Abstract
Air embolism is a rare, often misdiagnosed, potentially fatal condition. It is most frequently associated with invasive vascular procedures and mechanical ventilation. Air emboli developing from peripheral intravenous lines are uncommon. We present a case of symptomatic venous air embolism likely arising from peripheral intravenous access gained during an interventional pain procedure. This case highlights the need to consider air embolism in the differential diagnoses of patients presenting with neurological symptoms following vascular interventions.
Keywords: Air embolism, intravenous access, interventional pain procedure
Air embolism is a predominantly iatrogenic condition that most frequently arises following otolaryngological and neurosurgical procedures, cervical spine fusion, barotrauma, use of rapid infusion systems, and invasive vascular procedures.1–8 Air embolism has been reported with insertion or removal of intravenous catheters at an estimated incidence of 1 in 47 to 1 in 3000.1 Though the risk of air introduction is present with any vascular intervention,8 few cases of air embolism have been reported from intravenous access alone.
CASE DESCRIPTION
A 47-year-old woman presented with sudden-onset, pulsatile, nonradiating left temporal headache, slurred speech, gait imbalance, and vertigo, which started 12 hours before presentation. She denied prior episodes, recent trauma, fever, ear discharge, nausea, and vomiting. She received regular facet joint blocks for her back pain; her most recent injection had been 2 days earlier. She described difficulty obtaining intravenous access prior to the nerve block. On arrival in the emergency department, she was alert and oriented. Her temperature was 36.3°C; blood pressure 165/90 mm Hg; heart rate 52 beats/min; respirations 20 breaths/min; and oxygen saturation 100% on room air.
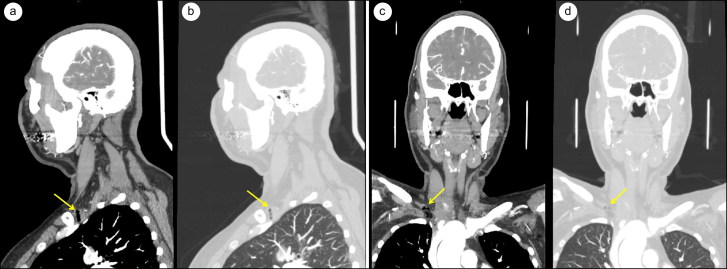
Her pupils were round, regular, equal, and reactive to light and accommodation. Extraocular movements were intact without nystagmus. She had full visual fields. Funduscopy demonstrated a normal optic disk and retinal vessels. No facial weakness or asymmetry was present. The tongue was midline without atrophy or fasciculations. Deep tendon reflexes were intact and symmetrical. Muscle strength was 5/5 in all extremities. Her gait was wobbly and slow. Otherwise, her physical examination was unremarkable. An electrocardiogram revealed sinus rhythm with normal PR, QRS, and QT intervals. Computed tomography (CT) of the head revealed no intracranial pathology, but CT angiogram detected air in the main pulmonary arteries, right cavernous sinus, subclavian veins, and deep tissues of the neck (Figure 1).
Figure 1.
CT angiogram of the neck. (a, b) Sagittal views showing punctate air lobules in the right subclavian vein (arrows). (c, d) Coronal views showing punctate air lobules in the right subclavian vein (arrows).
The patient was started on high-flow oxygen, placed in the Trendelenburg position, and admitted to the medical intensive care unit. Magnetic resonance imaging revealed no evidence of ischemia. Transthoracic echocardiogram with agitated saline did not show any septal defects. Her symptoms improved over the next 3 days. Repeat imaging 48 hours later demonstrated resolution of the air emboli. The patient displayed minimal residual intermittent lightheadedness at discharge without specific aggravating or relieving factors but was otherwise stable.
DISCUSSION
The severity of air embolism is determined largely by the volume of air and the rate at which it enters the circulation.3 A pressure gradient of just 5 cm of H2O across a 14-gauge needle can generate an airflow of 100 mL/s, capable of delivering a lethal dose of air in seconds.9 For venous air embolism, the pressure gradient correlates closely to the height of the vein relative to the heart.
In this case, the patient had onset of neurological symptoms shortly after a facet joint block. Air embolism has been reported following hip and greater trochanteric bursa injections but has not been encountered as a complication of facet joint blocks.10 Intravenous access was difficult to obtain for sedation prior to this patient’s facet joint injection. She had no other history of recent intravascular interventions, indicating that intravenous access was the most likely source of the air embolism.
Management of suspected venous air embolism involves high-flow oxygen and repositioning the patient in the Trendelenburg and left lateral decubitus position (Durant’s maneuver).1 High-flow oxygen corrects hypoxemia and can cause air emboli to shrink by increasing the gradient for nitrogen to diffuse out of the air bubbles.11 The Trendelenburg position and Durant’s maneuver theoretically allow the air to pool in the apex of the right ventricle and prevent further embolization.12 In patients with hemodynamic instability or evidence of end-organ damage, treatment with hyperbaric oxygen therapy should be started. In addition to further increasing the rate of nitrogen resorption, hyperbaric oxygen physically compresses the air emboli through increased ambient pressure.2,3 Retrospective studies have provided evidence that early therapy (preferably within 6 hours) is associated with better outcomes.13,14
The occurrence of an air embolism in this patient following routine intravenous access suggests that this is a more common complication than previously thought. In addition, the patient displayed significant neurological symptoms that did not completely disappear despite resolution of the air emboli on imaging. This indicates the possibility of significant morbidity even in cases of nonlethal air embolism.
References
- 1.Gordy S, Rowell S. Vascular air embolism. Int J Crit Illn Inj Sci. 2013;3:73–76. doi: 10.4103/2229-5151.109428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarthy CJ, Behravesh S, Naidu SG, Oklu R. Air embolism: practical tips for prevention and treatment. J Clin Med. 2016;5:93. doi: 10.3390/jcm5110093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirski MA, Lele AV, Fitzsimmons L, Toung TJ. Diagnosis and treatment of vascular air embolism. Anesthesiology. 2007;106:164–177. doi: 10.1097/00000542-200701000-00026. [DOI] [PubMed] [Google Scholar]
- 4.van Hulst RA, Klein J, Lachmann B. Gas embolism: pathophysiology and treatment. Clin Physiol Funct Imaging. 2003;23:237–246. doi: 10.1046/j.1475-097X.2003.00505.x. [DOI] [PubMed] [Google Scholar]
- 5.Cruz AS, Moisi M, Page J, et al. Venous air embolus during prone cervical spine fusion: case report. J Neurosurg Spine. 2016;25:681–684. doi: 10.3171/2016.5.SPINE16109. [DOI] [PubMed] [Google Scholar]
- 6.Mercurio I, Capano D, Torre R, et al. A case of fatal cerebral air embolism after blunt lung trauma: postmortem computed tomography and autopsy findings. Am J Forensic Med Pathol. 2018;39:61–68. [DOI] [PubMed] [Google Scholar]
- 7.Pant D, Narani KK, Sood J. Significant air embolism: a possibility even with collapsible intravenous fluid containers when used with rapid infuser system. Indian J Anaesth. 2010;54:49–51. doi: 10.4103/0019-5049.60498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook LS. Infusion-related air embolism. J Infus Nurs. 2013;36:26–36. doi: 10.1097/NAN.0b013e318279a804. [DOI] [PubMed] [Google Scholar]
- 9.Flanagan JP, Gradisar IA, Gross RJ, Kelly TR. Air embolus—a lethal complication of subclavian venipuncture. N Engl J Med. 1969;281:488–489. doi: 10.1056/NEJM196908282810907. [DOI] [PubMed] [Google Scholar]
- 10.McCauley RG, Wunderlich BK, Zimbler S. Air embolism as a complication of hip arthrography. Skeletal Radiol. 1981;6:11–13. [DOI] [PubMed] [Google Scholar]
- 11.Piantadosi C, Brown S. Principles of Critical Care. 3rd ed New York, NY: McGraw-Hill; 2005. [Google Scholar]
- 12.Palmon SC, Moore LE, Lundberg J, Toung T. Venous air embolism: a review. J Clin Anesth. 1997;9:251–257. doi: 10.1016/S0952-8180(97)00024-X. [DOI] [PubMed] [Google Scholar]
- 13.Moon R, Gorman D Treatment of the decompression disorders. In: Brubakk A, Neuman T, eds. Physiology and Medicine of Diving. 5th ed London, UK: Saunders; 2003:600–650. [Google Scholar]
- 14.Blanc P, Boussuges A, Henriette K, Sainty JM, Deleflie M. Iatrogenic cerebral air embolism: importance of an early hyperbaric oxygenation. Intensive Care Med. 2002;28:559–563. doi: 10.1007/s00134-002-1255-0. [DOI] [PubMed] [Google Scholar]