5 |
| Drug report for pregabalin? | 352 | 21,5 |
| Usage period for pregabalin (month) | 336 | 20,5 |
| Frequency of pregabalin usage | 356 | 21,7 |
| Dose of pregabalin | 356 | 21,7 |
| Pregabalin started before imprisonment? | 366 | 22,3 |
| Usage of gabapentin? | 1559 | 95,1 |
| Drug report for gabapentin? | 414 | 25,2 |
| Usage period for gabapentin (months) | 371 | 22,6 |
| Frequency of gabapentin usage | 422 | 25,7 |
| Dose of gabapentin | 423 | 25,8 |
| Gabapentin started before imprisonment? | 428 | 26,1 |
| Usage of antidepressant, antipsychotic or other antiepileptic drugs? | 1621 | 98,9 |
| Drug report for other drugs? | 1078 | 65,8 |
| Usage period for other drugs (months) | 1003 | 61,2 |
| Frequency of usage of other drugs | 1071 | 65,3 |
| Doses of other drugs | 1061 | 64,7 |
| Other drugs started before imprisonment? | 1092 | 66,6 |
| Diagnosis | 1639 | 100 |
| Name of the drugs | 1639 | 100 |
| Multiple drug usage | 1634 | 99,6 |
| In which step of health institution the drugs were started? | 1498 | 91,3 |
| Alcohol addiction | 1411 | 86 |
| Dope addiction | 1446 | 88,2 |
| Going to the infirmary (last 1 year) | 1233 | 75,2 |
| Going to the infirmary (last 6 months) | 1639 | 100 |
| Going to the infirmary (last 3 months) | 1080 | 65,9 |
| Referring to the hospital (last 1 year) | 1171 | 71,4 |
| Referring to the hospital (last 6 months) | 950 | 57,9 |
| Referring to the hospital (last 3 months) | 946 | 57,7 |
| Duration of imprisonment (intervals of months or years) | 1377 | 84 |
| Tend to engage in violence against others? | 1559 | 95,1 |
| Tend to engage in violence against the self? | 1555 | 94,8 |
| Withdrawal symptoms occurring when the drug is not used | ||
| Sweating | 985 | 60,1 |
| Shivering | 1021 | 62,3 |
| Having fever | 932 | 56,8 |
| Stomachache | 894 | 54,5 |
| Nausea | 900 | 54,9 |
| Vomiting | 880 | 53,7 |
| Palpitation | 960 | 58,5 |
| Hallucination | 954 | 58,2 |
| Headache | 1063 | 64,8 |
| Dizziness | 952 | 58 |
| Nervousness | 1294 | 78,9 |
| Sleeplessness | 1318 | 80,4 |
| Nightmare | 947 | 57,7 |
| Epileptic seizure | 883 | 53,8 |
| Xerostomia | 958 | 58,4 |
| Restlessness | 1368 | 83,4 |
Table 2. Penal institutions, number of participants and number of participants using pregabalin or gabapentin (n=1,639).
| Institution | NP | P | G | Institution | NP | P | G | Institution | NP | P | G |
| Null | 6 | 1 | 0 | Diyarbakır | 2 | 1 | 0 | Kocaeli | 30 | 2 | 2 |
| F type | |||||||||||
| Adana | |||||||||||
| F type | 6 | 0 | 2 | Erzurum | 18 | 3 | 2 | Konya | 13 | 6 | 3 |
| Adana | 9 | 0 | 1 | Erzurum | 48 | 4 | 7 | Konya | 5 | 1 | 2 |
| Karataş | Oltu | Beyşehir | |||||||||
| Adana | 5 | 4 | 4 | Eskişehir | 15 | 4 | 2 | Konya | 3 | 0 | 1 |
| Kozan | Open | Seydişehir | |||||||||
| Adıyaman | 2 | 0 | 2 | Gaziantep | 5 | 0 | 1 | Manisa | 45 | 5 | 12 |
| Afyon | 29 | 2 | 18 | Giresun | 33 | 6 | 27 | Manisa | 4 | 0 | 1 |
| Akhisar | |||||||||||
| Afyon | 7 | 0 | 5 | Hatay | 1 | 0 | 0 | Manisa | 1 | 0 | 0 |
| Sandıklı | Closed | Alaşehir | |||||||||
| Ağrı | 14 | 0 | 3 | Isparta | 3 | 0 | 0 | Mersin | 149 | 2 | 6 |
| Yalvaç | |||||||||||
| Ankara | 120 | 46 | 9 | İstanbul | 37 | 8 | 10 | Muğla | 60 | 39 | 6 |
| Ankara | 5 | 2 | 2 | İstanbul | 14 | 1 | 2 | Nevşehir | 7 | 0 | 7 |
| Ayas | L type | ||||||||||
| Ankara | 11 | 7 | 2 | İstanbul | 19 | 6 | 6 | Niğde | 10 | 2 | 4 |
| Kızılcahamam | Silivri | Open | |||||||||
| Antalya | 26 | 3 | 2 | İzmir | 24 | 3 | 3 | Niğde | 11 | 1 | 11 |
| E type | |||||||||||
| Ardahan | 4 | 0 | 0 | İzmir | 4 | 1 | 2 | Osmaniye | 6 | 0 | 2 |
| Aliağa | |||||||||||
| Aydın | 5 | 0 | 2 | İzmir | 50 | 18 | 4 | Rize | 13 | 1 | 2 |
| Bergama | |||||||||||
| Aydın | 1 | 0 | 0 | İzmir | 11 | 0 | 6 | Samsun | 58 | 11 | 8 |
| Söke | Ödemiş | ||||||||||
| Balıkesir | 22 | 8 | 8 | İzmir | 7 | 7 | 0 | Samsun | 47 | 12 | 12 |
| T type | Bafra | ||||||||||
| Balıkesir | 12 | 0 | 5 | Kahramaraş | 44 | 3 | 24 | Samsun | 6 | 0 | 0 |
| Bandırma | Çarşamba | ||||||||||
| Balıkesir | 1 | 1 | 0 | Karabük | 15 | 6 | 1 | Sinop | 21 | 3 | 3 |
| L type | |||||||||||
| Batman | 11 | 0 | 4 | Karaman | 5 | 0 | 5 | Sinop | 4 | 1 | 2 |
| Boyabat | |||||||||||
| Bitlis | 25 | 2 | 9 | Karaman | 6 | 0 | 6 | Şanlıurfa | 15 | 6 | 1 |
| Ermenek | |||||||||||
| Bolu | 53 | 15 | 8 | Kastamonu | 18 | 6 | 15 | Şırnak | 61 | 5 | 13 |
| Bolu | 27 | 9 | 6 | Kastamonu | 4 | 0 | 3 | Tekirdağ | 8 | 0 | 1 |
| F type | Daday | ||||||||||
| Burdur | 23 | 6 | 12 | Kayseri | 4 | 0 | 2 | Tekirdağ | 1 | 0 | 0 |
| Open | |||||||||||
| Bursa | 4 | 1 | 0 | Kırıkkale | 46 | 9 | 16 | Tekirdağ | 16 | 0 | 8 |
| F type | |||||||||||
| Bursa | 11 | 3 | 1 | Kırıkkale | 6 | 4 | 2 | Tokat | 3 | 0 | 3 |
| H type | Sulakyurt | ||||||||||
| Çorum | 12 | 4 | 4 | Kırklareli | 8 | 5 | 1 | Tokat | 22 | 0 | 3 |
| Zile | |||||||||||
| Çorum | 5 | 4 | 1 | Kırşehir | 97 | 50 | 41 | Tunceli | 6 | 0 | 6 |
| Sungurlu | |||||||||||
| Çorum | |||||||||||
| Sungurlu | 5 | 4 | 1 | Kırşehir | 97 | 50 | 41 | Tunceli | 6 | 0 | 6 |
| Denizli | 4 | 0 | 4 | Kocaeli | 5 | 2 | 3 | Yalova | 5 | 0 | 0 |
| NP: Number of participants; P: Pregabalin; G: Gabapentin. | |||||||||||
The rate of the individuals participated in the questionnaire and using gabapentinoids are shown in Table 3.
Table 3. Percent of the individuals participated in the questionnaire, and percent of the individuals using gabapentinoids.
| City | A | B | C | D | E | City | A | B | C | D | E |
| Adana | 20 | 4,457 | 0,45 | 11 | 0,25 | Kahramanmaraş | 44 | 1966 | 2,24 | 27 | 1,37 |
| Adıyaman | 2 | 1,427 | 0,14 | 2 | 0,14 | Karabük | 15 | 1121 | 1,34 | 7 | 0,62 |
| Afyon | 36 | 2,269 | 1,59 | 25 | 1,1 | Karaman | 11 | 1099 | 1 | 11 | 1 |
| Ağrı | 14 | 531 | 2,64 | 3 | 0,56 | Kastamonu | 22 | 1159 | 1,9 | 22 | 1,9 |
| Ankara | 136 | 6,661 | 2,04 | 68 | 1,02 | Kayseri | 4 | 1710 | 0,23 | 2 | 0,12 |
| Antalya | 26 | 3,817 | 0,68 | 5 | 0,13 | Kırıkkale | 52 | 607 | 8,57 | 31 | 5,11 |
| Ardahan | 4 | 70 | 5,71 | 0 | 0 | Kırklareli | 8 | 1694 | 0,47 | 6 | 0,35 |
| Aydın | 6 | 2,754 | 0,22 | 2 | 0,07 | Kırşehir | 97 | 1257 | 7,7 | 91 | 7,24 |
| Balıkesir | 35 | 4,823 | 0,73 | 22 | 0,46 | Kocaeli | 35 | 3595 | 0,97 | 9 | 0,25 |
| Batman | 11 | 453 | 2,43 | 4 | 0,88 | Konya | 21 | 2380 | 0,88 | 13 | 0,55 |
| Bitlis | 25 | 626 | 4 | 11 | 1,76 | Manisa | 50 | 3148 | 1,59 | 18 | 0,57 |
| Bolu | 80 | 1,657 | 4,83 | 38 | 2,3 | Mersin | 149 | 3321 | 4,49 | 8 | 0,24 |
| Burdur | 23 | 1,162 | 1,98 | 18 | 1,55 | Muğla | 60 | 2102 | 2,85 | 45 | 2,14 |
| Bursa | 15 | 3,598 | 0,42 | 5 | 0,14 | Nevşehir | 7 | 667 | 1,05 | 7 | 1,05 |
| Çorum | 17 | 1,903 | 0,9 | 13 | 0,68 | Niğde | 21 | 1269 | 1,65 | 18 | 1,42 |
| Denizli | 4 | 2,481 | 0,16 | 4 | 0,16 | Osmaniye | 6 | 2159 | 0,28 | 2 | 0,09 |
| Diyarbakır | 2 | 2,58 | 0,08 | 1 | 0,04 | Rize | 13 | 983 | 1,32 | 3 | 0,31 |
| Erzurum | 66 | 2,131 | 3,1 | 16 | 0,75 | Samsun | 111 | 2492 | 4,45 | 43 | 1,73 |
| Eskişehir | 15 | 1,967 | 0,76 | 6 | 0,31 | Sinop | 25 | 852 | 2,93 | 9 | 1,06 |
| Gaziantep | 5 | 3,409 | 0,15 | 1 | 0,03 | Şanlıurfa | 15 | 1722 | 0,87 | 7 | 0,41 |
| Giresun | 33 | 856 | 3,86 | 33 | 3,86 | Şırnak | 61 | 1193 | 5,11 | 18 | 1,51 |
| Hatay | 1 | 2,551 | 0,04 | 0 | 0 | Tekirdağ | 25 | 3156 | 0,8 | 9 | 0,29 |
| Isparta | 3 | 1,219 | 0,25 | 0 | 0 | Tokat | 25 | 1673 | 1,5 | 6 | 0,36 |
| İstanbul | 70 | 19,338 | 0,36 | 33 | 0,17 | Tunceli | 6 | 51 | 11,76 | 6 | 11,76 |
| İzmir | 96 | 10,051 | 0,96 | 42 | 0,42 | Yalova | 5 | 51 | 9,8 | 0 | 0 |
| A: Total number of the prisoners and convicts participated in the questionnaire on the basis of city; B: Total number of the prisoners and convicts on the basis of city; C: Percent of the individuals participated in the questionnaire; D: Number of the individuals using gabapentinoids; E: Percent of the individuals using gabapentinoids. | |||||||||||
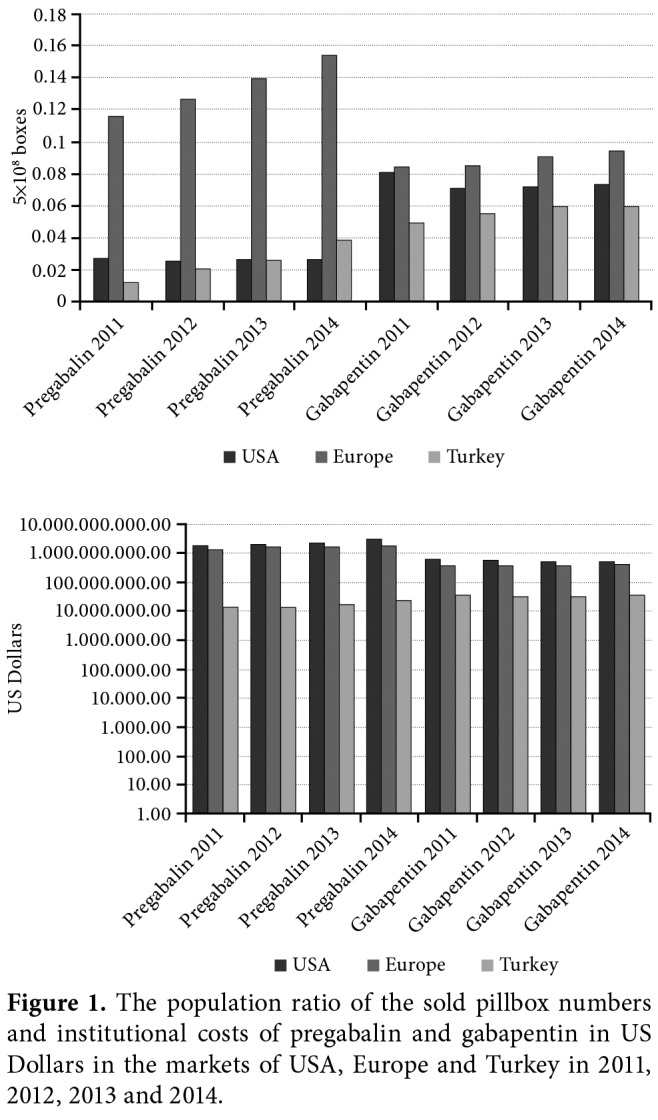
A total of 302 (23.1%) participants were using pregabalin. Ninety seven (27.6%) of the participants had drug reports provided by the hospitals. The question asking the usage frequency of pregabalin was answered as once a day by 25.8%, twice a day by 59.8%, three times a day by 14.0%, and four times a day by 0.3%. The median value of the duration of pregabalin use was five (range, 2 to 13) months. The percent of the individuals using pregabalin for ≥6 months was 48.5%. The question about when pregabalin was started was answered as after imprisonment by 59% of the participants. The question asking the daily pregabalin dose was answered as below: 50 mg by 1.7%, 50-150 mg by 20.2%, 150-300 mg by 34.3%, 300-600 mg by 31.2%, 600-1,200 mg by 10.4%, 1,200-1,800 mg by 1.7%, and more than 1,800 mg by 0.6%. A total of 425 (27.3%) participants were using gabapentin. A hundred and seventy eight (43%) of them had a drug report. A total of 14.9% of the participants used gabapentin once a day, 31.8% twice a day, 49.5% three times a day, 3.8% four times a day. According to the total daily dose of gabapentin, those using it below 300 mg were 6.6%, 300-600 mg were 12.8%, 600-1,200 mg were 32.9%, 1,200-1,800 mg were 17.3% and more than 1,800 mg were 30.5%. The question about when gabapentin was started was answered as after imprisonment by 54.4% of the participants. The median value of the duration of gabapentin use was 10 (range, 4 to 20) months. The percent of the individuals using gabapentin for ≥6 months was 64.7%. It was shown that 36 participants (2%) were using both pregabalin and gabapentin simultaneously. A total of 1,067 participants (65.8%) were using an antidepressant, antipsychotic, or other antiepileptic drugs (other than pregabalin and gabapentin). A total of 14.7% of the participants had a drug report. The question asking the usage frequency of these drugs was answered as once a day by 71%, twice by 25%, three times by 3.5% and four times by 0.4%. While 43.1% of the participants were using the drugs at a dose ≤50 mg, 56.9% of them were using them at a dose above 50 mg. Also, 52.9% of the participants started these drugs after imprisonment. The rate of those who used these drugs for ≥6 months was 56.5% and median value of the duration of the drug use was eight (range, 3 to 20) months. The rates of the diagnosis are shown in Figure 2. The percent of gabapentinoid users was 33.7%, antidepressant users was 20.4%, antipsychotic users was 15.9%, gabapentinoid + antipsychotic users was 8.1%, gabapentinoid + antidepressant users was 6.5%, gabapentinoid + antidepressant + antipsychotic users was 2%. However, 25.2% of the participants gave the answer ‘Yes’ to the question of multiple drug use.
Figure 2. Percents of the diagnosis of the participants (n=1,639). Diagnosis-1: Neuropathic pain; Diagnosis-2: Chronic pain; Diagnosis-3: Depression; Diagnosis-4: Psychosis; Diagnosis-5: Fibromyalgia syndrome; Diagnosis-6: Epilepsy; Other diagnosis: Allergy etc.
While the percent of alcohol use was 58.2% (415 social drinkers and 407 addicted), the percent of those who were addicted was 28.8%. Also, 50.9% of the participants used dope (164 social drinkers and 573 addicted), while 39.6% were addicted. In addition, 27.6% of the participants tended to engage in violence against others, while 28.9% of them tended to engage in violence against the self. The rates of going to the infirmary and referring to the hospital numbers of participants are given in Table 4.
Table 4. Percents of going to the infirmary and referring to the hospital numbers of participants in last three months, six months and one year.
| Number of going to the infirmary | Last 3 months (n=1,080) | Last 6 months (n=1,639) | Last 1 year (n=1,233) |
| (%) | (%) | (%) | |
| 0 | 0 | 36,2 | 0,2 |
| 1-3 | 32,1 | 11,0 | 14,4 |
| 4-7 | 42,5 | 14,3 | 13,1 |
| 8-11 | 16,0 | 17,6 | 13,0 |
| 12-15 | 5,2 | 9,8 | 15,7 |
| 16-20 | 3,0 | 5,9 | 13,9 |
| 21-26 | 1,2 | 4,9 | 29,1 |
| >26 | 0 | 0,2 | 0,6 |
| Number of referring to the hospital | Last 3 months (n=946) | Last 6 months (n=950) | Last 1 year (n=1,171) |
| (%) | (%) | (%) | |
| 0 | 0,2 | 0,1 | 0,2 |
| 1-3 | 67,8 | 46,4 | 31,5 |
| 4-7 | 23,4 | 31,1 | 31,1 |
| 8-11 | 5,7 | 12,1 | 17,2 |
| 12-15 | 2,3 | 5,6 | 8,4 |
| 16-20 | 0,4 | 3,4 | 4,4 |
| 21-26 | 0,2 | 1,1 | 6,9 |
| >26 | 0 | 0,3 | 0,3 |
The highest rates among the withdrawal symptoms were seen in restlessness (75.7%), sleeplessness (73.5%), and nervousness (73.0%). Other withdrawal symptoms were headache (50.5%), shivering (42.1%), sweating (39.1%), xerostomia (33.4%), palpitation (31%), nightmare (28.9%), having fever (28.4%), hallucination (26.4%), dizziness (24.9%), nausea (15.2%), stomachache (13.1%), epileptic seizure (11.2%), and vomiting (9.7%). Withdrawal symptoms reported by the participants with their individual expressions apart from the questions asked were pain in different regions of the body, thinking of bad things, allergic symptoms and acnes in the body, anti-sociality, hyper-reflection, paresthesia in the feet, burning and itching, contractions and cramping, fainting, biting lips, fatigue, depression, reluctance to work, discouragement and fear, urinary incontinence at night, restless leg syndrome, melancholy, tendency to be asocial, diarrhea, lack of appetite, teeth grinding, self-destruction and giving harm to others, panic attack, impatience, suicide attempt, skepticism, becoming seduced, obsession, and being cold. There was a positive correlation between the pregabalin use and alcohol addiction (Cramer ʼs V=0.212), dope addiction (Cramer ʼs V=0.147), number of going to the infirmary in the last one year (Cramer ʼs V=0.241), last six months (Cramer ʼs V=0.229) and last three months (Cramer ʼs V=0.223) and number of referring to the hospital in the last one year (r=0.245), last six months (Cramer ʼs V=0.258) and last three months (Cramer ʼs V=0.196). While there was no correlation between pregabalin use and tendency to engage in violence against others (Cramer ʼs V=0.030), there was positive correlation between pregabalin use and tendency to engage in violence against the self (Cramer ʼs V=0.072). There was a positive correlation between pregabalin use and withdrawal symptoms such as sweating (Cramer ʼs V=0.059), having fever (Cramer ʼs V=0.091), stomachache (Cramer ʼs V=0.076), nausea (Cramer ʼs V=0.107), vomiting (Cramer ʼs V=0.101), hallucination (Cramer ʼs V=0.058), headache (Cramer ʼs V=0.066), nervousness (Cramer ʼs V=0.061), sleeplessness (Cramer ʼs V=0.139), nightmare (Cramer ʼs V=0.095) and restlessness (Cramer ʼs V=0.087). There was a positive correlation between the duration of pregabalin use and alcohol addiction (Cramer ʼs V=0.186), dope addiction (Cramer ʼs V=0.166), number of going to the infirmary in the last one year (Cramer ʼs V=0.268) and last six months (Cramer ʼs V=0.201), number of referring to the hospital in the last three months (Cramer ʼs V=0.273). While there was no correlation between the duration of pregabalin use and tendency to engage in violence against others (Cramer ʼs V=0.066), there was a positive correlation between the duration of pregabalin use and tendency to engage in violence against the self (Cramer ʼs V=0.100). There was a positive correlation between the duration of pregabalin use and withdrawal symptoms such as stomachache (Cramer ʼs V=0.183), palpitation (Cramer ʼs V=0.151), hallucination (Cramer ʼs V=0.330), dizziness (Cramer ʼs V=0.221), nervousness (Cramer ʼs V=0.153), sleeplessness (Cramer ʼs V=0.183), epileptic seizure (Cramer ʼs V=0.258), xerostomia (Cramer ʼs V=0.178) and restlessness (Cramer ʼs V=0.134). In addition, there was a positive correlation between the dose of pregabalin and alcohol addiction (Cramer ʼs V=0.152), dope addiction (Cramer ʼs V=0.132), number of going to the infirmary in the last six months (Cramer ʼs V=0.268), number of referring to the hospital in the last six months (Cramer ʼs V=0.245) and last three months (Cramer ʼs V=0.229). However, there was no correlation between the dose of pregabalin and tendency to engage in violence either against others or the self (Cramer ʼs V=0.073 and Cramer ʼs V=0.020, respectively). There was a positive correlation between the dose of pregabalin and withdrawal symptoms such as sweating (Cramer ʼs V=0.155), stomachache (Cramer ʼs V=0.166), nausea ( C r a m e r ʼs V = 0 . 1 5 4 ) , v o m i t i n g ( C r a m e r ʼs V = 0 2 0 1 ) , palpitation (Cramer ʼs V=0.163), hallucination (Cramer ʼs V=0.226), dizziness (Cramer ʼs V=0.245), sleeplessness (Cramer ʼs V=0.194), nightmare (Cramer ʼs V=0.257), epileptic seizure (Cramer ʼs V=0.240), and xerostomia (Cramer ʼs V=0.245). There was a positive correlation between the usage frequency of pregabalin and alcohol addiction (Cramer ʼs V=0.147), number of going to the infirmary in the last one year (Cramer ʼs V=0.209), last six months (Cramer ʼs V=0.219), and last three months (Cramer ʼs V=0.186), and number of referring to the hospital in the last three months (Cramer ʼs V=0.160). While there was a correlation between the usage frequency of pregabalin and tendency to engage in violence against others (Cramer ʼs V=0.120), there was no correlation between the usage frequency of pregabalin and tendency to engage in violence against the self (Cramer ʼs V=0.006). There was a positive correlation between the usage frequency of pregabalin and withdrawal symptoms such as sweating (Cramer ʼs V=0.229), having fever (Cramer ʼs V=0.226), nausea (Cramer ʼs V=0.212), vomiting (Cramer ʼs V=0.294), hallucination (Cramer ʼs V=0.236), dizziness (Cramer ʼs V=0.215), sleeplessness (Cramer ʼs V=0.211), nightmare (Cramer ʼs V=0.231), epileptic seizure (Cramer ʼs V=0.224), and xerostomia (Cramer ʼs V=0.167). There was a positive correlation between the gabapentin use and alcohol addiction (Cramer ʼs V=0.125), dope addiction (Cramer ʼs V=0.135), number of going to the infirmary in the last one year (Cramer ʼs V=0.275), last six months (Cramer ʼs V=0.260) and last three months (Cramer ʼs V=0.251), and number of referring to the hospital in the last one year (Cramer ʼs V=0.179). While there was no correlation between gabapentin use and tendency to engage in violence against others (Cramer ʼs V=0.025), there was positive correlation between gabapentin use and tendency to engage in violence against the self (Cramer ʼs V=0.046). There was a positive correlation between gabapentin use and withdrawal symptoms such as sweating (Cramer ʼs V=0.060), having fever (Cramer ʼs V=0.097), palpitation (Cramer ʼs V=0.056) , headache (Cramer ʼs V=0.120 ) , nervousness (Cramer ʼs V=0.094), sleeplessness (Cramer ʼs V=0.085), and restlessness (Cramer ʼs V=0.076). There was positive correlation between the duration of gabapentin use and alcohol addiction (Cramer ʼs V=0.227), dope addiction (Cramer ʼs V=0.239), number of going to the infirmary in the last one year (Cramer ʼs V=0.216) and last six months (Cramer ʼs V=0.198), and number of referring to the hospital in the last six months (Cramer ʼs V=0.200). There was a positive correlation between the duration of gabapentin use and tendency to engage in violence against others and against the self (Cramer ʼs V=0.156 and Cramer ʼs V=0.188, respectively). There was a positive correlation between the duration of gabapentin use and withdrawal symptoms such as palpitation (Cramer ʼs V=0.110), hallucination (Cramer ʼs V=0.128), dizziness (Cramer ʼs V=0.169), nervousness (Cramer ʼs V=0.149), sleeplessness (Cramer ʼs V=0.170), xerostomia (Cramer ʼs V=0.136), and restlessness (Cramer ʼs V=0.117). On the other hand, there was no correlation between the dose of gabapentin and alcohol addiction, dope addiction, number of going to the infirmary and referring to the hospital, tendency to engage in violence against others or the self (p>0.05). There was a positive correlation between the dose of gabapentin and withdrawal symptoms such as sweating (Cramer ʼs V=0.133), vomiting (Cramer ʼs V=0.196), palpitation (Cramer ʼs V=0.149), headache (Cramer ʼs V=0.149), and nervousness (Cramer ʼs V=0.125). There was a positive correlation between the frequency of gabapentin usage and dope addiction (Cramer ʼs V=0.120), number of going to the infirmary in the last one year (Cramer ʼs V=0.190) and last six months (Cramer ʼs V=0.239). There was a positive correlation between the frequency of gabapentin usage and tendency to engage in violence against others and against the self (Cramer ʼs V=0.129 and Cramer ʼs V=0.184, respectively). There was a positive correlation between the frequency of gabapentin usage and withdrawal symptom of sleeplessness (Cramer ʼs V=0.120). There was a positive correlation between the use of other drugs comprising antidepressant, antipsychotic, and antiepileptics (other than gabapentinoids) and alcohol addiction (Cramer ʼs V=0.136), dope addiction (Cramer ʼs V=0.084), number of going to the infirmary in the last one year (Cramer ʼs V=0.286), last six months (Cramer ʼs V=0.277) and last three months (Cramer ʼs V=0.259), and number of referring to the hospital in the last one year (Cramer ʼs V=0.210). While there was no correlation between the use of these drugs and tendency to engage in violence against others (Cramer ʼs V=0.033), there was a positive correlation between the use of these drugs and tendency to engage in violence against the self (Cramer ʼs V=0.057). There was also a positive correlation between the use of these drugs and withdrawal symptoms such as sweating (Cramer ʼs V=0.068), having fever (Cramer ʼs V=0.095), vomiting (Cramer ʼs V=0.072), hallucination (Cramer ʼs V=0.120), headache (Cramer ʼs V=0.088), sleeplessness (Cramer ʼs V=0.276), nightmare (Cramer ʼs V=0.133), and epileptic seizure (Cramer ʼs V=0.096). There was a positive correlation between the multiple drug use and alcohol addiction (Cramer ʼs V=0.056), dope addiction (Cramer ʼs V=0.033), number of going to the infirmary in the last one year (Cramer ʼs V=0.137), last six months (Cramer ʼs V=0.129) and last three months (Cramer ʼs V=0.087) and number of referring to the hospital in the last one year (Cramer ʼs V=0.124), last six months (Cramer ʼs V=0.120), and last three months (Cramer ʼs V=0.070). While there was no correlation between the multiple drug use and tendency to engage in violence against others (Cramer ʼs V=0.76), there was a positive correlation between the multiple drug use and tendency to engage in violence against the self (Cramer ʼs V=0.075). There was a positive correlation between the multiple drug use and withdrawal symptoms such as sweating (Cramer ʼs V=0.068), having fever (Cramer ʼs V=0.086), stomachache (Cramer ʼs V=0.127), nausea (Cramer ʼs V=0.147), vomiting (Cramer ʼs V=0.151), hallucination (Cramer ʼs V=0.223), headache (Cramer ʼs V=0.087), nervousness (Cramer ʼs V=0.076), sleeplessness (Cramer ʼs V=0.151), nightmare (Cramer ʼs V=0.189), and restlessness (Cramer ʼs V=0.075). However, there was no significant correlation between the duration of imprisonment (<6 months in 14.7%, 6 months-1 year in 16%, 1-3 years in 30.3%, 3-6 years in 13.9%, 6-10 years in 11.9% and >10 years in 13.2%) and other variables.
Discussion
The major finding of our study is that it is the first study about the use of gabapentinoids and addiction in penal institutions. One of the limitations of our study is that since the participants were completely free in participating in the questionnaire and answering the questions, there was a high dependence on participants, particularly about not telling the truth in terms of drug addiction and abuse. By a higher participation and application of a stricter questionnaire accompanied by medical records, independent of participants, the results would be much realistic. The response rate was low to some questions, as they were concerning the small part of the participants who were using gabapentinoids. For instance, the question asking the pregabalin drug report or the question asking the duration of pregabalin use had response rates about 20%, as the participants who did not use pregabalin previously did not answer these questions. However, the response rates in the questions that concern all the participants were high (Table 1). According to the drug market data, it was estimated that the number of individuals using gabapentin was about 240,682, while the number of individuals using pregabalin was about 249,793. Considering that the population above 18 years old was 52,314,553 individuals (according to 2014 data of Turkish Statistical Institute),[20] it was thought that the rate of gabapentinoid usage of normal population was about 0.94%. At the E column in Table 3, it is seen that the rate of gabapentinoid usage was quite above the normal population, particularly in some institutions. It was found that pregabalin, which is recommended to be used twice a day, was used at a percent of 14.3% three times a day and more. While ideal daily dose of pregabalin is accepted as 300 mg (rarely can be increased up to 600 mg/day), it was used at a percent of 43.9% more than 300 mg daily. This may be due to the fact that the drug was abused or that the patients and infirmary personnel were not sufficiently informed by physicians. Moreover, that 59% started pregabalin after imprisonment and 48.5% used it for ≥6 months can be interpreted as to be careful in terms of abuse and addiction. It was found that gabapentin, which is recommended to be used as at least 1,800 mg daily in three divided doses, was used in true frequency only by 49.5% of the participants and in true doses only by 47.8%. Similar to pregabalin, that 54.4% started gabapentin after imprisonment and 64.7% used it for ≥6 months can be interpreted as to be careful in terms of abuse and addiction. The fact that 36 participants (2%) have used these two groups of drugs simultaneously, although simultaneous use of pregabalin and gabapentin is not recommended, shows the importance of questioning drug use by physicians, sufficiently informing the patient and considering drug abuse. Besides, the rate of high usage of antidepressant, antipsychotic, or other antiepileptic drugs, and mostly starting these drugs after imprisonment and their long duration of use indicate that the physicians should be careful while managing the treatments. That 16.6% of the participants have used drugs simultaneously in more than one group and 2% of them have used gabapentinoid + antidepressant + antipsychotic simultaneously revealed the requirement for being careful about multiple drug use and drug abuse and addiction. Neuropathic pain examples encountered in the clinic can be considered as post herpetic neuralgia, diabetic neuropathy, post-traumatic neuralgia and central post-stroke pain syndrome. Frequently encountered symptoms in neuropathic pain cases are spontaneous pain, allodynia, hyperalgesia, and paresthesia in the painful region.[21] The presence of neuropathic pain in 35.5% of the participants suggests the question whether the necessary criteria were adequately questioned for this diagnosis, as the maximum prevalence of neuropathic pain is 1% in the Western societies.[21] The high rate of those reporting that they were alcohol and/or drug addicted strengthen the predictions regarding that probability of addiction may be high in penal institutions, and reveal the possibility that use of gabapentinoids which can also be used in the treatment of addiction can be more than predicted in penal institutions. The numbers of going to the infirmary and referring to the hospital were generally high in participants. However, the rates of referring to the hospital were lower in the last three months, compared to the last one year. This can be interpreted in a way that condition of the patients becomes more stabilized as a result of the treatment. Withdrawal symptoms such as restlessness, sleeplessness and nervousness show that abuse and addiction potential of these drugs should be kept in mind. Significant correlations between the gabapentinoid use, dose, usage frequency, duration of use and alcohol/dope addiction, number of going to the infirmary, referring to the hospital and also various withdrawal symptoms suggest abuse and addiction potential of these drugs, and also it should be noted that they may have a role in the treatment of addiction. There was a significant correlation between the use of other drugs comprising antidepressant, antipsychotics, other antiepileptics, and alcohol/dope addiction, the number of going to the infirmary and referring to the hospital and also various withdrawal symptoms. Also, multiple drug use was high and there was significant correlation between the multiple drug use and alcohol/dope addiction, number of going to the infirmary and referring to the hospital and also various withdrawal symptoms. The presence of the results which can be accepted as contradictory in the questions about violence against others or violence against the self were attributed to the accuracy and consistency levels of the answers given by the participants to these questions. Addiction is a chronic neurobiological disease involving genetic, psychosocial, and environmental factors in its development. Addiction is a manifestation occurring when a substance is taken for the wrong purposes and in gradually increasing amounts as a result of the tolerance developing against that substance, when it is continued to be used although it causes problems in the life of the person, and as withdrawal symptoms appear, when substance intake is reduced or quitted. The common feature of the addictive substances is that they have a reinforcing effect on their intake. Due to the effects on the reward system in brain, the person is addicted to pleasure- inducing feature of the substance and becomes addicted upon using it repeatedly. Addicted person continues to use substance s/he is addicted compulsively despite negative results s/he experienced. It is shown that the usage rates of antipsychotic and antidepressant were quite high among those participating in our study. The studies conducted with antidepressant drugs have shown that these drugs back up the treatment in the presence of comorbid depression in alcohol addicts, they treat depression and reduce alcohol intake.[22-25] Although typical antipsychotics relieve the psychotic symptoms originating from dope addictions, usage frequency of substance may increase in these patients due to the side effects. Studies on olanzapine, clozapine, and quetiapine in regard to the use of antipsychotics in the treatment of alcohol addiction are available. In previous studies, the results regarding that olanzapine, clozapine treatments decreased the desire for alcohol in patients diagnosed with schizophrenia and schizoaffective disorder.[26-28] The studies examining the effects of quetiapine on alcohol and substance intake were conducted primarily in the patient populations accompanied by bipolar and schizophrenia diagnoses. Quetiapine was associated with the days of staying sober in the alcohol addiction and is shown to have reduced anxiety, depression and food craving. Several studies have shown that it increases substance abuse in patients only with substance use disorders. On the other hand, cases about the abuse of quetiapine and risk of addiction are increasing more and more in the literature. The most promising antipsychotic agent in the treatment of alcohol addiction seems to be aripiprazole. In a study comparing the aripiprazole, a partial dopamine agonist, with naltrexone, it is reported that aripiprazole is as effective as naltrexone in reducing alcohol use and food craving.[29-31] Antiepileptic drugs are known to be used frequently in the treatment of cleaning in alcohol addiction, withdrawal symptoms and epileptic seizures.[32] Data regarding that valproate and lamotrigine reduce the desire for and intake of alcohol in the patients with bipolar disorder are obtained.[32-34] The GABA and gabapentin are among the agents the use of which would be considered in the treatment of alcohol addiction, particularly in the withdrawal period in the future.[22,35] Several studies have concluded that pregabalin does not show apparent drug interactions, and there is not any tolerance and abuse;[36] however Grosshans et al.[17] presented the first pregabalin addiction case in 2010. A 47-year-old male patient in whom pregabalin was started due to alcohol addiction used 7,500 mg/day pregabalin to eliminate alcohol withdrawal symptoms. Although no toxic finding was encountered, sweating, shivering, restlessness, and hypertension were seen in its deprivation and these findings were treated with benzodiazepines; however, the patient continued to use 6,000 mg/day pregabalin again. It is concluded that it is necessary to pay attention, particularly to those who have an addiction history in regard to the abuse of pregabalin.[17] There was a significant correlation between the pregabalin use and various withdrawal symptoms in our study. It is found that the usage rate of pregabalin and gabapentin together with antipsychotic/ antidepressants was high in our study. This situation gives rise to the thought that gabapentinoids can be used off-label with neuropathic pain or epilepsy diagnoses, although they have not taken the aforementioned indications yet in Turkey. In conclusion, although gabapentinoids seem to be used in the treatment of addiction and are proved effective treatment agents in terms of true diagnosis, suitable follow-up and timely completion of the treatment, it is necessary to strictly control their use due to the probability of abuse and addiction.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Dooley DJ, Donovan CM, Meder WP, Whetzel SZ. Preferential action of gabapentin and pregabalin at P/Q-type voltage-sensitive calcium channels: inhibition of K+-evoked [3H]-norepinephrine release from rat neocortical slices. Synapse. 2002;45:171–190. doi: 10.1002/syn.10094. [DOI] [PubMed] [Google Scholar]
- 2.Gee NS, Brown JP, Dissanayake VU, Offord J, Thurlow R, Woodruff GN. The novel anticonvulsant drug, gabapentin (Neurontin), binds to the alpha2delta subunit of a calcium channel. J Biol Chem. 1996;271:5768–5776. doi: 10.1074/jbc.271.10.5768. [DOI] [PubMed] [Google Scholar]
- 3.Kelly KM. Gabapentin. Kelly KM. Gabapentin. Antiepileptic mechanism of action. Neuropsychobiology 1998;38:139-44. doi: 10.1159/000026529. [DOI] [PubMed] [Google Scholar]
- 4.Dooley DJ, Donovan CM, Pugsley TA. Stimulus-dependent modulation of [(3)H]norepinephrine release from rat neocortical slices by gabapentin and pregabalin. J Pharmacol Exp Ther. 2000;295:1086–1093. [PubMed] [Google Scholar]
- 5.Jones DL, Sorkin LS. Systemic gabapentin and S(+)-3- isobutyl-gamma-aminobutyric acid block secondary hyperalgesia. Brain Res. 1998;810:93–99. doi: 10.1016/s0006-8993(98)00890-7. [DOI] [PubMed] [Google Scholar]
- 6.Fink K, Dooley DJ, Meder WP, Suman-Chauhan N, Duffy S, Clusmann H, et al. Inhibition of neuronal Ca(2+) influx by gabapentin and pregabalin in the human neocortex. Neuropharmacology. 2002;42:229–236. doi: 10.1016/s0028-3908(01)00172-1. [DOI] [PubMed] [Google Scholar]
- 7.Dooley DJ, Mieske CA, Borosky SA. Inhibition of K(+)-evoked glutamate release from rat neocortical and hippocampal slices by gabapentin. Neurosci Lett. 2000;280:107–110. doi: 10.1016/s0304-3940(00)00769-2. [DOI] [PubMed] [Google Scholar]
- 8.Maneuf YP, Hughes J, McKnight AT. Gabapentin inhibits the substance P-facilitated K(+)-evoked release of [(3)H] glutamate from rat caudial trigeminal nucleus slices. Pain. 2001;93:191–196. doi: 10.1016/S0304-3959(01)00316-5. [DOI] [PubMed] [Google Scholar]
- 9.Bialer M, Johannessen SI, Kupferberg HJ, Levy RH, Loiseau P, Perucca E. Progress report on new antiepileptic drugs: a summary of the fourth Eilat conference (EILAT IV) Epilepsy Res. 1999;34:1–41. doi: 10.1016/s0920-1211(98)00108-9. [DOI] [PubMed] [Google Scholar]
- 10.Welty D, Wang Y, Busch JA, Taylor CP, Vartanian MG, Radulovic LL. Pharmacokinetics (PK) and pharmacodynamics (PD) of CI-1008 (pregabalin) and gabapentin in rats with maximal electroshock. Epilepsia. 1997;38:35–35. [Google Scholar]
- 11.Brodie MJ, French JA. Management of epilepsy in adolescents and adults. Lancet. 2000;356:323–329. doi: 10.1016/S0140-6736(00)02515-0. [DOI] [PubMed] [Google Scholar]
- 12.Oulis P, Konstantakopoulos G. Pregabalin in the treatment of alcohol and benzodiazepines dependence. CNS Neurosci Ther. 2010;16:45–50. doi: 10.1111/j.1755-5949.2009.00120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perrot S, Dickenson AH, Bennett RM. Fibromyalgia: harmonizing science with clinical practice considerations. Pain Pract. 2008;8:177–189. doi: 10.1111/j.1533-2500.2008.00190.x. [DOI] [PubMed] [Google Scholar]
- 14.Arnold LM, Goldenberg DL, Stanford SB, Lalonde JK, Sandhu HS, Keck PE Jr, et al. Gabapentin in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled, multicenter trial. Arthritis Rheum. 2007;56:1336–1344. doi: 10.1002/art.22457. [DOI] [PubMed] [Google Scholar]
- 15.Schwan S, Sundström A, Stjernberg E, Hallberg E, Hallberg P. A signal for an abuse liability for pregabalin--results from the Swedish spontaneous adverse drug reaction reporting system. Eur J Clin Pharmacol. 2010;66:947–953. doi: 10.1007/s00228-010-0853-y. [DOI] [PubMed] [Google Scholar]
- 16.Ilhanli I, Guder N. Abuse and addiction of gabapentinoids versus treatment: Two sharp knife edges. Int J Curr Pharmaceut Clin Res. 2016;6:4–9. [Google Scholar]
- 17.Grosshans M, Mutschler J, Hermann D, Klein O, Dressing H, Kiefer F, et al. Pregabalin abuse, dependence, and withdrawal: a case report. Am J Psychiatry. 2010;167:869–869. doi: 10.1176/appi.ajp.2010.09091269. [DOI] [PubMed] [Google Scholar]
- 18.Yargic I, Özdemiroglu FA. Pregabalin abuse: Case report. Bulletin of Clinical. Psychopharmacology. 2011;21:64–66. [Google Scholar]
- 19.Teltzrow R. International Conference on Mental Health and Addiction; 2013 Feb 27-28. Bucharest: 2013. Drug use in Prisons-Risks, Public Health and Human Rights; pp. 5–9. [Google Scholar]
- 20. Available from: www.tuik.gov.tr. [Google Scholar]
- 21.Neuropathic pain. Available from: http://www.jcp.sagepub.com/cgi/content/full. [Google Scholar]
- 22.Patel KH. Pharmacologic management of alcohol dependence. US Pharmacist. 2009;34:1–4. [Google Scholar]
- 23.Graham K, Massak A. Alcohol consumption and the use of antidepressants. CMAJ. 2017;176:633–637. doi: 10.1503/cmaj.060446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muhonen LH, Lahti J, Sinclair D, Lönnqvist J, Alho H. Treatment of alcohol dependence in patients with co-morbid major depressive disorder--predictors for the outcomes with memantine and escitalopram medication. Subst Abuse Treat Prev Policy. 2008;3:20–20. doi: 10.1186/1747-597X-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.García-Portilla MP, Bascarán MT, Saiz PA, Mateos M, González-Quirós M, Pérez P, et al. Effectiveness of venlafaxine in the treatment of alcohol dependence with comorbid depression. Actas Esp Psiquiatr. 2005;33:41–45. [PubMed] [Google Scholar]
- 26.Hutchison KE, Ray L, Sandman E, Rutter MC, Peters A, Davidson D, et al. The effect of olanzapine on craving and alcohol consumption. Neuropsychopharmacology. 2006;31:1310–1317. doi: 10.1038/sj.npp.1300917. [DOI] [PubMed] [Google Scholar]
- 27.Azorin JM, Bowden CL, Garay RP, Perugi G, Vieta E, Young AH. Possible new ways in the pharmacological treatment of bipolar disorder and comorbid alcoholism. Neuropsychiatr Dis Treat. 2010;6:37–46. doi: 10.2147/ndt.s6741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wiesbeck GA, Weijers HG, Lesch OM, Glaser T, Toennes PJ, Boening J. Flupenthixol decanoate and relapse prevention in alcoholics: results from a placebo-controlled study. Alcohol Alcohol. 2001;36:329–334. doi: 10.1093/alcalc/36.4.329. [DOI] [PubMed] [Google Scholar]
- 29.Martinotti G, Di Nicola M, Di Giannantonio M, Janiri L. Aripiprazole in the treatment of patients with alcohol dependence: a double-blind, comparison trial vs. naltrexone. J Psychopharmacol. 2009;23:123–129. doi: 10.1177/0269881108089596. [DOI] [PubMed] [Google Scholar]
- 30.Wang LL, Yang AK, He SM, Liang J, Zhou ZW, Li Y, et al. Identification of molecular targets associated with ethanol toxicity and implications in drug development. Curr Pharm Des. 2010;16:1313–1355. doi: 10.2174/138161210791034030. [DOI] [PubMed] [Google Scholar]
- 31.Erdoğan A, Yurteri N. Aripiprazole treatment in the adolescent patients with inhalants use disorders and conduct disorder: a retrospective case analysis. Symposium. 2010;48:229–233. [Google Scholar]
- 32.Fernandez Miranda JJ, Marina González PA, Montes Pérez M, Díaz González T, Gutierrez Cienfuegos E, Antuña Díaz MJ, et al. Topiramate as add-on therapy in non-respondent alcohol dependant patients: a 12 month follow-up study. Actas Esp Psiquiatr. 2007;35:236–242. [PubMed] [Google Scholar]
- 33.Johnson BA, Rosenthal N, Capece JA, Wiegand F, Mao L, Beyers K, et al. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641–1651. doi: 10.1001/jama.298.14.1641. [DOI] [PubMed] [Google Scholar]
- 34.Rubio G, López-Muñoz F, Alamo C. Effects of lamotrigine in patients with bipolar disorder and alcohol dependence. Bipolar Disord. 2006;8:289–293. doi: 10.1111/j.1399-5618.2006.00292.x. [DOI] [PubMed] [Google Scholar]
- 35.Kampman KM. New medications for the treatment of cocaine dependence. Ann Ist Super Sanita. 2009;45:109–115. [PubMed] [Google Scholar]
- 36.Bech P. Dose-response relationship of pregabalin in patients with generalized anxiety disorder. A pooled analysis of four placebo-controlled trials. Pharmacopsychiatry. 2007;40:163–168. doi: 10.1055/s-2007-984400. [DOI] [PubMed] [Google Scholar]