Abstract
Colorectal cancer (CRC) incidence rates are rising in younger Americans and mortality rates are increasing among younger white Americans. We used New York State Cancer Registry data to examine New York City CRC incidence and mortality trends among adults ages 20–54 years by race from 1976 to 2015. Annual percent change (APC) was considered statistically significant at P less than .05 using a two-sided test. CRC incidence increased among those ages 20–49 years, yet blacks had the largest APC of 2.2% (1993–2015; 95% confidence interval [CI] = 1.4% to 3.1%) compared with 0.5% in whites (1976–2015; 95% CI = 0.2% to 0.7%). Among those aged 50–54 years, incidence increased among blacks by 0.8% annually (1976–2015; 95% CI = 0.4% to 1.1%), but not among whites. CRC mortality decreased among both age and race groups. These findings emphasize the value of local registry data to understand trends locally, the importance of timely screening, and the need for clinicians to consider CRC among all patients with compatible signs and symptoms.
National trends indicate colorectal cancer (CRC) incidence rates are rising in Americans ages 20–54 years (1). Further, although CRC mortality rates are decreasing overall (2), white adults ages 20–54 years show increased mortality rates whereas rates among black adults remain stable (3). We found no studies examining these trends locally, specifically in urban environments. New York City (NYC) provides a unique opportunity for consideration given its racial diversity and substantial foreign-born population (4). Such an analysis may inform CRC-prevention efforts in urban settings nationwide.
We obtained New York State Cancer Registry NYC CRC incidence and mortality population data for 1976–2015 among whites, blacks, and all. We compared rates for those younger and older than age 50 years, when screening should begin according to current United States Preventive Services Task Force (5) and NYC-specific guidelines (6). We used the Joinpoint Regression Program (National Cancer Institute, version 4.5.0.1) to calculate CRC incidence and mortality rates (age-adjusted to the 2000 US standard population) and fit log-linear regression models by ages (20–49 and 50–54 years) and race. Annual percent change (APC) was considered statistically significant at P less than .05 using a two-sided test. This study did not require institutional review board approval.
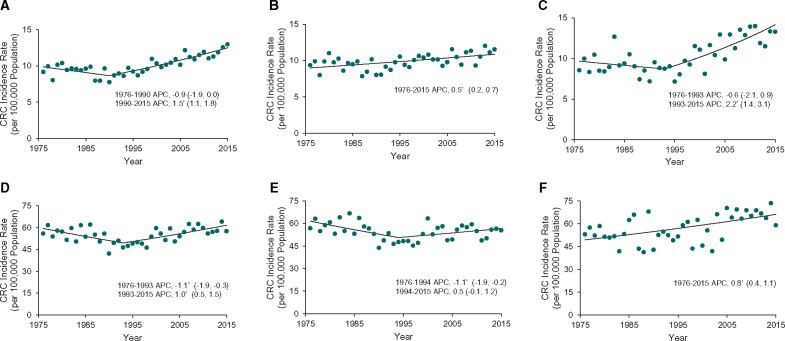
From 1976 to 2015, 22 018 individuals ages 20–54 years received a CRC diagnosis (of all CRC diagnoses among all ages, 7.3% were ages 20–49 years and 5.8% were ages 50–54 years); 58.5% white, 30.2% black. Incidence data among those ages 20–49 years showed annual CRC rate increases of 1.5% (95% confidence interval [CI] = 1.1% to 1.8%) overall from 1990 to 2015, 0.5% (95% CI = 0.2% to 0.7%) for whites from 1976 to 2015, and 2.2% (95% CI = 1.4% to 3.1%) for blacks from 1993 to 2015 (Figure 1). Notably, the incidence rates among blacks increased by 1.6 times between 1993 (8.7 per 100 000) and 2015 (14.1 per 100 000). Incidence rates among adults ages 50–54 years decreased annually by 1.1% (95% CI = −1.9% to −0.3%) from 1976 to 1993 and increased by 1.0% annually (95% CI = 0.5% to 1.5%) from 1993 to 2015. Among whites ages 50–54 years, CRC incidence rates decreased by 1.1% annually (95% CI = −1.9% to −0.2%) from 1976 to 1994 and remained stable from 1994 to 2015. In contrast, CRC incidence rates increased among blacks ages 50–54 years from 1976 to 2015 by 0.8% annually (95% CI = 0.4% to 1.1%).
Figure 1.
Annual percent change (APC) in colorectal cancer incidence rates among adults ages 20– 49 and 50–54 years in New York City by race, 1976–2015. A) All races combined, ages 20–49 years. B) White race, ages 20–49 years. C) Black race, ages 20–49 years. D) All races combined, ages 50–54 years. E) White race, ages 50–54 years. F) Black race, ages 50–54 years. CRC = colorectal cancer. *The Annual Percent Change (APC) is statistically significantly different from zero at α=0.05. Rates among those ages 20–49 years are age-adjusted to the 2000 United States Standard Population. To make trends more apparent, the scale of the y-axis varies.
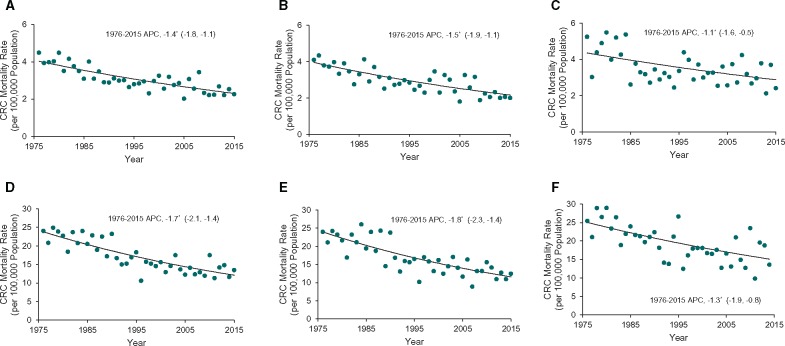
CRC was the cause of death for 6550 individuals ages 20–54 years from 1976 to 2015 (of all CRC deaths among all ages, 5.2% were ages 20–49 years and 4.2% were ages 50–54 years); 58.8% were white and 32.9% were black. Among those ages 20–49 years, overall CRC mortality rates decreased annually by 1.4% (95% CI = −1.8% to −1.1%), by 1.5% (95% CI = −1.9% to −1.1%) among whites and by 1.1% (95% CI = −1.6% to −0.5%) among blacks from 1976 to 2015 (Figure 2). Among those ages 50–54 years, CRC mortality rates decreased annually by 1.7% (95% CI = −2.1% to −1.4%) overall, by 1.8% (95% CI = −2.3% to −1.4%) among whites, and by 1.3% (95% CI = −1.9% to −0.8%) among blacks from 1976 to 2015.
Figure 2.
Annual percent change (APC) in colorectal cancer mortality rates among adults ages 20–49 and 50–54 years in New York City by race, 1976–2015. A) All races combined, ages 20–49 years. B) White race, ages 20–49 years. C) Black race, ages 20–49 years. D) All races combined, ages 50–54 years. E) White race, ages 50–54 years. F) Black race, ages 50–54 years. CRC = colorectal cancer. *The Annual Percent Change (APC) is statistically significantly different from zero at α=0.05. Rates among those ages 20–49 years are age-adjusted to the 2000 United States Standard Population. To make trends more apparent, the scale of the y-axis varies.
Similar to national trends (1), which led the American Cancer Society to update its CRC screening guidelines (7), we found increases in CRC incidence rates among ages 20–49 years and 50–54 years. However, substantial differences exist among races across age categories. Stratification showed that blacks ages 20–49 years had a larger upward APC than whites. This novel finding differs from national incidence increases limited to non-Hispanic whites (8) and Hispanics ages 20–49 years (9). Among those ages 50–54 years, incidence increased among blacks and not whites. Conversely, mortality decreased among both age and race groups, whereas nationally (3) only whites experienced an increase. Compared to the United States (70.3% white and 13.6% black), NYC is a more diverse population (40.8% white and 24.4% black). Further, 14.7% of the US population is foreign born as compared with 41.0% in NYC, highlighting NYC’s unique demographic. Among the black population ages 0–54 years, 9.5% are foreign born nationally, whereas 29.0% are foreign born in NYC (4). Racial differences in risk behaviors may have contributed to the observed incidence trends. Given the greater diversity and foreign-born population in NYC, risk behavior in earlier birth cohorts could differ greatly from national trends (10); however, historical local survey data are not available to examine this.
These findings emphasize three key ideas: 1) the value of local registry data analyses to understand trends locally and inform targeted policies and programming; 2) the continued importance of timely screening beginning promptly at age 50 years given the increasing incidence in the overall population and of a larger magnitude among blacks; and 3) the need for clinicians to consider CRC among patients of all ages and races with compatible signs and symptoms.
Although our analyses provide important new information, they could be augmented in several ways. Local data for stage at diagnosis would help determine whether the incidence increase is, in part, a result of earlier detection due to improved screening rates. Subsequent years of data will allow us to determine the impact of the elimination of racial screening disparities in 2007 (11) given this recent achievement and the time it often takes CRC to develop. The elimination of racial disparities may have contributed to increased detection among subgroups and could partially explain the increased incidence among blacks ages 50–54 years after 2007. However, the differences in incidence among those age 50 years and older are likely not attributable to racial differences in screening alone. Despite this, we suspect that sustained elimination of racial screening disparities will contribute to reducing incidence disparities in the future.
This study is limited by the long-term availability of data on other races, specifically for Asian and Hispanic populations. We did not compare colon and rectal incidence rates separately because of sparse data. Mortality rates should not be analyzed by subsite because of the large proportion of rectal cancer deaths that are misclassified as colon cancer deaths (12,13). Further, the incidence analysis was not delay-adjusted; therefore the APCs for increasing incidence may be underestimated.
Rising CRC incidence among those younger than age 50 years prompted widespread attention nationally. Although the absolute and relative risks of developing CRC are increasing among those younger than age 50 years nationally and in NYC as presented in this analysis, the greatest absolute risk remains in adults ages 50 years and older. Public health departments and health professionals should examine local data in light of national trends to better understand and act on the differences among the populations they serve.
Funding
The authors have no funding or support to report.
Notes
Affiliations of authors: New York City Department of Health and Mental Hygiene, Queens, NY.
KCVB, JJ, and KR had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. KCVB and JJ drafted the manuscript. JJ and KR provided the statistical analysis. JJB, SMF, and JML provided supervision. All authors contributed to the concept and design; acquisition, analysis, or interpretation of data; and critical revision of the manuscript.
The authors report no conflicts of interest.
The views expressed in this article are those of the authors and do not necessarily reflect the official position of the New York City Department of Health and Mental Hygiene.
References
- 1. Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst. 2017;109(8). doi: 10.1093/jnci/djw322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, et al. Trends and patterns of disparities in cancer mortality among US counties, 1980–2014. JAMA. 2017;317(4):388–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Siegel RL, Miller KD, Jemal A.. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970–2014. JAMA. 2017;318(6):572–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ruggles S, Genadek K, Goeken R, Grover J, Sobek M.. Integrated Public Use Microdata Series: Version 7.0 [American Community Survey 5-Year Sample, 2012-2016]. Minneapolis, MN: University of Minnesota; 2017. [Google Scholar]
- 5. US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(23):2564–2575. [DOI] [PubMed] [Google Scholar]
- 6. New York City Department of Health and Mental Hygiene. Preventing colorectal cancer. City Health Inf. 2009;28(Suppl 2):1–4. [Google Scholar]
- 7. Wolf AM, Fontham ET, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018. doi:10.3322/caac.21457. [DOI] [PubMed] [Google Scholar]
- 8. Austin H, Henley SJ, King J, Richardson LC, Eheman C.. Changes in colorectal cancer incidence rates in young and older adults in the United States: what does it tell us about screening. Cancer Causes Control. 2014;25(2):191–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Siegel RL, Jemal A, Ward EM.. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2009;18(6):1695–1698. [DOI] [PubMed] [Google Scholar]
- 10. Argeseanu Cunningham S, Ruben JD, Narayan KM.. Health of foreign-born people in the United States: a review. Health Place. 2008;14(4):623–635. [DOI] [PubMed] [Google Scholar]
- 11. Itzkowitz SH, Winawer SJ, Krauskopf M, et al. New York Citywide Colon Cancer Control Coalition: a public health effort to increase colon cancer screening and address health disparities. Cancer. 2016;122(2):269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chow W, Devesa SS.. Death certificate reporting of colon and rectal cancers. JAMA. 1992;267(22):3028.. [PubMed] [Google Scholar]
- 13. Percy C, Stanek E, Gloeckler L.. Accuracy of cancer death certificates and its effect on cancer mortality statistics. Am J Public Health. 1981;71(3):242–250. [DOI] [PMC free article] [PubMed] [Google Scholar]