ABSTRACT
Background
An increased serum glucose level in patients with acute coronary syndrome (ACS) is associated with adverse clinical outcome. This hyperglycemia has been attributed, at least in part, to acute stress reaction. Our objective was to determine whether hyperglycemia is a stress‐related phenomenon or whether it represents a more sustained and possibly significant background dysglycemia.
Hypothesis
Hyperglycemia in patients undergoing coronary angiography is related to background dysglycemia.
Methods
Blood samples were obtained at the time of cardiac catheterization. Patients with hemoglobin A1c >6.5% were excluded to avoid patients with chronic glucose levels above 135 mg/dL. A logistic regression model was created to assess the influence of different variables on hyperglycemia (glucose levels above 140 mg/dL). We also evaluated the effect of glucose levels above 140 mg/dL on major adverse cardiovascular events (MACEs) up to 36 months.
Results
There were 2554 consecutive patients prospectively recruited. Serum glucose levels above 140 mg/dL was a strong predictor of MACE (hazard ratio: 2.2, 95% confidence interval [CI]: 1.3‐3.6, P = 0.002). Both diabetes mellitus and ACS were associated with hyperglycemia (glucose levels above 140 mg/dL). Nevertheless, the incidence of hyperglycemia was doubled in diabetic patients (odds ratio [OR]: 9.4, 95% CI: 3.9‐22.4, P < 0.001) compared with patients with ACS (OR: 4.6, 95% CI: 2.3‐9.0, P < 0.001). Combining both conditions was associated with a high likelihood of elevated glucose levels (OR: 15.5, 95% CI: 7.4‐32.9, P < 0.001).
Conclusions
Hyperglycemia in patients undergoing cardiac catheterization is a strong predictor of adverse outcome. It is mainly related to background dysglycemia and to a lesser extent to the acute stress accompanying ACS.
Introduction
Increased serum glucose concentrations in patients presenting with acute coronary syndrome (ACS) are associated with increased mortality.1 A potential pathophysiological link between increased serum glucose concentrations and adverse outcomes is related to the prothrombotic shift that appears during hyperglycemic states.2 Elevated glucose levels have been shown to be an independent predictor of early mortality, readmission, and ventricular systolic dysfunction in patients with ACS treated by percutaneous coronary intervention (PCI).3
It is unknown whether hyperglycemia at presentation to the catheterization laboratory is a transient stress‐related phenomenon or whether it represents a more sustained and significant background metabolic pathology. Such knowledge could single out patients with unidentified diabetes mellitus (DM). This type of information could have important prognostic value in terms of treatment strategies of patients undergoing coronary angiography.4 It could influence the type of stent used (bare metal vs. drug eluting) and the revascularization strategy chosen for the patient.5, 6, 7
The aim of the present study was to evaluate whether hyperglycemia at presentation to the catheterization laboratory is a stress‐related phenomenon or whether it represents a significant background dysglycemic disorder.
Methods
Study Design and Patient Selection
The data in this study were collected from the Tel Aviv Prospective Angiographic Survey (TAPAS). TAPAS is a prospective, single‐center registry that enrolls all patients undergoing cardiac catheterization at the Tel Aviv Medical Center.8, 9, 10, 11, 12, 13, 14 The current study cohort consists of consecutive patients referred for coronary angiography in our institution for various clinical presentations during 2008 to 2013. Excluded were patients with baseline hemoglobin A1c (HbA1c) above 6.5% (regardless of their diabetic status) to avoid patients with chronic glucose levels above 140 mg/dL, which would bias our analysis regarding possible causes of hyperglycemia.15 We included patients with HbA1c levels above 6.5% as a control group of patients with a significant and sustained background hyperglycemia.
All of the participants provided written informed consent for participation in the study, which was approved by the institutional ethics committee in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Definition of Cardiovascular Risk Factors
Diabetes mellitus (DM) was defined if the patient has been informed of having DM by a physician or was receiving hypoglycemic treatments (dietary, oral antidiabetic agents, or insulin).16
Hypertension was defined according to a medical history of elevated blood pressure on at least 2 separate occasions or the use of antihypertensive medications. Dyslipidemia was defined by medical history, the use of lipid‐lowering medications, or low‐density lipoprotein (LDL) concentrations >160 mg/dL in the fasting state. Smoking status was obtained from the medical history.
ACS status was established in patients with a clinical diagnosis of unstable angina or non–ST‐elevation myocardial infarction (STEMI) as defined by the attending physician according to current guidelines.17
Laboratory Tests
Arterial blood was obtained from all participants via the arterial access puncture sites as a part of the coronary angiography procedure. All of the patients underwent angiography after an overnight fast. Complete chemistry was analyzed using reagents, calibrators, and control materials from Bayer Diagnostics (Berkshire, UK) on the ADVIA 1650 (Siemens Healthcare, Erlangen, Germany).
Glucose Cutoffs
To evaluate which factors are associated with elevated glucose during cardiac catheterization, we used the well‐established cutoff that has been shown to have prognostic value and defined by the American Diabetes Association as above 140 mg/dL.15, 18, 19
Definition of a Clinical Cardiovascular Event
The primary end point of the study was the occurrence of a major cardiovascular event (MACE). MACE was defined as the composite rate of all‐cause mortality, myocardial infarction (MI), and stroke. The individual components of the composite end point were obtained by medical chart review and by regular telephone interviews up to 36 months following the index coronary angiography. The end of follow‐up for MACE outcome was defined as the first from the following events: MACE or January 1, 2013.
Statistical Analysis
Continuous variables are presented as mean and standard deviation or median and interquartile range, whereas categorical variables are displayed as number (percent) of patients within each group. Categorical data were compared using the χ2 test. The sample Kolmogorov‐Smirnov test and Q‐Q plots were used to test for normality of distributions. Continuous variables were compared using the independent sample t test or Mann‐Whitney test. We performed a logistic regression model using the hyperglycemia (glucose levels above 140 mg/dL) as the dependent variable. The potential confounders were variables with either known or suspected influence on glucose levels and included diabetic status, ACS status, as well as all variables found with P <0.1 in the univariate analysis, and other established risk factors and universal confounders. To compare the effect of DM and ACS status on hyperglycemia, we divided our population into 4 groups according to their ACS and diabetes status: group 1, patients without DM or ACS; group 2, patients without DM and with ACS; group 3, patients without ACS and with DM; and group 4, patients with both DM and ACS. Odds ratio (OR) with a 95% confidence interval (CI) were reported and presented by an illustration with x‐axis log scale using a metadata viewer version 1.04 (U.S. Department of Health & Human Services).
The influence of hyperglycemia on the composite MACE end point (MI, stroke, all‐cause mortality) was evaluated using multivariate Cox regression (backward method). All clinical features, biochemical variables, and potential confounders as presented in the Table were available for selection in this model (glucose levels above 140 mg/dL, history of DM, dyslipidemia, hypertension, age, gender, peripheral vascular disease, history of stroke/transient ischemic attack, history of ischemic heart disease, history of MI, history of coronary artery bypass grafting [CABG], troponin levels, high‐sensitivity C‐reactive protein, white blood cell, total cholesterol, triglycerides, LDL cholesterol, high‐density lipoprotein cholesterol, glomerular filtration rate, body mass index, ACS status, and number of diseased coronary arteries). Differences between patients with and without hyperglycemia was demonstrated using a survival curve. A 2‐tailed P value of <0.05 was considered significant for all analyses. All analyses were performed with the SPSS 19.0 software (IBM, Armonk, NY).
Table 1.
Clinical Characteristics of the Study Population
| Glucose Below 140 mg/dL, n = 2252 | Glucose Above 140 mg/dL, n = 135 | P Value | |
|---|---|---|---|
| Age, y (range) | 65 ± 13 (24–95) | 67 ± 13 (31–91) | 0.08 |
| Males | 1613 (72%) | 92 (68%) | 0.44 |
| BMI | 27 ± 4.5 | 27 ± 4.2 | 0.85 |
| Diabetes | 273 (12%) | 49 (36%) | <0.001 |
| Current smokers | 568 (25%) | 30 (22%) | 0.44 |
| Hypertension | 1402 (62%) | 91 (67%) | 0.23 |
| Dyslipidemia | 1483 (66%) | 88 (65%) | 0.874 |
| Ischemic heart disease | 1008 (45%) | 60 (44%) | 0.94 |
| Prior stroke | 229 (10%) | 16 (12%) | 0.53 |
| Prior CABG | 300 (13%) | 15 (11%) | 0.46 |
| Indications for coronary angiography | |||
| MI | 798 (35%) | 86 (64%) | <0.001 |
| Unstable angina | 609 (27%) | 22 (16%) | |
| Stable angina | 845 (38%) | 27 (20%) | |
| Medications | |||
| ACE inhibitors | 983 (44%) | 48 (36%) | 0.07 |
| Aspirin | 1865 (83%) | 110 (82%) | 0.69 |
| β‐blockers | 1362 (61%) | 57 (42%) | <0.001 |
| Clopidogrel | 898 (40%) | 53 (39%) | 0.89 |
| Angiotensin receptor blockers | 184 (8%) | 11 8%) | 0.99 |
| Statins | 1545 (69%) | 66 (49%) | <0.001 |
| Oral hypoglycemics | 147 (6.5%) | 33 (24%) | <0.001 |
| Insulin | 14 (1%) | 7 (5%) | <0.001 |
| Laboratory | |||
| High‐sensitivity C‐reactive protein | 10 ± 24 | 12 ± 27 | 0.84 |
| Total cholesterol | 168 ± 39 | 172 ± 36 | 0.24 |
| Triglycerides | 131 ± 81 | 111 ± 63 | <0.001 |
| Low‐density lipoprotein | 100 ± 33 | 107 ± 34 | 0.01 |
| High‐density lipoprotein | 42 ± 12 | 43 ± 12 | 0.4 |
| Hemoglobin A1c | 5.7 ± 0.4 | 5.9 ± 0.4 | <0.001 |
| Troponin, pg/dL | 2.5 ± 8.7 (0.01‐0.69) | 2.3 ± 7.5 (0.03‐0.95) | 0.87 |
| Coronary artery disease severity | |||
| 0 vessel | 541 (24%) | 18 (10%) | 0.001 |
| 1 vessel | 490 (22%) | 35 (26%) | |
| 2 vessel | 537 (24%) | 29 (22%) | |
| 3 vessel/LM | 674 (30%) | 53 (39%) |
Abbreviations: ACE, angiotensin‐converting enzyme; BMI, body mass index; CABG, coronary artery bypass graft; LM, left main; MI, myocardial infarction.
Results
A total of 2554 consecutive patients were included in this study. The mean age was 66 ± 12 years (range, 25–92 years), and 73% were males. Demographic data, clinical characteristics, and medications used by the study population are shown in the Table, according to the 140 mg/dL glucose cutoff. The incidence of MI at presentation was higher in patients with hyperglycemia (64% vs 35%, P < 0.001), and so was the incidence of diabetes (36% vs 12%, P < 0.001). Patients with hyperglycemia had more advanced coronary artery disease and were more often treated by PCI (67% vs 28%, P < 0.001). Furthermore, patients with hyperglycemia were less often treated with evidence‐based medications (β‐blockers, statins), and as expected, they used more oral hypoglycemic medications compared to patients with no hyperglycemia.
Glucose Levels and Outcome
During the follow‐up period (median; 424 days; range, 1–1435 days), a total of 262 MACEs were recorded. There were 53 (2%) patients with myocardial infarction, another 30 (1%) patients suffered from a stroke, and 179(7%) patients died. Similar to previous reports, glucose levels above 140 mg/dL was a strong predictor of adverse outcome (hazard ratio: 2.2, 95% CI: 1.3‐3.6, P = 0.002). Figure 1 demonstrates the survival curves according to the 140 mg/dL cutoff.
Figure 1.
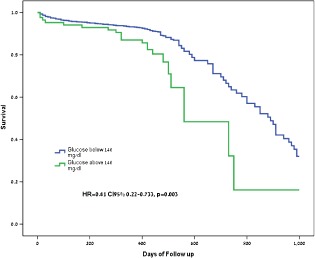
Survival in the entire cohort according to the glucose cutoff of above 140 mg/dL.
The cohort was divided into 4 groups as follows: group 1 included 695 patients without DM or ACS, group 2 included 1008 patients with ACS but without DM, group 3 included 293 patients with DM but without ACS, and group 4 included 558 patients with both DM and ACS.
DM and ACS Status in Patients With HbA1c <6.5%
Both DM and ACS were associated with hyperglycemia (glucose levels above 140 mg/dL). Nevertheless, the incidence of hyperglycemia was doubled in patients with DM (OR: 9.4, 95% CI: 3.9‐22.4, P < 0.001) compared to patients with ACS (OR: 4.6, 95% CI: 2.3‐9.0, P < 0.001). There was significant synergistic interaction between ACS and diabetic status as can be seen in Figure 2A. The presence of both conditions was associated with a high likelihood of hyperglycemia (glucose levels above 140 mg/dL) (OR: 15.5, 95% CI: 7.4‐32.9, P < 0.001) (Figure 2B).
Figure 2.
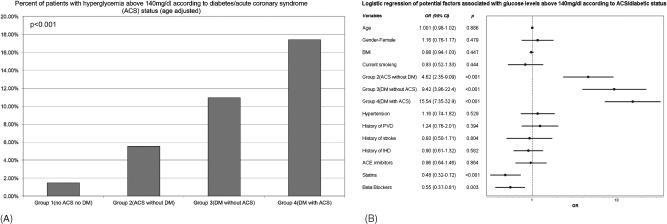
(A) Percent of patients with hyperglycemia above 140 mg/dL according to diabetes/acute coronary syndrome (ACS) status (age adjusted). (B) Logistic regression of potential factors associated with glucose levels above 140 mg/dL according to ACS/diabetic status. Abbreviations: ACE, angiotensin‐converting enzyme; BMI, body mass index; DM, diabetes mellitus; IHD, ischemic heart disease; PVD, peripheral vascular disease.
DM and ACS Status in Patients With HbA1c ≥6.5%
In the control group (HbA1c ≥6.5%), we recruited 1136 patients. Six hundred sixty‐nine patients had hyperglycemia (64%). Hyperglycemia was not affected by ACS status in patients without known DM (OR: 2.86, 95% CI: 0.29‐27.8, P = 0.37). However, hyperglycemia was strongly associated with background DM (OR: 13.56, 95% CI: 1.79‐102.7, P = 0.011). Similarly, there was significant synergistic interaction between ACS and diabetic status on hyperglycemia (OR: 21.8, 95% CI: 2.8‐164.6, P = 0.003).
Discussion
The main finding of the present study was that in patients with HbA1c lower than 6.5% presenting for cardiac catheterization, hyperglycemia (defined as glucose levels above 140 mg/dL) is related to the patients' background dysglycemic status.
Many studies have demonstrated a significant and independent relationship between elevated serum glucose levels and increased risk of mortality and other adverse clinical outcomes in patients with ACS.1, 19 These studies have evaluated glucose levels in patients without excluding patients with chronic elevation of glucose levels (manifested by elevated HbA1c levels). Our study is novel by its selection of a normoglycemic population and demonstrating the importance of hyperglycemia in this selected population.
Hyperglycemia has also been associated with “no‐reflow phenomenon” following PCI, greater infarct size, worse left ventricular systolic function, and acute kidney injury.20 In addition, we demonstrated that patients with hyperglycemia had more advanced coronary artery disease and were more often treated by PCI. Elevated glucose level during stress is a consequence of sympathetic nervous system activity and overproduction of catecholamines and cortisol, which encourage processes of gluconeogenesis, glycogenolysis, and lipolysis.21
Zhang et al.22 examined the results of 853 patients who were treated by primary PCI for STEMI without DM. Patients with admission serum glucose over 180 mg/dL experienced a significantly higher incidence of mortality, stent thrombosis and composite MACE, and these findings correlate with our results. We add to their study by demonstrating the causes of hyperglycemia as well as the adverse effect of lower glucose levels (140 mg/dL).
The results of the present study show that the ACS status contributes less to the serum glucose levels compared with the chronic dysglycemic state of the patient as expressed by diabetes mellitus. It is conceivable that patients with ACS are more stressed than non‐ACS patients, and this is also true for the intensity of their inflammatory response. Nevertheless, as shown in Figure 2, the ACS status itself had a smaller influence on the glucose concentrations compared with DM status. The association of hyperglycemia with background diabetic status was also examined in the control group. The results were similar. Patients with hyperglycemia were mainly affected by background DM and less by their ACS status.
Our findings support the idea that the elevation of the glucose levels seen in patients with hyperglycemia might have started some time prior to the day of cardiac catheterization, because their HbA1c levels were already relatively elevated when they presented for the procedure (mean, 5.9 ± 0.4 vs 5.7 ± 0.4, P < 0.001). This finding is substantiated by the more advanced coronary artery disease in patients presenting with hyperglycemia.23
Hyperglycemia in the catheterization laboratory is usually explained as an acute stress reaction especially in ACS patients.4 The idea that patients with glucose levels above 140 mg/dL have a high likelihood of diabetes mellitus should be considered, because it might alter the treatment plan for these patients. Patients with diabetes are more likely to receive drug‐eluting stents and undergo CABG compared to patients without diabetes.5, 7 Therefore, patients with hyperglycemia during coronary angiography should be screened for diabetes/metabolic syndrome.4, 15, 23, 24, 25
Conclusion
Hyperglycemia in patients undergoing cardiac catheterization is a strong predictor for adverse outcome. It is mainly related to background dysglycemia and to a lesser extent to the acute stress accompanying ACS.
Limitations
Our study is comprised of patients referred for coronary angiography, and therefore might suffer from selection bias. Furthermore, our group of patients with glucose levels above 140 mg/dL is relatively small, because they all had HbA1c <6.5%.
All of the authors contributed to the study by conception and design (Y.A., H.S., A.H., S.B., S.B., I.S.), collection of the data (A.H., I.H., A.S., G.K., A.F., S.B.), and revision (Y.A., H.S., S.B.) of the manuscript.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. De Caterina R, Madonna R, Sourij H, et al. Glycaemic control in acute coronary syndromes: prognostic value and therapeutic options. Eur Heart J. 2010;31:1557–1564. [DOI] [PubMed] [Google Scholar]
- 2. Lemkes BA, Hermanides J, Devries JH, et al. Hyperglycemia: a prothrombotic factor? J Thromb Haemost. 2010;8:1663–1669. [DOI] [PubMed] [Google Scholar]
- 3. Hoebers LP, Damman P, Claessen BE, et al. Predictive value of plasma glucose level on admission for short and long term mortality in patients with ST‐elevation myocardial infarction treated with primary percutaneous coronary intervention. Am J Cardiol. 2012;109:53–59. [DOI] [PubMed] [Google Scholar]
- 4. Timmer JR, Hoekstra M, Nijsten MW, et al. Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST‐segment‐elevation myocardial infarction treated with percutaneous coronary intervention. Circulation. 2011;124:704–711. [DOI] [PubMed] [Google Scholar]
- 5. Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary‐artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–972. [DOI] [PubMed] [Google Scholar]
- 6. Ryden L, Standl E, Bartnik M, et al. Guidelines on diabetes, pre‐diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J. 2007;28:88–136. [DOI] [PubMed] [Google Scholar]
- 7. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio‐Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI) , Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501–2555. [DOI] [PubMed] [Google Scholar]
- 8. Arbel Y, Sternfeld A, Barak A, et al. Inverse correlation between coronary and retinal blood flows in patients with normal coronary arteries and slow coronary blood flow. Atherosclerosis. 2014;232:149–154. [DOI] [PubMed] [Google Scholar]
- 9. Arbel Y, Halkin A, Finkelstein A, et al. Impact of estimated glomerular filtration rate on vascular disease extent and adverse cardiovascular events in patients without chronic kidney disease. Can J Cardiol. 2013;29:1374–1381. [DOI] [PubMed] [Google Scholar]
- 10. Arbel Y, Birati EY, Finkelstein A, et al. Platelet inhibitory effect of clopidogrel in patients treated with omeprazole, pantoprazole, and famotidine: a prospective, randomized, crossover study. Clin Cardiol. 2013;36:342–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Steinvil A, Banai S, Leshem‐Rubinow E, et al. The development of anemia of inflammation during acute myocardial infarction. Int J Cardiol. 2012;156:160–164. [DOI] [PubMed] [Google Scholar]
- 12. Arbel Y, Finkelstein A, Halkin A, et al. Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography. Atherosclerosis. 2012;225:456–460. [DOI] [PubMed] [Google Scholar]
- 13.Steinvil A, Arbel Y, Leshem‐Rubinow E, et al. Erythrocyte aggregation portends worse outcomes in unstable angina patients undergoing percutaneous coronary interventions. Clin Hemorheol Microcirc. 2013;55(2):213–221. [DOI] [PubMed] [Google Scholar]
- 14. Arbel Y, Rind E, Banai S, et al. Prevalence and predictors of slow flow in angiographically normal coronary arteries. Clin Hemorheol Microcirc. 2012;52:5–14. [DOI] [PubMed] [Google Scholar]
- 15. Nathan DM, Kuenen J, Borg R, et al. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31:1473–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. American Diabetes Association . Standards of medical care in diabetes—2007. Diabetes Care. 2007;30(suppl 1):S4–S41. [DOI] [PubMed] [Google Scholar]
- 17. ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction): Developed in Collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–e304. [DOI] [PubMed] [Google Scholar]
- 18. Deedwania P, Kosiborod M, Barrett E, et al. Hyperglycemia and acute coronary syndrome: a scientific statement from the American Heart Association Diabetes Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2008;117:1610–1619. [DOI] [PubMed] [Google Scholar]
- 19. Kosiborod M, McGuire DK. Glucose‐lowering targets for patients with cardiovascular disease: focus on inpatient management of patients with acute coronary syndromes. Circulation. 2010;122:2736–2744. [DOI] [PubMed] [Google Scholar]
- 20. Iwakura K, Ito H, Ikushima M, et al. Association between hyperglycemia and the no‐reflow phenomenon in patients with acute myocardial infarction. J Am Coll Cardiol. 2003;41:1–7. [DOI] [PubMed] [Google Scholar]
- 21. Mladenovic V, Zdravkovic V, Jovic M, et al. Influence of admission plasma glucose level on short‐ and long‐term prognosis in patients with ST‐segment elevation myocardial infarction. Vojnosanit Pregl. 67:291–295. [DOI] [PubMed] [Google Scholar]
- 22. Zhang JW, Zhou YJ, Cao SJ, et al. Impact of stress hyperglycemia on in‐hospital stent thrombosis and prognosis in nondiabetic patients with ST‐segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coron Artery Dis. 2013;24:352–356. [DOI] [PubMed] [Google Scholar]
- 23. Arbel Y, Zlotnik M, Halkin A, et al. Admission glucose, fasting glucose, HbA1c levels and the SYNTAX score in non‐diabetic patients undergoing coronary angiography. Clin Res Cardiol. 2014;103:223–227. [DOI] [PubMed] [Google Scholar]
- 24. Wexler DJ, Nathan DM, Grant RW, et al. Prevalence of elevated hemoglobin A1c among patients admitted to the hospital without a diagnosis of diabetes. J Clin Endocrinol Metab. 2008;93:4238–4244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Noto D, Barbagallo CM, Cefalu AB, et al. The metabolic syndrome predicts cardiovascular events in subjects with normal fasting glucose: results of a 15 years follow‐up in a Mediterranean population. Atherosclerosis. 2008;197:147–153. [DOI] [PubMed] [Google Scholar]


