Abstract
Background
Our goal was to define the prevalence of radiation‐induced valvular heart (RIVD) disease among patients undergoing cardiac valve surgery in a community‐based, regional academic medical center. Mediastinal radiation is a treatment modality for various hematologic and solid malignancies; however, long‐term cardiac complications, including radiation‐induced valvular heart disease, can occur years after the radiation treatments.
Hypothesis
Mediastinal radiation exposure is an independent risk factor for valvular heart disease often necessitating valve replacement in patients without other risk factors for valve disease.
Methods
Between January 1, 1998 and September 1, 2007, we retrospectively analyzed our institution's cardiac surgical database over a 10 year period and identified 189 consecutive patients ≤ 50 years of age who underwent valve surgery. Using case‐control matching, we assessed the prevalence of mediastinal radiation among these young patients with valve disease necessitating surgery and to their matched controls from all patients admitted to the hospital.
Results
Nine individuals (4.8%) were identified as having received previous mediastinal radiation, significantly increased from controls (p<0.0001), and 8 of whom had surgical or pathologic findings consistent with radiation damage. Compared with a matched case‐control population, individuals who had severe valve disease and underwent valve replacement had a markedly increased prevalence of prior mediastinal radiation therapy.
Conclusions
In conclusion, cardiologists must remain aware of the potential long term valvular complications in patients treated with mediastinal radiation. Increased surveillance for RIVD may be considered in the decades following radiation therapy.
Introduction
Mediastinal radiation is a treatment modality utilized for various hematologic and solid‐tumor malignancies, including Hodgkin and non‐Hodgkin lymphoma, testicular cancer, and breast cancer. Along with other oncologic therapies, mediastinal radiation has allowed for improved survival rates among people with various malignancies. Recently, the Centers for Disease Control and Prevention (CDC) and the National Cancer Institute (NCI) published a report regarding the increasing number of current cancer survivors in the United States. Using epidemiologic data, the CDC and NCI estimated that 1 in 25 adults is a cancer survivor as of the year 2007.1 Although many patients have survived a malignancy, they have an increased risk of morbidity, including cardiac complications, as the result of cancer treatments alone.2
Cardiac complications, due to the proximity of the heart to commonly used radiation fields, may occur years later. Some estimate the aggregate incidence of radiation‐induced cardiac disease to be between 10% and 30% by 5 to 10 years after treatment, most of which is asymptomatic.3 Long‐term cardiac complications associated with mediastinal radiation include acute and chronic pericarditis, premature coronary artery disease (CAD), fibrosis of the myocardium, and cardiac conduction abnormalities.4, 5 Radiation‐induced valvular disease (RIVD) is another complication that manifests a number of years after therapy, at times necessitating valve surgery in patients without other risk factors for valve disease. Valvular changes have been reported in patients with a cumulative mediastinal radiation dose >1500 cGy.2, 5, 6, 7, 8, 9 More recently, a retrospective study on childhood cancer survivors found a 5‐fold increase in valvular abnormalities in cancer survivors compared with their sibling matched controls.2 In this study we considered the association between prior radiation and subsequent valve disease in a large regional academic medical center.
Methods
The Society of Thoracic Surgeons (STS) database is a national database that collects information from adult cardiovascular, thoracic, and congenital surgical cases for the purpose of outcomes research. After obtaining approval from the institutional review board, we retrospectively reviewed our institution's STS database to identify all patients age <50 years who underwent valve surgery between January 1, 1998, and September 1, 2007. This age was chosen arbitrarily, to limit the likelihood of confounding, age‐related causes of valvular damage. Radiation valvulopathy was not reported in the STS database at the time of our study; therefore, all available hospital records were retrospectively analyzed by the authors to identify patients with a previous malignancy or a documented history of mediastinal radiation.
Case matching based on age, sex, and time of hospitalization was conducted to assess whether there was increased prevalence among patients age <50 years who underwent valve surgery at our institution, compared with matched controls. Our research staff contacted all cases and matched controls by telephone to verify medical history using a prespecified questionnaire. All patients were contacted except 1 (188/189). This individual had known rheumatic heart disease and no previous mediastinal radiation but could not be contacted secondary to relocation. Among controls, individuals having a prior history of malignancy or radiation therapy were contacted by the authors to verify the presence or absence of previous mediastinal radiation.
All cases and matched controls were included in the final analysis. The χ2 test for independent groups was used to compare proportions of cases and controls with respect to comorbidities. McNemar's test for correlated proportions was used to compare the impact of mediastinal radiation exposure on cases vs controls. Multivariable conditional fixed‐effects logistic regression was performed to assess the impact of cardiovascular comorbidities on RIVD. Because none of the controls were found to have previous radiation exposure, odds ratios (ORs), adjusted for comorbidities, were estimated using exact methods.10, 11
Results
During the approximate 10‐year time period, we identified 189 patients age <50 years who underwent cardiac valve surgery at our institution. Of these individuals, 9 patients (4.8%) had previous mediastinal radiation at some point during their lifetimes. Baseline characteristics for the individuals with a history of mediastinal radiation are listed in Table 1.
Table 1.
Baseline Characteristics for those Individuals Receiving Mediastinal Radiation
| Patient# | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| Height (centimeters) | 168 | 160 | 163 | 193 | 174 | 155 | 176.5 | 163 | 152 |
| BMIa | 27 | 29.1 | 37.7 | 22.6 | 36.3 | 31.3 | 28.4 | 29.1 | 25.7 |
| HTNe | 0 | 0 | 0 | 0 | 0 | + | 0 | + | 0 |
| Smoker | + | + | 0 | 0 | 0 | 0 | + | 0 | + |
| Current smoker | + | + | 0 | 0 | 0 | 0 | + | 0 | 0 |
| Diabetes | 0 | 0 | 0 | 0 | + | + | + | + | 0 |
| Dyslipidemia | 0 | 0 | 0 | + | + | + | + | + | 0 |
| CKDc | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Family history of CADc | + | 0 | 0 | 0 | 0 | + | 0 | + | 0 |
| History of endocarditis | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CVAd | 0 | 0 | 0 | 0 | + | + | 0 | 0 | 0 |
| PVD f | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Congenital heart disease | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Connective tissue disease | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Bicuspid aortic valve | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Rheumatoid heart disease | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Heart block | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CADb | + | + | 0 | 0 | + | + | + | 0 | 0 |
Abbreviations:
BMI = Body Mass Iindex;
CAD= Coronary Artery Disease;
CKD = Chronic Kidney Disease;
CVA = Cerebral Vascular Accident;
HTN = Hypertension;
PVD = Peripheral Vascular Disease.
The patients who received mediastinal radiation were treated between the years 1970 and 1991 for various malignancies before being diagnosed with significant valvular heart disease that necessitated surgery. Of those 9 patients, 4 were treated for Hodgkin lymphoma, 3 for testicular cancer, 1 for non‐Hodgkin lymphoma, and 1 for breast cancer. According to the patients' admission medical records at the time of their surgery, a documented history of malignancy that led to radiation therapy was found in 6 of the 9 patients' preoperative medical records. The other 3 patients had prior documentation of malignancy or radiation. Of those with the documented history of malignancy on admission, prior radiation therapy was only mentioned in 3 of these patients' histories. In only 1 patient was it specified that the radiation therapy was to the mediastinum.
For the 9 patients in our study, we found the mean age at the time of their radiation treatment to be 22 years (range, 14–23 y) and the mean age at the time of valve replacement was 46.2 years (range, 37–50 y). The mean interval from radiation treatment to the time of their valve surgery was 22.9 years (range, 12–33 y), as seen in Figure 1. Despite review of available medical records and patient interviews, we were unable to obtain the radiation therapy–treatment details of the patients in our study.
Figure 1.
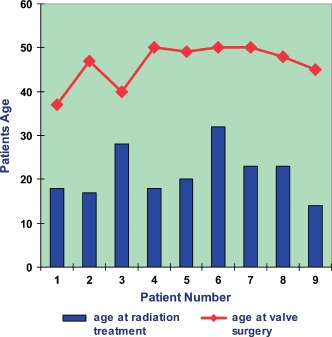
Time increment between mediastinal radiation and valve disease necessitating surgery, which represents the time interval between the ages at which the 9 patients underwent mediastinal radiotherapy to delayed onset of radiation‐induced valve disease necessitating surgery.
Most patients were followed in private offices outside of our institution, so we were unable to ascertain records of when the patient's valve disease was first diagnosed or became clinically significant. All patients previously treated with mediastinal radiation had left‐sided valvular lesions, and 3 patients had concomitant right‐sided lesions. The primary affected valve was the aortic valve, which was severe enough to require replacement in 7 of the 9 patients (Table 2). Of those 7 patients, 5 had concomitant mitral‐valve disease requiring surgery. Of the 2 patients who did not have aortic‐valve involvement, 1 had isolated mitral regurgitation and the other had both mitral and tricuspid regurgitation requiring surgery. None of our patients who underwent mediastinal radiation had a history of rheumatic heart disease or bicuspid aortic valve (Table 1).
Table 2.
Temporal Sequence and Surgical/Pathological Findings of Patients With a History of Mediastinal Radiation
| Patient No. | Radiation Age, y | Surgery Age, y | Valve Lesions | Type of Valve Surgery | Intraoperative | Pathology | Multivalvular Calcifications |
|---|---|---|---|---|---|---|---|
| 1 | 18 | 37 | AR, MR | VR, MVA | + | + | + |
| 2 | 17 | 47 | AS, MS, TR | AVR, MVR, TVA | + | + | |
| 3 | 28 | 40 | AR, MR, TR | AVR, MVR, TVA | + | + | |
| 4 | 18 | 50 | AS | AVR | + | + | |
| 5 | 20 | 49 | MR | MVA | |||
| 6 | 32 | 50 | MR, TR | MVA, TVA | + | ||
| 7 | 23 | 50 | AS, MR | AVR, MVA | + | + | + |
| 8 | 23 | 48 | AS | AVR | + | + | + |
| 9 | 14 | 45 | AS, MR | AVR, MVA | + | + | + |
Abbreviations: AR, aortic regurgitation; AS, aortic stenosis; AVR, aortic valve replacement; MR, mitral regurgitation; MS, mitral stenosis; MVA, mitral valve annuloplasty/repair; MVR, mitral valve replacement; TR, tricuspid regurgitation; TVA, tricuspid valve annuloplasty.
One patient had both mitral and aortic stenosis, along with tricuspid valve regurgitation. According to both the patient and medical records, there was no documented history of rheumatic fever, renal disease, or connective‐tissue disease. Her echocardiogram showed valve thickening but no other classic features of rheumatic heart disease (doming of the mitral valve, commissural fusion, subvalvular thickening, or restriction of the tips of the mitral valve). In addition, she was noted to have severe annular calcification of both the mitral and tricuspid valve along with calcification of the ascending aorta, a finding characteristic of RIVD.5, 12 The presence of extensive multivalvular calcifications was found in 6 of the 9 patients (Table 2). No other explanation for this finding other than RIVD existed in these relatively young patients.
Six of the patients were found to have typical intraoperative findings consistent with radiation damage, such as fibrinous adhesions in the mediastinum and of the internal mammary arteries, thickened epicardium, and thickened pericardium noted in the operative report.5, 6, 12, 13 Of the other 3 patients without intraoperative findings, 2 had multivalvular calcifications in addition to pathological findings consistent with RIVD (Figure 2).5, 14 One patient with prior mediastinal radiation had no intraoperative findings nor pathological changes consistent with RIVD, but did have a dilated cardiomyopathy associated with severe mitral regurgitation, thus making the diagnosis of RIVD. This patient did have a history of chemotherapy, but the regimen used was unavailable as it was performed at an outside institution decades ago. Pericardial changes associated with prior radiation therapy were specifically noted intraoperatively in 6 of the 9 patients, but none had been diagnosed previously with clinical pericarditis.
Figure 2.
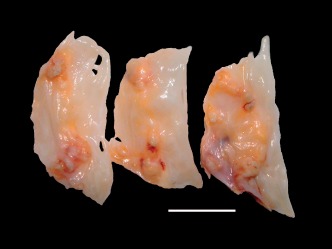
Aortic valve specimen from a patient in the study. Pathological findings consisted of nodular thickening and calcification. This individual also had intraoperative changes consistent with radiation‐induced valvular disease.
In Table 3, a comparison of the classical risk factors for valve disease is presented, in addition to the impact of mediastinal radiation exposure on cases and their controls. As expected, significantly more risk factors were found in the cardiac‐surgery group. In the case‐matched control group, no individuals had previous mediastinal radiation, whereas 9 patients in the cardiac‐surgery group were previously treated with mediastinal radiation (P < 0.0001). Excluding the patient without evidence of RIVD seen intaoperatively or with pathologic analysis, the statistical significance of the study was not changed (P < 0.0001). None of the 9 cases with mediastinal radiation exposure evidenced the presence of any of the comorbidities except CAD, (not surprising, given the known association between mediastinal radiation and the development of premature CAD); the conditional logistic regression model included only CAD as a potential confounder. Adjusted for CAD, patients with radiation exposure were nearly 15× more likely to experience cardiac surgery (OR = 14.92, P = 0.0153) than the control group.
Table 3.
Prevalence of Risk Factors for Cardiac Valvular Surgery Between a Cased‐Matched Population
| Risk Factors | Cases, n = 189, % (n) | Controls, n = 189, % (n) | P Value |
|---|---|---|---|
| Aortic dissection/dilation | 5.3 (10) | 0.5 (1) | 0.0106 |
| MVP/chordal abnormalities | 15.9 (30) | 0.0 (0) | <0.0001 |
| Bicuspid aortic valve | 26.5 (50) | 0.0 (0) | <0.0001 |
| Coronary artery disease | 32.3 (61) | 4.8 (9) | <0.0001 |
| MI with papillary muscle dysfunction | 4.8 (9) | 0.0 (0) | 0.0035 |
| Congenital heart disease | 4.2 (8) | 0.5 (1) | 0.0387 |
| Endocarditis | 4.8 (9) | 0.5 (1) | 0.0199 |
| Rheumatic heart disease | 15.9 (30) | 0.0 (0) | <0.0001 |
| Mediastinal radiation | 4.8 (9) | 0.0 (0) | <0.0001 |
Abbreviations: MI, myocardial infarction; MVP, mitral valve prolapse.
Discussion
We found that approximately 5% of patients age <50 years who underwent valve surgery in our community had RIVD as the likely etiology. In our study, 8 of 9 patients had typical findings consistent with radiation damage. Combined with the absence of usual valve‐disease etiologies, we are reasonably certain that all but 1 of our identified cases is in fact RIVD. Our results suggest that radiation exposure is an independent predictor of valve surgery for RIVD. In contrast to previous reports, we focused on the impact of RIVD on contemporary cardiology and surgical practice. Other prospective studies have estimated the incidence and risk of RIVD among the general population; however, this is the first systematic evaluation of RIVD looking backward from surgery.3, 7
Prospective studies can only approximate the impact of this disorder due to the long latency between radiation treatments and clinically significant valvular disorders. Similarly, retrospective studies are limited by this long latency, as patients included are those recruited or available to researchers, a population that may not be representative. Most of our patients were not being followed by oncologists or other treating physicians with regard to their cancers from >20 years earlier. In fact, in many of our patients, this diagnosis was no longer being mentioned in their medical reports, and mediastinal radiation was mentioned only rarely. Only a detailed review of the patients undergoing valve surgery, as we have done, can reveal the current impact of these distant treatments. Records of every patient in our study group were meticulously reviewed to ensure that a history of chest radiation was not overlooked.
The mean interval from the time of radiation to surgery was 23 years, which may lead to failure to diagnose RIVD. As seen in Table 2, all but 1 of our patients were diagnosed and treated for various malignancies in their teens or 20s, whereas the development of critical valvular heart disease did not occur until much later in life. The delayed onset of RIVD in our patient population is consistent with prior reports on valvular disease after mediastinal radiation.2, 7, 8, 15, 16 Carlson et al. showed an increased incidence of asymptomatic valve disease 11.5 years post‐radiation, which subsequently progressed to symptomatic valvular disease 5 years later.5 Hull et al. similarly demonstrated the development of clinically significant valvular disease a median of 22 years after treatment with mediastinal radiotherapy.8 Recently reported, the cumulative incidence rate of developing moderate or severe valvular disease is almost 9% at 25 years after mediastinal radiation, and the standard incidence ratio for valve surgery was 9.2% (95% confidence interval: 8.07–10.31) compared with the general population.7
Although reported in the literature, RIVD is not high on the radar screen of adult cardiologists, illustrated by the fact that the diagnosis was considered preoperatively by cardiologists in only 2 of the 9 patients we describe here. Radiation‐induced valvular disease requiring surgery was uncommon in our population (8 cases over 9 years) but still represents a finite percentage of valve surgery in younger patients. Another reason for the underappreciation of this entity among cardiologists, we believe, is that most of the published literature on cardiac complications after mediastinal radiation comes from the oncology literature. One recently published study, coauthored by one of us, had only 2 of 32 references from cardiology journals.7 Though some references were from the general medical literature (Journal of the American Medical Association, The New England Journal of Medicine), the overwhelming majority were from oncology/hematology journals, a resource not widely read by cardiologists. In fact, the most recent review on cardiovascular complications of cancer therapy in the cardiology literature, by Yeh and Bickford, does not even mention RIVD.17
Currently, there are no established cardiology guidelines or consensus statements on the follow‐up of those patients who have received mediastinal radiation; nonetheless, adult cardiologists will encounter this issue as a result of increasing survival among patients with various malignancies. Several surveillance recommendations have been suggested in the oncology literature, including serial echocardiographic examinations and stress testing, depending on radiation dose, chemotherapeutic agent and dose, and other cardiac risk factors that are present.7, 8, 14, 15, 18 Recently, the CDC and NCI highlighted the need to identify those with late effects from radiation therapy among the growing population of cancer survivors.1
A limitation of our study is that we undoubtedly missed some patients who underwent mediastinal radiation in their early decades and did not develop RIVD until after age 50 years, our arbitrary age cutoff, possibly underestimating the problem. The median age of diagnosis for Hodgkin disease is 25 years, for example; this would mean that a substantial percentage of these patients would develop clinically significant valve disease after the age of 50. Given the latency of >2 decades, patients presenting with any malignancy later in life and subsequently treated with mediastinal radiation would also be missed in our assessment.7 Our inability to obtain details of the initial diagnosis of valve disease, radiation treatments, and chemotherapy decades earlier is also a limitation of our study. Knowing the time between the initial diagnoses of cardiac‐valve disease until surgery may have given an idea of the temporal progression of RIVD.
Conclusion
Elucidating the etiology of valvular heart disease becomes more difficult as individuals age and degenerative etiologies of valve disorders become more frequent. Additionally, we have only enumerated those patients whose valve disease was severe enough to require open‐heart surgery, which may reflect only the tip of the iceberg of those affected by RIVD. Fortunately, RIVD will likely decrease over time due to lower radiation volumes, better methods of shielding, and limiting therapeutic fields; however, the dose threshold at which radiation exposure will not cause valve disease is unknown, if it even exists at all.8 Among young patients with severe valve disease requiring surgery, previous mediastinal radiation was found in a minority. Cardiologists must remain aware of this potential late complication of mediastinal radiation, because RIVD is not clinically recognized until years after oncologic treatment and the number of survivors of radiation therapy continues to increase.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Centers for Disease Control and Prevention (CDC) . Cancer survivors—United States, 2007. MMWR Morb Mortal Wkly Rep. 2011;60:269–272. [PubMed] [Google Scholar]
- 2. Mulrooney DA, Yeazel MW, Kawashima T, et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the childhood cancer survivor study cohort. BMJ. 2009;339:b4606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carver JR, Shapiro CL, Ng A, et al. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol. 2007;25:3991–4008. [DOI] [PubMed] [Google Scholar]
- 4. Libby P, Rcb Bonow, Mann DL, et al. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 8th ed. Philadelphia, PA: Saunders/Elsevier; 2008:2115. [Google Scholar]
- 5. Carlson RG, Mayfield WR, Normann S, et al. Radiation‐associated valvular disease. Chest. 1991;99:538–545. [DOI] [PubMed] [Google Scholar]
- 6. Crestanello JA, McGregor CG, Danielson GK, et al. Mitral and tricuspid valve repair in patients with previous mediastinal radiation therapy. Ann Thorac Surg. 2004;78:826–831. [DOI] [PubMed] [Google Scholar]
- 7. Galper SL, Yu JB, Mauch PM, et al. Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation. Blood. 2011;117:412–418. [DOI] [PubMed] [Google Scholar]
- 8. Hull MC, Morris CG, Pepine CJ, et al. Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of Hodgkin lymphoma treated with radiation therapy. JAMA. 2003;290:2831–2837. [DOI] [PubMed] [Google Scholar]
- 9. Veeragandham RS, Goldin MD. Surgical management of radiation‐induced heart disease. Ann Thorac Surg. 1998;65:1014–1019. [DOI] [PubMed] [Google Scholar]
- 10. Mehta CR, Patel NR, Senchaudhuri P. Exact stratified linear rank tests for ordered categorical and binary data. J Comput Graph Stat. 1992;1:21–40. [Google Scholar]
- 11. Mehta CR, Patel NR, Senchaudhuri P. Efficient Monte Carlo methods for conditional logistic regression. J Am Stat Assoc. 2000;95:99–108. [Google Scholar]
- 12. Veinot JP, Edwards WD. Pathology of radiation‐induced heart disease: a surgical and autopsy study of 27 cases. Hum Pathol. 1996;27:766–773. [DOI] [PubMed] [Google Scholar]
- 13. Hooning MJ, Botma A, Aleman BM, et al. Long‐term risk of cardiovascular disease in 10‐year survivors of breast cancer. J Natl Cancer Inst. 2007;99:365–375. [DOI] [PubMed] [Google Scholar]
- 14. Brosius FC 3rd, Waller BF, Roberts WC. Radiation heart disease: analysis of 16 young (aged 15 to 33 years) necropsy patients who received over 3500 rads to the heart. Am J Med. 1981;70:519–530. [DOI] [PubMed] [Google Scholar]
- 15. Heidenreich PA, Hancock SL, Lee BK, et al. Asymptomatic cardiac disease following mediastinal irradiation. J Am Coll Cardiol. 2003;42:743–749. [DOI] [PubMed] [Google Scholar]
- 16. Hancock SL, Donaldson SS, Hoppe RT. Cardiac disease following treatment of Hodgkin's disease in children and adolescents. J Clin Oncol. 1993;11:1208–1215. [DOI] [PubMed] [Google Scholar]
- 17. Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;16;53:2231–2247. [DOI] [PubMed] [Google Scholar]
- 18. Hancock SL, Tucker MA, Hoppe RT. Factors affecting late mortality from heart disease after treatment of Hodgkin's disease. JAMA. 1993;270:1949–1955. [PubMed] [Google Scholar]


