Abstract
Background
There are substantial concerns about GP workload. The Quality and Outcomes Framework (QOF) has been perceived by both professionals and patients as bureaucratic, but the full impact of the QOF on GP workload is not well known.
Aim
To assess the impact of the QOF on GP consultation rates for patients with diabetes mellitus.
Design and setting
This study used interrupted time series of 13 248 745 general practice consultations for 37 065 patients with diabetes mellitus in England.
Method
Clinical Practice Research Datalink general practice data were used from 2000/2001 to 2014/2015, with introduction of the QOF (1 April 2004) as the intervention, and mean annual GP consultation rates as the primary outcome.
Results
Mean annual GP clinical consultation rates were 8.10 per patient in 2000/2001, 6.91 in 2004/2005, and 7.09 in 2014/2015. Introduction of the QOF was associated with an annual change in the trend of GP clinical consultation rates of 0.46 (95% confidence interval [CI] = 0.23 to 0.69, P = 0.001) consultations per patient, giving a post-QOF trend increasing by 0.018 consultations per year. Introduction of the QOF was associated with an immediate stepped increase of ‘other’ out-of-hours and non-clinical encounters, and trend change of 0.57 (95% CI = 0.34 to 0.81, P<0.001) per year, resulting in a post-QOF trend increasing by 0.27 other encounters per year.
Conclusion
Introduction of the QOF was associated with a modest increase in clinical GP consultation rates and substantial increase in other encounters for patients with diabetes independent of changes in diabetes prevalence. National prevalence of diabetes increased by 90.7% from 2004/2005 to 2014/2015, which, combined with this study’s findings, means GPs would have provided nearly double the number of consultations for patients with diabetes over this timescale.
Keywords: diabetes mellitus, incentives, primary care, workload
INTRODUCTION
Nearly two in five (39%) GPs report considerable or high likelihood of quitting direct patient care in the next 5 years, and it is known that increasing workloads is a leading contributor to GP stress.1 The Quality and Outcomes Framework (QOF) has been perceived by both professionals and patients to promote a more bureaucratic type of care, but the full impact of the QOF on GP workload is not well known.2 This groundbreaking pay-for-performance financial incentive scheme was introduced in 2004 as part of the new General Medical Services contract for GPs, linking approximately 25% of practice income to performance on a set of over 100 quality indicators.3–5 Income from the QOF has since fallen to 12–15% of practice income.6
Studies of the QOF have found it has had a modest impact on clinical care. A systematic review7 found modest improvements in diabetes care,8 modest slowing of a previously underlying increase in emergency admissions,9 increase in consultations for people with severe mental illness,10 and no clear association between the QOF and mortality.11 Removal of indicators from the QOF in 2006 and 2011 found levels of performance were generally stable after removal of the incentives;12 however, removal of further indicators in 2014 was associated with an immediate decline in documented quality of care.13
Improvements in patient care associated with the QOF may not have been achievable without increasing the frequency of general practice consultations, but few studies have directly examined this. A longitudinal study found that patients with serious mental illness had higher consultation rates than matched controls, and that the introduction of the QOF was associated with a modest increase in consultation rates for these patients.10
Diabetes was one of the original QOF conditions and has been consistently associated with a high number of points and therefore income. To the authors’ knowledge, the impact of the QOF on consultation rates for patients with diabetes has not been investigated previously. This study aimed to assess the impact of the introduction of the QOF on GP consultation rates for patients with diabetes mellitus.
METHOD
Data
The Clinical Practice Research Datalink (CPRD) is one of the largest longitudinal primary care databases in the world (https://www.cprd.com/home/). The study purposively sampled 125 practices from the CPRD database, to be broadly nationally representative in terms of list size and area deprivation in the practice locality. There were 2500 patients with one or more QOF conditions randomly sampled from each practice (all patients were sampled from practices with fewer than 2500 eligible patients). The variables were examined for integrity and miscoded data. Duplicate consultations of the same type, day, staff member, and patient were removed to avoid over-counting. (Please note, the dataset cannot be shared owing to licensing restrictions.)
How this fits in
There are substantial concerns about GP workload in England. The Quality and Outcomes Framework (QOF) was a groundbreaking financial incentive scheme introduced in 2004 for GPs in the UK that has had a modest impact on patient care, but its impact on GP workload is not well understood. This study demonstrates how the introduction of the QOF was associated with a modest increase in clinical GP consultation rates for patients with diabetes mellitus and a substantial increase in other GP encounters. When combined with increased prevalence of diabetes, this has contributed to a large increase in GP workload, and any refinements to the QOF need to carefully consider both impacts on patient quality of care and GP workload.
Study design
An interrupted time series (ITS) was used to assess trends in clinical consultation rates for patients with diabetes, with introduction of the QOF (on 1 April 2004) as the intervention. All entries to a patient’s electronic record are described by CPRD as a ‘consultation’. A ‘clinical consultation’ was defined as in-hours ‘direct contact between a clinician and a patient’ in keeping with previous studies;10 that is, all face-to-face, telephone, and home visit encounters. All other consultations captured by the CPRD were defined as ‘other’ encounters (further information on CPRD codes and Read codes are available from the authors on request); a highly heterogeneous group including out-of-hours and third-party consultations, mail from patients, hospital reports, and other non-clinical consultation entries were included to give some insight into changes in overall general practice activity in keeping with previous studies.10
The annual GP clinical consultation rate was chosen as the primary outcome, and annual practice nurse clinical consultation rates, type of GP consultation (face-to-face, telephone, and home visits), and other encounters as secondary outcomes. (Codes used to define ‘GP’ are available from the authors on request.)
Time was divided into 15 annual ‘bins’ corresponding with the financial years 2000/2001 to 2014/2015 in keeping with previous studies.8,10 All time points were included except for 1 April 2003 to 31 March 2004, which was treated as a ‘preparatory year’ and excluded in line with previous studies, as information about the QOF was publicly available during that time and may have influenced consultation rates.7,10,14 Separate models were used for each primary and secondary outcome.
There are no pre-defined limits to the number of data points needed for an ITS as the power depends not only on the number of data points, but also their distributions pre- and post-intervention, variability within the data, strength of effect, and confounding effects.15 However, ITS with 12–18 data points should be interpreted with some caution,16 and as such the primary outcome was also analysed at quarterly intervals.
Participants
There were 37 065 patients with diabetes in the sample after the selection process. Patients with diabetes mellitus were identified using a broader list of diagnostic Read codes than that captured by QOF registers. (Read code information is available from the authors on request.) Once diagnosed, the condition was assumed to be permanent in keeping with other studies.10 This study aimed to include all GP clinical consultation data post-diagnosis for all patients with diabetes (regardless of indication), including those registered for a short period of time or those nearing the end of their life, as these comprise an important part of GP workload.
A patient was defined as ‘active’ in an annual bin and their consultation data collected if: 1) they were registered with the practice and diagnosed with diabetes prior to the end of that bin; 2) did not transfer out or die until after the start of that bin; 3) the practice had their last collection date after the end of that bin; and 4) the practice data were at research standard. All other consultation data were excluded.
Patient demographics
Patient age was approximated to the nearest year for anonymity. Age range, mean, standard deviation, median, interquartile range, and sex distribution for each year is given.
Statistical methods
Annual consultation rates were calculated as the number of consultations divided by the number of active patient days in each bin, multiplied by 365 (366 for leap years). Quarterly analysis was calculated as consultation rates per patient day. To test the null hypothesis that consultation rates did not change following the introduction of the QOF, an ITS analysis using segmented linear regression analyses was performed to assess relationships between consultation rates and time with dummy variables for the introduction of the QOF. A Durbin–Watson statistic was calculated for each of the regression analyses to test for serial autocorrelation of the error terms in the regression model.17,18 Values can range from 0 to 4 and values close to 2 indicate no first-order auto-correlation. A Prais–Winsten statistic was used for Durbin–Watson statistics outside of the 1.5–2.5 range; Prais–Winsten uses a generalised least-squares method to estimate the parameters in a linear regression model in which the errors are assumed to follow a first-order autoregressive process.19 Data were analysed using Stata version 15 and α level of 5%.
RESULTS
There were 37 065 patients with a diagnosis of diabetes, and a total of 13 248 745 consultations included in the sample during the study period; 6119 consultations without a date were excluded.
Patient demographics
The age range of patients was 0–106 years, and mean age increased from 63.3 years in 2000/2001 to 64.5 years in 2014/2015 (Table 1). The proportion of males increased from 54.4% in 2000/2001 to 56.9% in 2014/2015, and the number of active patients with diabetes mellitus increased from 5080 in 2000/2001 to 15 056 in 2014/2015.
Table 1.
Patient demographics of the sample each year
| Year | Age range, years | Mean age, years (SD) | Median age, years (IQR) | Number of ‘active’ patients with diabetes | Male (%) | Female (%) |
|---|---|---|---|---|---|---|
| 2000/2001 | 0–102 | 63.3 (15.7) | 66 (54–74) | 5080 | 2764 (54.4) | 2316 (45.6) |
| 2001/2002 | 2–103 | 63.5 (15.4) | 66 (55–75) | 6616 | 3607 (54.5) | 3009 (45.5) |
| 2002/2003 | 3–100 | 63.6 (15.4) | 66 (55–75) | 8255 | 4515 (54.7) | 3740 (45.3) |
| 2003/2004 | 0–101 | 63.7 (15.4) | 66 (55–75) | 9909 | 5472 (55.2) | 4437 (44.8) |
| 2004/2005 | 1–99 | 63.7 (15.4) | 66 (55–75) | 11 197 | 6207 (55.4) | 4990 (44.6) |
| 2005/2006 | 1–105 | 63.8 (15.4) | 66 (55–75) | 12 971 | 7172 (55.3) | 5799 (44.7) |
| 2006/2007 | 2–106 | 63.7 (15.4) | 66 (55–75) | 14 069 | 7769 (55.2) | 6300 (44.8) |
| 2007/2008 | 2–104 | 63.8 (15.4) | 65 (55–75) | 14 885 | 8281 (55.6) | 6604 (44.4) |
| 2008/2009 | 1–101 | 63.9 (15.3) | 65 (55–75) | 15 833 | 8874 (56.0) | 6959 (44.0) |
| 2009/2010 | 1–102 | 63.9 (15.4) | 65 (55–75) | 17 029 | 9596 (56.4) | 7433 (43.6) |
| 2010/2011 | 2–103 | 63.9 (15.4) | 65 (55–75) | 18 266 | 10 335 (56.6) | 7931 (43.4) |
| 2011/2012 | 2–104 | 64.0 (15.5) | 66 (55–75) | 19 367 | 10 994 (56.8) | 8373 (43.2) |
| 2012/2013 | 3–105 | 64.2 (15.5) | 66 (55–75) | 20 698 | 11 713 (56.6) | 8985 (43.4) |
| 2013/2014 | 3–104 | 64.5 (15.4) | 66 (55–75) | 18 363 | 10 528 (57.3) | 7835 (42.7) |
| 2014/2015 | 0–102 | 64.5 (15.4) | 66 (55–75) | 15 056 | 8574 (56.9) | 6482 (43.1) |
IQR = interquartile range. SD = standard deviation.
Consultation rates in 2000/2001
The mean observed annual clinical consultation rate per patient with diabetes was 11.06, of which 8.10 were with GPs and 2.96 with nurses. There were 4.22 additional other encounters (Table 2).
Table 2.
Observed annual consultation rates per patient with GPs and nurses for patients with diabetes
| Year | Total GP clinical | GP face-to-face | GP telephone | Home visit | Other encounters | Total nurse clinical | Total clinical (GP plus nurse) | Nurse proportion of total clinical, % |
|---|---|---|---|---|---|---|---|---|
| 2000/2001 | 8.10 | 7.20 | 0.51 | 0.39 | 4.22 | 2.96 | 11.06 | 26.8 |
| 2001/2002 | 7.92 | 7.18 | 0.39 | 0.35 | 3.77 | 3.30 | 11.22 | 29.4 |
| 2002/2003 | 7.21 | 6.57 | 0.33 | 0.32 | 3.62 | 3.60 | 10.81 | 33.3 |
| 2003/2004 | 7.03 | 6.38 | 0.32 | 0.32 | 4.70 | 3.81 | 10.84 | 35.1 |
| 2004/2005 | 6.91 | 6.19 | 0.38 | 0.34 | 5.98 | 4.06 | 10.97 | 37.0 |
| 2005/2006 | 7.12 | 6.44 | 0.37 | 0.31 | 6.41 | 4.19 | 11.32 | 37.0 |
| 2006/2007 | 7.01 | 6.31 | 0.42 | 0.28 | 6.90 | 4.22 | 11.23 | 37.6 |
| 2007/2008 | 6.74 | 5.96 | 0.47 | 0.31 | 6.97 | 4.11 | 10.85 | 37.9 |
| 2008/2009 | 6.72 | 5.92 | 0.49 | 0.31 | 7.46 | 4.04 | 10.76 | 37.5 |
| 2009/2010 | 6.96 | 6.13 | 0.54 | 0.29 | 7.58 | 4.09 | 11.05 | 37.0 |
| 2010/2011 | 6.98 | 6.19 | 0.53 | 0.26 | 7.70 | 3.91 | 10.89 | 35.9 |
| 2011/2012 | 7.02 | 6.22 | 0.54 | 0.26 | 8.00 | 3.86 | 10.88 | 35.5 |
| 2012/2013 | 7.05 | 6.26 | 0.53 | 0.26 | 8.26 | 3.75 | 10.80 | 34.7 |
| 2013/2014 | 7.15 | 6.23 | 0.66 | 0.26 | 8.84 | 3.80 | 10.95 | 34.7 |
| 2014/2015 | 7.09 | 6.12 | 0.71 | 0.26 | 8.79 | 3.83 | 10.92 | 35.1 |
From the model, patients with diabetes had a mean 11.15 (95% confidence interval [CI] = 10.32 to 11.70) clinical consultations per year with their practice in 2000/2001, including 8.19 (95% CI = 7.47 to 8.91) with GPs and 2.96 (95% CI = 2.57 to 3.36) with nurses. There were 4.17 (95% CI = 3.45 to 4.90) other GP encounters per year (data not shown).
Impact of the QOF on consultation rates
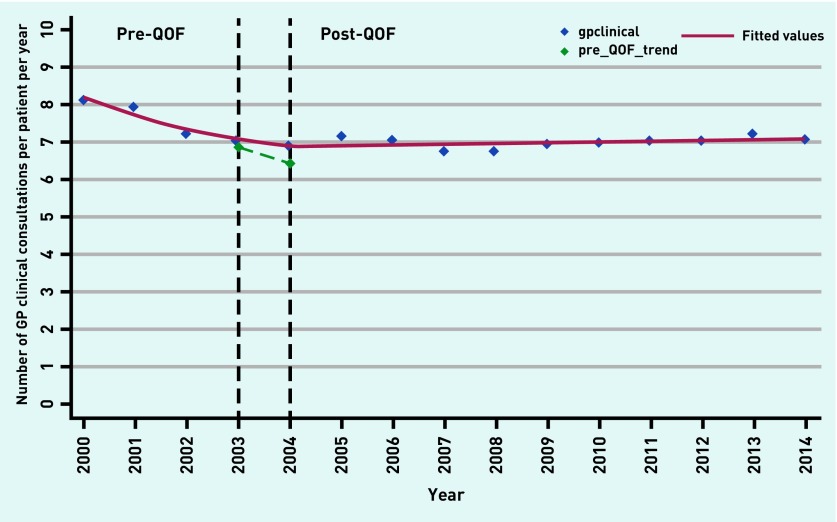
GP clinical consultation rates fell by nearly half a consultation (−0.45, 95% CI = −0.67 to −0.22) per year in the pre-QOF period (Table 3, Figure 1). When the QOF was introduced, there was an immediate non-significant rise of 0.017 (95% CI = −0.52 to 0.55, P = 0.95) GP clinical consultations per year. The magnitude of the underlying trend increased by nearly half a consultation (0.46, 95% CI = 0.23 to 0.69, P = 0.001) per year, giving a post-QOF trend increasing by 0.018 consultations per year. These trends are supported by the quarterly analysis (Table 3).
Table 3.
Interrupted time series analysis by type of consultation
| Dependent variable (consultation type) | Coefficient | P-value | 95% CI | Durbin–Watson | |
|---|---|---|---|---|---|
| Total GP clinical (annual) | Change in rate per year 2000–2003 | −0.445 | 0.001 | −0.673 to −0.217 | 1.62 |
| Step change in 2004 | 0.017 | 0.945 | −0.519 to 0.553 | ||
| Change in trend in 2004 | 0.463 | 0.001 | 0.232 to 0.693 | ||
| Post-QOF trend | 0.018 | ||||
|
| |||||
| Face-to-face | Change in rate per year 2000–2003 | −0.315 | 0.022 | −0.575 to −0.055 | 1.62 |
| Step change in 2004 | −0.144 | 0.610 | −0.754 to 0.466 | ||
| Change in trend in 2004 | 0.310 | 0.025 | 0.048 to 0.572 | ||
| Post-QOF trend | −0.005 | ||||
|
| |||||
| Telephone | Change in rate per year 2000–2003 | −0.090 | 0.004 | −0.145 to −0.035 | 1.56 |
| Step change in 2004 | 0.102 | 0.108 | −0.026 to 0.230 | ||
| Change in trend in 2004 | 0.120 | 0.001 | 0.065 to 0.175 | ||
| Post-QOF trend | 0.030 | ||||
|
| |||||
| Home visit | Change in rate per year 2000–2003 | −0.035 | 0.007 | −0.058 to −0.012 | 1.61 |
| Step change in 2004 | 0.046 | 0.085 | −0.008 to 0.100 | ||
| Change in trend in 2004 | 0.028 | 0.024 | 0.004 to 0.051 | ||
| Post-QOF trend | −0.007 | ||||
|
| |||||
| Other | Change in rate per year 2000–2003 | −0.300 | 0.015 | −0.529 to −0.071 | 2.13 |
| Step change in 2004 | 2.621 | <0.001 | 2.083 to 3.159 | ||
| Change in trend in 2004 | 0.574 | <0.001 | 0.343 to 0.806 | ||
| Post-QOF trend | 0.274 | ||||
|
| |||||
| Nurse | Change in rate per year 2000–2003 | 0.321 | <0.001 | 0.195 to 0.447 | 1.43 |
| Step change in 2004 | 0.321 | 0.036 | 0.025 to 0.616 | ||
| Change in trend in 2004 | −0.364 | <0.001 | −0.491 to −0.237 | ||
| Post-QOF trend | −0.043 | ||||
|
| |||||
| Nurse (Prais–Winsten adjustment) | Change in rate per year 2000–2003 | 0.321 | <0.001 | 0.196 to 0.446 | 1.59 |
| Step change in 2004 | 0.311 | 0.045 | 0.009 to 0.612 | ||
| Change in trend in 2004 | −0.363 | <0.001 | −0.489 to −0.236 | ||
| Post-QOF trend | −0.042 | ||||
|
| |||||
| GP and nurse clinical consultations | Change in rate per year 2000–2003 | −0.121 | 0.331 | −0.384 to 0.143 | 2.09 |
| Step change in 2004 | 0.328 | 0.265 | −0.291 to 0.947 | ||
| Change in trend in 2004 | 0.096 | 0.442 | −0.171 to 0.362 | ||
| Post-QOF trend | −0.025 | ||||
|
| |||||
| Total GP clinical (quarterly consultation rates per patient day) | Change in rate per year 2000–2003 | −0.00029 | <0.001 | −0.00042 to −0.00016 | 1.72 |
| Step change in 2004 | 0.00028 | 0.698 | −0.00116 to 0.00178 | ||
| Change in trend in 2004 | 0.00031 | <0.001 | 0.00017 to 0.00044 | ||
| Post-QOF trend | 0.00003 | ||||
QOF = Quality and Outcomes Framework.
Figure 1.
Annual GP clinical consultation rates per patient per year over time (year 2000 = 2000/2001, 2001 = 2001/2002, and so on) against predicted fitted values for patients with diabetes mellitus. Modelled estimates for 2003/2004 and 2004/2005 are shown based on the pre-QOF trend (pre_QOF_trend). QOF = Quality and Outcomes Framework.
Type of clinical GP consultation
Introduction of the QOF had a statistically significant impact on the previous declining trend for face-to-face, telephone, and home visit consultation rates (Table 3). The post-QOF trend of face-to-face and home visit consultations declined after the introduction of the QOF by 0.005 and 0.007 consultations per year, respectively, while telephone consultations increased by 0.03 per year.
Nurse consultations
Nurse consultations increased by 0.32 (95% CI = 0.20 to 0.45, Prais–Winsten adjustment) consultations per patient per year prior to the QOF. Immediately after the introduction of the QOF there was a stepped change of 0.31 (95% CI = 0.009 to 0.61, P = 0.045, Prais–Winsten adjustment), and the magnitude of the trend changed by −0.36 (95% CI = −0.49 to −0.24, P<0.001, Prais–Winsten adjustment) consultations per year, giving a post-QOF trend falling by 0.042 consultations per patient per year (Table 3).
Taking GP and nurse clinical consultations together, trends remained relatively static throughout the study period. Prior to the QOF, combined GP and nurse consultations fell by −0.12 (95% CI = −0.38 to 0.14, P = 0.331) per patient per year. After introduction of the QOF, there was a non-significant stepped change of 0.33 (95% CI = −0.29 to 0.95, P = 0.265) combined consultations and an increase in trend of 0.096 (95% CI = −0.17 to 0.36, P = 0.442) per year, giving a post-QOF trend falling by 0.025 consultations per patient per year. The proportion of nurse consultations increased from 26.8% in 2000/2001 to 37.0% in 2004/2005 and declined to 35.1% in 2014/2015 (Table 2).
Other consultations
From the model, patients had 4.17 other encounters with GPs in 2000/2001 such as out-of-hours consultations, non-consultation administrative entries, and test results. (Further data are available from the authors on request.) Trends in other encounters fell by −0.30 per patient per year prior to the QOF (95% CI = −0.53 to −0.071). Immediately after the introduction of the QOF there was a stepped increase of 2.62 (95% CI = 2.08 to 3.16, P<0.001) encounters, and the trend increased by 0.57 (95% CI = 0.34 to 0.81, P<0.001) per year, resulting in a post-QOF trend increasing by 0.274 per patient per year (Table 3).
DISCUSSION
Summary
Introduction of the QOF was associated with a modest increase in clinical GP consultation rates and a substantial increase in other encounters for patients with diabetes mellitus independent of changes in diabetes prevalence. Patients with a diagnosis of diabetes had 8.10 clinical consultations per year with their GP in 2000/2001, 6.91 in 2004/2005, and 7.09 in 2014/2015. From 2000/2001 to 2002/2003 these consultation rates were decreasing at a rate of −0.45 per patient per year. After the introduction of the QOF, the slope of the trend changed by 0.46 consultations per patient per year, and post-QOF annual GP consultation rates increased by 0.018 per year. The QOF was associated with statistically significant changes in the trends for all types of GP consultation. The biggest change was for other encounters: with a step change increase of 2.6 encounters immediately after the introduction of the QOF, the magnitude of the pre-QOF trend increased by 0.57 giving a post-QOF trend increasing by 0.27 per patient per year.
In contrast, nurse clinical consultations, which were increasing prior to the introduction of the QOF, had a stepped increase when the QOF was introduced, but subsequently fell. This decrease in nurse consultations offset the increase in GP consultations, so that overall rates remained relatively static throughout the study period. This suggests potential shifting of workload between GPs and nurses.
Strengths and limitations
This is the first longitudinal study that the authors are aware of that gives estimates for GP consultation rates for patients with diabetes mellitus, and how these have changed over time. One of the main strengths of this study is that it uses routinely collected consultation data from individual patient records drawn from a nationally representative sample of practices, capturing real-life practice.
However, there are a number of limitations. First, this is an observational study and so it cannot be certain that changes in consultation rates are fully attributable to the introduction of the QOF. It was not possible to include a control group as the QOF was introduced at a national level and there are no comparable national systems with available data to act as a control. However, ITS is the best quasi-experimental design for evaluating longitudinal effects of interventions in the absence of a control group.17
Second, this study shows changes in trends in consultation rates per patient with diabetes, independent of prevalence. Prevalence of diabetes mellitus since the QOF was introduced has increased by 90.7% from 3.34% in 2004/2005 to 6.37% in 2014/2015,20,21 so workload impacts at a practice level will be much higher. Changes in clinical diagnostic criteria such as use of glycated haemoglobin (HbA1c) recommended by the World Health Organization in 2011,22 and the fact that diabetes is being detected at an earlier stage than in the past,23 may alter the sample over time. The code list used in this study for diabetes may vary slightly from those used in other studies and may result in some selection bias. The sample in the current study was derived from a dynamic, purposively sampled population of patients with one or more QOF indications where the number of other QOF indicators may influence the number of patients in the sample each year. The current study considers all patients with diabetes captured by the sampling method rather than a specific subgroup.
Third, this study does not capture changes in other parts of care such as community appointments with diabetes specialist nurses or hospital care. All consultations, regardless of indication, were included rather than those specifically coded for diabetes due to concerns of coding accuracy for patients presenting with multiple conditions, therefore, the consultation rates are for patients with diabetes rather than specifically for diabetes care.
Fourth, the biggest change reported was for other encounters, which need to be interpreted with caution as this is a heterogeneous group of encounters. (Further information on CPRD consultation codes are available from the authors on request.) CPRD only captures computerised parts of the clinical record, and it is likely there was heterogeneity among practices regarding which parts of the record were computerised and when. In addition, ‘other encounters’ includes out-of-hours clinical GP encounters. However, the ‘other’ category does give an indication of the increasing electronic and administrative workload faced by GPs.
Comparison with existing literature
This study supports previous literature that total general practice workload has increased by 16% from 2007 to 2014.24 Previous literature has also shown practice nurses accounted for 30.6% to 32.2% of consultations for patients with diabetes from 2002 to 2011.23 A study investigating the impact of the QOF on consultation rates, comparing patients with serious mental illness to matched controls, found similar trends to those in this current study. Annual face-to-face consultation rates in the control group decreased by −0.05 per patient per year in the pre-QOF period and increased by 0.01 per patient per year post-QOF. For patients with serious mental illness, annual consultation rates declined by −0.04 per patient per year pre-QOF and increased by 0.19 consultations per patient per year post-QOF.10 Changes in other encounters may be explained in part by administrative GP work associated with tests, as it is estimated that the average GP spent 1.5–2.0 hours reviewing tests each work day in 2015/2016 compared with 25–35 minutes a day in 2000/2001 as the number of tests has increased substantially.25 For example, the diabetes QOF indicators include albumin:creatinine ratio test and cholesterol measurement in the preceding 12 months and serum HbA1c titration to target.26
Implications for research and practice
This study has provided evidence that introduction of the QOF was associated with a modest increase in clinical consultations with GPs at an individual patient level and more substantial increase in other encounters for GPs. However, at a practice level, this combined with increases in diabetes prevalence means a large increase in workload. For example, NHS Digital reported mean practice list size in 2014 as 6944;27 based on the authors’ observed consultation rates, a static practice of 6944 patients with prevalence of 3.34% diabetes in 2004/200520 and 6.37% in 2014/201521 would have provided 1602 GP clinical consultations for patients with diabetes in 2004/2005 and nearly double this number (95.8% increase) at 3137 per year in 2014/2015. Similarly, general practices would have provided 1411 other encounters for patients with diabetes in a practice of 6944 patients in 2004/2005 compared with 4087 other encounters in 2014/2015, and further consideration of the impact of the QOF on non-clinical workload is warranted. This current study is likely to have underestimated total increases in GP workload as other studies of GP workload have shown GP consultation length has increased as well as rate.24 Total practice burden of work imposed by the QOF is likely to be even higher as administrative work by other members of the team recording the data needed for QOF payments is not captured.
Increases in consultation rates are not necessarily undesirable, as improvements in clinical outcomes are likely to have been influenced by clinical activity. However, both GPs and practice nurses face a recruitment crisis, as 15.3% of GP positions and 12.5% of practice nurse positions are currently unfilled,28,29 and any further refinement and development of the QOF system expected after the recent NHS England review of the QOF30 needs to carefully consider impact on patient quality of care and both GP and nurse workload.
The QOF has been discontinued in Scotland, with its quality improvement function being replaced by a system of GP peer-support clusters.31 GPs in Scotland are divided on whether stopping the QOF had eased workload; when surveyed, 40% thought workload had not improved, 33% thought it had, and 27% were unsure.32 This demonstrates the importance of carefully considering the implications on workload of introducing, and of removing, quality improvement initiatives.33
Acknowledgments
Thanks to Lu Han and Robert Smith (Research Fellows at the University of York) for their advice and assistance extracting the data into the sample used in this study.
Funding
This study was not directly funded. The National Institute for Health Research funded Claire Gilbert’s Academic Clinical Fellowship salary while this work was conducted. The interpretation and conclusions contained in this study are those of the authors alone.
Ethical approval
The dataset in this study was approved by the independent scientific advisory committee (ISAC) for Clinical Practice Research Datalink research (reference number: 14_104R). All data were provided in anonymised form and provided by consenting practices. No further ethics approval was required for the analysis of the data.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Gibson J, Sutton M, Spooner S, Checkland K. Ninth National GP Worklife Survey. 2017. PRUComm. http://blogs.lshtm.ac.uk/prucomm/files/2018/05/Ninth-National-GP-Worklife-Survey.pdf (accessed 3 Jul 2019)
- 2.Guthrie B, Tang J. What did we learn from 12 years of QOF? Scottish School of Primary Care. 2016 http://www.sspc.ac.uk/media/media_547662_en.pdf (accessed 3 Jul 2019) [Google Scholar]
- 3.Roland M. Linking physicians’ pay to the quality of care — a major experiment in the United Kingdom. N Engl J Med. 2004;351(14):1448–1454. doi: 10.1056/NEJMhpr041294. [DOI] [PubMed] [Google Scholar]
- 4.NHS Employers Quality and Outcomes Framework. 2017. https://www.nhsemployers.org/pay-pensions-and-reward/primary-care-contacts/general-medical-services/quality-and-outcomes-framework (accessed 2 Jul 2019)
- 5.Health and Social Care Information Centre QOF 2004/05 background. 2012 https://nhsenglandfilestore.s3.amazonaws.com/qof/a650e6029e37652784108896e7021f8c.pdf (accessed 3 Jul 2019) [Google Scholar]
- 6.General Practitioners Committee . Focus on GP quality indicators. British Medical Association; 2018. [Google Scholar]
- 7.Forbes LJ, Marchand C, Doran T, Peckham S. The role of the Quality and Outcomes Framework in the care of long-term conditions: a systematic review. Br J Gen Pract. 2017 doi: 10.3399/bjgp17X693077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kontopantelis E, Reeves D, Valderas JM, et al. Recorded quality of primary care for patients with diabetes in England before and after the introduction of a financial incentive scheme: a longitudinal observational study. BMJ Qual Saf. 2012;22(1):53–64. doi: 10.1136/bmjqs-2012-001033. [DOI] [PubMed] [Google Scholar]
- 9.Harrison MJ, Dusheiko M, Sutton M, et al. Effect of a national primary care pay for performance scheme on emergency hospital admissions for ambulatory care sensitive conditions: controlled longitudinal study. BMJ. 2014;349:g6423. doi: 10.1136/bmj.g6423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kontopantelis E, Olier I, Planner C, et al. Primary care consultation rates among people with and without severe mental illness: a UK cohort study using the Clinical Practice Research Datalink. BMJ Open. 2015;5(12):e008650. doi: 10.1136/bmjopen-2015-008650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryan AM, Krinsky S, Kontopantelis E, Doran T. Long-term evidence for the effect of pay-for-performance in primary care on mortality in the UK: a population study. Lancet. 2016;388(10041):268–274. doi: 10.1016/S0140-6736(16)00276-2. [DOI] [PubMed] [Google Scholar]
- 12.Kontopantelis E, Springate D, Reeves D, et al. Withdrawing performance indicators: retrospective analysis of general practice performance under UK Quality and Outcomes Framework. BMJ. 2014;348:g330. doi: 10.1136/bmj.g330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Minchin M, Roland M, Richardson J, et al. Quality of care in the United Kingdom after removal of financial incentives. N Engl J Med. 2018;379(10):948–957. doi: 10.1056/NEJMsa1801495. [DOI] [PubMed] [Google Scholar]
- 14.Doran T, Kontopantelis E, Valderas JM, et al. Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK Quality and Outcomes Framework. BMJ. 2011;342:d3590. doi: 10.1136/bmj.d3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang F, Wagner AK, Ross-Degnan D. Simulation-based power calculation for designing interrupted time series analyses of health policy interventions. J Clin Epidemiol. 2011;64(11):1252–1261. doi: 10.1016/j.jclinepi.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 18.Durbin J, Watson GS. Testing for serial correlation in least squares regression. I. Biometrika. 1950;37(3–4):409–428. [PubMed] [Google Scholar]
- 19.Linden A, Arbor A. Conducting interrupted time-series analysis for single-and multiple-group comparisons. Stata J. 2015;15(2):480–500. [Google Scholar]
- 20.NHS Digital Quality and Outcomes Framework, achievement, prevalence and exceptions data. (Quality and Outcomes Framework — England, 2004–05 SHA and England level, Data tables, Disease prevalence). https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/quality-and-outcomesframework-statistics-england-2004-05-sha-level (accessed 5 Jul 2019)
- 21.NHS Digital Quality and Outcomes Framework, achievement, prevalence and exceptions data. (QOF 2014–15 Report for England v1.1) https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/quality-and-outcomes-framework-qof-2014-15 (accessed 5 Jul 2019)
- 22.World Health Organization Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. Abbreviated report of a WHO consultation. 2011. https://www.who.int/diabetes/publications/diagnosis_diabetes2011/en/ (accessed 3 Jul 2019) [PubMed]
- 23.Murrells T, Ball J, Maben J, et al. Nursing consultations and control of diabetes in general practice: a retrospective observational study. Br J Gen Pract. 2015 doi: 10.3399/bjgp15X686881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hobbs FDR, Bankhead C, Mukhtar T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet. 2016;387(10035):2323–2330. doi: 10.1016/S0140-6736(16)00620-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Sullivan JW, Stevens S, Hobbs FDR, et al. Temporal trends in use of tests in UK primary care, 2000–15: retrospective analysis of 250 million tests. BMJ. 2018;363:k4666. doi: 10.1136/bmj.k4666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Institute for Health and Care Excellence NICE Quality and Outcomes Framework indicator. About QOF https://www.nice.org.uk/standards-and-indicators/qofindicators (accessed 3 Jul 2019)
- 27.Health and Social Care Information Centre General practice trends in the UK to 2015. 2016. http://content.digital.nhs.uk/media/21726/General-Practice-Trends-in-the-UK-to-2015/pdf/General_Practice_Trends_in_the_UK_to_2015.pdf (accessed 3 Jul 2019)
- 28.Rosser E. Revealed: GP vacancy rates rocket with one in six roles unfilled. Pulse. 2018. Jul 6, http://www.pulsetoday.co.uk/partners-/practice-business/revealed-gp-vacancy-rates-rocket-with-one-in-six-roles-unfilled/20036995.article (accessed 3 Jul 2019)
- 29.Madsen M. One in eight GP practice nurse positions is vacant. Pulse. 2016. Jun 17, http://www.pulsetoday.co.uk/news/gp-topics/employment/one-in-eight-gp-practice-nurse-positions-is-vacant/20032083.article (accessed 3 Jul 2019)
- 30.NHS England Report of the Review of the Quality and Outcomes Framework in England. 2018. https://www.england.nhs.uk/publication/report-of-the-review-of-the-quality-and-outcomes-framework-in-england/ (accessed 3 Jul 2019)
- 31.British Medical Association QOF guidance. 2018. https://www.bma.org.uk/advice/employment/contracts/gp-partner-contracts/qof-guidance (accessed 3 Jul 2019)
- 32.Bostock N. Exclusive: GPs back scrapping QOF to ease practice workload. GP Online. 2016. Aug 19, http://www.gponline.com/exclusive-gps-back-scrapping-qof-ease-practice-workload/article/1404620 (accessed 3 Jul 2019)
- 33.Scottish Government Improving together: a national framework for quality and GP clusters in Scotland. 2017. https://www.gov.scot/publications/improving-together-national-framework-quality-gp-clusters-scotland/ (accessed 3 Jul 2019)