Abstract
Background
Chronic Kidney Disease (CKD) is a worldwide public health problem. The prevalence of CKD is rising especially in elderly, as consequence of population-ageing related to socioeconomic development and better life expectancy. There are scarce studies evaluating CKD progression and its associated factors in elderly patients.
Methods
This is a retrospective observational study including 340 patients (≥ 65 years old) CKD stages 3a–5 non-dialysis, incidents in an outpatient CKD clinic, followed by 2.1 years. CKD progression was assessed by the slope of eGFR calculated by CKD-EPI and BIS 1 equations. The patients were divided in progressor and non-progressor groups (eGFR slope < or ≥ 0 mL/min/1.73 m2/year, respectively).
Results
Kidney function declined in 193 (57%) patients. In this group, the progression rate was -2.83 (-5.1 / -1.1) mL /min /1.73 m2 /year. Compared to non progressor, the progressor patients were younger [72 (69–78) vs. 76 (69–80) years; p = 0.02]; had higher proportion of diabetic nephropathy, higher serum phosphorus [3.8 (3.3–4.1) vs. 3.5 (3.9–4.1) mg/dL; p = 0.04] and proteinuria [0.10 (0–0.9 vs. 0 (0–0.3)] g/L; p = 0.007)] at the admission. In the logistic regression analysis adjusted for gender and eGFR, proteinuria was independently associated with CKD progression [OR (Odds Ratio) (1.83; 95% CI, 1.17–2.86; p < 0.01)].
Conclusion
CKD progression was observed in the majority of elderly CKD patients and proteinuria was the most important factor associated to the decline of kidney function in this population.
Introduction
Chronic Kidney Disease (CKD) is a worldwide public health problem. CKD is one of the leading causes of non-communicable diseases and its prevalence is rising especially among older adults, as a consequence of socioeconomic development and better life expectancy [1].
The estimated glomerular filtration rate (eGFR) in elderly people has been a challenge. The 2012 Clinical Practice Guidelines KDIGO [2] has recommended CKD Epidemiology Collaboration equation (CKD-EPI), despite only a few number of older adults have been included in the cohort that validated this equation. In the same year, two other formulas, the Berlin Initiative Study (BIS)-1, based on serum creatinine and the BIS-2, based on serum creatinine and cystatin [3], were suggested as the preferable methods to estimate GFR in older people. However, subsequent reports did not confirm the superiority of BIS over CKD-EPI to diagnose CKD in this population [4, 5].
Beyond diagnose, the progression of CKD in elderly people has been an additional task. As aging has been associated to kidney dysfunction, the differentiation between CKD progression, per se, and the age-related decreasing of GFR has been a matter of discussion [6]. Additionally, many definitions of CKD progression have been used over the years, such as: doubling of serum creatinine [7], eGFR decreasing > 15 mL/min/1.73 m2 and achievement of end stage renal disease (ESRD) [8]. In studies comprising elderly CKD populations, the changing of eGFR in mL/min/year has been the most frequently parameter used, albeit with conflicting results. In observational studies, while some authors have shown that elderly people present a slow or none decline of kidney function [9, 10], others reported that the rate of eGFR lost could be faster [11].
Based on the scarce and conflicting fore mentioned data, we aimed to describe the associated factors and the behavior of the CKD progression in a cohort of elderly patients.
Methodology
Population
All incident CKD stage 3-5ND patients from the outpatient CKD Clinic of the Federal University of São Paulo, Brazil, from April 2011 to April 2015, were evaluated. Among 1319 patients, 663 were ≥ 65 years. Exclusion criteria comprised: follow-up time shorter than one year (n = 218) or only one serum creatinine measurement (n = 105). Therefore, 340 elderly patients were included in the study.
The study was reviewed and approved by the Ethics Advisory Committee of the Federal University of São Paulo (approval number: 0912/2015, CAAE: 47507215.6.0000.5505) and the need for informed consent was waived. All data were anonymized to comply with the provisions of personal data protection legislation.
Study design and protocol
This was a single center retrospective observational study. All the demographic, clinical and laboratorial data at the first visit (admission) were obtained from patients´ files. Laboratory evaluation included: urea, hemoglobin, sodium, potassium, ionized calcium, phosphorus, intact parathyroid hormone, bicarbonate, glucose, glycated hemoglobin, uric acid, low- (LDL) and high-density lipoprotein (HDL) cholesterol and triglycerides. Proteinuria was assessed in spot urine sample and classified as absent, mild (>0 to 0.99 g/L), moderate (≥1 to < 3 g/L) or severe (≥3g/L). The creatinine of the admission and the last one available in the patients’ files were used to calculate eGFR (CKD-EPI) 1 and 2, respectively. CKD progression was assessed by the rate of eGFR slope over time [(eGFR 2 –eGFR1)/ follow up (yr)]. The patients were classified into ‘progressor’ and ‘non-progressor’ groups (eGFR slope < or ≥ 0 mL/min/1.73 m2/year, respectively). Patients with slope < - 5 mL/min/1.73 m2/year were considered as fast progressors. The BIS 1 equation was also determined. Hypertension was defined as blood pressure > 140/90mmHg or use of any anti-hypertensive drug; anemia as hemoglobin < 10 mg/dL; and obesity and overweight as body mass index (BMI) ≥ 30 and 25 Kg/m2, respectively.
Statistical analysis
Mean and standard deviation, median and interquartile range or frequencies (proportion) were calculated for each variable, as appropriate. The Kolmogorov-Smirnov statistical test was used to investigate the variable distribution. Comparisons of continuous variables were performed using Student’s t-test and the Mann-Whitney U-test, for normal and skewed data, respectively. Comparisons of proportions were performed using chi-squared analysis or Fisher’s exact test, as appropriate. Multiple imputations were performed for missing data using MICE package of software R. This approach was applied only to variables with up to 25% missing data. Thus, all the patients were included for the logistic regression analysis. A stepwise multivariate model was constructed to test the variables associated with CKD progression. This method selected variables with p < 0.10, adjusted for gender and CKD-EPI at the admission. Cox proportional hazards model was used to investigate the impact of the occurrence of death on the CKD progression. Values of p < 0.05 were considered statistically significant. All analyses were performed using a standard statistical package (SPSS for Windows, version 20; SPSS, Chicago, IL, USA).
Results
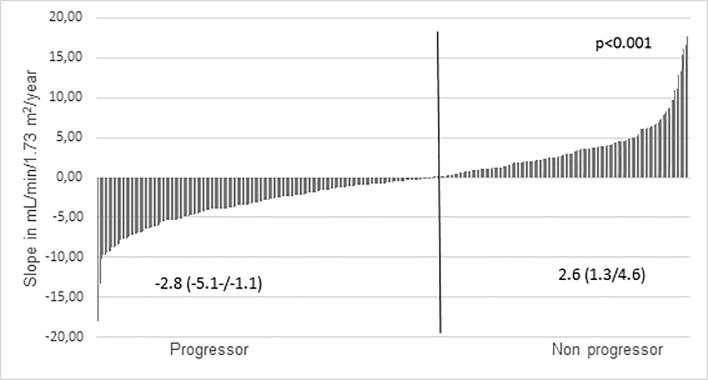
Table 1 depicts the patient’s characteristics at the admission. Patients were predominantly male, white, and CKD stages 3a (11.5%), 3b (37%), 4 (43%) and 5 (9%). Diabetic nephropathy and hypertension were the main cause of CKD. Hypertension was present in 62% and anemia in 11% of the patients. Proteinuria was observed in 46% of the population. The prevalence of obesity and overweight were 28% and 40%, respectively. The patients were followed for 2.1 (1.5–3.1) years. Of all, 12 (3.5%) patients have died, 53 (16%) withdrawal treatment and 20 (6%) required dialysis during the follow up period. The median eGFR 1 was 29.1 (20.9–39.0) and eGFR 2 was 27.9 (18.7–38.2) mL/min/1.73m2. During the follow up eGFR declined in 193 (57%) patients (progressor group, Fig 1)
Table 1. Characteristics of all patients and comparison of demographic, clinical and laboratory parameters inter group.
| n | All | Progressor n = 193 | Non progressor n = 147 | p | |
|---|---|---|---|---|---|
| Age (years) | 340 | 73 (69–79) | 72 (69–78) | 76 (69–80) | 0.02 |
| Male n (%) | 340 | 191 (56) | 105 (54) | 86 (58) | 0.45 |
| Caucasian n (%) | 298 | 194 (65) | 114 (67) | 80 (62) | 0.34 |
| Etiology n (%) | 340 | 0.04 | |||
| Hypertension | 63 (19) | 29 (15) | 34 (24) | ||
| Diabetes mellitus | 94 (28) | 62(32) | 32 (22) | ||
| Others | 183 (54) | 102 (53) | 81 (55) | ||
| iACE/ARB use(%)a | 340 | 227 (67) | 135 (70) | 92 (62) | 0.15 |
| Body mass index (Kg/m2) | 238 | 27.1 (24.2–30.4) | 27.0 (24.0–30.4) | 27.4 (24.6–30.0) | 0.98 |
| Systolic Blood Pressure (mmHg) | 339 | 140 (130–160) | 140 (130–160) | 140 (120–150) | 0.12 |
| Diastolic Blood Pressure (mmHg) | 339 | 80 (80–90) | 80 (80–90) | 80 (72–90) | 0.07 |
| Creatinine (mg/dL) | 340 | 1.94 (1.60–2.57) | 1.92 (1.52–2.58) | 2.00 (1.67–2.46) | 0.13 |
| Ureia (mg/dL) | 319 | 80 (63–106) | 79 (62–102) | 80 (64–108) | 0.85 |
| Proteinuria (g/L) | 286 | 0.00 (0.00–0.50) | 0.10 (0.00–0.90) | 0.00 (0.00–0.30) | 0.007 |
| Sodium (mmol/L) | 295 | 140 (138–142) | 140 (138–142) | 140 (138–142) | 0.31 |
| Potassium (mmol/L) | 314 | 4.8 (4.4–5.2) | 4.8 (4.4–5.3) | 4.7 (4.4–5.2) | 0.27 |
| Hemoglobin (g/dL) | 299 | 12.4 ±2.0 | 12.4 ± 2.0 | 12.4 ± 2.1 | 0.88 |
| Ionic Calcium (mmol/L) | 130 | 1.27 ± 0.08 | 1.28 ± 0.08 | 1.26 ± 0.09 | 0.35 |
| Phosphorus (mg/dL) | 180 | 3.7 (3.2–4.1) | 3.8 (3.3–4.1) | 3.5 (2.9–4.1) | 0.04 |
| Parathyroid hormone (pg/mL) | 71 | 124 (79–197) | 133 (94–189) | 95 (53–226) | 0.28 |
| Bicarbonate (mmol/L) | 129 | 25.17 ± 3.63 | 25.44 ± 3.33 | 24.84 ± 3.98 | 0.35 |
| Fasting plasma glucose (mg/dL) | 269 | 104 (91–120) | 104 (90–122) | 105 (97–114) | 0.74 |
| Glycated hemoglobin (A1C) (%)b | 142 | 7.1 (6.4–8.4) | 7.4 (6.4–8.6) | 7.0 (6.4–8.3) | 0.34 |
| LDL cholesterol (mg/dL) | 278 | 104 (81–130) | 105 (81–135) | 103 (81–122) | 0.52 |
| HDL cholesterol (mg/dL) | 227 | 44 (35–55) | 44 (35–55) | 43 (35–55) | 0.76 |
| Triglycerides (mg/dL) | 224 | 132 (94–177) | 139 (93–192) | 129 (95–173) | 0.51 |
| Uric acid (mg/dL) | 88 | 7.6 ± 1.82 | 7.7 ± 1.54 | 7.6 ± 2.14 | 0.71 |
a—angiotensin-converting-enzyme inhibitors or angiotensin-receptor blockers
b- only diabetes patients
Fig 1. Cohort classification according individual eGFR slope during the study eGFR slope of each patient during the study and cohort classification.
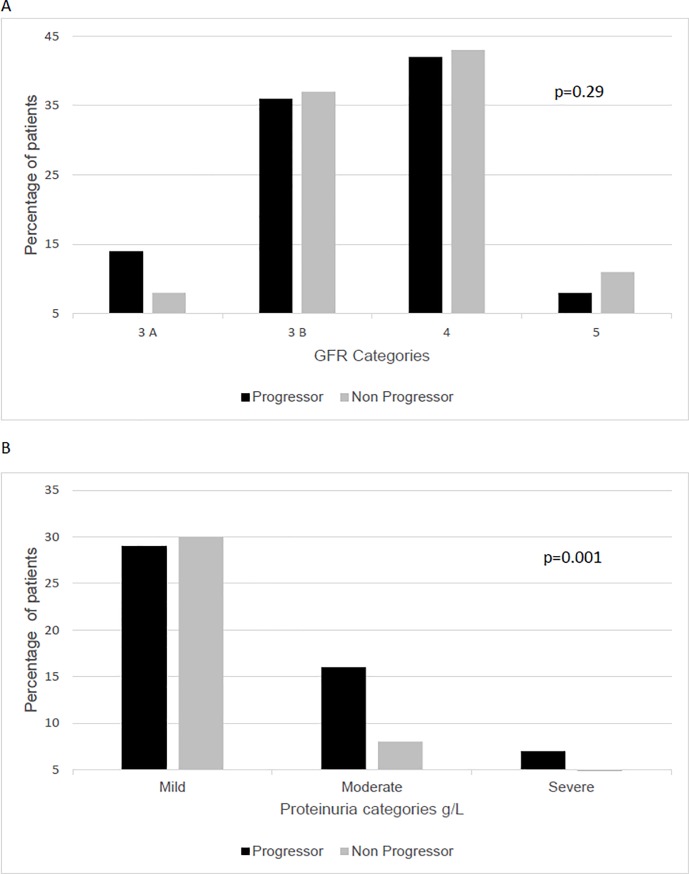
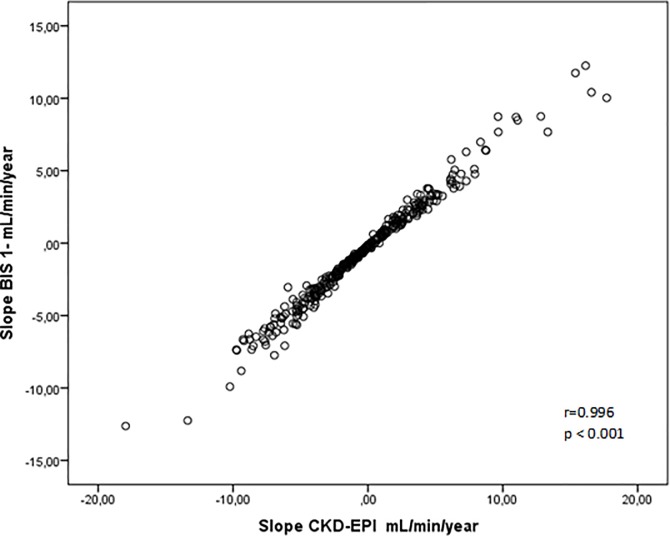
The characteristics of the progressor and non progressor groups were showed in Table 1. Comparing to non progressors, the progressors patients were younger, had higher proportion of diabetic nephropathy and had higher proteinuria and serum phosphorus. There was a trend to a higher diastolic blood pressure in the progressor group. The distribution of the patients according to CKD stages and proteinuria categories were shown in Fig 2A and 2B. CKD stages were similar in both groups (Fig 2A), and the proportion of patients with moderate and severe proteinuria was significantly higher in the progressor group (p = 0.001, Fig 2B). There were no differences regarding the use of angiotensin-converting-enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs). In the logistic regression analysis, only proteinuria was independently associated with CKD progression [OR (Odds Ratio) (1.83; 95% CI, 1.17–2.86; p < 0.01)]. In the Cox proportional-hazards model, the occurrence of death was not associated to CKD progression [HR 0.54 (CI 0.17–1.70)]. Table 2 shows the comparison between eGFR data and slope, based on the CKD-EPI and BIS 1 equations. No significant difference in the measurements of eGFR1 between groups either based on CKD-EPI or BIS 1 equations. As expected, eGFR2 was significantly lower and higher than eGFR1, in progressor and non progressor groups, respectively. Fig 3 depicts the slopes, calculated by both equations (r = 0.99, p<0.001).
Fig 2.
A Distribution of the patients according to CKD stages at baseline Fig 2. B Distribution of the patients according to proteinuria at baseline.
Table 2. Comparison of renal function and progression parameters inter groups.
| Progressor (n = 193) | Pa | Non Progressor (n = 147) | Pb | Inter groups | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| eGFR 1 | eGFR 2 | Slope | eGFR 1 | eGFR 2 | Slope | PE | PU | |||
| CKD-EPI(mL/min/1.73m2) | 30.1 (21.5/39.3) | 22.0 (14.8/31.8) | -2.8 (-5.1/ -1.1) | <0.001 | 29.0 (20.5/36.7) | 37.6 (27.7/44.9) | 2.6 (1.3/4.6) | <0.001 | 0.28 | <0.001 |
| BIS (mL/min/1.73m2) | 32.6 (25.8/39.7) | 25.9 (19.8/33.5) | -2.5 (-4.4/ -1.1) | <0.001 | 31.4 (23.1/36.8) | 36.8 (29.3/43.1) | 1.8 (0.8/3.3) | <0.001 | 0.08 | <0.001 |
pa = p intra group progressor; pb = intra group non progressor; pE = p intergroups admission; pu = p intergroup last creatinine available
Fig 3. Correlation between BIS-1 slope and CKD-EPI slope.
In the progressor group, 49 out of 193 (25%) patients were fast progressors and their median eGFR slope was -6.9 (-8.4 / -5.6) mL/min/1.73 m 2 /year. The comparison between the fast and the remaining progressor patients showed that the former ones were younger [70 (68–75) vs. 73 (69–79) years; p = 0.01], had higher prevalence of diabetic nephropathy (45 vs. 28%, p = 0.03) and higher eGFR 1 [35.5 (25.5–45.5) vs. 28.2 (19.4–37.3) mL/min/1.73 m2; p = 0.001]. The other variables were similar in both groups.
Discussion
In the present single center retrospective observational study, regardless the equation used to estimate GFR, almost 60% of the elderly patients showed a decline in kidney function over a median of two years of follow-up. CKD progression was related to younger age, diabetic nephropathy, higher serum phosphorus and proteinuria.
It has been reported a rate of CKD progression varying from 13% to 70% [8, 12, 13]. Such wide variability might be partially explained by different equation, characteristics of the studied populations and the different criteria used across studies to define CKD progression. Although the calculation of GFR by CKD-EPI for elderly people has been questioned, studies that compared CKD-EPI’s accuracy with equations like BIS-1 and BIS– 2, developed specifically for elderly, there were no difference [4, 5]. Confirming this, in the present study, the CKD progression was calculated by CKD-EPI and BIS-1 was similar. Other reason that explain the high variation of CPK progression prevalence are the different criteria uses in the definition of progression. In the last years, CKD progression has been defined by reduction in 25–50% of GFR [14], change of CKD category [2], or the mean annual change of GFR over follow-up time, expressed in mL/min/year [9, 10]. Arora et al [10], in an elderly cohort, showed that less than fifty percent present CKD progression. Comparing our results, this less prevalence could be related with the definition of CKD progression (- 1 mL/min/1.73 m 2 /year) used in the study, once we and other authors [13] utilized a valor of < 0 mL/min/1.73 m 2 /year and found higher rates of progression. Unexpectedly, 43% of the patients presented some increase of eGFR during the study. The reasons why there was an improvement in the kidney function remain to be clarified. One could hypothesize that the implementation of the treatment could have had a beneficial impact in the eGFR. Moreover, some of the patients could have experienced an acute renal insult before the admission in the program. Of note, similar to our findings some authors also observed in prospective studies that 30% and 48% of the patients maintained or improved kidney function during the follow up [12, 13].
Several factors could be related to CKD progression, such as baseline eGFR, age, presence of proteinuria, and diabetes among others. Older age has been associated with the occurrence and higher progression of CKD [10, 11, 15, 16]. In a 3.322 adults patients cohort, 13% of the patients that declined kidney function 77% were elderly [8]. However, like ours, other studies [8, 13, 17] showed that the eGFR slope and its magnitude were higher in younger patients. A possible explanation for that, suggested by O´Hare et al, [18] is the competing risk for death over end renal stage kidney disease present in the elderly population. Besides age, the category of CKD influences on the disease progression. Elderly cohorts or predominantly elderly, the prevalence of CKD progression was higher as less as GFR of baseline with rates until 70% in patients with GFR < 30mL/min/1.73m2 [9, 12]. A meta-analysis that included 2 million participants, found that the lower eGFR at baseline, the higher magnitude of CKD progression [19]. This fact was confirmed when evaluated just elderly patients [9]. Differently, on this study, the GFR on baseline was similar in the progression and non progression groups. Unlike expected, fast progressors patients present a higher GFR at baseline. This fact could be observed for other authors [8].
The presence of proteinuria, the major marker of kidney damage, is the best-known risk factor for CKD progression. Several studies observed that proteinuria was associated with a faster rate of kidney function decline and achievement of ESRD [13, 19–21]. Recently, Arora et al [10], in an elderly cohort, similar to ours, showed that proteinuria was independently associated with increased eGFR slope.
Another important risk for CKD progression and faster decline of renal function is the presence of diabetes, in general [21, 22] and elderly population [9, 10]. Of note, in the present study, a higher prevalence of diabetic nephropathy in the progressor as well as in faster progressor patients was observed. However, in the multiple model analysis the presence of diabetic nephropathy was not associated to CKD progression probably due to its close relationship with proteinuria. Other factor involved in CKD progression is the calcium-phosphorus metabolism disorders. Several studies have shown an association between high serum phosphorus and risk of CKD progression [13, 23]. In our study, higher serum phosphorus was observed in the progressor group. Experimental study demonstrated that an increase phosphate excretion per nephron was associated with tubule-interstitial lesions including tubular atrophy and dilatation [24]. Moreover, high phosphorus contributes to the formation of calciprotein (cytotoxic nanoparticles of calcium-phosphate crystal and mineral binding proteins) that cause chronic inflammation and tubular damage [25]. Although based in unclear mechanisms, increased FGF-23 and decreased klotho expression, due to phosphorus overload [26], seem also to be related to CKD progression [23].
Some limitations of this study should be address: a single center and retrospective study, a relatively small follow up and proteinuria evaluated by spot urine sample. Despite that, using the two currently recommended equations for estimate GFR, this study was able to identify CKD progression in the majority of elderly patients.
In conclusion, CKD progression was observed in the majority of elderly CKD patients and proteinuria was the most important factor associated to kidney function decline in this population.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Jha V, Wang AY, Wang H. The impact of CKD identification in large countries: the burden of illness. Nephrol Dial Transplant. 2012;27 Suppl 3:iii32–8. 10.1093/ndt/gfs113 . [DOI] [PubMed] [Google Scholar]
- 2.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease.: Kidney International Supplement; 2013. p. 1–150. [Google Scholar]
- 3.Schaeffner ES, Ebert N, Delanaye P, Frei U, Gaedeke J, Jakob O, et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Annals of internal medicine. 2012;157(7):471–81. Epub 2012/10/03. 10.7326/0003-4819-157-7-201210020-00003 . [DOI] [PubMed] [Google Scholar]
- 4.Vidal-Petiot E, Haymann JP, Letavernier E, Serrano F, Clerici C, Boffa JJ, et al. External validation of the BIS (Berlin Initiative Study)-1 GFR estimating equation in the elderly. Am J Kidney Dis. 2014;63(5):865–7. Epub 2014/02/20. 10.1053/j.ajkd.2014.01.421 . [DOI] [PubMed] [Google Scholar]
- 5.Fan L, Levey AS, Gudnason V, Eiriksdottir G, Andresdottir MB, Gudmundsdottir H, et al. Comparing GFR Estimating Equations Using Cystatin C and Creatinine in Elderly Individuals. J Am Soc Nephrol. 2015;26(8):1982–9. Epub 2014/12/19. 10.1681/ASN.2014060607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cove-Smith WWA. Kidney disease in the elderly. Medicine 2015;43(8):489–92. 10.1016/j.mpmed.2015.05.002. [DOI] [Google Scholar]
- 7.Bakris GL, Sarafidis PA, Weir MR, Dahlof B, Pitt B, Jamerson K, et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet (London, England). 2010;375(9721):1173–81. Epub 2010/02/23. 10.1016/s0140-6736(09)62100-0 . [DOI] [PubMed] [Google Scholar]
- 8.Marks A, Fluck N, Prescott GJ, Robertson LM, Simpson WG, Smith WC, et al. Definitions of progression in chronic kidney disease—predictors and relationship to renal replacement therapy in a population cohort with a 6 year follow-up. Nephrol Dial Transplant. 2014;29(2):333–41. Epub 2013/09/29. 10.1093/ndt/gft393 . [DOI] [PubMed] [Google Scholar]
- 9.Hemmelgarn BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, et al. Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int. 2006;69(12):2155–61. Epub 2006/03/08. 10.1038/sj.ki.5000270 . [DOI] [PubMed] [Google Scholar]
- 10.Arora P, Jalal K, Gupta A, Carter RL, Lohr JW. Progression of kidney disease in elderly stage 3 and 4 chronic kidney disease patients. Int Urol Nephrol. 2017. Epub 2017/02/24. 10.1007/s11255-017-1543-9 . [DOI] [PubMed] [Google Scholar]
- 11.Sesso R, Prado F, Vicioso B, Ramos LR. Prospective study of progression of kidney dysfunction in community-dwelling older adults. Nephrology (Carlton). 2008;13(2):99–103. 10.1111/j.1440-1797.2008.00919.x . [DOI] [PubMed] [Google Scholar]
- 12.Baek SD, Baek CH, Kim JS, Kim SM, Kim JH, Kim SB. Does stage III chronic kidney disease always progress to end-stage renal disease? A ten-year follow-up study. Scand J Urol Nephrol. 2012;46(3):232–8. Epub 2012/05/01. 10.3109/00365599.2011.649045 . [DOI] [PubMed] [Google Scholar]
- 13.Yuste C, Barraca D, Aragoncillo-Sauco I, Vega-Martínez A, Abad S, Verdalles-Guzmán Ú, et al. Factors related with the progression of chronic kidney disease. Nefrologia. 2013;33(5):685–91. 10.3265/Nefrologia.pre2013.May.11900 . [DOI] [PubMed] [Google Scholar]
- 14.Rahman M, Baimbridge C, Davis BR, Barzilay J, Basile JN, Henriquez MA, et al. Progression of kidney disease in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin versus usual care: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Am J Kidney Dis. 2008;52(3):412–24. Epub 2008/08/05. 10.1053/j.ajkd.2008.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fox CS, Larson MG, Leip EP, Culleton B, Wilson PW, Levy D. Predictors of new-onset kidney disease in a community-based population. JAMA. 2004;291(7):844–50. 10.1001/jama.291.7.844 . [DOI] [PubMed] [Google Scholar]
- 16.McIntyre NJ, Fluck RJ, McIntyre CW, Taal MW. Risk profile in chronic kidney disease stage 3: older versus younger patients. Nephron Clin Pract. 2011;119(4):c269–76. 10.1159/000329109 . [DOI] [PubMed] [Google Scholar]
- 17.Shojamoradi MH, Saberi Isfeedvajani M, Mahdavi-Mazdeh M, Ahmadi F, Gatmiri SM, Abbasi Larki R. Chronic kidney disease progression in elderly Iranian patients: a cohort study. Nephrourol Mon. 2014;6(5):e20748 Epub 2014/09/05. 10.5812/numonthly.20748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Hare AM, Choi AI, Bertenthal D, Bacchetti P, Garg AX, Kaufman JS, et al. Age affects outcomes in chronic kidney disease. J Am Soc Nephrol. 2007;18(10):2758–65. Epub 2007/09/12. 10.1681/ASN.2007040422 . [DOI] [PubMed] [Google Scholar]
- 19.Hallan SI, Matsushita K, Sang Y, Mahmoodi BK, Black C, Ishani A, et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA. 2012;308(22):2349–60. 10.1001/jama.2012.16817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turin TC, James M, Ravani P, Tonelli M, Manns BJ, Quinn R, et al. Proteinuria and rate of change in kidney function in a community-based population. J Am Soc Nephrol. 2013;24(10):1661–7. Epub 2013/07/05. 10.1681/ASN.2012111118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones C, Roderick P, Harris S, Rogerson M. Decline in kidney function before and after nephrology referral and the effect on survival in moderate to advanced chronic kidney disease. Nephrol Dial Transplant. 2006;21(8):2133–43. Epub 2006/04/27. 10.1093/ndt/gfl198 . [DOI] [PubMed] [Google Scholar]
- 22.Vejakama P, Ingsathit A, Attia J, Thakkinstian A. Epidemiological study of chronic kidney disease progression: a large-scale population-based cohort study. Medicine (Baltimore). 2015;94(4):e475 10.1097/MD.0000000000000475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Voormolen N, Noordzij M, Grootendorst DC, Beetz I, Sijpkens YW, van Manen JG, et al. High plasma phosphate as a risk factor for decline in renal function and mortality in pre-dialysis patients. Nephrol Dial Transplant. 2007;22(10):2909–16. Epub 2007/05/21. 10.1093/ndt/gfm286 . [DOI] [PubMed] [Google Scholar]
- 24.Haut LL, Alfrey AC, Guggenheim S, Buddington B, Schrier N. Renal toxicity of phosphate in rats. Kidney Int. 1980;17(6):722–31. . [DOI] [PubMed] [Google Scholar]
- 25.Kuro-o M., Klotho phosphate and FGF-23 in ageing and disturbed mineral metabolism. Nat Rev Nephrol. 2013;9(11):650–60. Epub 2013/06/18. 10.1038/nrneph.2013.111 . [DOI] [PubMed] [Google Scholar]
- 26.Cheng CY, Kuro-o M, Razzaque MS. Molecular regulation of phosphate metabolism by fibroblast growth factor-23-klotho system. Advances in chronic kidney disease. 2011;18(2):91–27. Epub 2011/03/17. 10.1053/j.ackd.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.