Abstract
Background:
Unprotected left main coronary artery (ULMCA) disease occurs in 3% to 5% of patients with coronary artery disease and is mainly treated by coronary artery bypass grafting (CABG) surgery. Drug‐eluting stents (DESs) have renewed interest for the percutaneous coronary intervention (PCI) treatment of ULMCA stenosis. This study compared the long‐term clinical outcome of PCI with DESs or CABG in real world patients with ULMCA disease.
Hypothesis:
PCI with DESs may be a better treatment for ULMCA disease compared with CABG.
Methods:
Consecutive patients who had coronary revascularization because of ULMCA disease in Zhongshan Hospital, from May 2003 to November 2009, were retrospectively enrolled. They were classified in the PCI or the CABG group according to treatments that were given initially. Of 515 patients having follow‐up data, 233 were treated by PCI, whereas 282 were treated by CABG. The patients in the CABG group were of older age, had higher European System for Cardiac Operative Risk Evaluation (EuroSCORE) and Synergy Between PCI With Taxus Drug‐Eluting Stent and Cardiac Surgery (SYNTAX) scores, and had longer hospitalization stays than the PCI group.
Results:
At the end of follow‐up, there was no difference in major adverse cardiac and cerebrovascular events between the 2 groups. However, the incidence of cardiac death (0.4% vs 4.6%) in the PCI group was less than that in the CABG group, whereas target vessel revascularization (7.3% vs 3.2%) was higher in the PCI group.
Conclusions:
In ULMCA disease, CABG tends to be chosen in patients with higher risk according to the EuroSCORE and SYNTAX scores. PCI with DESs seemed to have favorable early and long‐term clinical outcomes compared with CABG in our center. Clin. Cardiol. 2012 DOI: 10.1002/clc.22070
Qing Qin, MD, and Juying Qian, MD, contributed equally to this work.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Unprotected left main coronary artery (ULMCA) disease occurs in 3% to 5% of patients with coronary artery disease and is the subject of intense investigation. Coronary artery bypass grafting (CABG) surgery is considered the standard of care for the treatment of ULMCA stenosis according to current guidelines.1, 2 However, continued technical evolution of percutaneous coronary intervention (PCI), especially the introduction of drug‐eluting stents (DESs), has renewed interest for the percutaneous treatment of ULMCA stenosis. Several studies have shown the feasibility and the favorable midterm outcomes of PCI with DESs.3, 4 It seems that both PCI and CABG had similar long‐term mortality; however, PCI with stenting, even with DESs, was associated with higher rates of repeated revascularization than CABG.5, 6, 7 The aim of this study was to evaluate the early and long‐term clinical outcome of ULMCA treated by PCI with DESs or CABG in real‐world patients, as well as to indicate the factors that may be associated with the outcome of patients with ULMCA disease.
Methods
Patient Population and Follow‐up
Consecutive patients who had coronary revascularization either by PCI with DESs or by CABG because of ULMCA disease, in the database of Zhongshan Hospital from May 2003 to November 2009, were retrospectively enrolled. ULMCA disease was defined as >50% diameter stenosis in a quantitative coronary angiogram with clinical indications of revascularization such as ischemic evidence or intravascular ultrasound report (minimum lumen area <6.0 mm2). Patients with patent graft to the left anterior descending artery or left circumflex artery were excluded. Patients with previous stenting in any coronary artery were not excluded. The decision for PCI or CABG was based on the surgical risk and the preference of patients and/or doctors. The patients were classified as PCI group or CABG group according to the initial treatment in the hospital. The baseline clinical data and in‐hospital outcome were obtained by chart‐record review. The surgical risk of the patient was evaluated according to the European System for Cardiac Operative Risk Evaluation (EuroSCORE).8 All of the initial coronary angiograms of the enrolled patients were reviewed, and the severity of coronary artery disease was evaluated using the recently published Synergy Between PCI with Taxus Drug‐Eluting Stent and Cardiac Surgery (SYNTAX) score.9 During follow‐up, a coronary angiogram was performed only if clinically indicated. Long‐term outcome of the patients was obtained by the outpatient clinical follow‐up or telephone interview. The study was approved by the local hospital ethics committee.
Procedural Characteristics
All surgical and percutaneous procedures were performed in a standard fashion by the same interventionalist and surgical team. All patients treated with PCI were premedicated with 300 mg aspirin and 300 mg clopidogrel the night before the procedure, and during the procedure unfractionated heparin was given (80–100 U/kg) and 2000 U for every extra hour. The use of glycoprotein IIb/IIIa inhibitor was left to the operator's discretion. PCI procedures were done with either a femoral or radial approach, and only DESs were used. Different stenting techniques for left main coronary artery (LMCA) bifurcation lesions were decided by the operators according to the actual angiographic findings. Simple stenting techniques were preferred over complicated techniques. Predilation of the side branch (SB) was a criterion of the operators. After main vessel stent implantation, the origin of the SB was carefully evaluated, and in cases of no compromise the procedure was finished. On the contrary, if significant stenosis of the SB ostium remained, the SB was then rewired, and balloon dilation of the ostium was performed across the metal structure of the stent. Stenting of the SB origin was considered in the presence of residual stenosis >50%, with obvious dissection which may slow blood flow or lead to acute vascular occlusion or a coronary thrombolysis in myocardial infarction flow <3. Final kissing balloon techniques were required in all patients with LMCA bifurcation involvement. Cardiac enzymes were not measured routinely unless there was a clinical suspicion of ischemia and therefore was not a designated outcome of the study. The poststenting antiplatelet regimen included lifetime aspirin of 100 mg/day if without contraindications and clopidogrel 75 mg/day for at least 12 months after the procedure, and the patients were recommended to take dual antiplatelet agents as long as possible.
For those patients taking aspirin and clopidogrel, surgery was delayed to 5 days after discontinuing clopidogrel. On‐ or off‐pump operation was decided by the operator according to the patient's characteristics. Left internal mammary artery grafts (LIMA) were the first choice in the operation. The use of an intra‐aortic balloon pump was left to the operator's discretion. Aspirin was recommended for life and clopidogrel for 12 months after the procedure. Cardiac enzymes were not measured routinely unless there was a clinical suspicion of ischemia.
In both groups of patients, other medicines including the angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker, β‐blocker, calcium antagonist, or statins were used according to the clinical indications.
Study End Points and Definitions
The primary end point of the study was the long‐term incidence of a major adverse cardiac and cerebrovascular event (MACCE), including the composite of death, nonfatal myocardial infarction (MI), target vessel revascularization (TVR), or cerebral events. The secondary end point was the rate of the individual MACCE. Death was attributed to cardiac death unless proven otherwise. Nonfatal MI was defined as ischemia symptom, ischemic electrocardiogram changes, and an increase of cardiac biomarkers, either creatine phosphokinase isoenzyme MB or troponin, to 3 times higher than the upper limit of normal after PCI and 5 times higher after CABG. TVR was defined as any repeated revascularization in the left anterior descending artery or left circumflex artery as well as in the target segment. Cerebral events included both ischemic and hemorrhagic stroke and transient ischemic attack.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation and were compared by Student ttest. Categorical variables were presented as counts, and percentages and were compared by χ 2 test or Fisher exact test, as appropriate. The Kaplan‐Meier method was used to show long‐term event‐free survival curves, and differences between groups were analyzed with the log‐rank test. Independent predictors of MACCE at long‐term follow‐up were analyzed using the Cox proportional hazards regression model. Noncorrelated variables with P < 0.05 on univariate analyses, as well as the method of revascularization (stent or surgery), were included in the multivariate analysis. Statistical analysis was performed using commercially available software (SPSS 13 for Windows; IBM, Armonk, NY). A P value of <0.05 was considered statistically significant.
Results
Patient Characteristics
A total of 595 consecutive patients who had coronary revascularization either by PCI with DESs or by CABG because of ULMCA disease in Zhongshan Hospital from May 2003 to November 2009 were retrospectively enrolled. Of them, 80 (13.4%) were lost to follow‐up (45 in the PCI group and 35 in the CABG group) and were excluded from the study. The remaining 515 patients comprised the study population. PCI was performed in 233 patients, whereas CABG was performed in 282 patients. Baseline clinical and angiographic characteristics are listed in Table 1. Compared with PCI group, the CABG group included patients with older age (66.7 ± 8.3 vs 64.9 ± 10.5 years old, P = 0.031), more hypertension (69.1% vs 56.7%, P = 0.003), lower left ventricular ejection fraction (61.6 ± 10.5% vs 65.1 ± 9.1%, P = 0.001), higher EuroSCORE (4.5 ± 2.6 vs 3.7 ± 2.3, P < 0.001) and SYNTAX score (34.5 ± 12.0 vs 24.1 ± 10.5, P < 0.001), and longer hospitalizations (20.5 ± 10.8 vs 8.9 ± 5.3 days, P < 0.001). However, as for the percentage of patients whose EuroSCORE was ≥6, an indication of high risk during surgery, there was no difference between the 2 groups. The PCI group had a higher prior PCI rate (30.5% vs 9.2%, P < 0.001). There were fewer patients who had left main and 3‐vessel disease in the PCI group than in the CABG group (13.7% vs 61.3%, P < 0.001). Left main bifurcation lesions were more common in the CABG group (75.5%) than in the PCI group (66.5%) but with no statistical significance.
Table 1.
Baseline Clinical and Angiographic Characteristics
| Variable | PCI, n = 233 | CABG, n = 282 | P Value |
|---|---|---|---|
| Age, y | 64.9 ± 10.5 | 66.7 ± 8.3 | 0.031 |
| Male gender (%) | 197 (84.5) | 246 (87.2) | 0.382 |
| Hypertension (%) | 132 (56.7) | 195 (69.1) | 0.003 |
| Diabetes (%) | 57 (24.5) | 77 (27.3) | 0.464 |
| Hyperlipidemia (%) | 82 (35.2) | 113 (40.1) | 0.256 |
| Smoking (%) | 112 (48.1) | 133 (47.2) | 0.838 |
| Prior myocardial infarction (%) | 56 (24) | 57 (20.2) | 0.297 |
| Prior PCI (%) | 71 (30.5) | 31 (9.2) | <0.001 |
| Prior CABG | 2 | 0 | |
| Body mass index, kg/m2 | 23.8 ± 3.0 | 24.5 ± 2.9 | 0.016 |
| eGFR, mL/min/1.73 m2 | 76.4 ± 23.8 | 73.4 ± 23.1 | 0.189 |
| Ejection fraction, % | 65.1 ± 9.1 | 61.6 ± 10.5 | 0.001 |
| Ejection fraction <40% (%) | 10 (4.3) | 23 (8.2) | 0.075 |
| Clinical diagnosis before angiography | 0.01 | ||
| Stable angina (%) | 57 (24.5) | 80 (28.4) | |
| Unstable angina (%) | 137 (58.8) | 125 (44.3) | |
| NSTEMI (%) | 18 (7.7) | 47 (16.7) | |
| STEMI (%) | 7 (3) | 7 (2.5) | |
| Subacute MI (%) | 8 (3.4) | 13 (4.6) | |
| Other (%) | 6 (2.6) | 10 (3.5) | |
| NYHA class | 0.05 | ||
| I (%) | 17 (7.3) | 14 (5.0) | |
| II (%) | 169 (72.5) | 182 (64.5) | |
| II I (%) | 44 (18.9) | 79 (28.0) | |
| IV (%) | 3 (1.3) | 7 (2.5) | |
| EuroSCORE | 3.7 ± 2.3 (0 –11) | 4.5 ± 2.6 (0 –17) | <0.001 |
| EuroSCORE ≥6 | 57 (24.5) | 88 (31.2) | 0.09 |
| Stenotic vessel | <0.001 | ||
| Left main coronary only (%) | 36 (15.5) | 7 (2.5) | |
| Left main coronary and 1 vessel (%) | 84 (36.1) | 29 (10.3) | |
| Left main coronary and 2 vessel (%) | 81 (34.8) | 73 (25.9) | |
| Left main coronary and 3 vessel (%) | 32 (13.7) | 173 (61.3) | |
| Location of left main | 0.061 | ||
| Ostium (%) | 48 (20.6) | 41 (14.5) | |
| Shaft (%) | 25 (10.7) | 19 (6.7) | |
| Bifurcation (%) | 155 (66.5) | 213 (75.5) | |
| Diffuse (%) | 3 (1.3) | 8 (2.8) | |
| Occlusion from ostium (%) | 2 (0.9) | 1 (0.4) | |
| SYNTAX score | 24.1 ± 10.5 | 34.5 ± 12.0 | <0.001 |
| Average hospital stay, d | 8.9 ± 5.3 | 20.5 ± 10.8 | <0.001 |
Abbreviations: CABG, coronary artery bypass grafting; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; NSTEMI, non–ST‐segment elevation myocardial infarction; NYHA, New York Heart Association; PCI, percutaneous coronary intervention; STEMI, ST‐segment elevation myocardial infarction.
Procedural Findings and Complications
Detailed information of procedural findings and complications is shown in Table 2. In the PCI group, lesions involving bifurcation were most often treated by 1 stent cross‐over (80.2%), and crush technique accounted for 13.9%, whereas T, V, or Cullotte stenting techniques 10 were seldom used (3.7%, 0.5%, 1.6%, respectively). Other procedural‐related complications included 2 cases of side branch occlusion, 3 cases of no/slow reflow, 1 case of acute thrombosis, 1 case of vascular perforation, and 1 case of acute heart failure. In the CABG group, 232 (82.3%) patients underwent off‐pump CABG. LIMA was used in 222 (78.7%) cases of all CABG patients. Nine patients in the CABG group suffered from renal failure that needed dialysis, and 10 patients suffered from abnormal liver enzyme elevation of more than 2‐fold the upper limit of aspartate aminotransferase or alanine aminotransferase after surgery. Other procedural‐related complications included 3 cases of severe infection needing surgery, 2 cases of hemorrhage needing surgery, and 1 case of distal embolization of the lower extremities. No renal failure, liver enzyme abnormality, severe infection, or hemorrhage was detected in the PCI group.
Table 2.
Procedural Findings and Complications
| PCI group, n = 233 | |
|---|---|
| Stenting techniques for left main bifurcations (n = 187) | |
| Crossover (%) | 150 (80.2) |
| Crush (%) | 26 (13.9) |
| T stent (%) | 7 (3.7) |
| Cullotte (%) | 1 (0.5) |
| V stent (%) | 3 (1.6) |
| Stent type and number (n = 233) | |
| Sirolimus‐eluting stent | 160 (68.7) |
| Paclitaxel‐eluting stent | 58 (24.9) |
| Zotarolimus‐eluting stent | 15 (6.4) |
| No. of used stents at left main lesion | 1.09 ± 0.33 |
| Complications (n = 233) | |
| Side branch occlusion (%) | 2 (0.9) |
| No/slow reflow (%) | 3 (1.3) |
| Acute thrombosis (%) | 1 (0.4) |
| Vascular perforation (%) | 1 (0.4) |
| Acute heart failure (%) | 1 (0.4) |
| CABG group (n = 282) | |
| Procedures | |
| Off‐pump (%) | 232 (82.3) |
| On‐pump (%) | 50 (17.7) |
| CABG with other cardiac surgery (%) | 21 (7.4) |
| Left internal mammary artery (%) | 222 (78.7) |
| Complications | |
| Blood transfusion (%) | 126 (44.7) |
| Renal failure needs emergent dialysis (%) | 9 (1.1) |
| Abnormal liver enzyme (%)a | 10 (3.5) |
| Severe infection needs operation (%) | 3 (1.1) |
| Hemorrhage needs operation (%) | 2 (0.7) |
| Distal embolization (%) | 1 (0.4) |
Abbreviations: CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention.
Abnormal liver enzyme is defined as more than 2‐fold the upper limit of aspartate aminotransferase or alanine aminotransferase.
Clinical Outcome at Follow‐up
Clinical outcomes at follow‐up are shown in Table 3.
Table 3.
Short‐ and Long‐term Clinical Outcomes of the Study Groups
| PCI Group, n = 233 | CABG Group, n = 282 | P Value | |
|---|---|---|---|
| In‐hospital outcomes | |||
| Death (%) | 1 (0.4) | 8 (2.8) | 0.045 |
| Cardiac death (%) | 1 (0.4) | 7 (2.5) | 0.078 |
| MI (%) | 0 | 1 (0.4) | |
| TVR (%) | 0 | 1 (0.4) | |
| Stroke (%) | 1 (0.4) | 2 (0.7) | |
| MACCE (%) | 2 (0.9) | 10 (3.5) | 0.074 |
| 30‐day outcomes | |||
| Death (%) | 1 (0.4) | 11 (3.9) | 0.009 |
| Cardiac death (%) | 1 (0.4) | 9 (3.2) | 0.026 |
| MI (%) | 2 (0.9) | 1 (0.4) | 0.592 |
| TVR (%) | 0 | 1 (0.4) | |
| Stroke (%) | 1 (0.4) | 3 (1.1) | 0.630 |
| MACCE (%) | 4 (1.7) | 14 (5.0) | 0.046 |
| Long‐term outcomes | |||
| Death (%) | 4 (1.7) | 18 (6.4) | 0.01 |
| Cardiac death (%) | 1 (0.4) | 13 (4.6) | 0.004 |
| Non‐fatal MI (%) | 3 (1.3) | 3 (1.1) | 0.835 |
| TVR (%) | 17 (7.3) | 9 (3.2) | 0.026 |
| Stroke (%) | 7 (3.0) | 18 (6.4) | 0.056 |
| MACCE (%) | 29 (12.4)a | 46 (18.4)a | 0.229 |
Abbreviations: CABG, coronary artery bypass grafting; MACCE, major adverse cardiac and cerebrovascular event; MI, myocardial infarction; PCI, percutaneous coronary intervention; TVR, target vessel revascularization.
In the PCI group, 1 patient suffered from both stroke and TVR, and 1 patient died of stroke. In the CABG group, 1 patient suffered from MI and had TVR, and 1 patient died of stroke.
In‐Hospital and 30‐Day Clinical Outcomes
The CABG group showed more adverse events during hospital stay, and the 2 groups differed in death (2.8% vs 0.4%, P = 0.045). Thirty‐day results indicated that patients in the CABG group had a significantly higher incidence of MACCE (5.0% vs 1.7%, P = 0.046), cardiac death (3.2% vs 0.4%, P = 0.026), and death (3.9% vs 0.4%, P = 0.009) than those in PCI group (Table 3). The only patient who died in the PCI group had a bicuspid aortic valve whose echocardiography showed pulmonary artery systolic pressure of 71 mm Hg. His EuroSCORE was 8 and SYNTAX score was 31 before the PCI procedure. The angiogram showed left main bifurcation and 3‐vessel disease. Five DESs were implanted. The patient died 11 days after surgery because of heart failure. In the CABG group, 1 patient who suffered from angina 3 days after surgery underwent emergency PCI. A total occlusion of the saphenous vein graft was confirmed by angiogram and treated with DES implantation.
Long‐term Follow‐up
The mean follow‐up duration was 769 ± 492 days in the PCI group and 768 ± 529 days in the CABG group (P = 0.982). At the end of the follow‐up, the incidence of cardiac death and stroke in the PCI group was significantly less than the CABG group, whereas the incidence of TVR was more (Table 3). Kaplan‐Meier analysis showed lower cardiac death‐free survival (Figure 1, D, P = 0.004) and higher TVR‐free survival (Figure 1, C, P = 0.026) in the CABG group than the PCI group. However, Kaplan‐Meier analysis showed no difference in stroke‐free survival (Figure 1, B, P = 0.056) and MACCE‐free survival (Figure 1, A, P = 0.229) between the 2 groups.
Figure 1.
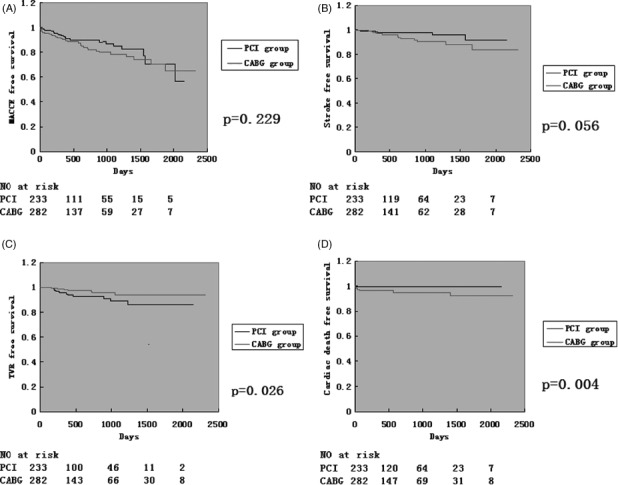
Kaplan‐Meier curves for outcomes in patients who underwent percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) therapy. (A) Major adverse cardiac and cerebrovascular event (MACCE)‐free survival. (B) Stroke‐free survival. (C) Target vessel revascularization (TVR)‐free survival. (D) Cardiac death‐free survival.
Predictors of Long‐term MACCE
The following variables were entered into a stepwise multivariable Cox proportional hazard model for MACCE‐free survival: age, gender, hypertension, diabetes mellitus, EuroSCORE, SYNTAX score, left ventricular ejection fraction, New York Heart Association (NYHA) class IV, left main and 3‐vessel disease, and CABG. The significant univariate predictors were left main and 3‐vessel disease, NYHA class IV, and EuroSCORE. In the final Cox model, the significant predictors of the hazard of MACCE were NYHA class IV and EuroSCORE. After analysis of MACCE‐free survival in the CABG and PCI group, separately in the same way, we found out that the independent predictors of the hazard of MACCE in the CABG group was NYHA class IV and EuroSCORE. In the PCI group, no independent predictors were found.
DISCUSSION
Our study showed a trend of lower risk of long‐term events (MACCE) after PCI compared with CABG. Although Kaplan‐Meier analysis did not show any benefit of survival in the PCI group over the CABG group, overall MACCE at the end of the follow‐up in the PCI and the CABG group showed this trend (MACCE 12.4% in PCI the group, 18.4% in the CABG group). Two studies published recently7, 11 compared the long‐term (5‐year for DES and 10‐year for bare metal stent [BMS]) prognosis of PCI and CABG in the treatment of ULMCA disease. They concluded that PCI with stent implantation (both DES and BMS) had similar long‐term mortality and rate of death, Q‐wave MI, or stroke compared with CABG. However, both DES and BMS implantation was associated with higher rates of repeat revascularization than CABG. The LMCA subgroup analysis of the SYNTAX trial9 and Seung et al12 came to a similar finding. Our results are consistent with these studies. However, cardiac death at the follow‐up manifested a significant difference between the 2 groups (0.4% in the PCI group, 4.6% in the CABG group, P = 0.001). As LIMA was used in 78.7% of patients undergoing CABG, which is below the usual percentage, this may be the cause for more cardiac death in the CABG group. The TVR percentage in this study is quite low compared with previous studies. Capodanno et al reported a TVR of 11.4% in the PCI group and 5.4% in the CABG group in a meta‐analysis of LMCA disease.13 Several factors may account for this. First, lesions of medium risk were selected in the PCI group, and physicians tend to treat complicated lesions by simple techniques. The average SYNTAX score in the PCI group was 24.1. It is in the medium risk group according to the SYNTAX trial. Over 80% of bifurcation lesions were treated by 1 stent crossing over the side branch. Second, we do not routinely perform an angiography follow‐up, and only 30.9% of patients come back for an angiogram because of symptom or personal will.
Although there was no significant difference in the incidence of stroke in the PCI and the CABG group (3.0% vs 6.4%, P = 0.056) at the end of follow‐ups, the Kaplan‐Meier analysis showed dissociation of 2 curves during long‐term follow‐up. We can conclude that there was a trend of more strokes in the CABG group, and that a bigger sample size is needed. Both the SYNTAX trial and the 5‐year group of Asan Medical Center‐Left Main Revascularization (ASAN‐MAIN) registry showed more strokes in the CABG group than the PCI group. Also, the meta‐analysis of 4 randomized clinical trials data published recently showed less cerebrovascular accident in the PCI group compared with the CABG group (0.1% vs 1.7%, P = 0.013) during a follow‐up time of 1 year.13 However, the 10‐year follow‐up group did not show this trend. There are many explanations for more cerebral events in the CABG group, including more aggressive antiplatelet therapy in the PCI group9 and cerebral ischemia during surgery.14 These may partly explain the high stroke occurrence during short‐term follow‐up, and a longer follow‐up time may diminish the difference in stroke between the 2 groups.
In our study, the CABG group had more short‐term complications within the first month after surgery (5.0% vs 1.7%, P = 0.046) compared with the PCI group. In the CABG group, cardiac death occurred more often than in the PCI group. About 82.3% patients in the CABG group underwent off‐pump CABG (OPCAB) in the study, which is different from a previous studies,6, 7 in which most CABG patients had on‐pump CABG (ONCAB). OPCAB for LMCA disease in selected patients is a common Chinese practice. Based on our previous experience and evidence from other centers,15, 16 OPCAB is safe and better than ONCAB in qualified patients. As our center has a team experienced in CABG, especially OPCAB, the difference in operation type selection may be only a minor factor of increased cardiac death instead of a major factor. During the long‐term follow‐up, however, TVR in the PCI group increased and became more than in the CABG group, and this led to no significant difference of MACCE between the 2 groups in the long run. This result was also observed in the Left Main Coronary Artery Stenting (LE MANS) trial,17 the only randomized trial in this range.
Clinical outcomes after unprotected LMCA PCI have been shown to vary according to clinical and angiographic features. In‐hospital mortality was 0% to 4% in the PCI procedure according to literature.18, 19 One in‐hospital death (0.4%) was seen in our study, where the patient had severe and diffuse coronary disease together with valvulopathy. The patient died of heart failure 11 days after the PCI procedure. There were no early deaths or TVR during a 1‐month follow‐up in the PCI group. Meta‐analysis20 shows the average 30‐day death rate after DES implantation is 2.4%, whereas our death rate within 1 month was 0.4%, which is consistent with the results of others.
Cox proportional hazard model was used in the study and NYHA class IV and EuroSCORE were confirmed to be significant predictors of the MACCE hazard. After analyzed separately, no predictor of MACCE in the PCI group was found, whereas NHYA class IV and EuroSCORE were the predictors in the CABG group. SYNTAX score seems to have no predictive value both in the PCI and the CABG group. It is quite easy to explain in the CABG group, as SYNTAX score only shows the complexity of the PCI procedure and does not have a strong relation with the surgery. In the PCI group, perhaps as most patients we enrolled were in the medium group with low MACCE, the efficacy of the SYNTAX score could not be shown in this population.
Bifurcation lesion accounted for 66.5% in the PCI group, whereas the average stent used in left main coronary lesions was 1.09 ± 0.33 per patient. This is consistent with Seung et al's report of 1.2 ± 0.5 per patient.12 It is because the simple stenting technique (1 stent cross‐over) was preferred in the procedure and is in accordance with what is done in the real world. The baseline characteristics showed little imbalance in the severity of the disease between the 2 groups. Patients who underwent CABG tended to be older, with more complicated and diffuse disease (higher SYNTAX score and more vessels involved) and higher EuroSCORE, which adds difficulty to the PCI procedure. However, the percentage of patients with high operation risk (EuroSCORE ≥6) was equal in both groups. This reflects the selection trend in our daily clinical work.
Our hospital is a university teaching hospital and performs large number of PCI/CABG surgeries each year. Perhaps the good results we obtained are due to an experienced interventional and cardiac surgery team.
Study Limitations
This is a retrospective study with a 13.4% loss of follow‐up (45 in the PCI group and 35 in the CABG group), who were excluded from the study. There is a possibility that the loss of follow‐up was due to death, and the exclusion of those patients from the study would cause an underestimation of MACCE in both groups. Additionally, about 62% were local patients, and we completed follow‐up when they came to our outpatient department for medication. For the rest of the patients from other provinces, we did the follow‐up by telephone interviews. Cardiac enzymes were not measured routinely unless there was a clinical suspicion of ischemia; as a result, MI without symptoms after PCI or CABG could not be detected. There is no routine angiogram follow‐up in the whole study, which may have resulted in low detection of in‐stent stenosis or late stent thrombosis, and as a result low TVR.
Conclusion
During long‐term follow‐up with DES and CABG therapy, PCI with coronary stenting and CABG were associated with similar long‐term MACCE for patients with ULMCA disease. It is feasible to treat ULMCA disease in selected patients and selected lesions.
References
- 1. Patel MR, Dehmer GJ, Hirshfeld JW, et al. ACCF/SCAI/STS/ AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization: a report by the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2009;53:530–553. [DOI] [PubMed] [Google Scholar]
- 2. Kushner FG, Hand M, Smith SC Jr, et al. 2009. focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54: 2205–2241. [DOI] [PubMed] [Google Scholar]
- 3. Chieffo A, Stankovic G, Bonizzoni E, et al. Early and mid‐term results of drug‐eluting stent implantation in unprotected left main. Circulation. 2005;111:791–795. [DOI] [PubMed] [Google Scholar]
- 4. Valgimigli M, van Mieghem CA, Ong AT, et al. Short‐ and long‐term clinical outcome after drug‐eluting stent implantation for the percutaneous treatment of left main coronary artery disease: insights from the Rapamycin‐Eluting and Taxus Stent Evaluated At Rotterdam Cardiology Hospital registries (RESEARCH and T‐SEARCH). Circulation. 2005;111:1383–1389. [DOI] [PubMed] [Google Scholar]
- 5. Chieffo A, Morici N, Maisano F, et al. Percutaneous treatment with drug‐eluting stent implantation versus bypass surgery for unprotected left main stenosis: a single‐center experience. Circulation. 2006;113:2542–2547. [DOI] [PubMed] [Google Scholar]
- 6. Lee MS, Kapoor N, Jamal F, et al. Comparison of coronary artery bypass surgery with percutaneous coronary intervention with drug‐eluting stents for unprotected left main coronary artery disease. J Am Coll Cardiol. 2006;47:864–870. [DOI] [PubMed] [Google Scholar]
- 7. Park DW, Kim YH, Yun SC, et al. Long‐term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 10‐year results of bare‐metal stents and 5‐year results of drug‐eluting stents from the ASAN‐MAIN (ASAN Medical Center‐Left MAIN Revascularization) Registry. J Am Coll Cardiol. 2010;56:1366–1375. [DOI] [PubMed] [Google Scholar]
- 8. Nashef SA, Roques F, Michel P, et al. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16:9–13. [DOI] [PubMed] [Google Scholar]
- 9. Serruys PW, Morice MC, Kappetein AP, et al; SYNTAX Investigators. Percutaneous coronary intervention versus coronary‐artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;10:961–972. [DOI] [PubMed] [Google Scholar]
- 10. Iakovou I, Ge L, Colombo A. Contemporary stent treat‐ ment of coronary bifurcations. J Am Coll Cardiol. 2005;46(8): 1446–1455. [DOI] [PubMed] [Google Scholar]
- 11. Park DW, Seung KB, Kim YH, et al. Long‐term safety and efficacy of stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 5‐year results from the MAIN‐COMPARE (Revascularization for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascularization) registry. J Am Coll Cardiol. 2010;56:117–124. [DOI] [PubMed] [Google Scholar]
- 12. Seung KB, Park DW, Kim YH, et al. Stents versus coronary‐artery bypass grafting for left main coronary artery disease. N Engl J Med. 2008;358:1781–1792. [DOI] [PubMed] [Google Scholar]
- 13. Capodanno D, Stone GW, Morice MC, et al. Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: a meta‐analysis of randomized clinical data. J Am Coll Cardiol. 2011;58:1426–1432. [DOI] [PubMed] [Google Scholar]
- 14. Shroyer AL, Grover FL, Hattler B, et al. On‐pump versus off‐pump coronary‐artery bypass surgery. N Engl J Med. 2009;361:1827–1837. [DOI] [PubMed] [Google Scholar]
- 15. Thomas GN, Martinez EC, Woitek F, et al. Off‐pump coronary bypass grafting is safe and efficient in patients with left main disease and higher EuroScore. Eur J Cardiothorac Surg. 2009;36:616–620. [DOI] [PubMed] [Google Scholar]
- 16. Marui A, Kimura T, Tanaka S, et al. Significance of off‐pump coronary artery bypass grafting compared with percutaneous coronary intervention: a propensity score analysis. Eur J Cardiothorac Surg. 2012;41:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Buszman PE, Kiesz SR, Bochenek A, et al. Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J Am Coll Cardiol. 2008;51:538–545. [DOI] [PubMed] [Google Scholar]
- 18. Agostoni P, Valgimigli M, Van Mieghem CA, et al. Comparison of early outcome of percutaneous coronary intervention for unprotected left main coronary artery disease in the drug‐eluting stent era with versus without intravascular ultrasonic guidance. Am J Cardiol. 2005;95:644–647. [DOI] [PubMed] [Google Scholar]
- 19. Park SJ, Kim YH, Lee BK, et al. Sirolimus‐eluting stent implantation for unprotected left main coronary artery stenosis: comparison with bare metal stent implantation. J Am Coll Cardiol. 2005;45:351–356. [DOI] [PubMed] [Google Scholar]
- 20. Taggart DP, Kaul S, Boden WE, et al. Revascularization for unprotected left main stem coronary artery stenosis stenting or surgery. J Am Coll Cardiol. 2008;51:885–892. [DOI] [PubMed] [Google Scholar]


