ABSTRACT
Background
Appropriate use criteria (AUC) for single‐photon emission computed tomographic myocardial perfusion imaging (SPECT MPI) were revised in 2009 to include 15 new clinical scenarios. We assessed multivariable predictors and overall appropriateness of MPI studies performed in a rural tertiary care setting.
Hypothesis
We hypothesized that appropriate utilization rates of SPECT MPI imaging in a rural tertiary care center are similar for cardiology and non cardiology providers.
Methods
We reviewed all SPECT MPI studies performed for over a 6‐month period at our center. Using 67 scenarios in AUC, we categorized these studies as appropriate, inappropriate, uncertain, or unclassifiable.
Results
Of 328 MPI studies, 287 (88%) studies were classified as appropriate, 18 (5.5%) as inappropriate, 23 (7%) as uncertain, and none as unclassifiable. Preoperative testing accounted for 44% of the inappropriate studies; 61% of uncertain tests were ordered for cardiovascular risk assessment in patients with prior normal coronary angiography or normal stress tests. The ordering provider specialty did not show any relation with appropriateness of the test (P = 0.46). Patients with inappropriate and uncertain studies were younger than patients with appropriate studies (P = 0.007).
Conclusions
We found that a majority of MPI studies are performed for appropriate indications regardless of ordering provider specialty. Few common scenarios accounted for the majority of the inappropriate or uncertain studies.
Background
Previous investigators have reported a significant increase in the utilization of imaging studies in cardiovascular medicine, disproportionate to the prevalence of cardiovascular disease.1 As a result, utilization of imaging studies is now being closely scrutinized by the healthcare payers, often necessitating preauthorization. The Deficit Reduction Act of 2005 implemented a new cap system for reimbursement of imaging studies, which includes cardiac radionuclide imaging and echocardiography.2
In an attempt to improve appropriate cardiac imaging utilization, appropriateness use criteria (AUC) for single‐photon emission computed tomographic myocardial perfusion imaging (SPECT MPI) were first published in 2005.3 Since this publication, the applicability of AUC has been evaluated in various settings.4, 5, 6, 7, 8, 9, 10 Previous studies have pointed out limitations in AUC published in 2005, such as inadequate number of clinical scenarios, resulting in 9% to 11% of patients having tests for unclassifiable indications.4 With the availability of new clinical data, AUC were revised in 2009.11 Few studies have evaluated the applicability of 2009 AUC in clinical practice.10
The purpose of this study was 3‐fold: (1) to evaluate the rates of appropriate utilization of MPI studies done in a rural tertiary health care system, (2) to assess the relation between the specialty of the ordering provider (cardiologist vs noncardiologist) and appropriateness of the indication, (3) to assess the most common scenarios constituting inappropriate or uncertain indications.
Methods
Study Design
This observational study was conducted at the Guthrie Health System/Robert Packer Hospital, an integrated healthcare system in rural northern Pennsylvania and western New York. Through a network of outreach offices, this healthcare system provides primary and specialty care to patients from Bradford, Sullivan, Tioga, Wyoming, and Lycoming counties in Pennsylvania, all of which are designated as rural counties by the Pennsylvania Office of Rural Health.12 This network also serves populations in the Chemung, Schuyler, Tompkins, and Tioga counties in New York State, designated as rural counties based on census places (all areas outside census places with 50,000 or more people).13 We evaluated all consecutive MPI studies performed between April 2011 and September 2011 (N = 328) at our center. We collected baseline demographic and clinical information such as age, sex, comorbidities, history of coronary artery disease or equivalents, and prior stress test results. We also collected follow‐up information on patients with inappropriate and uncertain studies, who underwent further testing such as cardiac catheterization or revascularization. This study was approved by institutional review board.
Outcomes
The primary study outcome was the overall rate of appropriate, inappropriate, uncertain, and unclassifiable indication for the MPI studies. The secondary analysis included relation of the specialty of ordering provider with appropriateness, most common indications for these studies, and the multivariable predictors of inappropriate studies.
Classification of MPI Studies
Board‐certified radiologists or cardiologists reported MPI studies as part of their patients' routine clinical care, independent of and prior to the design of this analysis. MS, PD, and DHJ were involved in the classification process. All studies classified as inappropriate or uncertain as per AUC were again reviewed by MS and DHJ. However, we did not formally assess interobserver agreement. We classified the MPI studies into 4 groups based on 67 clinical scenarios provided in the 2009 AUC publication11: appropriate, inappropriate, uncertain, and unclassifiable. The 2009 AUC document describes 67 unique clinical scenarios for SPECT MPI studies. Of these, 33 scenarios are considered as appropriate indications for ordering SPECT study, whereas 25 scenarios are considered inappropriate and 9 scenarios are considered to have an uncertain clinical indication for MPI. Ordering providers were classified in 2 categories, cardiologists and noncardiologists. Studies ordered by residents, fellows, physician assistants, and nurse practitioners were categorized according to the specialty of the supervising physician. For application of indications, we used the flowchart (algorithm for using tables according to hierarchy of application)11 provided in AUC documents to avoid classifying patients in more than 1 category. For multivariable analysis, relevant clinical variables were tested in the regression model. These clinical variables included age, gender, hypertension, history of coronary artery disease, peripheral vascular disease, abdominal aortic aneurysm, cerebrovascular accident, and specialty of the ordering provider.
Statistical Analysis
Baseline characteristics are described as mean ± 1 standard deviation for continuous variables and percentages for categorical variables. We performed multivariable analysis to assess predictors of inappropriate or uncertain studies and to estimate the independent impact of ordering‐provider specialty on level of appropriateness. Multivariable analysis was performed using backward stepwise variable selection. Variables were dropped from the multivariable model if they did not show a significant relation with the level of appropriateness, except for the variable relating to provider specialty, which was kept in the model irrespective of its significance. Statistical analysis was performed using Statview version 5.0 (SAS Institute, Cary, NC).
Results
Overall Appropriateness
The results of appropriateness analysis are shown in Figure 1. Of the 328 studies, 245 (75%) were ordered in the outpatient setting and 83 (25%) in the inpatient setting. Two hundred eighty‐seven (88%) studies were classified as appropriate, whereas 18 (5.5%) and 23 (7%) were classified as inappropriate and uncertain, respectively. No study was deemed unclassifiable.
Figure 1.
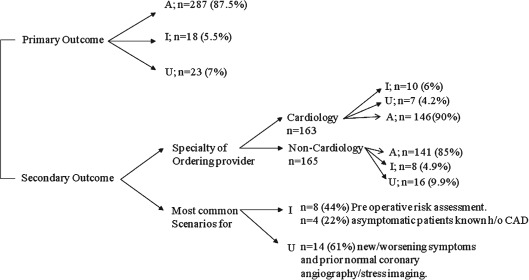
A total of 328 Studies were included in the analysis. Of these studies, 287 (87.5%) were classified as appropriate (A), whereas 18 (5.5%) and 23 (7%) were classified as inappropriate (I) and uncertain (U), respectively. No study was deemed unclassifiable. Abbreviations: CAD, coronary artery disease.
Predictors of Inappropriate and Uncertain Studies
Baseline characteristics of the 3 groups are presented in Table 1. Patients with appropriate tests were similar to those with not appropriate (uncertain and inappropriate) studies, except for older age (68 vs 60 years, P < 0.0001) and higher prevalence of coronary artery disease (CAD) (40% vs 27%, P = 0.046). There were similar rates of appropriate studies regardless of practice setting (outpatient vs inpatient setting, 73 (88%) and 214 (87%), respectively, P = 0.885). In multivariable logistic regression analysis (which included CAD, age, ordering provider); only age remained a significant predictor of appropriateness of the studies (P = 0.0007). Younger patients were more likely to have studies ordered for either inappropriate or uncertain indications.
Table 1.
Baseline Clinical Characteristics
| All Studies, N = 328 | Appropriate, N = 287 | Inappropriate, N = 18 | Uncertain, N = 23 | P Valuea | |
|---|---|---|---|---|---|
| Mean age, y | 67 | 68 | 61 | 59 | <0.0001 |
| Sex, female | 145 (44%) | 131 (46%) | 8 (44%) | 6 (26%) | 0.165 |
| Hypertension | 262 (80%) | 234 (82%) | 11 (61%) | 17 (74%) | 0.228 |
| Hyperlipidemia | 213 (65%) | 187 (65%) | 9 (50%) | 17 (74%) | 0.630 |
| Average BMI, kg/m2 | 31.28 | 30.77 | 29.62 | 33.45 | 0.672 |
| Current smokers | 45 (14%) | 38 (13%) | 0 | 7 (30%) | 0.715 |
| Coronary artery disease | 125 (38%) | 114 (40%) | 5 (28%) | 6 (26%) | 0.046 |
| Diabetes mellitus requiring treatment | 109 (33%) | 95 (33%) | 6 (33%) | 8 (35%) | 0.502 |
| Abdominal aortic aneurysm | 14 (4%) | 11 (3.8%) | 3 (17%) | 0 | 0.305 |
| Cerebrovascular disease | 29 (8.8%) | 28 (9.8%) | 0 | 1 (4.3%) | 0.122 |
| Peripheral vascular disease | 28 (8.5%) | 24 (8.4%) | 3 (17%) | 1 (4.3%) | 0.820 |
Abbreviations: BMI, body mass index.
Data are presented as n (%).
P value for appropriate vs not appropriate (uncertain and inappropriate studies).
Specialty of Ordering Provider
Figure 2 shows appropriateness of the studies according to the specialty of ordering provider. A majority of the noncardiologist providers were either primary care physicians or hospitalists. Cardiology providers ordered a total of 163 studies, whereas noncardiology providers ordered 165 studies. Of the 163 studies ordered by cardiologists, 146 (90%) were classified as appropriate, and 10 (6%) and 7 (4.2%) were classified as inappropriate and uncertain, respectively. Of the 165 studies ordered by noncardiologists, 141 (85%) were classified as appropriate, and 8 (4.9%) and 16 (9.9%) were classified as inappropriate and uncertain, respectively. The specialty of ordering provider did not show a univariable or multivariable correlation with the appropriateness of the tests (P = 0.46).
Figure 2.
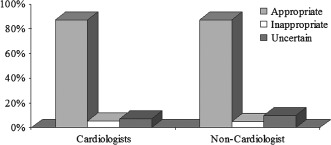
Appropriateness by ordering provider.
Appropriateness by Indication
Of the 287 studies ordered appropriately, 120 (42%) were ordered for evaluation of patients with ischemic equivalent of a nonacute nature. Symptoms considered to be ischemic equivalent are defined in the AUC 2009 document.11 Another 66 (23%) of the appropriate studies were ordered for evaluation of new symptoms of myocardial ischemia or ischemic equivalent in patients with prior revascularization. The rest of the appropriate studies were ordered for various other appropriate scenarios mentioned in the AUC document.
Of the 18 inappropriate studies, 8 (44%) studies were ordered for risk assessment in patients undergoing noncardiac surgery, and 4 (22%) for risk assessment in asymptomatic patients (or patients with stable symptoms) with a prior history of known coronary disease or prior abnormal stress imaging. The remainder of the inappropriate studies were ordered for various other scenarios mentioned in the AUC document.
Performance of SPECT MPI studies for patients with new or worsening symptoms with prior test results and/or known chronic stable CAD accounted for 14 (61%) of the uncertain studies. Of the remainder, 4 (17%) studies were performed for risk assessment in asymptomatic patients with prior abnormal coronary angiography or abnormal prior stress imaging study but no prior revascularization, 3 (13%) for risk assessment in asymptomatic patients with prior normal stress imaging tests, and 2 (8.6%) for risk assessment in asymptomatic patients with prior percutaneous coronary intervention (PCI).
Follow‐up of Inappropriate and Uncertain Studies
Results of the inappropriate and uncertain SPECT MPI studies and further follow‐up testing are shown in Figure 3.
Figure 3.
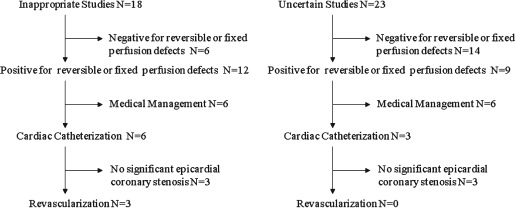
Further analysis of inappropriate and uncertain studies.
Interestingly, 12 of 18 (67%) of the studies performed for inappropriate indications were positive for fixed or reversible ischemia. Six of these patients underwent cardiac catheterization. Of these 6 patients, 3 were true positives and required revascularization, and the other 3 were false positive with no significant epicardial coronary stenosis. Nine (39%) of the uncertain studies were abnormal; 3 of these patients underwent cardiac catheterization and were not found to have any significant epicardial coronary stenosis.
Discussion
The principal finding of our study is that in a rural tertiary care center, only a very small proportion of MPI studies are ordered for inappropriate (5.5%) or uncertain (7%) indications. This is lower than the rates of inappropriate testing reported in previous studies assessing MPI tests, the majority of which were performed in urban locations.
We are not aware of any prior studies that have evaluated utilization of cardiac imaging in a rural healthcare setting after publication of the 2009 AUC document. The findings from our study with regard to trends in utilization of cardiac imaging that could be considered as a surrogate for quality of patient care are discordant with general observations about lower quality of care in rural centers.
In comparison with other studies performed in urban centers, we observed lower rates of inappropriate utilization of MPI. Gibbons et al evaluated MPI studies done at the Mayo Clinic using the AUC published in 2005, and classified 14% studies as inappropriate; a sizeable number of studies remained unclassifiable (11%). Screening of asymptomatic or low‐risk patients for coronary artery disease (48%) and preoperative risk assessment (17%) accounted for a major proportion of inappropriate studies.4
A large prospective multicenter study by Hendel and colleagues showed inappropriate utilization in 14.4%, using the AUC published in 2005. These investigators reported that noncardiologists ordered a higher number of inappropriate studies as compared to cardiologists (19.5% vs 13.2%, P < 0.0001). Five common indications accounted for almost 92% of inappropriate studies.6 Most common of these indications was for the detection of CAD in asymptomatic patients who were at low risk of coronary heart disease. Other indications were performance of SPECT MPI testing <2 years after PCI in an asymptomatic patient, preoperative risk assessment, or testing in low‐risk patients with chest pain.
Carryer and colleagues compared 2009 AUC with the 2005 AUC. Using the 2009 AUC for classification of 281 MPI studies done in 2005, they reported a utilization rate of 24.2% for inappropriate studies, 59.7% for appropriate studies, 16% for uncertain studies, and none of the studies were unclassifiable.10
In a recent study by Doukky and colleagues,14 they evaluated 1511 studies ordered in the Chicago metropolitan area. This study reported a much higher rate of inappropriate studies (45.5% of all studies) as compared to other studies (Table 2). More importantly, these inappropriate studies with abnormal results had no predictive value for future adverse cardiovascular events.
Table 2.
Prior Studies
| Author | Year | No. | Setting | AUC Criteria Applied | I | A | U | UN | Most Common Inappropriate Indication |
|---|---|---|---|---|---|---|---|---|---|
| Gibbons4 | 2008 | 284 | University hospital | 2005 | 14% | 64% | 11% | 10% | 10 (48%), 16 (17%), 12 (13%) |
| Mehta8 | 2008 | 1209 | University hospital | 2005 | 13% | 80% | 7% | 3% | 1 (57%), 31 (14%), 32 (14%) |
| McCully5 | 2009 | 298 | University hospital | 2005 | |||||
| Hendel6a | 2010 | 6351 | 6 sites: 3 urban, 2 semiurban, 1 rural | 2005 | 14.4% | 70.7% | 14.9% | 6.7% | 10 (45%), 40 (24%), 1 (16%) |
| Gibbons9 | 2010 | 284 | University hospital | 2005 | 7% | 66% | 15% | 12% | 10 (55%), 1 (20%) |
| Carryer10 | 2010 | 281 | University hospital | 2009 | 24.2% | 59.8% | 16% | 0% | 12 and 13 (43%), 23–25 (15%) |
| Gibbons7b | 2011 | 273 | University hospital | 2005 | 11.7% | 60.1% | 13.2% | 15% | |
| Gholamrezanezhad15 c | 2011 | 291 | Tertiary care center based in Asia | 2009, 2005 | 16.8% | 75.3% | 5.2% | 2.7% | |
| Koh19 | 2011 | 1623 | Tertiary care center based in Asia | 2009 | 10% | 82% | 5% | 3% | 40–42, 44–46, 48 (39%) 12, 13, 20 (17.5%) |
| Doukky14 | 2013 | 1511 | Office‐based setting in Chicago metropolitan area | 2009 | 45.5% | 51.6% | 2.9% | 0% |
Abbreviations: A, appropriate; AUC, appropriate use criteria; I, inappropriate; N, sample size; U, uncertain; UN, unclassifiable.
Preintervention cohort. b2008 cohort. cClassification based on 2009 criteria.
Although direct comparisons across different studies in disparate healthcare settings are difficult, we found a lower inappropriate utilization of MPI than prior studies (5.5% vs ∼14.4%).4, 6, 15 It is conjectural whether this reflects an actual change in practice due to increased awareness of AUC criteria, wider utilization of a preauthorization process, or is merely a reflection of regional differences in utilization of cardiovascular imaging.16, 17
We did not find any difference in the frequency of appropriate indications by the specialty of ordering provider. Both cardiologists and noncardiologists were equally likely to order inappropriate studies. It is possible that this is due to a greater collaboration between cardiology and noncardiology providers at our institution.
According to the latest change in terminology for the AUC, inappropriate and uncertain studies have been aptly redefined as “rarely appropriate” or “maybe appropriate.”18 Although not adequately powered to show statistical significance, this is reflected in the subanalysis of the inappropriate and uncertain studies in our study. Although it was disconcerting to note that in a small number of patients who were classified as having inappropriate or uncertain studies, 51% had abnormal test results that required cardiac catheterization (22%) and percutaneous or surgical coronary revascularization (7%). It is somewhat reassuring that recent studies have reported overall low event rates in this group of patients. In a recent study by Koh et al,19 of all the inappropriate studies ordered for low or intermediate risk patients undergoing preoperative evaluation, 40% had abnormal findings. However, these preoperative evaluation patients had low cardiovascular event rates compared to patients who underwent testing for appropriate indications and had detectable ischemia on MPI.20 Moreover, there was a high rate of false‐positive studies in patients with inappropriate or uncertain studies and abnormal results who underwent cardiac catheterization.
Even though the number of inappropriate studies was low in our analysis, it shares a common theme with previous studies,4, 6, 19, 20 with relatively few scenarios accounting for the vast majority of inappropriate and uncertain studies. In a recent study from Asia, patients referred for preoperative evaluation for low‐risk surgery accounted for the highest proportion of inappropriate studies.19 In another recent study by the same authors, 39.8% of all the studies referred for preoperative evaluation were observed to be inappropriate.20 In our study, two‐thirds of all the inappropriate tests were ordered for clinical scenarios related to either preoperative testing in low‐risk patients or testing in presently asymptomatic patients with prior history of known coronary disease or abnormal stress imaging. This finding may have implications for streamlining the preauthorization process in cardiac imaging; such a preauthorization process should be limited to indications that account for the majority of the inappropriately ordered tests. Ongoing education for healthcare providers regarding appropriateness criteria for MPI may help further reduce the rates of inappropriate utilization of MPI studies. Considering that there are approximately 10 million MPI studies performed annually in the United States,21 lowering the number of inappropriate studies could translate significantly in terms of cost containment, assuming it would help avoid unnecessary downstream testing. However, by the same token, it would be concerning to miss a diagnosis of CAD if all studies were appropriate. It is plausible that the patients with uncertain indication who got revascularization might have had worse outcomes if they had not had the MPI. More studies of association of AUC with clinical outcomes and quality of care are needed.
To further reduce the inappropriate studies, use of Web‐based applications may be helpful, which can help with the incorporation of AUC ratings in patient records.
Limitations
We did not assess the possible bias due to the preauthorization process. It is possible that the studies that could have been inappropriate were screened out during preauthorization. However, our study represents a real‐world scenario in terms of ordering and approving MPI studies reflecting current trends. We did not assess interobserver variability in terms of categorizing the studies. We did not assess whether the patients with inappropriate tests could have been served by a less costly noninvasive treadmill electrocardiograph stress test or stress echocardiogram. Last, although 12 of the 18 inappropriate studies were abnormal (fixed or reversible ischemia), we did not assess other variables such as the severity of the ischemia or extent of CAD on angiography in this group, and this finding should be interpreted with caution due to the absence of a fair comparison group.
Conclusion
We found that, regardless of ordering physician specialty, only a minority of MPI studies are performed for inappropriate or uncertain indications at our multispecialty practice rural health center. Certain common scenarios account for the majority of inappropriate or uncertain studies, suggesting a continuing need for provider education and possibly targeting the preauthorization process to selected clinical scenarios. It may be useful to incorporate AUC criteria into the electronic medical record such that it is readily accessible for the providers at the point of order entry.
The authors have no funding, Dr. Harjai and Dr. Sattur are co‐founders of the website “www.aucmonkey.com” operated by AUC Portal, LLC.
References
- 1. Lucas FL, DeLorenzo MA, Siewers AE, et al. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Congressional Budget Office . Geographic variation in health care spending. http://www.cbo.gov/sites/default/files/cbofiles/ftpdocs/89xx/doc8972/02‐15‐geoghealth.pdf. Published February 2008. Accessed May 31, 2013.
- 3. Brindis RG, Douglas PS, Hendel RC, et al. ACCF/ASNC appropriateness criteria for single‐photon emission computed tomography myocardial perfusion imaging (SPECT MPI): a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group and the American Society of Nuclear Cardiology endorsed by the American Heart Association. J Am Coll Cardiol. 2005;46:1587–1605. [DOI] [PubMed] [Google Scholar]
- 4. Gibbons RJ, Miller TD, Hodge D, et al. Application of appropriateness criteria to stress single‐photon emission computed tomography sestamibi studies and stress echocardiograms in an academic medical center. J Am Coll Cardiol. 2008;51:1283–1289. [DOI] [PubMed] [Google Scholar]
- 5. McCully RB, Pellikka PA, Hodge DO, et al. Applicability of appropriateness criteria for stress imaging: similarities and differences between stress echocardiography and single‐photon emission computed tomography myocardial perfusion imaging criteria. Circ Cardiovasc Imaging. 2009;2:213–218. [DOI] [PubMed] [Google Scholar]
- 6. Hendel RC, Cerqueira M, Douglas PS, et al. A multicenter assessment of the use of single‐photon emission computed tomography myocardial perfusion imaging with appropriateness criteria. J Am Coll Cardiol. 2010;55:156–162. [DOI] [PubMed] [Google Scholar]
- 7. Gibbons RJ, Askew JW, Hodge D, et al. Appropriate use criteria for stress single‐photon emission computed tomography sestamibi studies: a quality improvement project. Circulation. 2011;123:499–503. [DOI] [PubMed] [Google Scholar]
- 8. Mehta R, Ward RP, Chandra S, et al. Evaluation of the American College of Cardiology Foundation/American Society of Nuclear Cardiology appropriateness criteria for SPECT myocardial perfusion imaging. J Nucl Cardiol. 2008;15:337–344. [DOI] [PubMed] [Google Scholar]
- 9. Gibbons RJ, Askew JW, Hodge D, et al. Temporal trends in compliance with appropriateness criteria for stress single‐photon emission computed tomography sestamibi studies in an academic medical center. Am Heart J. 2010;159:484–489. [DOI] [PubMed] [Google Scholar]
- 10. Carryer DJ, Hodge DO, Miller TD, et al. Application of appropriateness criteria to stress single photon emission computed tomography sestamibi studies: a comparison of the 2009 revised appropriateness criteria to the 2005 original criteria. Am Heart J. 2010;160:244–249. [DOI] [PubMed] [Google Scholar]
- 11. Hendel RC, Berman DS, Di Carli MF, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119:e561–e587. [DOI] [PubMed] [Google Scholar]
- 12. Pennsylvania Office of Rural Health website . http://www.porh.psu.edu/docs/PORH_RuralDefined.pdf. Accessed May 31, 2013.
- 13. United States Department of Agriculture . Economic Research Service. New York: three rural definitions based on census places. http://www.ers.usda.gov/datafiles/Rural_Definitions/StateLevel_Maps/NY.pdf. Accessed May 31, 2013.
- 14. Doukky R, Hayes K, Frogge N, et al. Impact of appropriate use on the prognostic value of single‐photon emission computed tomography myocardial perfusion imaging. Circulation. 2013;128:1634–1643. [DOI] [PubMed] [Google Scholar]
- 15. Gholamrezanezhad A, Shirafkan A, Mirpour S, et al. Appropriateness of referrals for single‐photon emission computed tomography myocardial perfusion imaging (SPECT‐MPI) in a developing community: a comparison between 2005 and 2009 versions of ACCF/ASNC appropriateness criteria. J Nucl Cardiol. 2011;18:1044–1052. [DOI] [PubMed] [Google Scholar]
- 16. U.S. Government Printing Office . Deficit Reduction Act of 2005. http://www.gpo.gov/fdsys/pkg/BILLS‐109s1932enr/pdf/BILLS‐109s1932enr.pdf. Accessed May 31, 2013.
- 17. Song Y, Skinner J, Bynum J, et al. Regional variations in diagnostic practices. N Engl J Med. 2010;363:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hendel RC, Patel MR, Allen JM, et al. Appropriate use of cardiovascular technology: 2013 ACCF appropriate use criteria methodology update: a report of the American College of Cardiology Foundation appropriate use criteria task force. J Am Coll Cardiol. 2013;61:1305–1317. [DOI] [PubMed] [Google Scholar]
- 19. Koh AS, Flores JL, Keng FY, et al. Evaluation of the American College of Cardiology Foundation/American Society of Nuclear Cardiology appropriateness criteria for SPECT myocardial perfusion imaging in an Asian tertiary cardiac center. J Nucl Cardiol. 2011;18:324–330. [DOI] [PubMed] [Google Scholar]
- 20. Koh AS, Flores JL, Keng FY, et al. Correlation between clinical outcomes and appropriateness grading for referral to myocardial perfusion imaging for preoperative evaluation prior to non‐cardiac surgery. J Nucl Cardiol. 2012;19:277–284. [DOI] [PubMed] [Google Scholar]
- 21. Einstein AJ, Tilkemeier P, Fazel R, et al. Radiation safety in nuclear cardiology‐current knowledge and practice: results from the 2011 American Society of Nuclear Cardiology member survey. JAMA Intern Med. 2013;173:1021–1023. [DOI] [PubMed] [Google Scholar]


