Abstract
Background
Inadequate recruitment of women and an exclusion of patients with end‐stage renal disease (ESRD) in coronary revascularization trials have led to knowledge gaps of gender‐based outcomes.
Hypothesis
Women have equivalent cardiovascular outcomes when compared to men.
Methods
We conducted a retrospective observational study utilizing Kaiser Permanente Northern California (KPNC) databases and identified 1015 adults with ESRD who underwent coronary revascularization between 1996 and 2008. We ascertained baseline characteristics, primary (mortality at 5 years) and secondary (myocardial infarction [MI] and repeat revascularization) outcomes from KPNC databases, state death certificates, and Social Security Administration files. A multivariable logistic regression was used to determine the association of gender to the prespecified outcomes.
Results
Men and women were similar in age (P = 0.23). The mean number of baseline comorbidities was higher in women (2.7, 95% confidence interval [CI]: 2.5‐2.9) compared to men (2.3, 95% CI: 2.1‐2.4, P = 0.0002). The risk‐adjusted odds ratios (OR) of female gender to death at 5 years (OR: 1.12, 95% CI: 0.83‐1.52), MI (OR: 1.19, 95% CI: 0.86‐1.64), and repeat revascularization (OR: 1.01, 95% CI: 0.70‐1.45) were similar to men. Age modified the effect of gender for the primary outcome death (P interaction < 0.048), with a trend toward worse outcomes in younger women and improved outcomes in older women. This effect was noted more in patients who underwent coronary artery bypass grafting.
Conclusions
Although the overall relative risk of cardiovascular outcomes after coronary revascularization in ESRD was equivalent between men and women, age had a significant interaction with gender on overall mortality.
Introduction
There is a paucity of data addressing gender‐specific outcomes after coronary revascularization by either percutaneous coronary intervention (PCI)1 or coronary artery bypass grafting (CABG)2 in patients with end‐stage renal disease (ESRD). Advancing age and an increase in the number of baseline comorbidities have been noted in women with normal renal function referred for coronary revascularization by PCI3 or CABG.4 Whether this differential comorbidity profile between men and women explains the variations in outcomes in patients with ESRD is still under debate.2, 3, 5, 6 More gender‐specific research is needed.7, 8, 9
The double threat of inadequate recruitment of women and the exclusion of patients with advanced kidney disease, especially those with ESRD into clinical trials,10, 11, 12 have led to large gaps of knowledge in this area. Therefore, the purpose of this study was to specifically focus on the understanding of gender differences in cardiovascular outcomes8 between adult men and women with ESRD on chronic dialysis after coronary revascularization by PCI or CABG.
Methods
Our source population included members of Kaiser Permanente Northern California (KPNC), a large, integrated, healthcare delivery system that is highly representative of the local surrounding and statewide population.13 Utilizing a retrospective observational study design, we identified 1015 patients through the KPNC databases14, 15 on chronic dialysis who underwent an index coronary revascularization procedure by either PCI or CABG without an accompanying valve or other cardiac surgery procedure between January 1996 and December 2008. The baseline clinical and medication variables that were obtained were very similar to those used in 3 recent studies and are noted in Table 1.16, 17, 18 The baseline medications obtained were based on information from dispensed prescriptions and refill patterns from the KPNC databases. We obtained the majority of baseline angiographic variables such as the type of stent used (drug eluting or bare metal) and the number of vessels involved in the index revascularization (CABG or PCI) from procedure codes. Individual patient chart review was also performed, and data were abstracted from surgical or PCI procedure reports. All components of the study were approved by the KPNC institutional review board.
Table 1.
Baseline Clinical Variables Stratified by Gender and P Value
| Variable | Male, n = 649 | Female, n = 366 | P Value |
|---|---|---|---|
| Age, % | |||
| <65 years | 53.8 | 49.4 | 0.28 |
| 65–75 years | 31.3 | 36.1 | |
| >75 years | 15.0 | 14.5 | |
|
Duration of dialysis in years prior to revascularization, mean ± SD |
2.3 ± 2.3 | 2.7 ± 2.9 | 0.19 |
| Categorized year of revascularization, % | |||
| 1996–1999 | 18.9 | 14.5 | 0.11 |
| 2000–2003 | 31.0 | 29.5 | |
| 2004–2008 | 50.1 | 56.0 | |
| Baseline comorbidities, % | |||
| Tobacco use | 49.3 | 35.5 | <0.0001 |
| Myocardial infarction | 40.1 | 45.9 | 0.07 |
| Diabetes mellitus | 71.2 | 77.6 | 0.03 |
| Hyperlipidemia | 81.4 | 87.2 | 0.02 |
| Hypertension | 91.4 | 94.3 | 0.11 |
| Heart failure | 37.6 | 40.4 | 0.38 |
| Liver disease | 4.2 | 3.8 | 0.87 |
| Lung disease | 20.9 | 27.9 | 0.01 |
| Stroke/transient ischemic attack | 6.6 | 7.9 | 0.45 |
| Atrial fibrillation/flutter | 14.6 | 14.8 | NS |
| Baseline medications, % | |||
| Angiotensin converting enzyme‐inhibitor | 30.7 | 34.4 | 0.23 |
| Angiotensin receptor blocker | 12.6 | 17.2 | 0.05 |
| β‐Blocker | 63.3 | 65.0 | 0.63 |
| Diabetes medication | 50.1 | 57.9 | 0.02 |
| Calcium channel blocker | 59.2 | 60.1 | 0.79 |
| Statin | 51.6 | 56.8 | 0.12 |
Abbreviations: NS, not significant; SD, standard deviation.
Data on the primary outcome of all‐cause mortality at 5‐years and the secondary outcomes of myocardial infarction14 (MI) and repeat revascularization were obtained by using KPNC databases, state death certificates, and Social Security Administration files. We also assessed all‐cause mortality at 30 days, 1 year, and 3 years. MI was identified as a hospitalization, with a primary discharge International Classification of Diseases, 9th Revision code of acute MI, and obtained through KPNC databases and identified as a hospitalization for an MI more than 14 days after the index revascularization. Repeat revascularization was defined as a first revascularization procedure occurring more than 14 days after the index revascularization. Patients were followed until death or they were censored when they met any of the following criteria: end of study as of December 31, 2008, organ transplantation, or disenrollment from the health plan.
Statistical Analysis
All statistical analyses were performed using Stata version 12, (StataCorp, College Station, TX). Initial bivariate analysis stratified by gender was performed using the Fisher exact test or a χ2 analysis for categorical variables and a nonparametric test (Kruskal‐Wallis rank test) or t test (for unequal variances) for continuous variables. We used multivariable logistic regression and report results as odds ratio (OR) and 95% confidence interval (CI) to assess the association between gender and the prespecified outcomes. The primary predictor was female (vs male) gender. We also performed well‐validated assessments of interactions,19 using a multiplicative interaction term, between the primary predictor gender and important covariates based on an a priori hypothesis that age had an effect modification on gender for the primary outcome mortality. We subsequently graphed what we felt was a biologically plausible19 model‐predicted probability, stratified by gender, with age on the abscissa, which included the interaction term between age and gender.
Results
Baseline Clinical Comorbidities
Women constituted 36.1% of the total cohort (see Supporting Information, Figure 1, in the online version of this article). There were no significant differences in the proportion of men and women within each age category (P = 0.28), duration of dialysis prior to revascularization (P = 0.19), and in the proportion of coronary revascularization within each categorized year (P = 0.11, Table 1). The mean number of baseline comorbidities was higher in women compared to men (OR: 2.7, 95% CI: 2.5‐2.9; OR: 2.3, 95% CI: 2.1‐2.4, P = 0.0002). The model‐predicted probability of the number of comorbidities by age, stratified by gender, over the age spectrum is shown in Figure 1. This demonstrates that although the overall number of comorbidities decreases with age, the differential in comorbidities between men and women continue to diverge with age.
Figure 1.
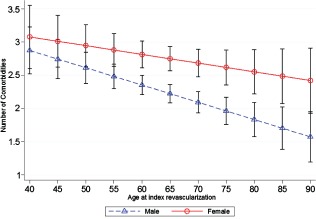
Model‐predicted number of comorbidities vs age, stratified by gender, with 95% confidence intervals. Model includes the dependent variable number of baseline comorbidities, gender, age, duration of dialysis, and an interaction term between gender and age as a continuous variable.
Baseline Intervention Characteristics
PCI was the more common revascularization modality used among both men and women compared to CABG (P = 0.005). There were no gender differences in the number of drug‐eluting stents received (P = 0.25) or the number of vessels bypassed (P = 0.39). Also, there was no difference between men and women in the total number of vessels intervened upon by either revascularization modality (P = 0.10).
Primary and Secondary Outcomes
We found no significant difference in the crude risk of death at 5 years postrevascularization between men (298/591, 50.4%) and women (177/339, 52.2%; P = 0.6). After adjustment for potential confounders, gender was not associated with mortality at 5 years, the primary outcome. Furthermore, in the adjusted multivariable regression model, female gender was not associated with a significant increase in risk of early (30 days) or later (1, 3, 5 years) mortality compared with male gender (Table 2).
Table 2.
Relative Risk for Women Compared to Men for Primary and Secondary Outcomes
| Outcome | Unadjusted Odds Ratio, HR (95% CI) | Adjusted Odds Ratio, HR (95% CI) |
|---|---|---|
| Death | ||
| 5 years | 1.07 (0.82‐1.40) | 1.12 (0.83‐1.52) |
| 3 years | 1.05 (0.78‐1.40) | 1.09 (0.78‐1.52) |
| 1 year | 1.27 (0.84‐1.93) | 1.26 (0.77‐2.06) |
| 30 days | 0.39 (0.13‐1.19) | 0.55 (0.12‐2.54) |
| Myocardial infarction | 1.39 (1.03‐1.85) | 1.19 (0.86‐1.64) |
| Repeat revascularization | 1.11 (0.79‐1.57) | 1.01 (0.70‐1.45) |
Abbreviations: CI, confidence interval; HR, hazard ratio.
Model includes female gender, year of revascularization, age, duration of dialysis, number of vessels intervened, and baseline comorbidities.
For the secondary outcome, postrevascularization MI, we found a slight increase in the crude risk of MI in women (114/366, 31.2%) compared to men (159/649, 24.5%; P = 0.02). However, after adjustment for potential confounders, gender was not independently associated with the outcome MI (Table 2). Finally, we found no significant difference in the crude risk of repeat revascularization between women (63/366, 17.2%) and men (102/649, 15.7%; P = 0.54). Adjustment for confounders continued to show that gender was not independently associated with repeat revascularization (Table 2). A sensitivity analysis was done for the outcomes MI and repeat revascularization with the 14‐day exclusion removed, with no materially significant change in the risk estimates.
For the primary outcome death, we found significant interactions between gender and age (P interaction = 0.048) and between gender and a baseline history of congestive heart failure (P = 0.03). We graphed only the model‐predicted probability of death by age, stratified by gender, which included an interaction term between gender and age, as this was felt to be a biologically plausible interaction (Figure 2). It suggested a trend toward worse outcomes in younger women and improved outcomes in older women. In an analysis restricted to those patients who underwent PCI, there did not appear to be any significant differences. However, in those who underwent CABG, women had a minimal increase in risk throughout the age spectrum. However, men had a lower risk under the age of 65 years and a higher risk after the age of 65 years when compared to women (Figure 3).
Figure 2.
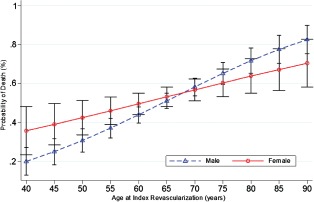
Model‐predicted probability of death vs age, stratified by gender, with 95% confidence intervals. The model is similar to Table 2, with an additional interaction term between gender and age.
Figure 3.

Model‐predicted probability of death vs age, stratified by gender, with 95% confidence intervals. The model is similar to Figure 2. The top graph is restricted to those patients who underwent percutaneous coronary intervention. The bottom graph is restricted to those patients who underwent coronary artery bypass grafting.
Discussion
In congruence with findings from studies of patients with normal renal function, our study conducted at KPNC, in a well‐described cohort of patients with ESRD referred for coronary revascularization, showed that women when compared to men presented with a higher baseline comorbidity profile. In the setting of earlier studies having mixed results, our findings confirmed that despite this higher baseline comorbidity profile, we found no significant risk‐adjusted associations between men and women for all 3 of our prespecified outcomes. We expanded our analysis further and found an effect modification of gender by age (ie, women under the age of 65 years trended toward doing slightly worse, whereas women over the age of 65 years trended toward doing slightly better compared to their male counterparts). This interaction was even more apparent when the analysis was restricted to those patients who received CABG.
The leading cause of death in women continues to be cardiovascular disease.8, 9, 20 However, women and patients with ESRD continue to be under‐represented in cardiovascular clinical trials.8, 21 Recent observational studies that have reported gender‐specific outcomes have noted mixed results.17, 18 One study that included patients hospitalized for an index coronary revascularization after initiation of dialysis reported that female sex was associated with a 17% increased relative risk of death.16 However, a more recent report from the same group found that female gender was not significantly associated with death after coronary revascularization.17 The discrepancy between these 2 studies may be related to secular trends, variations in statistical adjustment of comorbidities, and variations in the methods of revascularization stratification. Our study found similar survival between men and women when compared to the later report,17 which also included MI and repeat revascularization as secondary outcomes and also noted no gender‐based differences for these 2 outcomes.
Another recent study reported on the interaction that gender had on the coronary revascularization modality used, and found that men undergoing CABG had a slightly larger benefit than women with respect to outcomes.18 We assessed interactions and found a statistically significant interaction between gender and age on the primary outcome death. We graphed this interaction over the age spectrum, stratified by gender, and found that women less than 65 years of age did slightly worse than men, whereas women over the age of 65 years did slightly better (Figure 2). When the graph‐predicted mortality was restricted to only those who underwent CABG (Figure 3), we found that the relative risk in women was uniform throughout the age spectrum, whereas the risk to men was materially different before and after 65 years of age. This finding perhaps sheds light on the Chang study18 that found the benefit of CABG in men may be related through the effect of age. Although there appears to be a biological basis for this finding, interpretation should be done cautiously and findings validated in future studies. Some hypotheses for this finding may be that physicians chose the revascularization modality based on the extent of comorbidities after an assessment of frailty, angiographic characteristics (size of coronary arteries and extent of coronary artery disease), and/or personal wishes by individual patients. We were not able to capture in this study any covariates that represented frailty, the angiographic characteristics mentioned above, or personal wishes that perhaps would have been able to further refine our model.
Prior studies have noted an increased number of baseline comorbidities in women when compared to men.1, 2, 5 The BMC2 (Blue Cross Blue Shield of Michigan Cardiovascular Consortium) study22 included 22 725 patients with normal renal function and showed that, despite an increased baseline comorbidity profile, 5‐year outcomes were similar. Our finding of an increased baseline comorbidity profile in the ESRD cohort should not be surprising. We expanded on this initial finding and assessed how baseline comorbidities were related to age when stratified by gender. As shown in Figure 1, although the overall number of comorbidities decreased as age at index revascularization increased, women continued to have a higher number of comorbidities. Further work is needed to understand this interesting relationship between the number of baseline comorbidities, age, gender, and the type of revascularization chosen.
Limitations
Although not a true limitation, the generalizability of this study may be limited to integrated health systems. Despite having approximately 40% women in our study, the study could have been underpowered to detect small differences. We also did not know the specific indications that led to the initial coronary revascularization. This additional knowledge may have helped to gain further insight into mechanisms for the outcome.
Conclusion
We found that women with ESRD presented for their coronary revascularization procedure with a higher comorbidity profile than men. This differential comorbidity increased as a function of age. Despite this, women had equivalent cardiovascular outcomes compared to men. We also found that age had an effect modification on gender for the outcome all‐cause mortality with a trend toward younger women doing slightly worse than older women compared to men. This finding appeared to be even more evident when restricting the analysis to patients after CABG. The above findings will hopefully generate further interest and work in understanding the interactions of age and gender on coronary revascularization in patients with advanced kidney disease as well as in those with normal renal function.
Supporting information
Supporting Figure 1. Creation of the study cohort.
This work was funded by the Kaiser Permanente Northern California Community Benefit Grant and the Stanford‐Kaiser Permanente American Heart Association–Cardiovascular Outcomes Research Center (grant 0875162 N).
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Lansky AJ, Hochman JS, Ward PA, et al. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation. 2005;111:940–953. [DOI] [PubMed] [Google Scholar]
- 2. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:2610–2642. [DOI] [PubMed] [Google Scholar]
- 3. Jackson EA, Moscucci M, Smith DE, et al. The association of sex with outcomes among patients undergoing primary percutaneous coronary intervention for ST elevation myocardial infarction in the contemporary era: Insights from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2). Am Heart J. 2011;161:106–112.e101. [DOI] [PubMed] [Google Scholar]
- 4. Fox AA, Nussmeier NA. Does gender influence the likelihood or types of complications following cardiac surgery? Sem Cardiothorac Vasc Anesth. 2004;8:283–295. [DOI] [PubMed] [Google Scholar]
- 5. Lundberg G, King S. Coronary revascularization in women. Clin Cardiol. 2012;35:156–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim C, Redberg RF, Pavlic T, et al. A systematic review of gender differences in mortality after coronary artery bypass graft surgery and percutaneous coronary interventions. Clin Cardiol. 2007;30:491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stock EO, Redberg R. Cardiovascular disease in women. Curr Probl Cardiol. 2012;37:450–526. [DOI] [PubMed] [Google Scholar]
- 8. Kim ES, Menon V. Status of women in cardiovascular clinical trials. Arterioscler Thromb Vasc Biol. 2009;29:279–283. [DOI] [PubMed] [Google Scholar]
- 9. Pinn VW. Research on women's health: progress and opportunities. JAMA. 2005;294:1407–1410. [DOI] [PubMed] [Google Scholar]
- 10. Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516. [DOI] [PubMed] [Google Scholar]
- 11. BARI 2D Study Group ; Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360:2503–2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375–2384. [DOI] [PubMed] [Google Scholar]
- 13. Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census‐based methodology. Am J Public Health. 1992;82:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 15. Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. [DOI] [PubMed] [Google Scholar]
- 16. Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation. 2002;106:2207–2211. [DOI] [PubMed] [Google Scholar]
- 17. Shroff GR, Solid CA, Herzog CA. Long‐term survival and repeat coronary revascularization in dialysis patients after surgical and percutaneous coronary revascularization with drug‐eluting and bare metal stents in the united states. Circulation. 2013;127:1861–1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chang TI, Shilane D, Kazi DS, et al. Multivessel coronary artery bypass grafting versus percutaneous coronary intervention in ESRD. J Am Soc Nephrol. 2012;23:2042–2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vittinghoff DG, Glidden DV, Shiboski SC, et al. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. 2nd ed New York, NY: Springer; 2012. [Google Scholar]
- 20.Centers for Disease Control and Prevention. Women's health. Leading causes of death in females. http://www.cdc.gov/women/lcod. Accessed March 25, 2014.
- 21. Coca SG, Krumholz HM, Garg AX, et al. Underrepresentation of renal disease in randomized controlled trials of cardiovascular disease. JAMA. 2006;296:1377–1384. [DOI] [PubMed] [Google Scholar]
- 22. Duvernoy CS, Smith DE, Manohar P, et al. Gender differences in adverse outcomes after contemporary percutaneous coronary intervention: an analysis from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) percutaneous coronary intervention registry. Am Heart J. 2010;159:677–683.e671. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Figure 1. Creation of the study cohort.


