ABSTRACT
Coronary artery development is a delicate, complex, and finely tuned process that includes multiple interactions among many pathways, especially in the pericardium and the developing myocardium. There still exists some controversy on the exact origin of certain cellular components. Nevertheless, an understanding of this extremely important developmental process is paramount in identifying some of the causes of anomalous coronary development. There are different patterns of anomalous coronary arteries, with variable risk of myocardial ischemia, malignant arrhythmias, and sudden cardiac death. These anomalies can be broadly categorized into 2 basic anatomic subsets: those with origin of the anomalous coronary artery from the opposite aortic sinus, and those with origin of the anomalous coronary artery from the pulmonary artery. Diagnosis and management of such patterns continues to be challenging. A good knowledge of the normal and abnormal coronary artery development could potentially help us explore new avenues in the treatment of ischemic heart disease as well as anomalous coronary arteries.
Overview of Embryonic Coronary Artery Development
Coronary artery disease is a major source of morbidity and mortality in the world. Congenital coronary artery anomalies, although less prevalent, are a potential cause for malignant arrhythmias, myocardial ischemia, and myocardial dysfunction.1 An understanding of the process of coronary artery formation during development could potentially advance treatments, including potential coronary artery regeneration. The origins and mechanisms of coronary vessel development are not fully understood; however, a growing body of literature is emerging on this topic. From an evolutionary standpoint, the coronary arterial system evolved to supply the thick‐walled myocardium, which cannot be appropriately supplied with oxygen and nutrients by simple diffusion from the heart lumen, as is the case in invertebrate animals and fish. Before 1989, it was generally believed that coronary arteries and veins developed from outgrowths from the aorta and the systemic venous sinus, respectively. However, in a study by Bogers et al, coronary arteries were identified even before the presence of coronary arterial orifices, which led to the novel concept of ingrowth instead of outgrowth of the coronary arterial vasculature.2
Epicardium (historically seen as part of the pericardium and referred to as “visceral pericardium”) is essential for coronary vessel development.3 The term epimyocardium has been used, implying that the epicardium and myocardium may have a common origin. This theory was challenged as early as 1909 by Kurkiewicz et al, but only recently has the separate origin of the visceral pericardium and myocardium become widely accepted.4 The epicardium originates from an extracardiac structure, the proepicardium, which is located near the venous pole of the heart above the liver primordium (Figure 1).5 Epicardial cells form a sheet of single cells that surround the heart and are necessary for coronary vessel formation. An elaborate interaction of epicardial cells with myocardial cells leads to the transformation of epicardial cells into mesenchymal cells, as precursors of building blocks of coronary vessels.6 Interestingly, hematopoietic progenitor cells also play an important role in the transformation of epicardial into mesenchymal cells (Lluri et al, unpublished data, 2013). In humans, at about the 25th embryonic day, vessel‐like structures are observed in the space between the epicardium and myocardium. However, it should be emphasized that at this point there is no blood flow in these vessel‐like structures, which are not necessarily contiguous. In a matter of days, these structures fuse to form a vascular plexus. This diffuse elaborate vascular network ultimately contacts and penetrates the aortic root, leading to abrupt exposure to systemic pressure and high flow (Figure 2). These changes result in the maturation of these vessels, including migration of smooth‐muscle cells, proper arrangement of these cells, growth of some vessels, and regression of others through apoptosis. Any abnormalities during this delicate, well‐controlled process may lead to congenital coronary artery anomalies.
Figure 1.
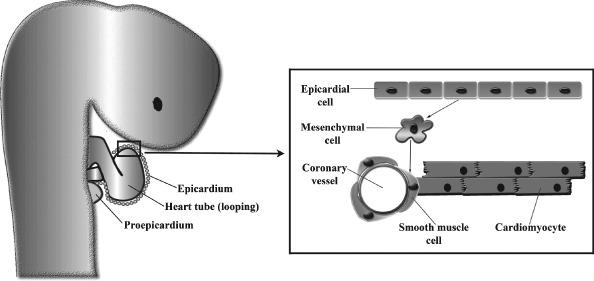
Epicardium and coronary artery development.
Figure 2.
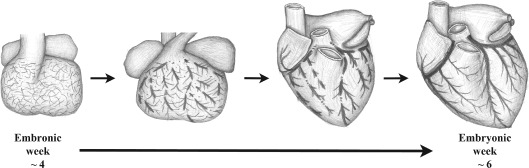
Development of coronary vessels during embryogenesis.
There are limited data on the molecular pathways involved in the formation of the coronary artery ostia. A high density of vascular endothelial growth factor (VEGF) receptors (VEGFR‐2 and VEGFR‐3) at the sites of coronary ostia underlies the importance of VEGF and its receptors in the process of coronary stem formation and penetration of the aorta.7 Furthermore, animal studies support the role of neural crest cells in the formation of coronary artery stems; experimental ablation of the neural crest cells results in a single coronary artery stem.8 In addition, a mutation to perlecan, a heparin sulfate proteoglycan expressed in the basement membrane during development, has been associated with anomalous origin of the coronary arteries.9 Interestingly, similar coronary anomalies occur with mutations to connexin43, a gap junction complex.10 Further characterization of these pathways may lead to a better understanding of the molecular signals responsible for the formation of anomalous coronary arteries.
Recent studies suggest that coronary arterial and venous vessel development originates from different endothelial embryonic cell populations, anatomically from different sites, and at different times11, 12 Although there is a growing body of knowledge dealing with coronary arterial development, there is a paucity of knowledge on the embryologic development of the cardiac venous system.
Coronary Artery Anomalies
Historically, coronary artery anomalies have been defined and described according to an elaborate anatomic classification system.13, 14 However, there has been a growing emphasis on categorization of coronary artery anomalies according to prognostic significance, specifically the increased risk of malignant arrhythmias and sudden cardiac death associated with certain subsets.1, 15 Clinically significant coronary arterial anomalies may be classified into 2 basic anatomic subsets: those with origin of the anomalous coronary artery from the opposite aortic sinus, and those with origin of the anomalous coronary artery from the pulmonary artery (PA). Anomalous coronary artery from the opposite sinus includes the right coronary artery (RCA) arising from the left sinus (ARCA) or the left coronary artery (LCA) arising from the right sinus. In this category, the most common finding is the left circumflex artery (LCX) arising from the right sinus (ALCX).16 This is followed by ARCA (Figure 3), and lastly the left main coronary artery (LM) arising from the right sinus (ALM; Figure 4). There are other unusual subsets, which include an anomalous left anterior descending artery (LAD) originating from the RCA (Figure 5), occasionally seen in tetralogy of Fallot and other congenital abnormalities.17 If the anomalous coronary artery courses in the sulcus between the PA and the aorta, which occurs in ALM, there is an increased risk of malignant arrhythmias and sudden death.18 The increased risk may be due to the intra‐arterial course of the anomalous coronary with resultant compression or the larger myocardial mass supplied by anomalies of this type. The presence of a slit‐like origin and intramural course of the proximal coronary artery arising from the contralateral sinus likely plays an important role in coronary ischemia and malignant arrhythmias.19, 20, 21 Anginal symptoms and malignant arrhythmias often occur with exercise and are likely caused by myocardial ischemia that may be due to any or all of the above factors.22 Surgical treatment traditionally has been performed for symptomatic patients, or those with evidence of stress‐induced ischemia or ventricular arrhythmias, and is considered standard of care for asymptomatic patients with ALM because of the increased risk of mortality in these patients. Various surgical techniques have been described, from coronary artery bypass grafting to unroofing of the proximal anomalous coronary to reimplantation of the affected coronary artery. Transcatheter interventional angioplasty and stenting is a potential alternative with good immediate results but limited long‐term data available.23 For patients who do not have ALM and who are truly asymptomatic and have no evidence of stress‐induced ischemia or stress‐induced arrhythmias, there is no clear consensus on management, as the risks of the coronary repair or stenting need to be weighed against the low risk of malignant arrhythmias or death. There may be a role for intravascular ultrasound and invasive fractional flow reserve and pressure measurement at rest and with pharmacologic stress or exercise in determining the hemodynamic significance of an anomalous coronary artery from the contralateral aortic sinus. The limited published case reports on the use of these more nuanced tools for coronary flow and pressure assessment are compelling.24, 25, 26, 27
Figure 3.
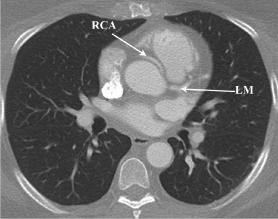
RCA arising from left sinus. Abbreviations: LM, left main coronary artery; RCA, right coronary artery.
Figure 4.
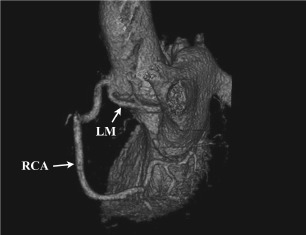
LM arising from right sinus. Abbreviations: LM, left main coronary artery; RCA, right coronary artery.
Figure 5.
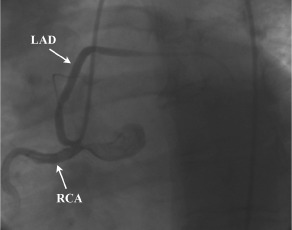
LAD arising from RCA. Abbreviations: LAD, left anterior descending artery; RCA, right coronary artery.
A coronary artery originating from the PA is much more rare, occurring in about 1 in 300 000 cases, more commonly involving the LCA originating from the main PA.15, 28 These patients often present early in life with signs of congestive heart failure, dilated cardiomyopathy, and mitral regurgitation. However, in the presence of a well‐developed collateral network and pulmonary hypertension, these patients may not be diagnosed until later in life. Nevertheless, surgical therapy is warranted in patients with such anomalies, emphasizing the need for a 2‐coronary system for improved survival.29 Various surgical approaches have been described, including reimplantation of the LCA into the aorta, bypass grafting and ligation of the origin at the PA, and baffling of the aorta to the ostium of the anomalous left coronary.30
In certain conditions, the anomaly is not at the origin of the arteries. Myocardial bridging, when a segment of the vessel enters the myocardium and courses for a variable length before reemerging back to the epicardium, was described as early as the 18th century, but its clinical significance was not understood until much later.31, 32 There has been a significant variation on the reporting of the frequency of myocardial bridging. When diagnosed clinically, the frequency ranges from 0.5% to 40%, and 15% to 85% when found at autopsy.33 This discrepancy suggests that not all myocardial bridges cause symptoms. However, when symptoms are present, usually they are secondary to ischemia.34 The most common vessel affected is the middle portion of the LAD artery; however, the RCA and LCX can also be affected.35 In addition to coronary angiography, newer techniques such as intravascular ultrasound can be used to detect not only the presence of myocardial bridging, but arterial‐wall morphology as well.36 Medical therapy, including β‐blockers or calcium channel blockers, is considered first‐line therapy for symptomatic patients. If patients continue to remain symptomatic despite medical therapy, supra‐arterial myotomy has been reported as an alternative.37 Stenting is an alternative as well; however, restenosis and stent fracture need to be taken into consideration when choosing this strategy.38, 39
Finally, a coronary fistula is an abnormal terminal connection between a coronary artery and any of the cardiac chambers or the great vessels. Krause reported coronary fistulas as early as 1865, but it was Maude Abbott in 1906 who described in detail the pathology of this condition.40 Congenital coronary artery fistulas represent 0.4% of all congenital heart defects.41 Furthermore, coronary artery fistulas may occur secondary to chest trauma or iatrogenic causes. Most commonly, congenital artery fistulas arise from the RCA and drain into the right heart chambers; those draining in the left ventricle or left atrium comprise 17% and 6%, respectively.42 Symptoms, including fatigue, shortness of breath, angina, and eventually congestive heart failure, may occur and are related to the size of the fistula and the resultant shunt. Symptoms typically occur in the adult population and are far less common in infants or children.43 Coronary angiography remains the gold standard for the diagnosis of coronary artery fistulas; however, electrocardiographically gated computed tomography angiography can readily and noninvasively identify these structures. Once diagnosed, the management remains a topic of controversy.44 Surgical intervention, first described in 1947 by Bjork and Crafoord, is recommended for symptomatic patients.45 Almost 40 years later, in 1983, the first successful transcatheter closure of a coronary fistula was performed.46 Since then, transcatheter closure has become an acceptable alternative to surgical repair in select patients.44 However, there is no clear consensus on the management of asymptomatic coronary fistulas, which are found incidentally. Some authors suggest that if asymptomatic coronary fistulas are hemodynamically significant, they should be closed at the time of diagnosis.47 Other groups advocate for intervention regardless of symptoms or hemodynamic findings, because of future possible complications.48
Conclusion
Coronary artery development is a delicate and finely tuned process that includes a complex interaction among the pericardium and myocardium, involving multiple cellular pathways and yet‐to‐be‐identified other factors. There has been a growing interest in the study of coronary artery development. Such an understanding is paramount in identifying some of the causes of anomalous coronary development. There are different patterns of anomalous coronary arteries, with variable risk of myocardial ischemia, malignant arrhythmias, and sudden cardiac death. A good understanding of this process could potentially help us explore new avenues in the treatment of ischemic heart disease as well as clinically relevant anomalous coronary arteries.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation. 2007;115:1296–1305. [DOI] [PubMed] [Google Scholar]
- 2. Bogers AJ, Gittenberger‐de Groot AC, Poelmann RE, et al. Development of the origin of the coronary arteries, a matter of ingrowth or outgrowth? Anat Embryol (Berl). 1989;180:437–441. [DOI] [PubMed] [Google Scholar]
- 3. Pérez‐Pomares JM, de la Pompa JL. Signaling during epicardium and coronary vessel development. Circ Res. 2011;109:1429–1442. [DOI] [PubMed] [Google Scholar]
- 4. Kirby ML. Cardiac Development Oxford and New York, NY: Oxford University Press; 2007. [Google Scholar]
- 5. Viragh S, Challice CE. The origin of the epicardium and the embryonic myocardial circulation in the mouse. Anat Rec. 1981;201:157–168. [DOI] [PubMed] [Google Scholar]
- 6. Olivey HE, Svensson EC. Epicardial‐myocardial signaling directing coronary vasculogenesis. Circ Res. 2010;106:818–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tomanek RJ, Holifield JS, Reiter RS, et al. Role of VEGF family members and receptors in coronary vessel formation. Dev Dyn. 2002;225:233–240. [DOI] [PubMed] [Google Scholar]
- 8. Hood LC, Rosenquist TH. Coronary artery development in the chick: origin and deployment of smooth muscle cells, and the effects of neural crest ablation. Anat Rec. 1992;234:291–300. [DOI] [PubMed] [Google Scholar]
- 9. González‐Iriarte M, Carmona R, Pérez‐Pomares JM, et al. Development of the coronary arteries in a murine model of transposition of great arteries. J Mol Cell Cardiol. 2003;35:795–802. [DOI] [PubMed] [Google Scholar]
- 10. Li WE, Waldo K, Linask KL, et al. An essential role for connexin43 gap junctions in mouse coronary artery development. Development. 2002;129:2031–2042. [DOI] [PubMed] [Google Scholar]
- 11. Wu B, Zhang Z, Lui W, et al. Endocardial cells form the coronary arteries by angiogenesis through myocardial‐endocardial VEGF signaling. Cell. 2012;151:1083–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Red‐Horse K, Ueno H, Weissman IL, et al. Coronary arteries form by developmental reprogramming of venous cells. Nature. 2010;464:549–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Roberts WC. Major anomalies of coronary arterial origin seen in adulthood. Am Heart J. 1986;111:941–963. [DOI] [PubMed] [Google Scholar]
- 14. Loukas M, Groat C, Khangura R, et al. The normal and abnormal anatomy of the coronary arteries. Clin Anat. 2009;22:114–128. [DOI] [PubMed] [Google Scholar]
- 15. Frommelt PC, Frommelt MA. Congenital coronary artery anomalies. Pediatr Clin North Am. 2004;51:1273–1288. [DOI] [PubMed] [Google Scholar]
- 16. Click RL, Holmes DR Jr, Vlietstra RE, et al. Anomalous coronary arteries: location, degree of atherosclerosis and effect on survival—a report from the Coronary Artery Surgery Study. J Am Coll Cardiol. 1989;13:531–537. [DOI] [PubMed] [Google Scholar]
- 17. Mawson JB. Congenital heart defects and coronary anatomy. Tex Heart Inst J. 2002;29:279–289. [PMC free article] [PubMed] [Google Scholar]
- 18. Taylor AJ, Rogan KM, Virmani R. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol. 1992;20:640–647. [DOI] [PubMed] [Google Scholar]
- 19. Liberthson RR, Dinsmore RE, Fallon JT. Aberrant coronary artery origin from the aorta: report of 18 patients, review of literature and delineation of natural history and management. Circulation. 1979;59:748–754. [DOI] [PubMed] [Google Scholar]
- 20. Roberts WC, Kragel AH. Anomalous origin of either the right or left main coronary artery from the aorta without coursing of the anomalistically arising artery between aorta and pulmonary trunk. Am J Cardiol. 1988;62:1263–1267. [DOI] [PubMed] [Google Scholar]
- 21. Angelini P, Velasco JA, Flamm S. Coronary anomalies: incidence, pathophysiology, and clinical relevance. Circulation. 2002;105:2449–2454. [DOI] [PubMed] [Google Scholar]
- 22. Cheitlin MD, MacGregor J. Congenital anomalies of coronary arteries: role in the pathogenesis of sudden cardiac death. Herz. 2009;34:268–279. [DOI] [PubMed] [Google Scholar]
- 23. Tejada JG, Hernandez F, Sanchez I, et al. Stenting of anomalous left main coronary artery arising from the right sinus of Valsalva: a case report. Int J Cardiol. 2007;119:266–267. [DOI] [PubMed] [Google Scholar]
- 24. Angelini P, Velasco JA, Ott D, et al. Anomalous coronary artery arising from the opposite sinus: descriptive features and pathophysiologic mechanisms, as documented by intravascular ultrasonography. J Invasive Cardiol. 2003;15:507–514. [PubMed] [Google Scholar]
- 25. Porto I, MacDonald ST, Selvanayagam JB, et al. Intravascular ultrasound to guide stenting of an anomalous right coronary artery coursing between the aorta and pulmonary artery. J Invasive Cardiol. 2005;17:E33–E36. [PubMed] [Google Scholar]
- 26. Schrale RG, Channon KM, Ormerod OJ. IVUS‐guided evaluation and percutaneous intervention in an anomalous left main coronary artery. J Invasive Cardiol. 2007;19:E195–E198. [PubMed] [Google Scholar]
- 27. Park K, Koo BK, Oh IY, et al. Two cases of anomalous origin of a right coronary artery: same anatomy, but different physiology. Can J Cardiol. 2011;27:263e29–263.e30. [DOI] [PubMed] [Google Scholar]
- 28. Wesselhoeft H, Fawcett JS, Johnson AL. Anomalous origin of the left coronary artery from the pulmonary trunk: its clinical spectrum, pathology, and pathophysiology, based on a review of 140 cases with seven further cases. Circulation. 1968;38:403–425. [DOI] [PubMed] [Google Scholar]
- 29. Schwartz ML, Jonas RA, Colan SD. Anomalous origin of left coronary artery from pulmonary artery: recovery of left ventricular function after dual coronary repair. J Am Coll Cardiol. 1997;30:547–553. [DOI] [PubMed] [Google Scholar]
- 30. Reul RM, Cooley DA, Hallman GL, et al. Surgical treatment of coronary artery anomalies: report of a 37½‐year experience at the Texas Heart Institute. Tex Heart Inst J. 2002;29:299–307. [PMC free article] [PubMed] [Google Scholar]
- 31. Geiringer E. The mural coronary. Am Heart J. 1951;41:359–368. [DOI] [PubMed] [Google Scholar]
- 32. Ferreira AG Jr, Trotter SE, Konig B Jr, et al. Myocardial bridges: morphological and functional aspects. Br Heart J. 1991;66:364–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Loukas M, Von Kriegenbergh K, Gilkes M, et al. Myocardial bridges: a review. Clin Anat. 2011;24:675–683. [DOI] [PubMed] [Google Scholar]
- 34. Mohlenkamp S, Hort W, Ge J, et al. Update on myocardial bridging. Circulation. 2002;106:2616–2622. [DOI] [PubMed] [Google Scholar]
- 35. Kayalar N, Burkhart HM, Dearani JA, et al. Congenital coronary anomalies and surgical treatment. Congenit Heart Dis. 2009;4:239–251. [DOI] [PubMed] [Google Scholar]
- 36. Ge J, Erbel R, Gorge G, et al. High wall shear stress proximal to myocardial bridging and atherosclerosis: intracoronary ultrasound and pressure measurements. Br Heart J. 1995;73:462–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Huang XH, Wang SY, Xu JP, et al. Surgical outcome and clinical follow‐up in patients with symptomatic myocardial bridging. Chin Med J (Engl). 2007;120:1563–1566. [PubMed] [Google Scholar]
- 38. Tandar A, Whisenant BK, Michaels AD. Stent fracture following stenting of a myocardial bridge: report of two cases. Catheter Cardiovasc Interv. 2008;71:191–196. [DOI] [PubMed] [Google Scholar]
- 39. Haager PK, Schwarz ER, vom Dahl J, et al. Long term angiographic and clinical follow up in patients with stent implantation for symptomatic myocardial bridging. Heart. 2000;84:403–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Luo L, Kebede S, Wu S, et al. Coronary artery fistulae. Am J Med Sci. 2006;332:79–84. [DOI] [PubMed] [Google Scholar]
- 41. Burch GH, Sahn DJ. Congenital coronary artery anomalies: the pediatric perspective. Coron Artery Dis. 2001;12:605–616. [DOI] [PubMed] [Google Scholar]
- 42. Hobbs RE, Millit HD, Raghavan PV, et al. Coronary artery fistulae: a 10‐year review. Cleve Clin Q. 1982;49:191–197. [DOI] [PubMed] [Google Scholar]
- 43. Liberthson RR, Sagar K, Berkoben JP, et al. Congenital coronary arteriovenous fistula: report of 13 patients, review of the literature and delineation of management. Circulation. 1979;59:849–854. [DOI] [PubMed] [Google Scholar]
- 44. Mangukia CV. Coronary artery fistula. Ann Thorac Surg. 2012;93:2084–2092. [DOI] [PubMed] [Google Scholar]
- 45. Biorck G, Crafoord C. Arteriovenous aneurysm on the pulmonary artery simulating patent ductus arteriosus botalli. Thorax. 1947;2:65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Reidy JF, Sowton E, Ross DN. Transcatheter occlusion of coronary to bronchial anastomosis by detachable balloon combined with coronary angioplasty at same procedure. Br Heart J. 1983;49:284–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Schumacher G, Roithmaier A, Lorenz HP, et al. Congenital coronary artery fistula in infancy and childhood: diagnostic and therapeutic aspects. Thorac Cardiovasc Surg. 1997;45:287–294. [DOI] [PubMed] [Google Scholar]
- 48. Kamiya H, Yasuda T, Nagamine H, et al. Surgical treatment of congenital coronary artery fistulas: 27 years' experience and a review of the literature. J Card Surg. 2002;17:173–177. [DOI] [PubMed] [Google Scholar]


