Abstract
Background
Financial hardships experienced by cancer survivors have become a prominent public health issue in the United States. Few studies of financial hardship have assessed financial holdings, including assets, debts, and their values, associated with a cancer history.
Methods
Using the 2008–2011 Medical Expenditure Panel Survey, we identified 1603 cancer survivors and 34 915 individuals age 18–64 years without a cancer history to assess associations between self-reported cancer history and assets, debts, and net worth. Distributions of self-reported asset and debt ownership, their values, and net worth were compared for adults with and without a cancer history with chi-square statistics. Multivariable ordered probit regression analysis was conducted to assess the association between cancer history and net worth using a two-sided Wald test. All analyses were stratified by age group (18–34, 35–44, 45–54, and 55–64 years). Statistical tests were two-sided.
Results
Among those age 45–54 years, cancer survivors had a lower proportion of home ownership than individuals without a cancer history (59.0% vs 67.1%, P = .0014) and were statistically significantly more likely to have negative net worth (≤–$3000) and less likely to have positive net worth (≥$3000). Cancer survivors were more likely to have debt than individuals without a cancer history, especially among those age 18–34 years (41.3% vs 27.1%, P < .001).
Conclusions
Cancer history is associated with lower asset ownership, more debt, and lower net worth, especially in survivors age 45–54 years. Longitudinal studies of financial holdings will be important to inform development of interventions to reduce financial hardship.
The number of cancer survivors is expected to grow from 15.5 million in 2016 to 20.3 million by 2026 in the United States (1) due to an aging and growing population and increasing survival resulting from improvements in early detection and treatment. The cost of cancer treatment is also expected to increase over this time. The average launch price of a new therapeutic agent in oncology has increased by an average of $8500 per year (2), from 1995 to 2013, and currently novel anticancer drugs can cost more than $60 000 for a month of treatment (3). Cancer survivors and their family caregivers may also experience limitations in ability to work (4,5), reducing household income and limiting access to employer-based health insurance. Consequently, the medical costs associated with cancer have led to considerable financial hardship for survivors, especially the working-age population and their families (6). Recent studies estimated that between 13% and 34% of working-age cancer survivors (age 18–64 years) report ever having to borrow money or go into debt because of cancer, its treatment, or lasting effects of treatment (6,7), about six times the proportion of cancer survivors age 65 years and older (6). Younger age (<40) is also associated with up to 10 times the rate of bankruptcy filings among cancer survivors (8).
Empirical studies have demonstrated that financial hardship is associated with lower adherence to cancer treatments (9–12), lower quality of life and perceived quality of care (13,14), and subsequently poorer health outcomes, including increased mortality (15). Thus, financial hardship is also an increasingly significant social and public health issue.
As mentioned previously, material measures of financial hardship are typically measured as out-of-pocket spending by survivors for their medical care and health care in general and productivity loss, including lost income, missed work days, inability to participate in usual activities, or family members’ personal leave from work. However, the scope of financial hardship in cancer survivors is not particularly well understood, and few studies have assessed the underlying financial holdings, including ownership of assets, debts, and their values, as novel measures of financial hardship of individuals following a cancer diagnosis compared with those without a cancer history. An older study used data from the 2002 Health and Retirement Study to examine assets in cancer survivors and individuals without a cancer history age 55 years and older, but information was not available about the working-age population younger than age 55 years, which is likely to be most vulnerable to the risk of financial hardship (16). In addition, these data were collected before more modern high-cost cancer care and did not include any information about debt or net worth. Other studies of debt in cancer survivors have been limited by lack of a comparison group without a cancer history (6,7) or have been conducted in defined geographic regions and were not representative of the US population (8). In this study, we used nationally representative data to assess the association between a cancer history and asset ownership, debts, and net worth among working-age individuals age 18–64 years.
Methods
Data Source and Study Population
This cross-sectional study used data from the 2008–2011 Medical Expenditure Panel Survey (MEPS) Household Component sponsored by the Agency for Healthcare Research and Quality (AHRQ). The MEPS is an ongoing nationally representative survey of health insurance, access to care, utilization, and health care expenditures in the US civilian noninstitutionalized population. In-person interviews are conducted with a family member who typically responds for all family members in the household over a two-year period consisting of five rounds of interviews. Asset and debt data are collected in round 5 only and are considered restricted use (only available through the AHRQ Data Center); 2008–2011 are the most recently available years of the survey with edited and reliable asset and debt data (17). MEPS estimate of net worth and asset holdings compare well to the Survey of Income and Program Participation (SIPP), and MEPS is comparable along many dimensions to the Survey of Consumer Finances (SCF), (17,18). These survey years had a combined average annual response rate ranging from 54% to 59%. More information about survey design and content is available from http://www.meps.ahrq.gov/mepsweb/.
We identified 1603 working-age cancer survivors age 18–64 years based on responses to the question “Have you ever been told by a doctor or other health professional that you had cancer or a malignancy of any kind?” Individuals who did not respond to this question were excluded from the study. Consistent with prior studies, individuals who reported only a diagnosis of nonmelanoma skin cancer were not classified as cancer survivors and were included in the comparison group (19–21). The comparison group included 34 915 individuals age 18–64 years without a self-reported history of cancer.
Measures
Sample Characteristics
Sample characteristics for adults with and without a self-reported cancer history included age (18–34, 35–44, 45–54, and 55–64 years), sex, race/ethnicity (non-Hispanic white and other), marital status (married and not married/other), educational attainment (<high school and ≥high school), family size (1, 2 [eg, husband and wife or parent and child], and 3+), family income as percentage of the federal poverty line (FPL; <399%, and ≥400%), employment (employed and not employed), health insurance type (private, any public, uninsured), and survey year. Comorbid conditions were identified with a series of questions about whether a doctor or other health professional ever told the person they had any MEPS priority condition, including arthritis, asthma, diabetes, emphysema, coronary heart disease, hypertension, stroke, angina, and high cholesterol. Comorbid conditions were categorized by the number of MEPS priority medical conditions (0, 1, 2+). Time since cancer diagnosis and receipt of any cancer treatment during the year of the survey were measured only for cancer survivors.
Measures of Wealth
Measures of wealth included financial assets, debt, and net worth, which were estimated as previously described by Bernard et al. (17). Briefly, total financial assets included ownership and value of first home, vehicles, checking and savings accounts, other financial assets (ie, money market funds, stocks, government and corporate bonds, mutual funds, certificates of deposit), individual retirement accounts (ie, IRA, Keogh and 401(k)), other properties (ie, second homes, rental real estate, a business or farm, boats, trailer, or other recreational vehicles). Total debt included ownership and value of debts related to home, vehicles, second homes, rental real estate, a business or farm, boats or other recreational vehicles, credit card balances, debts owed to medical providers, life insurance policy loans, loans from relatives and other significant sources. Net worth was estimated as the value of all assets minus debts. Given that economic resources are shared among family members, measures of assets, debt, and income were estimated at the family level in MEPS. We categorized net worth using a $3000 cutoff (negative net worth ≤ –$3000; –$2999 ≤ net worth ≤ +$2999; and positive net worth ≥ +$3000) to represent monthly median household income after approximately 30% tax deductions in the period these data were collected, 2008–2011 (22–24).
Analyses
Descriptive statistics were calculated for all sample demographic and socioeconomic characteristics. Distributions of self-reported asset and debt ownership, their values, and net worth were compared for adults with and without a cancer history with chi-square statistics. Analyses were stratified by age group (18–34, 35–44, 45–54, and 55–64 years) to reflect phases of the life course with respect to debt and asset accumulation.
Multivariable ordered probit regression analysis was conducted to assess the association between cancer history and net worth. We present unadjusted, partially adjusted, and fully adjusted predicted probabilities of cancer history and each of the net worth categories to first evaluate the effects of patient demographic characteristics and then the addition of socioeconomic characteristics on these associations. Partially adjusted model covariates included sex, race/ethnicity, marital status, and number of comorbid conditions. Additional covariates in the fully adjusted models were educational attainment, family size, family income as percentage of FPL, employment status, type of health insurance, and survey year. All estimates were weighted to account for the MEPS complex survey design and survey nonresponse using Stata, version 13.1 (College Station, TX, USA). Two-sided P values were calculated using the Wald test. Comparisons with P values of less than .05 were considered statistically significant.
Results
Compared with individuals without a cancer history, survivors were relatively older (47.3% vs 17.8% age 55–64 years), mostly female (65.9% vs 49.8%), and less likely to be employed (64.2% vs 76.1%) (Table 1). Cancer survivors were also more likely to have two or more comorbid conditions (49.9% vs 23.9%) and less likely to not have any comorbid conditions (25.9% vs 52.6%) than those without a cancer history. Cancer survivors were less likely to be uninsured and more likely to have higher educational attainment and higher income as a percentage of the FPL. Of the cancer survivors, the clear majority were more than two years since first cancer diagnosis (81.6%) and not receiving cancer treatment at the time of the survey (81.8%). Therefore, the sample of cancer survivors was comprised mainly of longer-term cancer survivors with at least one additional chronic condition.
Table 1.
Characteristics of sample population
| Cancer survivor (n = 1603) |
No history of cancer(n = 34 915) |
||
|---|---|---|---|
| No. (weighted %) | No. (weighted %) | Chi-square P | |
| Age, y | |||
| 18–34 | 192 (10.6) | 13 513 (38.2) | <.01 |
| 35–44 | 241 (14.3) | 7772 (21.4) | <.01 |
| 45–54 | 457 (27.8) | 7796 (22.6) | <.01 |
| 55–64 | 713 (47.3) | 5834 (17.8) | <.01 |
| Sex | |||
| Male | 482 (34.1) | 1 612 (50.2) | <.01 |
| Female | 1121 (65.9) | 18 303 (49.8) | <.01 |
| Race/ethnicity | |||
| White, non-Hispanic | 1055 (80.6) | 15 153 (64.4) | <.01 |
| Black, Hispanic, other | 548 (19.4) | 19 762 (35.6) | <.01 |
| Marital status | |||
| Married | 882 (59.5) | 17 759 (52.5) | <.01 |
| Not married | 721 (40.5) | 17 156 (47.5) | <.01 |
| Education* | |||
| Less than high school | 280 (11.9) | 8492 (17.2) | <.01 |
| High school grad/college | 1319 (88.1) | 26 264 (82.8) | <.01 |
| Family size | |||
| Single | 292 (20.2) | 4847 (17.1) | <.01 |
| Dyad | 579 (38.9) | 7956 (26.6) | <.01 |
| 3+ | 732 (40.9) | 22 112 (56.2) | <.01 |
| Family income, % FPL | |||
| <399 | 1017 (53.5) | 24 293 (59.1) | <.01 |
| 400+ | 586 (46.5) | 10 604 (40.9) | <.01 |
| Employment status | |||
| Employed | 956 (64.2) | 25 165 (76.1) | <.01 |
| Retired/not employed/other | 647 (35.8) | 9750 (23.9) | <.01 |
| Health insurance | |||
| Private | 1029 (73.8) | 21 266 (70.7) | <.01 |
| Public only | 357 (15.7) | 5155 (10.5) | <.01 |
| Uninsured | 217 (10.5) | 8494 (18.8) | <.01 |
| No. of comorbid conditions | |||
| 0 | 409 (25.9) | 18 743 (52.6) | <.01 |
| 1 | 364 (24.2) | 7946 (23.5) | .96 |
| 2+ | 830 (49.9) | 8226 (23.9) | <.01 |
| Year | |||
| 2008 | 343 (20.6) | 7030 (20.9) | .22 |
| 2009 | 466 (29.2) | 10 360 (27.9) | .61 |
| 2010 | 427 (27) | 9276 (27.7) | .95 |
| 2011 | 367 (23.2) | 8249 (23.4) | .5 |
| Years since first cancer diagnosis | |||
| ≤1 | 206 (13.1) | N/A | |
| 2–5 | 459 (28.8) | ||
| 6–9 | 267 (16.1) | ||
| 10–19 | 358 (22.7) | ||
| ≥20 | 213 (14) | ||
| Missing | 100 (5.3) | ||
| In treatment† | |||
| Yes | 274 (18.2) | ||
| No | 1329 (81.8) | ||
Out of 1603 cancer survivors, four had missing values for educational attainment. Out of 34 915 individuals without a history of cancer, 159 had missing values. FPL = federal poverty level.
In treatment was defined as receiving chemotherapy or radiation therapy for a cancer condition in either an outpatient or office-based setting or having a prescription for an antineoplastic medication.
Asset Ownership
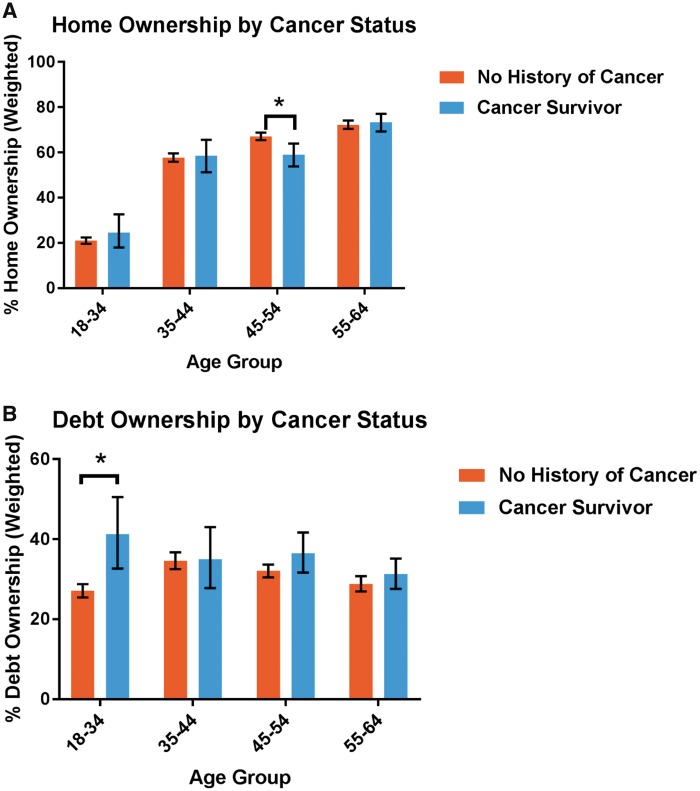
Asset ownership was higher among cancer survivors and individuals without a cancer history in the older age groups than the younger age groups. Among the group age 45 to 54 years, the proportion reporting family home ownership was statistically significantly lower for cancer survivors than those without a cancer history (59.0% vs 67.1%, P = .0014) (Figure 1). Asset ownership was similar for cancer survivors and individuals without a cancer history in the other age groups.
Figure 1.
Home and debt ownership by cancer status. A) Home ownership by cancer status. P = .0014 for age group 45–54 years, chi-square test. B) Debt ownership by cancer status. P < .001 for age group 18–34 years, chi-square test. *P < .05.
Debt
Among those age 18 to 34 years, a statistically significantly higher proportion of cancer survivors reported debt ownership than individuals without a cancer history (41.3% vs 27.1%, P < .001) (Figure 1; Appendix Table 1). In the group age 45–54 years, cancer survivors also had a higher proportion of debt ownership than individuals without a cancer history, although the difference was only marginally significant (36.5% vs 32.1%, P = .06).
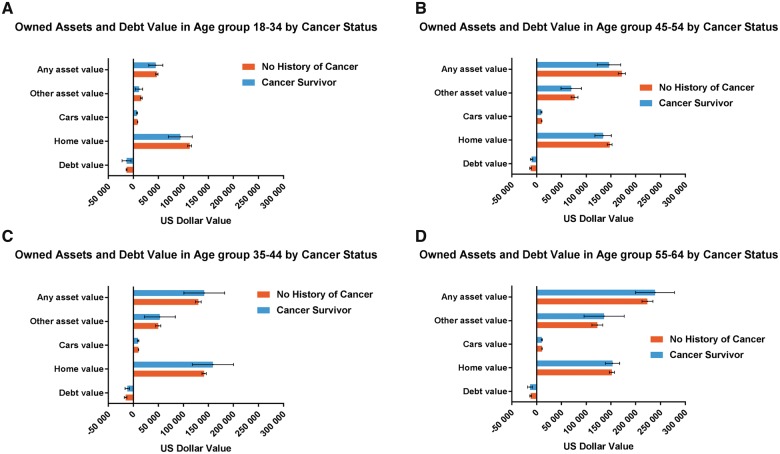
Net Worth
The summary of assets and debt values for cancer survivors and individuals without a cancer history who reported ownership is shown in Figure 2. No statistically significant differences were observed in the reported mean assets and debt values of cancer survivors compared with individuals without a history of cancer in the same age groups.
Figure 2.
Debts and assets values (2011 dollars) in cancer survivors and in individuals without a cancer history who reported ownership by age group. A) Owned assets and debt values in age group 18–34 years by cancer status. Error bars represent the 95% confidence interval. B) Owned assets and debt values in age group 35–44 years by cancer status. Error bars represent the 95% confidence interval. C) Owned assets and debt values in age group 45–54 years by cancer status. Error bars represent the 95% confidence interval. D) Owned assets and debt values in age group 55–64 years by cancer status. Error bars represent the 95% confidence interval. Other asset value refers to the values of all assets not including primary home and cars. Any asset value refers to the values of all assets.
Relative to those without a history of cancer, the unadjusted and adjusted likelihood of cancer survivors falling into three net worth categories is depicted in Table 2. Cancer survivors age 45–54 years were statistically significantly more likely to have a negative net worth and statistically significantly less likely to have a positive net worth than those individuals without a history of cancer (1.5%, 95% confidence interval [CI] = 0.2 to 2.7, and –4.7%, 95% CI = –9.0 to –0.6, respectively). Cancer survivors in the 18–34 age category were also more likely to have a negative net worth and less likely to have a positive net worth (2.3%, 95% CI = –0.2 to 4.7, and –5.8%, 95% CI = –12.1 to 0.5, respectively), although this was only statistically significant in unadjusted and partially adjusted models.
Table 2.
Cancer survivors and net worth categories relative to individuals without a history of cancer
| Age group, y | Unadjusted Mar eff (95% CI) | Partially adjusted Mar eff (95% CI) | Fully adjusted Mar eff (95% CI) |
|---|---|---|---|
| Negative net worth ≤ –$3000 | |||
| 18–34 | 0.034* (0.008 to 0.060) | 0.034* (0.009 to 0.060) | 0.023 (–0.002 to 0.047) |
| 35–44 | 0.025 (–0.001 to 0.051) | 0.019 (–0.006 to 0.044) | 0.010 (–0.013 to 0.033) |
| 45–54 | 0.026* (0.009 to 0.042) | 0.023* (0.008 to 0.038) | 0.015* (0.002 to 0.027) |
| 55–64 | 0.002 (–0.009 to 0.013) | 0.007 (–0.002 to 0.016) | 0.005 (–0.002 to 0.012) |
| –$2999 ≤ net worth ≤ +$2999 | |||
| 18–34 | 0.046* (0.011 to 0.081) | 0.048* (0.012 to 0.085) | 0.035 (–0.003 to 0.073) |
| 35–44 | 0.030 (–0.001 to 0.062) | 0.025 (–0.008 to 0.059) | 0.016 (–0.021 to 0.053) |
| 45–54 | 0.038* (0.014 to 0.063) | 0.041* (0.014 to 0.068) | 0.033* (0.004 to 0.062) |
| 55–64 | 0.004 (–0.019 to 0.026) | 0.018 (–0.006 to 0.042) | 0.017 (–0.009 to 0.043) |
| Positive net worth ≤ +$3000 | |||
| 18–34 | –0.080* (–0.141 to –0.018) | –0.083* (–0.145 to –0.020) | –0.058 (–0.121 to 0.005) |
| 35–44 | –0.055 (–0.114 to 0.002) | –0.045 (–0.104 to 0.015) | –0.026 (–0.086 to 0.034) |
| 45–54 | –0.064* (–0.105 to –0.023) | –0.063* (–0.105 to –0.022) | –0.047* (–0.090 to –0.006) |
| 55–64 | –0.006 (–0.038 to 0.027) | –0.025 (–0.058 to 0.008) | –0.022 (–0.054 to 0.011) |
P < .05. Marginal effect (Mar eff) shows the discrete change in probability when cancer status changes from 0 (without a history of cancer) to 1 (cancer survivor). Partially adjusted model covariates included sex, race/ethnicity, marital status, and number of comorbid conditions. Additional covariates in the fully adjusted models were educational attainment, family size, family income as percentage of the federal poverty level, employment status, type of health insurance, and survey year. CI = confidence interval.
Discussion
Using nationally representative data from the MEPS, we found that among those age 45–54 years, cancer survivors had a lower proportion of home ownership than individuals without a cancer history. They were also more likely to have a negative net worth, even after controlling for key sociodemographic characteristics, including educational attainment, family income as a percentage of the FPL, employment status, and type of health insurance, as well as prevalence of other comorbid conditions, which are more common among cancer survivors. The proportion of cancer survivors with debt was higher than individuals without a history of cancer, especially in the 18–34 years age group. These findings suggest that, compared with those without a cancer history, working-age individuals with a history of cancer have less financial stability, even many years after a cancer diagnosis. Longitudinal population-based studies will be important to assessing causality, patterns of debt, assets, and net worth throughout the cancer survivorship experience and to informing the development of interventions to reduce financial hardship.
Our study contributes to a growing body of research (25) documenting the financial hardships associated with a cancer diagnosis, including 1) material conditions that develop as a result of out-of-pocket expenses and lower income from inability to work, 2) psychological responses to costs associated with diagnosis, its treatment, and lasting effects of treatment, and 3) coping behaviors used to manage increased expenditures and reduced income during and following cancer care. These coping behaviors may include filling a prescription or delaying the start of a treatment (12,26), nonadherence to treatment (27), or abandonment of a therapy (28). Given the late- and long-term effects associated with treatment, increased risk of second cancers (29–31) and other chronic conditions (32), and the need for continued surveillance, such behaviors may adversely affect health outcomes among cancer survivors and result in higher medical expenditures and increased risk of mortality (13,15,33–36). Recent studies have highlighted the elevated economic burden associated with additional chronic conditions among cancer survivors (20,37). To our knowledge, our measures of financial hardship are novel, and the prevalence of both debt and assets or net worth has not been assessed using the MEPS or other data sources for working-age adults with other conditions, such as heart disease, or in adults identified as having high medical spending in the past year. As a result, it is unclear whether our findings are specific to cancer survivors or are also consistent for adults with other conditions having high medical costs compared with similar adults without those conditions. These will be important areas for additional research.
We found that assets and net worth, at the time of the survey, varied substantially by age group for both cancer survivors and individuals without a cancer history, with greatest home ownership and asset value in the older age groups (ie, 45–54 and 55–64 years). While not unexpected, these data suggest that considerations of life course are critical in the evaluation of financial hardship.
An older study examined assets and cancer history, based on the 2002 Health and Retirement Study in older Americans (≥55 years, mean age = 68 and 69 years for men and women, respectively) (16). Cancer survivors were defined as those who were diagnosed four or more years before the survey and did not receive treatment for their cancer in the preceding two years. This study referred to net worth but only measured the sum of housing equity and other assets and, unlike our study, did not incorporate debt into the measure. Further, the study found that male cancer survivors and those without a history of cancer had similar income and assets, but differed somewhat in net worth, although no association was observed between cancer history and assets among females (16). In our study, we did not have a sufficient sample to stratify our measures by both age group and sex. Exploring the effects of key demographic and socioeconomic characteristics on asset and debt accumulation over the life course will be an important area for future research.
The MEPS is the only nationally representative database containing specific questions devoted to asset and debt categories (ie, home ownership, car ownership, debts related to home, vehicles, and businesses) for adults of all ages and types of health insurance, as well as the uninsured. However, these unique data were only available through 2011, prior to implementation of many changes in health insurance as part of the Affordable Care Act (ACA). Our results provide important baseline information in evaluating the effects of the ACA and other insurance changes on debt accumulation, safeguarding of household assets, and risk of financial hardship for cancer survivors. Several provisions of the ACA are especially relevant to cancer survivors, including Medicaid eligibility expansions in some states, allowing dependent children to remain on their parents’ employment-based health insurance until age 26 years, elimination of annual and lifetime limits on coverage for essential health benefits, caps on out-of-pocket spending, and insurance premium tax credits and cost-sharing subsidies for individuals and families who meet eligibility requirements (7). As additional years of the MEPS asset module data become available, further investigations of the effects of changes in health insurance coverage in working-age adults are warranted.
Although this study provides unique information about measures of wealth, including assets, debt, and net worth, and will inform future studies of financial hardship, certain limitations should be noted. First, not all MEPS participants completed the MEPS assets module in round 5, but the distributions of sociodemographic characteristics, including age, sex, race/ethnicity, marital status, educational attainment, and number of MEPS priority conditions, in our sample and in other studies of cancer survivors and individuals without a cancer history using the MEPS are similar (20). Second, our study data, including financial holdings and cancer history, were self-reported and therefore subject to recall bias and misclassification. Third, for cancer survivors, we did not have information about stage at diagnosis, types of treatment(s) received, cancer recurrence, and other clinical characteristics likely to be associated with treatment. Fourth, the small number of survivors with specific cancers in our sample precluded us from reporting the results by cancer type. Patterns of asset and debt accumulation and employment options may vary substantially by cancer type and age at diagnosis. For example, survivors of pediatric cancers who received treatment during key developmental stages may have significant late and lasting effects of cancer and its treatment that affect employment, whereas early-stage breast cancer survivors with limited treatment may have few health effects and little employment disruption. Fifth, because the cancer diagnosis question refers to cancer or malignancy of any kind, it may have included individuals with pre-invasive disease. However, any misclassification of cancer history would likely bias our comparisons with individuals without a cancer history to a null association. Sixth, although a previous study surmised that poverty could place patients at greater risk for certain types of cancer (38), this doesn’t seem to be the mechanism in our sample. The cancer survivors in our study had higher insurance coverage, education level, and income. Further longitudinal studies are needed to tease apart whether cancer itself is the cause of poverty. Seventh, the most recent years of the assets section available were 2008–2011, which may not reflect current values. These years include the recent economic downturn in the United States. However, the proportion of cancer survivors and individuals without a cancer history included for each year were similar, our study compared cancer survivors and individuals without a cancer history (rather than trends), and we included survey year in our multivariable analyses. As a result, we do not believe that any specific year had a particular impact on our findings. Nonetheless, it is possible that the economic downtown might have affected cancer survivors more than other Americans in their assets, debts, and net worth as survivors were more susceptible to changes in employment and health insurance coverage or faced greater expenses due to their cancer diagnosis and greater comorbidity. Future studies are needed to confirm the magnitudes of difference observed in our study. Finally, as our study was cross-sectional across MEPS interview years, we were unable to assess the causal nature of the observed associations.
Our cross-sectional study provides evidence of material measures of financial hardship that working-age cancer survivors and their households may experience. We assessed the association between cancer history and the components of net worth and identified the age groups most affected by a cancer diagnosis. We found that cancer history has an association with asset ownership, debt, and net worth, especially in those age 45–54 years. Longitudinal studies that assess the causality and patterns of financial holdings throughout the cancer experience are warranted.
Notes
Affiliations of authors: Early Detection Branch, Division of Cancer Prevention, National Cancer Institute, Bethesda, MD (MD); Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Rockville, MD (DC); The Center for Health Research, Kaiser Permanente, Portland, OR (MPB); Surveillance and Health Services Research Program, American Cancer Society, Atlanta, GA (XH); Office of Health Policy, US Department of Health and Human Services, Washington, DC (KRY).
The authors are grateful to Dr. Paul F. Pinsky and Dr. Barry Kramer (National Cancer Institute) and Dr. Didem Bernard and Mr. Ray Kuntz (AHRQ) for assistance in study design, data assembly, and providing us with the most recent literature. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Cancer Institute or the Department of Health and Human Services, Kaiser Permanente, or the American Cancer Society. The work was performed by federal employees, and Drs. Matthew P. Banegas and Xuesong Han donated their time. Nonfederal employees did not receive funding for this project. Preliminary results from this study were presented at the 38th Annual Meeting of Society for Medical Decision Making conference in Vancouver, Canada, October 23–26, 2016.
Appendix
Appendix Table 1. Asset ownership by age group
| Cancer survivor | Without a cancer history | P | |
|---|---|---|---|
| (n = 1603) | (n = 34 915) | ||
| No. (weighted %) | No. (weighted %) | ||
| Asset owner, age 18–34 y | |||
| Home | 42 (24.6) | 2281 (21) | .32 |
| Transportation Vehicle | 111 (63.6) | 7131 (59.1) | .26 |
| Other assets | 108 (64.4) | 6826 (59.8) | .32 |
| Any assets | 134 (77.4) | 8934 (73.8) | .34 |
| Asset owner, age 35–44 y | |||
| Home | 117 (58.6) | 3829 (57.8) | .83 |
| Transportation Vehicle | 178 (80.7) | 5762 (79.7) | .75 |
| Other assets | 159 (74.8) | 5135 (74.8) | .99 |
| Any assets | 203 (89.4) | 6512 (88.8) | .78 |
| Asset owner, age 45–54 y | |||
| Home | 237 (59) | 4648 (67.1) | .00* |
| Transportation Vehicle | 351 (82.4) | 5866 (80.9) | .50 |
| Other assets | 301 (71.9) | 5362 (76.5) | .08 |
| Any assets | 385 (89.0) | 6696 (90.5) | .26 |
| Asset owner, age 55–64 y | |||
| Home | 486 (73.4) | 3846 (72.3) | .59 |
| Transportation Vehicle | 567 (83.6) | 4422 (81.4) | .19 |
| Other assets | 534 (80.7) | 4245 (79.5) | .47 |
| Any assets | 641 (93.1) | 5140 (92.0) | .33 |
P < .05.
References
- 1. American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2016-2017 .Atlanta: American Cancer Society; 2016. [Google Scholar]
- 2. Howard DH, Bach PB, Berndt ER, Conti RM.. Pricing in the market for anticancer drugs. J Econ Perspect. 2015;291:139–62. [DOI] [PubMed] [Google Scholar]
- 3. Bach PB. Why drugs cost so much. New York Times January 14, 2015.
- 4. de Moor JS, Dowling EC, Ekwueme DU et al. , . Employment implications of informal cancer caregiving. J Cancer Surviv. 2017;111:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ekwueme DU, Yabroff KR, Guy GP Jr et al. , . Medical costs and productivity losses of cancer survivors—United States, 2008-2011. MMWR Morb Mortal Wkly Rep. 2014;6323:505–510. [PMC free article] [PubMed] [Google Scholar]
- 6. Yabroff KR, Dowling EC, Guy GP Jr et al. , . Financial hardship associated with cancer in the United States: Findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;343:259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Banegas MP, Guy GP Jr, de Moor JS et al. , . For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Aff (Millwood) .2016;351:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ramsey S, Blough D, Kirchhoff A et al. , . Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood). 2013;326:1143–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL.. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol. 2014;324:306–311. [DOI] [PubMed] [Google Scholar]
- 10. Neugut AI, Subar M, Wilde ET et al. , . Association between prescription co-payment amount and compliance with adjuvant hormonal therapy in women with early-stage breast cancer. J Clin Oncol. 2011;2918:2534–2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Farias AJ, Du XL.. Association between out-of-pocket costs, race/ethnicity, and adjuvant endocrine therapy adherence among medicare patients with breast cancer. J Clin Oncol. 2017;351:86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zheng Z, Han X, Guy GP Jr et al. , . Do cancer survivors change their prescription drug use for financial reasons? Findings from a nationally representative sample in the United States. Cancer. 2017;1238:1453–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D.. Population-based assessment of cancer survivors' financial burden and quality of life: A prospective cohort study. J Oncol Pract. 2015;112:145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D.. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol. 2016;3415:1732–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ramsey SD, Bansal A, Fedorenko CR et al. , . Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;349:980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Norredam M, Meara E, Landrum MB, Huskamp HA, Keating NL.. Financial status, employment, and insurance among older cancer survivors. J Gen Intern Med. 2009;24(Suppl 2):S438–S445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bernard DM, Banthin JS, Encinosa WE.. Wealth, income, and the affordability of health insurance. Health Aff (Millwood) .2009;283:887–896. [DOI] [PubMed] [Google Scholar]
- 18.Panel on Measuring Medical Care Risk in Conjunction with the New Supplemental Income Poverty Measure, O'Grady MJ, Wunderlich GS. Medical Care Economic Risk : Measuring Financial Vulnerability From Spending on Medical Care. Washington, DC: National Academies Press; 2012. [PubMed]
- 19. Yabroff KR, Guy GP Jr, Ekwueme DU et al. , . Annual patient time costs associated with medical care among cancer survivors in the United States. Med Care. 2014;527:594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Guy GP Jr, Ekwueme DU, Yabroff KR et al. , . Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;3130:3749–3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML.. Burden of illness in cancer survivors: Findings from a population-based national sample. J Natl Cancer Inst. 2004;9617:1322–1330. [DOI] [PubMed] [Google Scholar]
- 22.US Census Bureau. Household income for states: 2010 and 2011. https://www.census.gov/prod/2012pubs/acsbr11-02.pdf. Accessed January 25, 2017.
- 23.US Census Bureau. Household income for states: 2007 and 2008. https://www.census.gov/prod/2009pubs/acsbr08-2.pdf. Accessed January 25, 2017.
- 24.US Census Bureau. Household income for states: 2009 and 2010. https://www.census.gov/prod/2011pubs/acsbr10-02.pdf. Accessed January 25, 2017.
- 25. Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR.. Financial hardships experienced by cancer survivors: A systematic review. J Natl Cancer Inst. 2017;1092:djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huntington SF, Weiss BM, Vogl DT et al. , . Financial toxicity in insured patients with multiple myeloma: A cross-sectional pilot study. Lancet Haematol. 2015;210:e408–e416. [DOI] [PubMed] [Google Scholar]
- 27. Zullig LL, Peppercorn JM, Schrag D et al. , . Financial distress, use of cost-coping strategies, and adherence to prescription medication among patients with cancer. J Oncol Pract. 2013;9(6 suppl):60s–63s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Streeter SB, Schwartzberg L, Husain N, Johnsrud M.. Patient and plan characteristics affecting abandonment of oral oncolytic prescriptions. J Oncol Pract. 2011;7(3 suppl):46s–51s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Berrington de Gonzalez A, Wong J, Kleinerman R, Kim C, Morton L, Bekelman JE.. Risk of second cancers according to radiation therapy technique and modality in prostate cancer survivors. Int J Radiat Oncol Biol Phys. 2015;912:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Grantzau T, Overgaard J.. Risk of second non-breast cancer after radiotherapy for breast cancer: A systematic review and meta-analysis of 762,468 patients. Radiother Oncol. 2015;1141:56–65. [DOI] [PubMed] [Google Scholar]
- 31. Lee JS, DuBois SG, Coccia PF, Bleyer A, Olin RL, Goldsby RE.. Increased risk of second malignant neoplasms in adolescents and young adults with cancer. Cancer. 2016;1221:116–123. [DOI] [PubMed] [Google Scholar]
- 32. Bluethmann SM, Mariotto AB, Rowland JH.. Anticipating the “Silver Tsunami”: Prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016;257:1029–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ubel PA, Abernethy AP, Zafar SY.. Full disclosure—out-of-pocket costs as side effects. N Engl J Med. 2013;36916:1484–1486. [DOI] [PubMed] [Google Scholar]
- 34. Zafar SY, Peppercorn JM, Schrag D et al. , . The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient's experience. Oncologist. 2013;184:381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zheng Z, Yabroff KR, Guy GP Jr et al. , . Annual medical expenditure and productivity loss among colorectal, female breast, and prostate cancer survivors in the United States. J Natl Cancer Inst. 2016;1085:djv382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Darkow T, Henk HJ, Thomas SK et al. , . Treatment interruptions and non-adherence with imatinib and associated healthcare costs: A retrospective analysis among managed care patients with chronic myelogenous leukaemia. Pharmacoeconomics. 2007;256:481–496. [DOI] [PubMed] [Google Scholar]
- 37. Guy GP Jr, Yabroff KR, Ekwueme DU, Rim SH, Li R, Richardson LC.. Economic burden of chronic conditions among survivors of cancer in the United States. J Clin Oncol. 2017;3518:2053–2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Boscoe FP, Johnson CJ, Sherman RL, Stinchcomb DG, Lin G, Henry KA.. The relationship between area poverty rate and site-specific cancer incidence in the United States. Cancer. 2014;12014:2191–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]