Abstract
Background
Prior studies have described racial/ethnic disparities in door‐to‐balloon (DTB) time for patients undergoing primary percutaneous coronary intervention (PCI). We sought to compare DTB time between different racial/ethnic groups undergoing primary PCI for ST‐elevation myocardial infarction in Get With the Guidelines (GWTG).
Hypothesis
There may be differences in D2B time associated with race/ethnicity.
Methods
We identified 7445 white (n = 6365), African American (n = 568), and Hispanic (n = 512) patients undergoing primary PCI.
Results
There were no differences in the median DTB time between white (74 minutes; intraquartile range [IQR], 54–99), African American (77 minutes; IQR, 57–100), and Hispanic (75 minutes; IQR, 56–100) (P = 0.13) patients. There were no crude differences in DTB time ≤90 minutes; however, after adjusting for confounders, African American race was associated with lower odds of DTB time ≤90 minutes (odds ratio [OR]: 0.84; 95% confidence interval [CI]: 0.70‐0.99; P = 0.04). This association was seen in African American males (OR: 0.66; 95% CI: 0.55‐0.80) but not African American females (OR: 1.27; 95% CI: 0.96‐1.68). Overall, Hispanic ethnicity was not associated with a difference in DTB time ≤90 minutes (OR: 0.98; 95% CI: 0.77‐1.25; P = 0.88); although Hispanic males did have a slightly longer median DTB time compared with whites. During the study, the proportion of patients with DTB times ≤90 minutes increased for all groups, and mortality was similar between groups (white 3.8%, African American 3.0%, Hispanic 4.1%, P = 0.62).
Conclusions
In GWTG‐Coronary Artery Disease, small differences in DTB times persist among different races/ethnicities. However, the proportion achieving DTB times ≤90 minutes has increased substantially for all patients over time, and there was no association between race/ethnicity and in‐hospital mortality.
Introduction
Revascularization within 90 minutes of presentation is a quality indicator in the treatment of patients with ST‐elevation myocardial infarction (STEMI).1, 2, 3 Previous studies have found that African Americans and patients of Hispanic ethnicity have significantly higher door‐to‐balloon time and mortality from acute myocardial infarction.4, 5, 6, 7 Analyses of the etiology of these disparities suggest that the differences may be related to systems problems at treating hospitals.4, 8 There have been numerous quality improvement initiatives to improve treatment for acute myocardial infarction, including efforts to reduce door‐to‐balloon time, since these data were collected.9, 10, 11 Some analyses have suggested that these efforts may have lessened but not resolved these previously described racial/ethnic disparities.
We hypothesized that increased attention on door‐to‐balloon time through quality improvement measures would reduce previously described disparities. We sought to determine if disparities in time to revascularization and mortality remain in patients undergoing primary percutaneous coronary intervention (PCI) at hospitals participating in the Get With the Guidelines‐Coronary Artery Disease (GWTG‐CAD) national quality improvement program. Furthermore, differences between racial/ethnic groups in door‐to‐balloon time and mortality were identified and studied to determine if these relationships changed over time. Finally, we sought to determine if race/ethnicity was associated with door‐to‐balloon time and door‐to‐balloon time ≤90 minutes after controlling for potential confounders.
Methods
Data Source and Study Population
Details of the American Heart Association's (AHA) GWTG‐CAD quality improvement program have been published previously.10, 14 In brief, the GWTG‐CAD database is an observational registry developed by the AHA to prospectively collect data and provide feedback on performance and quality of care to hospitals across the United States.10, 15 All participating institutions are required to comply with local regulatory and privacy guidelines, and if required, to secure institutional review board approval. Because data were used primarily at the local site for quality improvement, sites have been granted a waiver of informed consent under the common rule. Outcome Sciences, Inc. (Cambridge, MA) serves as the coordinating center, and the Duke Clinical Research Institute (Durham, NC) serves as the data analysis center.
Patients were included in the analysis if they were admitted to a participating GWTG‐CAD hospital and underwent primary PCI for STEMI (Supplementary Figure 1). Patients categorized themselves by race/ethnic group into non‐Hispanic white, African American/black (irrespective of ethnicity), and non‐black Hispanic. Patients of race other than non‐Hispanic white, African American/black, or ethnicity other than Hispanic were not included in this analysis.
A total of 7445 patients admitted to fully participating GWTG‐CAD hospitals from April 1, 2006 to June 30, 2009 were included in the analysis. Patients were excluded if they were admitted with heart failure or a diagnosis other than confirmed STEMI. Of the patients admitted with STEMI, those not treated with primary PCI within 24 hours of presentation were excluded. Patients were not included in the modeling if door‐to‐balloon time was missing, and sites were not included if they were not fully participating (<250 patients enrolled in the GWTG‐CAD registry during that quarter). Patients transferred from an institution to a GWTG‐CAD hospital were excluded due to the inability to calculate total time from initial presentation to revascularization.
Statistical Analysis
The median and interquartile range (IQR) was reported for all continuous variables. Categorical variables were reported as a number and percentage. Tests of significance between the different racial groups were performed using Pearson χ2 tests for categorical variables and Kruskal‐Wallis tests for continuous variables. Changes in the proportion of patients with door to balloon time ≤90 minutes from 2006 to 2009 were assessed with the Cochran‐Armitage trend test.
Differences in door‐to‐balloon time were determined and adjusted for potential confounders by developing sequential linear regression models using the generalized estimating equation method to account for hospital clustering. Door‐to‐balloon time was skewed; therefore, door‐to‐balloon time was log transformed prior to the development of the linear regression model. The log transformed door‐to‐balloon time data were only utilized in the linear regression models, and all other data presented reflected raw, nontransformed data. The coefficients from the log transformed linear regression model were then exponentiated and reflect the ratio between the geometric mean of the group under consideration and the reference group. Unadjusted models were developed that evaluated race/ethnicity (whites = reference), gender (male = reference) and the interaction between gender/race. Two separate models that adjusted for potential confounders were built using similar techniques. The first model evaluated race, gender, and potential confounders (medical history, age, body mass index, insurance, hospital characteristics [region, academic status, size]) and calendar time. We then evaluated whether the impact of race varied by gender by including an interaction term with gender/race.
The relationship between race/ethnicity and door‐to‐balloon time ≤90 minutes was studied using sequential multivariable logistic regression models (white = reference). Similar models were built to evaluate the relationship between race/ethnicity and in‐hospital mortality. These models were built utilizing generalized estimating to account for clustering.16 P values were computed using the Wald test. The first model evaluated the relationship between race/ethnicity and outcome without adjusting for potential confounders. Models were then developed in sequential fashion that controlled for baseline characteristics, baseline and hospital characteristics, baseline characteristics and insurance status, baseline/hospital characteristics and insurance status, and baseline characteristics and a multiplicative interaction term to assess for effect modification between race/ethnicity and gender. The final model controlled for baseline/hospital characteristics, insurance status, calendar time, and a multiplicative interaction term to assess for effect modification between gender and race/ethnicity. In‐hospital mortality was evaluated using similar models.
All statistical analyses were performed by the Duke Clinical Research Institute, which had full access to the data, using SAS version 9.2 (SAS Institute, Cary, NC). All P values were 2‐tailed with statistical significance set at 0.05, and confidence intervals (CIs) were calculated at the 95% level.
Results
A total of 7445 patients from 137 sites were included in the analysis; 6365 (85.5%) were white, 568 (7.6%) were African American, and 512 (6.9%) were Hispanic. White patients were older and less likely to be uninsured or insured with Medicaid. African Americans were more likely to have had a prior myocardial infarction, chronic kidney disease, heart failure, hypertension, cerebrovascular accident/transient ischemic attack, and to smoke. African Americans were more often treated at academic hospitals with cardiac surgery capabilities (Table 1).
Table 1.
Baseline Characteristics by Race/Ethnicity
| White, n = 6365 | African American, n = 568 | Hispanic, n = 512 | P Value | |
|---|---|---|---|---|
| Age, y [Median, IQR] | 60 [51, 70] | 57 [48, 65] | 57 [49, 68] | <0.001 |
| Male, No. (%) | 4384 (68.9) | 348 (61.3) | 357 (69.7) | <0.001 |
| Insurance, No. (%) | ||||
| No documented insurance | 796 (12.5) | 123 (21.7) | 127 (24.8) | <0.001 |
| Medicare | 1343 (21.1) | 100 (17.6) | 91 (17.7) | |
| Medicaid | 240 (3.8) | 74 (13.0) | 52 (10.2) | |
| Other | 3476 (54.6) | 244 (43.0) | 211 (41.2) | |
| Missing | 510 (8.0) | 27 (4.8) | 31 (6.1) | |
| No past medical history, No. (%) | 1204 (19.5) | 72 (13.0) | 102 (20.2) | <0.001 |
| Chronic/recurrent atrial fibrillation, No. (%) | 181 (2.9) | 8 (1.4) | 8 (1.6) | 0.03 |
| COPD/asthma, No. (%) | 540 (8.7) | 39 (7.0) | 25 (5.0) | <0.001 |
| Diabetes, No. (%) | 1155 (18.7) | 150 (27.0) | 178 (35.3) | <0.001 |
| Hyperlipidemia, No. (%) | 2919 (47.3) | 223 (40.1) | 231 (45.8) | 0.01 |
| Hypertension, No. (%) | 3462 (56.0) | 403 (72.5) | 277 (55.0) | <0.001 |
| Peripheral vascular disease, No. (%) | 273 (4.4) | 14 (2.5) | 21 (4.2) | 0.10 |
| CVA/TIA, No. (%) | 279 (4.5) | 40 (7.2) | 22 (4.4) | 0.02 |
| Heart failure, No. (%) | 230 (3.7) | 39 (7.0) | 15 (3.0) | <0.001 |
| End‐stage renal disease, No. (%) | 25 (0.4) | 10 (1.8) | 6 (1.2) | <0.001 |
| Chronic kidney disease, No. (%) | 129 (2.1) | 22 (4.0) | 15 (3.0) | 0.01 |
| Coronary artery disease, No. (%) | 1417 (22.9) | 129 (23.2) | 98 (19.4) | 0.19 |
| Prior MI, No. (%) | 959 (15.5) | 125 (22.5) | 83 (16.5) | <0.001 |
| Prior PCI, No. (%) | 392 (6.4) | 36 (6.5) | 26 (5.2) | 0.56 |
| Prior CABG, No. (%) | 114 (1.9) | 6 (1.1) | 6 (1.2) | 0.26 |
| Smoking, No. (%) | 2843 (44.7) | 327 (57.6) | 208 (40.6) | <0.001 |
| BMI [Median, IQR], kg/m2 | 28.2 [25.1, 32.1] | 28.5 [25.0, 33.1] | 28.1 [25.3, 31.6] | 0.40 |
| LVEF [Median, IQR] | 49.0 [40.0, 55.0] | 50.0 [40.0, 60.0] | 50.0 [40.0, 59.0] | 0.001 |
| Hospital characteristics | ||||
| Number of beds [Median, IQR] | 400 [265, 581] | 523 [349, 700] | 330 [261, 460] | <0.001 |
| Academic hospital, No. (%) | 3581 (56.3) | 476 (83.8) | 307 (60.0) | <0.001 |
| Hospital with PCI, No. (%) | 5012 (78.7) | 506 (89.1) | 398 (77.7) | <0.001 |
| Hospital with heart surgery, No. (%) | 5342 (83.9) | 532 (93.7) | 420 (82.0) | <0.001 |
| Region, No. (%) | ||||
| West | 1340 (21.1) | 74 (13.0) | 347 (67.8) | <0.001 |
| South | 1795 (28.2) | 213 (37.5) | 83 (16.2) | |
| Midwest | 2157 (33.9) | 209 (36.8) | 40 (7.8) | |
| Northeast | 1073 (16.9) | 72 (12.7) | 42 (8.2) | |
Abbreviations: BMI, body mass index; CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; CVA/TIA, cerebrovascular accident/transient ischemic attack; MI, myocardial infarction; IQR, interquartile range; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention.
The median door‐to‐balloon time for the overall cohort was 74 minutes (IQR, 55–99). There were no differences in the median door‐to‐balloon time between groups: whites (74 minutes; IQR, 54–99), African Americans (77 minutes; IQR, 57–100), and Hispanics (75 minutes; IQR, 56–100) (P = 0.13) (Figure 1A). Among males, African Americans had a longer door‐to‐balloon time (78 minutes; IQR, 57–102) than whites (72 minutes; IQR, 53–96), and Hispanics (75 minutes; IQR, 56–99) (P = 0.01). Among females, there were no differences in median door‐to‐balloon time between whites (78 minutes; IQR, 57–105), African Americans (79 minutes; IQR, 56–97), and Hispanics (76 minutes; IQR, 57–98) (P = 0.79) (Figure 1B).
Figure 1.
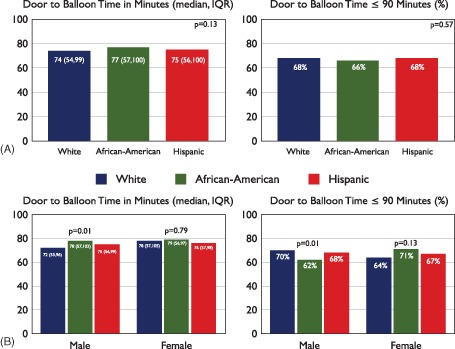
Door‐to‐balloon time and door‐to‐balloon time ≤ 90 minutes by race/ethnicity (A) and gender (B). Abbreviations: IQR, interquartile range.
In unadjusted linear regression models, African Americans were associated with a door‐to‐balloon time 7.5% longer than whites (estimate = 1.075; 95% CI: 1.010‐1.148) (P = 0.03). This association was not statistically significant after adjusting for potential confounders (estimate = 1.060; 95% CI: 0.996‐1.139) (P = 0.07). In similar models that evaluated sex specific differences, accounting for effect modification between race and gender, and adjusting for potential confounders, African American males had a door‐to‐balloon time that was 7.3% longer than white males (estimate = 1.073; 95% CI: 1.013‐1.137) (P = 0.02). There was no association with longer door‐to‐balloon time seen in African American females (estimate = 1.036; 95% CI: 0.929‐1.154) (P = 0.53). Hispanic ethnicity was associated with longer door‐to‐balloon time in both the unadjusted (estimate = 1.085; 95% CI: 1.011‐1.164) (P = 0.02) and adjusted (estimate = 1.089; 95% CI: 1.018‐1.164) (P = 0.01) linear regression models. After accounting for effect modification between race and gender, and adjusting for potential confounders, Hispanic males were associated with longer door‐to‐balloon time when compared with white males (estimate = 1.107; 95% CI: 1.022‐1.198) (P = 0.01). However, Hispanic females were not associated with longer door‐to‐balloon time when compared with white females (estimate = 1.038; 95% CI: 0.929‐1.160) (P = 0.51) (Table 2, Supplementary Table 1).
Table 2.
Effect of Age and Gender on Door‐to‐Balloon Time
| Exponentiated Regression Coefficient | 95% Lower CI | 95% Upper CI | P Value | |
|---|---|---|---|---|
| Unadjusted model | ||||
| Race/ethnicity | ||||
| African American | 1.075 | 1.006 | 1.148 | 0.03 |
| Hispanic | 1.085 | 1.011 | 1.16 | 0.02 |
| Gender | ||||
| Female | 1.103 | 1.071 | 1.137 | <0.001 |
| Unadjusted model including interaction for gender and race | 0.64a | |||
| Male | ||||
| African American | 1.078 | 1.015 | 1.146 | 0.02 |
| Hispanic | 1.101 | 1.013 | 1.196 | 0.02 |
| Female | ||||
| African American | 1.046 | 0.936 | 1.170 | 0.43 |
| Hispanic | 1.049 | 0.940 | 1.171 | 0.39 |
| Adjusted modelb | ||||
| African American | 1.060 | 0.996 | 1.129 | 0.07 |
| Hispanic | 1.089 | 1.018 | 1.164 | 0.01 |
| Female | 1.089 | 1.059 | 1.120 | <0.001 |
| Adjusted model including interaction for gender and race | 0.48a | |||
| Male | ||||
| African American | 1.073 | 1.013 | 1.137 | 0.02 |
| Hispanic | 1.107 | 1.022 | 1.198 | 0.01 |
| Female | ||||
| African American | 1.036 | 0.929 | 1.154 | 0.53 |
| Hispanic | 1.038 | 0.929 | 1.160 | 0.51 |
Abbreviations: CI, confidence interval.
The exponentiated regression coefficient represents the ratio between the geometric mean in the group under consideration and in the reference group. Reference group for race/ethnicity is white race. Reference group for gender is male.
P value for the interaction of gender and race. All P values are computed using the Wald test.
Adjusted models include: chronic obstructive pulmonary disease or asthma, diabetes (combined), hyperlipidemia, hypertension, heart failure, prior myocardial infarction, peripheral vascular disease, renal insufficiency, smoking, calendar time, hospital characteristics (teaching hospital, number of hospital beds, region), insurance (Medicare, Medicaid, none, or other).
The overall proportion of patients who achieved a door‐to‐balloon time ≤90 minutes was 68%. No differences in the proportion of patients achieving a door‐to‐balloon time ≤90 minutes were seen among the different groups: whites (68.0%), African Americans (65.9%), and Hispanics (67.8%) (P = 0.57) (Figure 2). Among males undergoing primary PCI, there were a lower proportion of African Americans who achieved door‐to‐balloon time ≤90 minutes (62.4%) as compared with whites (70.1%) and Hispanics (68.1%) (P = 0.01).
Figure 2.
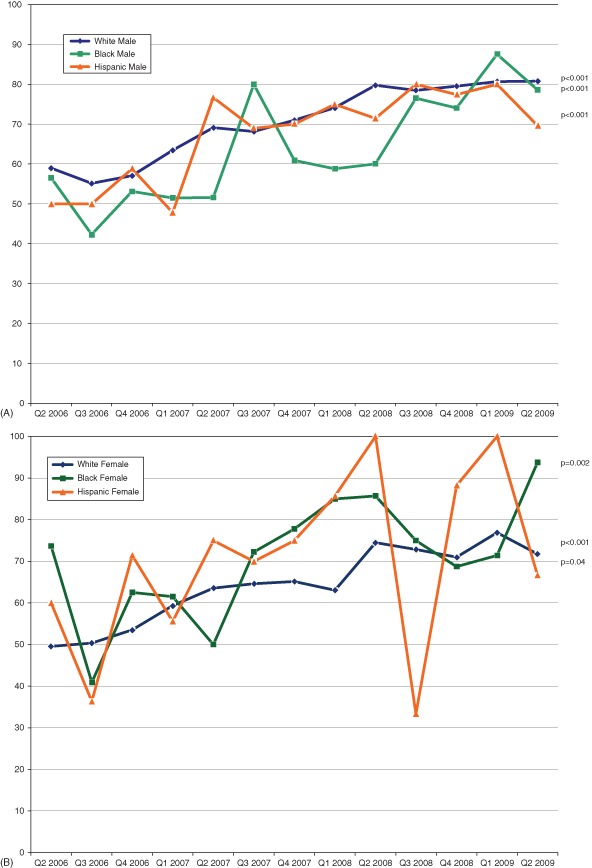
Trends in proportion of patients achieving a door‐to‐balloon time of ≤ 90 minutes in males (A) and females (B). P values are Cochran‐Armitage trend test. Abbreviations: Q, quarter.
In adjusted models that controlled for baseline and hospital characteristics, insurance status, race‐gender interaction, and time, African American males were associated with a lower odds of achieving a door‐to‐balloon time ≤90 minutes as compared with white males (odds ratio [OR]: 0.66; 95% CI: 0.55‐0.80) (P < 0.001) (Table 3). This relationship was not found in African American females (OR: 1.27; 95% CI: 0.96‐1.68) (P = 0.09) (P value for gender interaction <0.001). There was no association between Hispanic ethnicity and door‐to‐balloon time ≤90 minutes.
Table 3.
Unadjusted and Adjusted Odds of a Door‐to‐Balloon Time ≤90 Minutes
| Odds Ratio (95% CI) | P Value (Wald Test) | |
|---|---|---|
| Unadjusted | ||
| African American | 0.85 (0.73‐1.00) | 0.06 |
| Hispanic | 0.97 (0.77‐1.23) | 0.80 |
| Adjusted for baseline characteristicsa | ||
| African American | 0.86 (0.72‐1.01) | 0.07 |
| Hispanic | 0.99 (0.78‐1.25) | 0.92 |
| Adjusted for baseline characteristics plus race and gender interactionb | ||
| Male | < 0.001c | |
| African American | 0.69 (0.57‐0.83) | <0.001 |
| Hispanic | 0.92 (0.69‐1.22) | 0.54 |
| Female | ||
| African American | 1.27 (0.96‐1.67) | 0.09 |
| Hispanic | 1.21 (0.90‐1.63) | 0.21 |
| Adjusted for baseline and hospital characteristicsd | ||
| African American | 0.83 (0.70‐0.99) | 0.03 |
| Hispanic | 0.97 (0.76‐1.23) | 0.81 |
| Adjusted for baseline and hospital characteristics plus insurance statuse | ||
| African American | 0.84 (0.70‐0.99) | 0.04 |
| Hispanic | 0.98 (0.77‐1.25) | 0.88 |
| Adjusted for baseline and hospital characteristics, insurance status, calendar time plus race and gender interactionf | ||
| Male | <0.001c | |
| African American | 0.66 (0.55‐0.80) | <0.001 |
| Hispanic | 0.88 (0.66‐1.17) | 0.38 |
| Female | ||
| African American | 1.27 (0.96‐1.68) | 0.09 |
| Hispanic | 1.25 (0.93‐1.67) | 0.14 |
Abbreviations: CI, confidence interval.
Reference group = white.
Adjusted for age, gender, BMI, chronic obstructive pulmonary disease (COPD) or asthma, diabetes (combined), hyperlipidemia, hypertension, heart failure, prior myocardial infarction (MI), peripheral vascular disease (PVD), renal insufficiency, smoking.
Adjusted for age, gender, BMI, COPD or asthma, diabetes (combined), hyperlipidemia, hypertension, heart failure, prior MI, PVD, renal insufficiency, smoking, race*gender.
p‐value for interaction of race and gender.
Adjusted for age, gender, BMI, COPD or asthma, diabetes (combined), hyperlipidemia, hypertension, heart failure, prior MI, PVD, renal insufficiency, smoking, hospital characteristics (teaching hospital, number of hospital beds, region).
Adjusted for age, gender, BMI, COPD or asthma, diabetes (combined), hyperlipidemia, hypertension, heart failure, prior MI, PVD, renal insufficiency, smoking, hospital characteristics (teaching hospital, number of hospital beds, region), insurance (Medicare, Medicaid, none, or other).
Adjusted for age, gender, BMI, COPD or asthma, diabetes (combined), hyperlipidemia, hypertension, heart failure, prior MI, PVD, renal insufficiency, smoking, hospital characteristics (teaching hospital, number of hospital beds, region), insurance (Medicare, Medicaid, none, or other), race*gender interaction term.
[Corrections made to this Table after initial online publication].
The median door‐to‐balloon time for the overall cohort decreased over the study period from 82 minutes to 68 minutes. Decreases in median door‐to‐balloon time were also seen for each race/ethnicity in both males and females (Supplementary Table 2). The proportion of patients achieving a door‐to‐balloon time ≤90 minutes increased over time. These improvements were statistically significant and were seen across all racial, ethnic, and sex groups (Figure 2). Among African American males, the proportion achieving a door‐to‐balloon time ≤90 minutes increased from 56.5% to 78.6% (p < 0.001). Similar trends were seen in Hispanic and white subjects. There were equitable improvements for both males and females in white, African American and Hispanic groups in achieving a door‐to‐balloon time ≤90 minutes, which was present even after adjusting for potential confounders (Supplementary Table 3).
In‐hospital mortality for the overall cohort was low (3.8%, n = 273). There were no significant unadjusted differences seen between whites (3.8%), African Americans (3.0%), and Hispanics (4.1%) (P = 0.62) (Supplementary Figure 2) or associations between race/ethnicity and in‐hospital mortality after adjusting for potential differences in the patient populations (Supplementary Table 4).
Discussion
Small differences in door‐to‐balloon time and achieving a door‐to‐balloon time ≤90 minute persist between different racial and ethnic groups in GWTG‐CAD. We found no overall differences in door‐to‐balloon time, the proportion of patients achieving a door‐to‐balloon time ≤90 minutes, or in‐hospital mortality between patients of different race/ethnicity. After controlling for potential confounders, African Americans were associated with lower odds of achieving a door‐to‐balloon time ≤90 minutes and a relative 7.5% increase in door‐to‐balloon time, whereas Hispanic ethnicity was associated with a relative 8.9% increase in door‐to‐balloon time. When controlling for effect modification between gender and race/ethnicity, African American and Hispanic males, but not females, were associated with longer door‐to‐balloon time. These differences do not appear to be driven by race alone, because there are sex‐based differences in door‐to‐balloon time. In addition, we found the proportion of patients achieving a door‐to‐balloon time ≤90 minutes has substantially increased over time for all patients irrespective of race/ethnicity, and there were no differences in in‐hospital mortality.
Our study builds upon prior work showing that significant differences exist in door‐to‐balloon time between patients of different race/ethnicity.4, 5, 13, 17 We found that despite recent quality improvement initiatives such as the D2B Alliance and other quality improvement initiatives,18 the proportion of patients who achieved a door‐to‐balloon time within the 90‐minute time frame recommended by the ACC/AHA increased from 56% at the onset of the study to 78% by the second quarter of 2009. Furthermore, we found that the proportion of patients with a door‐to‐balloon time of ≤90 minutes increased for all patients irrespective of race/ethnicity. Each racial/ethnic group demonstrated improvements over time that was independent of any differences in patient and hospital characteristics. These improvements seen within the hospitals participating in the GWTG program are clinically meaningful and illustrate that dedicated quality improvement initiatives with specific aims, such as reducing disparities in door‐to‐balloon time, can improve care processes and quality indicators for all patients, irrespective of race/ethnicity.12, 17, 19
Our study does identify areas in need of further investigation. We found that African American race was associated with lower odds of achieving a door‐to‐balloon time ≤ 90 minutes. When studying this finding in more depth, we found that this relationship was driven by gender specific differences. African American males had 34% lower odds of achieving a door‐to‐balloon time ≤90 minutes; but this association was not present in African American females. A similar relationship was seen among Hispanic males who were associated with a relative 10.7% increase in the adjusted median door‐to‐balloon time, whereas there was no difference seen among females. Prior work has shown that door‐to‐balloon time is largely dependent on the time from presentation to catheterization lab activation rather than the time from activation to reperfusion. The differences in door‐to‐balloon time that we found among males of African American and Hispanic race/ethnicity suggest something unique about the presentation or treatment of this population that results in a longer door‐to‐balloon times. The mechanism and factors that drive this observation are in need of further study.
Our findings should be interpreted within the context of limitations of our analysis. Race/ethnicity was self‐reported and does not account for the multicultural background increasingly common in the United States. Socioeconomic differences are an important component of the study of racial/ethnic disparities; yet, we did not have the ability to control for this difference. Door‐to‐balloon time is self‐reported by the sites and is not independently adjudicated. Finally, our analysis was limited to hospitals in the GWTG registry. Although this provides an opportunity to study the effects of a quality improvement initiative on disparities, this may result in selection bias, because participation is voluntary and selects those hospitals most interested in quality improvement. Therefore, the results of our study do not necessarily reflect the findings at hospitals outside the GWTG program.
Conclusion
We found that even though substantial improvements have been made in all racial/ethnic groups in door‐to‐balloon time or door‐to‐balloon time ≤90 minutes, small differences by race/ethnicity persist among hospitals participating in the GWTG‐CAD program. African American race continues to be associated with slightly less likelihood of achieving revascularization within the recommended timeframe, whereas both African American and Hispanic patients are associated with longer door‐to‐balloon time after adjusting for potential confounders. It appears that these associations may be the result of individual patient factors other than race, because the association was seen among African American and Hispanic males but not females. The sex‐specific differences seen in door‐to‐balloon time demonstrate the need for further studies evaluating the mechanisms behind these associations. Yet, the significant improvements over time in door‐to‐balloon time for each race/ethnic group that we have found provide evidence that quality improvement initiatives are associated with improvements in care for all patients irrespective of race/ethnicity.
Supporting information
– Geometric Means of Door to Balloon Time in Whites, African‐American and Hispanic Patients
SupplementaryTable 2—Median door‐to‐balloon time per quarter
– Odds achieving door‐to‐balloon time ≥ 90 minutes for over time per 1 year increase in admission date*
– Unadjusted and Adjusted Odds of In‐hospital Mortality (reference group = White)
Study Flow
In‐hospital mortality by Race/Ethnicity
Dr. Fonarow is an advisor for Novartis. Dr. Cannon receives research grants from Accumetrics, AstraZeneca, GlaxoSmithKline, Merck, and Takeda. Dr. Peacock serves on the scientific advisory board of Abbott, Alere, Lily, and The Medicines Company. He receives research grants from Alere, Brahms, Novartis, and The Medicines Company. He serves on the speaker's bureau for Abbott, Alere, and EKR. He has ownership interest in Comprehensive Research Associates, Vital Sensors, and Emergencies in Medicine. Dr. Schwamm serves as chair of the national steering committee for GWTG (unpaid). Dr. Bhatt discloses the following relationships: advisory board: Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; board of directors: Boston VA Research Institute, Society of Cardiovascular Patient Care; chair: American Heart Association Get With The Guidelines Steering Committee; honoraria: American College of Cardiology (Editor, Clinical Trials, Cardiosource), Belvoir Publications (Editor‐in‐Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), Population Health Research Institute (clinical trial steering committee), Slack Publications (Chief Medical Editor, Cardiology Today's Intervention), WebMD (CME steering committees); other: Senior Associate Editor, Journal of Invasive Cardiology; data monitoring committees: Duke Clinical Research Institute; Mayo Clinic; Population Health Research Institute; research grants: Amarin, AstraZeneca, Bristol‐Myers Squibb, Eisai, Ethicon, Medtronic, sanofi‐aventis, The Medicines Company; unfunded research: FlowCo, PLx Pharma, Takeda.
This work was supported by a young investigator grant from the American Heart Association.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Stone GW, Dixon SR, Grines CL, et al. Predictors of infarct size after primary coronary angioplasty in acute myocardial infarction from pooled analysis from four contemporary trials. Am J Cardiol. 2007;100:1370–1375. [DOI] [PubMed] [Google Scholar]
- 2. Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: Is timing (almost) everything? Am J Cardiol. 2003;92:824–826. [DOI] [PubMed] [Google Scholar]
- 3. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction—Executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004;110:588–636. [DOI] [PubMed] [Google Scholar]
- 4. Bradley EH, Herrin J, Wang Y, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004;292:1563–1572. [DOI] [PubMed] [Google Scholar]
- 5. Cohen MG, Fonarow GC, Peterson ED, et al. Racial and ethnic differences in the treatment of acute myocardial infarction: findings from the Get With the Guidelines‐Coronary Artery Disease program. Circulation. 2010;121:2294–2301. [DOI] [PubMed] [Google Scholar]
- 6. Vaccarino V, Rathore SS, Wenger NK, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Guzman LA, Li S, Wang TY, et al. Differences in treatment patterns and outcomes between Hispanics and non‐Hispanic whites treated for ST‐segment elevation myocardial infarction: results from the NCDR ACTION Registry‐GWTG. J Am Coll Cardiol. 2012;59:630–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Skinner J, Chandra A, Staiger D, et al. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nallamothu BK, Krumholz HM, Peterson ED, et al. Door‐to‐balloon times in hospitals within the Get‐With‐The‐Guidelines registry after initiation of the door‐to‐balloon (D2B) Alliance. Am J Cardiol. 2009;103:1051–1055. [DOI] [PubMed] [Google Scholar]
- 10. LaBresh KA, Gliklich R, Liljestrand J, et al. Using “Get With The Guidelines” to improve cardiovascular secondary prevention. Jt Comm J Qual Saf. 2003;29:539–550. [DOI] [PubMed] [Google Scholar]
- 11. Moscucci M, Share D, Kline‐Rogers E, et al. The Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) collaborative quality improvement initiative in percutaneous coronary interventions. J Interv Cardiol. 2002;15:381–386. [DOI] [PubMed] [Google Scholar]
- 12. Krumholz HM, Herrin J, Miller LE, et al. Improvements in door‐to‐balloon time in the United States, 2005 to 2010. Circulation. 2011;124:1038–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Curtis JP, Herrin J, Bratzler DW, et al. Trends in race‐based differences in door‐to‐balloon times. Arch Intern Med. 2010;170:992–993. [DOI] [PubMed] [Google Scholar]
- 14. LaBresh KA, Ellrodt AG, Gliklich R, et al. Get with the guidelines for cardiovascular secondary prevention: pilot results. Arch Intern Med. 2004;164:203–209. [DOI] [PubMed] [Google Scholar]
- 15. Kumbhani DJ, Cannon CP, Fonarow GC, et al. Association of hospital primary angioplasty volume in ST‐segment elevation myocardial infarction with quality and outcomes. JAMA. 2009;302:2207–2213. [DOI] [PubMed] [Google Scholar]
- 16. Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- 17. Mehta RH, Bufalino VJ, Pan W, et al. Achieving rapid reperfusion with primary percutaneous coronary intervention remains a challenge: Insights from American Heart Association's Get With the Guidelines program. Am Heart J. 2008;155:1059–1067. [DOI] [PubMed] [Google Scholar]
- 18. Krumholz HM, Bradley EH, Nallamothu BK, et al. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door‐to‐Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008;1:97–104. [DOI] [PubMed] [Google Scholar]
- 19. Flynn A, Moscucci M, Share D, et al. Trends in door‐to‐balloon time and mortality in patients with ST‐elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Intern Med. 2010;170:1842–1849. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
– Geometric Means of Door to Balloon Time in Whites, African‐American and Hispanic Patients
SupplementaryTable 2—Median door‐to‐balloon time per quarter
– Odds achieving door‐to‐balloon time ≥ 90 minutes for over time per 1 year increase in admission date*
– Unadjusted and Adjusted Odds of In‐hospital Mortality (reference group = White)
Study Flow
In‐hospital mortality by Race/Ethnicity


