Abstract
Objective:
To assess treatment preference and attributes of two exercise-based treatments for people with chronic low back pain (LBP).
Design:
Cross-sectional study.
Setting:
Academic research setting.
Participants:
Individuals (n=154) with chronic LBP.
Interventions:
Not applicable.
Main Outcome Measure(s):
Participants completed a treatment preference assessment measure that described two treatments for chronic LBP [strength and flexibility (SF) and motor skill training (MST)]. Participants rated each treatment on four attributes: effectiveness, acceptability/logicality, suitability/appropriateness, and convenience. An overall score for each treatment was calculated as the mean of the four attribute ratings. The participants indicated either (1) no treatment preference or (2) preference for SF or MST.
Results:
One hundred four participants (67.5%) had a treatment preference; of those, 95 (91.3%) preferred SF and nine (8.7%) preferred MST. The SF preference group rated SF higher than MST overall and on all attributes (all ps < .01, ds ranged from .48–1.07). The MST preference group did not rate the treatments differently overall or on any of the attributes (all ps > .05, ds ranged from .43-.66). Convenience of SF (p = .05, d = .79) and effectiveness (d = 1.20), acceptability/logicality (d = 1.27), and suitability/appropriateness (d = 1.52) of MST (all ps < .01) were rated differently between the two preference groups.
Conclusions:
When presented with two treatment options, a majority of patients preferred SF over MST. Convenience was a particularly important attribute impacting preference. Assessing treatment preference and attributes prior to treatment initiation allows the clinician to identify factors that may need to be addressed to enhance adherence to, and outcomes of, treatment.
Keywords: exercise therapy, low back pain, motor skill, patient preference
Low back pain (LBP) is a significant health problem, affecting 60–90% of adults.1,2 Up to 75% of patients with LBP continue to report pain and disability 12 months after an initial episode,3 indicating LBP can become a long-standing condition with persistent or recurrent symptoms and disability. Exercise is a common treatment for LBP,4,5 and studies have indicated that adherence to a LBP exercise program is related to improved pain and disability.6–9 Yet, research has shown that adherence to a treatment which involves a lifestyle change (e.g., exercise) is often low.10
Many factors can affect adherence, including treatment preference.9–11 Treatment preference is the option a patient chooses after considering the risks and benefits of the multiple options available for treatment of a clinical condition.12 Treatment preference has been examined minimally in LBP,13–15 and the effect of treatment preference on adherence and outcomes in LBP is inconclusive due to the inadequate methodology used to assess preference.16–19 However, it is particularly important to assess treatment preference, and what contributes to that preference, in this population due to the equivalency of the treatment options.5,19–22
Treatment preference is, in part, the result of the patient’s perceptions of the attributes of different treatments. Attributes in this context refer to the suitability, appropriateness, effectiveness, and convenience of a treatment.11,23 Eliciting attribute ratings prior to assessing treatment preference allows the patient to make an informed decision about his preference.11,18,24 Patients will typically rate the attributes of the preferred treatment higher than those of the non-preferred treatment.23,24
Assessing treatment preference and attributes provides benefits for both the clinician and patient. Knowing the patient’s attribute ratings for each treatment option may help the clinician tailor the treatment plan. For example, if the patient rates the convenience of a treatment low, the clinician can implement strategies to enhance convenience. The potential result is improved adherence and outcomes.17,25 Furthermore, the process allows for a collaborative discussion between the clinician and patient about treatment options.11,23,25 This could positively affect outcomes, especially if treatment involves lifestyle changes.10,26 By assessing treatment preference and attributes prior to initiating treatment, the clinician gains insight into factors that may affect the patient’s participation. Identifying and addressing these factors early on permits the clinician to limit the negative effect these factors could have on adherence and outcomes.
To our knowledge, no studies have assessed treatment preference and attributes of exercise-based treatments for chronic LBP. Our purpose was to assess the treatment preference and attributes of two exercise-based treatments for people with chronic LBP. Additionally, we wanted to determine if there were differences in characteristics between the participants who preferred each treatment. We hypothesized that (1) a majority of participants would have a preference, (2) there would be no differences in the percentage or characteristics of those who preferred each treatment, and (3) if participants reported a treatment preference, the attributes of the preferred treatment would be rated higher than those of the non-preferred treatment.
METHODS
Participants
A total of 154 participants were recruited from December 2013 to August 2016 from the St. Louis metropolitan area as part of a prospective, randomized clinical trial comparing two physical therapy (PT) exercise-based treatments for chronic LBP (ClinicalTrials.gov Identifier: NCT02027623). Chronic LBP was defined as having LBP symptoms greater than half the days of the year.27 Additional inclusion criteria were (1) aged 18–60 years, (2) body mass index ≤ 30 kg/m2, (3) not in an acute flare-up,27 (4) a modified Oswestry Low Back Pain Disability Questionnaire (mODQ) score of ≥ 20%,28 and (5) self-reported limitations in 3 or more functional activities or a history of treatment for LBP. Participants were excluded if they reported a history of (1) serious spinal complications (e.g., tumor), (2) spinal surgery, (3) neurological disease requiring hospitalization, (4) specific LBP diagnosis (e.g., spinal stenosis), (5) current treatment for cancer or unresolved cancer, (6) chronic inflammatory or auto-immune diseases (e.g., Systemic Lupus Erythematosus), or (7) currently receiving workers’ compensation, disability benefits, or involved in litigation for LBP. A power analysis was conducted for the clinical trial to detect a minimally clinically important difference of 6 points on the mODQ,28 the primary outcome variable. The power analysis was performed using SAS version 9.3.a Assuming a significance level of .05 (two-tailed), power of .80, and a dropout rate of 20%,29 154 participants were required for the primary study. The Washington University Institutional Review Board provided approval, and all participants provided written informed consent prior to participation.
Procedures
Prior to randomization into one of two treatments, participants completed self-report measures of (1) demographics, (2) LBP and medical history, (3) a numerical rating scale (NRS),30 and (4) the mODQ. Participants then underwent a standardized clinical examination by a trained physical therapist. Participants then completed additional selfreport measures assessing previous LBP-related treatment, medication use, acute flareups,27 recurrences,31 fear avoidance behavior,32 absenteeism,33,34 presenteeism,35 and health status.36,37 Finally, participants completed a treatment preference assessment (TPA) measure.
Measures
Treatment Preference Assessment Measure
Assessment of treatment preference followed the method described by Sidani and colleagues.11 The TPA was modified for the PT-specific treatments provided in the clinical trial based on a validated preference measure.11 Aspects of validity that have been examined include internal consistency and construct validity.11,24 The TPA consists of written descriptions of each of the two PT treatments. Each description includes an explanation of the treatment, the expected schedule, and potential benefits and risks of the treatment. Appendix A includes the treatment descriptions provided to the participant. The participant rates each treatment on (1) effectiveness, (2) acceptability/logicality, (3) suitability/appropriateness, and (4) convenience. Effectiveness is how successful the participant perceives the treatment will be in improving his condition. Acceptability/logicality refers to how reasonable and valid the participant views the treatment. Suitability/appropriateness indicates how much the participant perceives the treatment to be the correct treatment for his condition. Convenience refers to the participant’s perception of how easy it will be to participate in the treatment. Responses for each question are rated on a 5-point Likert scale. The anchors are not at all (rating = 1) and very much (rating = 5; table 1). Higher scores indicate that the participant views the treatment as effective, acceptable/logical, suitable/appropriate, and convenient. An overall score for each treatment option is calculated as the mean of the four attribute ratings.
Table 1.
Questions and rating scale for the four attributes of the TPA measure
| Question | Score |
||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| How effective do you think this treatment will be in improving your low back pain? | Not effective at all | Some what effective | Effective | Very effective | Very much effective |
| How acceptable/logical does this treatment seem to you? | Not acceptable at all | Somewhat acceptable | Acceptable | Very acceptable | Very much acceptable |
| How suitable/appropriate does this treatment seem to be to your low back pain? | Not suitable at all | Somewhat suitable | Suitable | Very suitable | Very much suitable |
| How convenient is this treatment? | Not convenient at all | Somewhat convenient | Convenient | Very convenient | Very much convenient |
Two different treatments (appendix A) were presented randomly to the participant. The strength and flexibility (SF) description informed the participant that he would complete exercises to increase trunk strength and trunk and lower limb flexibility. The motor skill training (MST) description informed the participant that he would perform challenging practice of daily activities that were limited due to his LBP. The descriptions indicated that both treatments would be prescribed and progressed on an individual basis by a trained, licensed physical therapist. Both treatments would consist of six one-hour visits, weekly, for six weeks.
Data Collection
Data were collected and managed using Research Electronic Data Capture (REDCap)38 tools hosted in the Biostatistics Division of Washington University School of Medicine. REDCap is a secure, web-based application which supports data capture for research studies.
For each treatment, the participant viewed the description on a computer screen while the coordinator read the description. The participant was then asked to answer four questions related to the specific treatment description. The four questions assessed the participant’s rating of each attribute (table 1). Once answered, the process was repeated for the other treatment. Finally, the participant indicated if he had a treatment preference, and, if so, which treatment he preferred. Treatment preference was collected as a baseline characteristic and did not affect the participant’s randomization to treatment.
Data Analysis
The sample was divided into those who did not report a treatment preference, those who preferred SF, and those who preferred MST. Demographics and baseline characteristics were compared between the SF and MST preference groups using two-sample t-tests and contingency tables with Pearson’s chi-square test and Fisher’s exact test as needed. To evaluate the overall score and each of the four attribute ratings, data were organized to allow a unified analysis with mixed random effects analysis of variance with preference group and treatment as fixed effects and subject within preference group as a random effect. We adjusted for the variables that were significantly different, or close to significantly different, between the two preference groups (table 2). The analyses were adjusted for duration of LBP and the work subscale score of the Fear-Avoidance Beliefs Questionnaire. Post-hoc effect sizes were calculated for each attribute rating within and between treatment preference groups using G*Power 3.1.9.2.39 Effect sizes of 0.2 were considered small, 0.5 were considered medium, and 0.8 were considered large.40 All statistical analyses were performed using SAS version 9.4a with significance levels set at p ≤ .05.
Table 2.
Participant characteristics for the SF preference group and the MST preference group
| Characteristic | SF preference group (n=95) | MST preference group (n=9) | p-value |
|---|---|---|---|
| Sex (female) | 52 (54.7) | 5 (55.6) | 1.00 |
| Age (y) | 41.4 ± 11.7 | 38.0 ± 9.7 | .40 |
| Duration of LBP (y) | 11.5 ± 9.0 | 5.0 ± 3.2 | < .01 |
| NRS pain intensity* | |||
| Current | 4.0 ± 1.6 | 4.3 ± 2.0 | .53 |
| Average (7 day) | 4.5 ± 1.6 | 5.0 ± 1.2 | .38 |
| Worst (7 day) | 6.4 ± 1.8 | 6.9 ± 1.5 | .43 |
| mODQ (%)† | 32.1 ± 9.9 | 33.6 ± 8.8 | .68 |
| Medication use (# reporting yes)‡ | 60 (63.2) | 5 (55.6) | .45 |
| FABQ Physical Activity scale§ | 13.8 ± 5.6 | 15.0 ± 6.3 | .55 |
| FABQ Work scale‖ | 10.9 ± 8.5 | 16.7 ± 9.9 | .06 |
| Absenteeism (days)¶ | 3.1 ± 4.5 | 2.4 ± 3.7 | .69 |
| Stanford Presenteeism Scale | |||
| Work Output Score (%)† | 85.5 ± 17.2 | 79.4 ± 27.7 | .54 |
| Work Absenteeism Score (hours)# | 5.5 ± 13.7 | 2.4 ± 3.0 | .10 |
| Work Impairment Score** | 20.3 ± 5.9 | 22.3 ± 7.3 | .35 |
| SF-36 Physical Component Score†† | 42.2 ± 7.0 | 38.5 ± 8.3 | .14 |
| SF-36 Mental Component Score†† | 49.2 ± 10.9 | 52.2 ± 8.0 | .42 |
NOTE. Values are mean ± SD or n (%).
Abbreviations: y, years; FABQ, Fear Avoidance Beliefs Questionnaire.
Scores range from 0–10, with 0 being no symptoms and 10 being symptoms as bad as can be.
Scores range from 0–100%.
Includes non-prescription and prescription medication.
Scores range from 0–24.
Scores range from 0–42.
Scores range from 0–28 days.
Scores range from 0–160 hours.
Scores range from 10–50.
Scores range from 0–100.
RESULTS
Participant Characteristics
The sample included 154 participants (average age: 42.6 ± 11.7 years, 61.7% female). Participants had an average duration of LBP of 10.3 ± 8.6 years, an average pain rating over the past week of 4.7 ± 1.7, and mODQ score of 32.6 ± 9.7%.
Preference Groups
Fifty participants (32.5%) reported no treatment preference. The focus of this study is on participants who reported a treatment preference; therefore, data on participants without a treatment preference is not presented.
Of the 104 participants (67.5%) who had a treatment preference, 95 (91.3%) preferred SF and nine (8.7%) preferred MST. Participant characteristics are summarized in table 2. The SF preference group had a longer duration of LBP (p < .01, d = .96); otherwise, there were no differences between the groups on baseline characteristics (all ps > .05).
Treatment Preference Assessment Analysis
Within Preference Group
SF Preference Group.
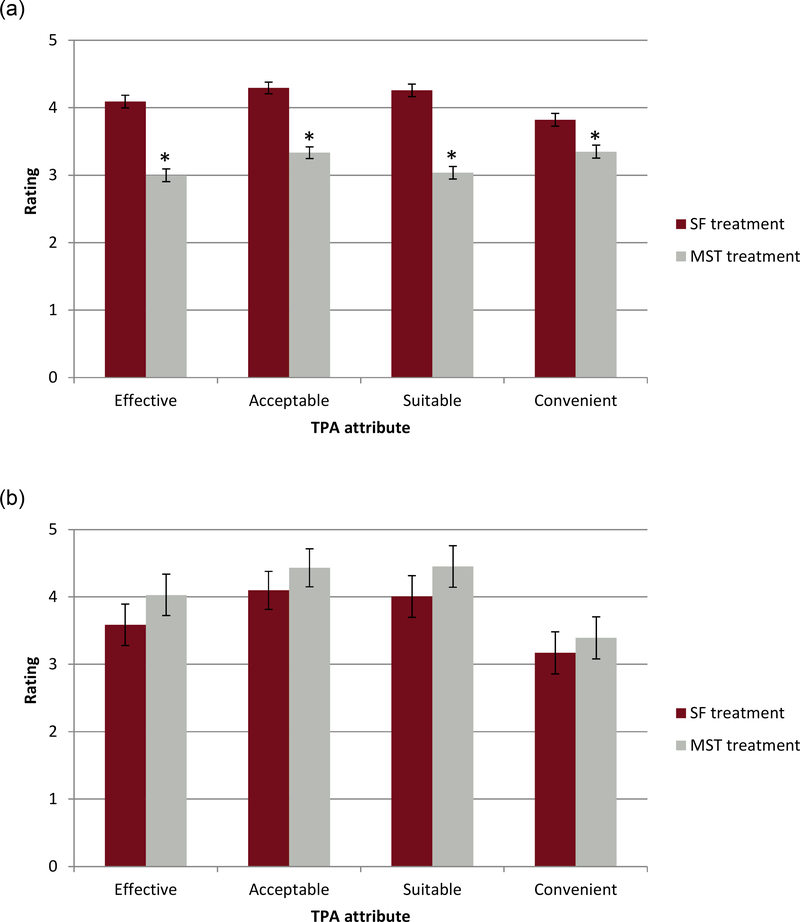
The SF preference group rated SF higher than MST overall (SF: 3.11 ± 0.08, MST: 2.18 ± 0.08, p < .01, d = 1.07). The SF preference group also rated each of the four SF attributes higher than the MST attributes (all ps < .01; effectiveness: d = 1.02, acceptability/logicality: d = 0.95, suitability/appropriateness: d = 0.99, convenience: d = 0.48; figure 1a).
Figure 1.
Attribute ratings for the (a) SF preference group, and (b) MST preference group
*indicates a significant difference (p ≤ .05)
MST Preference Group.
The MST preference group did not differ in the overall score of the two treatments (SF: 2.72 ± 0.26, MST: 3.08 ± 0.26, p = .14, d = .63), nor did they rate any of the attributes of the two treatments differently (all ps > .05, effectiveness: d = 0.43, acceptability/logicality: d = 0.66, suitability/appropriateness: d = 0.61, convenience: d = 0.51; figure 1b).
Between Preference Groups
Overall score.
The two preference groups did not differ in the overall score for SF (SF preference group rating: 3.11 ± 0.08, MST preference group rating: 2.72 ± 0.26, p = .14, d = .67). The SF preference group rated MST lower than the MST preference group (SF preference group rating: 2.18 ± 0.08, MST preference group rating: 3.08 ± 0.26, p < .01, d = 1.18).
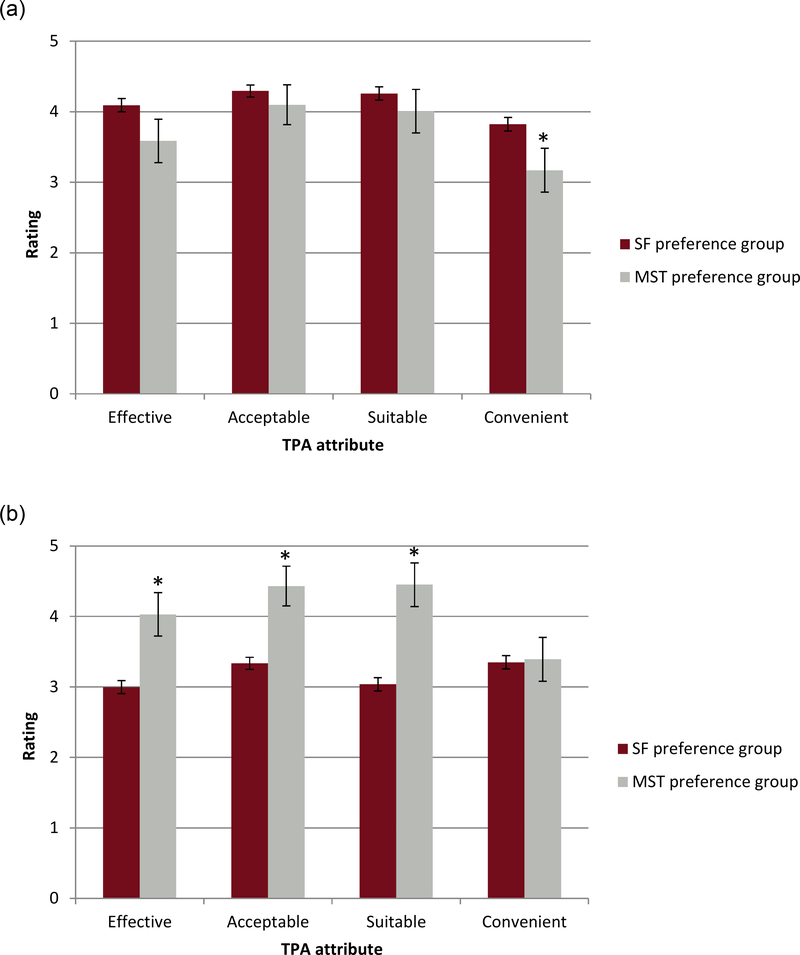
SF attributes (figure 2a).
Figure 2.
Attribute ratings between the two preference groups for the (a) SF attributes and (b) MST attributes
*indicates a significant difference (p ≤ .05)
The SF preference group rated the convenience of SF higher than the MST preference group (SF: 3.82 ± 0.10, MST: 3.17 ± 0.31, p = .05, d = .79). The two preference groups did not rate SF differently on the other three attributes (all ps > .05, effectiveness: d = 0.74, acceptability/logicality: d = 0.28, suitability/appropriateness: d = 0.33).
MST attributes (figure 2b).
The SF preference group rated three of the MST attributes (effectiveness, acceptability/logicality, and suitability/appropriateness) lower than the MST preference group (all ps < .01, effectiveness: d = 1.20, acceptability/logicality: d = 1.27, suitability/appropriateness: d = 1.52). The SF and MST preference groups did not rate the convenience of MST differently (SF: 3.35 ± 0.09, MS: 3.39 ± 0.31, p = .89, d = .04).
DISCUSSION
The purpose of this study was to assess treatment preference and attributes of two exercise-based treatments for people with chronic LBP. We hypothesized that most participants would report a treatment preference, the number of participants who preferred each treatment would not be different, nor would there be differences between the preference groups on any participant characteristics. Consistent with our hypothesis, a majority of participants reported a preference for treatment. However, there were differences in the number who preferred each treatment and the characteristics of the two preference groups. The majority of participants preferred SF to MST. Additionally, the participants who preferred SF reported a longer duration of LBP. We also hypothesized that the attributes of the preferred treatment would be rated higher than the attributes of the non-preferred treatment. Consistent with our hypothesis, the SF preference group rated all attributes of SF higher than the attributes of MST. The MST preference group, however, did not rate the attributes of the two treatments differently.
Contrary to our hypothesis, most of the participants in our study preferred SF to MST, even though both treatments were described similarly. One possible explanation for most participants preferring SF is that SF may be viewed as a more typical PT treatment for LBP41,42 and, therefore, may be more familiar to participants. A participant who has had experience with, or is more familiar with, a specific treatment is more likely to express a preference for that treatment.13,17 Additionally, the participants in the SF preference group reported a longer duration of LBP, which may have resulted in receiving more PT treatment for their LBP. Given that strength and flexibility exercises are commonly prescribed as part of PT,7,8,20 these participants may have had increased exposure to SF, which could have affected their preference. The concept of movement control during performance of daily activities (which is the focus of MST) is less widely prescribed,7,20,22,43 and therefore participants may have had less experience with this type of treatment.
Our hypotheses were based on research that participants who report a preference for a particular treatment rate the attributes of the preferred treatment higher than the non-preferred treatment.11,23 As hypothesized, those who preferred SF in our study rated all of the attributes of SF higher than the attributes of MST. Those who preferred MST, however, did not rate the attributes of the two treatments differently. The lack of difference in the attribute ratings by the MST preference group may be due to another attribute potentially contributing to their treatment preference. Sidani et al23 reported that participants have personal beliefs about a clinical condition, such as misconceptions about the cause of the condition or perception of a lack of control of the condition, which are related to their treatment preference. It is possible that the participants in the MST preference group held some beliefs about LBP that influenced their treatment preference other than the attributes we assessed.
Although other attributes may contribute to treatment preference, the attributes assessed in the current study provide the clinician with information about many factors that may influence preference. The clinician can use this information to initiate a collaborative discussion about treatments the clinician would like to incorporate into the treatment plan. In the current study, a majority of participants preferred SF. Therefore, if SF is indicated, the clinician may not need to discuss the advantages and disadvantages of SF. If the clinician, however, thinks that MST is indicated and the patient does not prefer MST, adherence and outcomes could be affected. The clinician should examine the attributes the patient rates unfavorably and discuss those attributes with the patient to enhance adherence and improve outcomes.
The patient’s attribute ratings for a specific treatment can guide the clinician as to which attributes to address when discussing that treatment with the patient. For example, within the SF preference group, the convenience of MST was rated lower than the convenience of SF. This lower rating indicates the participants thought it would be more difficult to participate in MST. Research has shown that patients want a treatment that is easy to implement in their daily lives.44–46 Thus, if MST is a treatment thought to be beneficial, the clinician can highlight that MST can be practiced during the activities the patient already performs throughout the day. Consequently, the patient does not have to take extra time to perform specific exercises. Given that exercise is not adhered to in the long-term,6,10,45 educating the patient that MST may be more convenient than SF may lead to increased adherence over time.
Study Limitations
There are limitations to this study. First, the attributes were not operationally defined for the participants. Thus, participants may have had different interpretations of the attributes. Second, treatment preference may have been influenced by our method of assessing the attributes prior to assessing treatment preference. Asking about treatment preference first may provide a more unbiased assessment of preference. Third, there is a minimal amount of literature documenting the psychometric properties of the TPA. Fourth, we only assessed two exercise-based treatments for participants with chronic LBP. Consequently, we cannot generalize our results to other treatments for chronic LBP or to treatments for acute or sub-acute LBP. Finally, we do not know how presenting more than two treatment options would affect treatment preference and attribute ratings.
CONCLUSIONS
A majority of participants had a preference for treatment, and the majority preferred SF to MST. Convenience appears to be an important attribute to consider, particularly when prescribing MST. The data suggest that the clinician should consider treatment preference when prescribing a treatment plan. Assessing treatment preference and attributes prior to treatment initiation allows the clinician to identify factors that could impact adherence to treatment. Identifying and addressing these factors early on could limit the potential negative effects on outcomes.
Supplementary Material
Acknowledgements:
The authors thank Sara Putnam, MS for her assistance with study design and the members of the Musculoskeletal Analysis Group for their assistance with recruitment and data collection, processing, and analysis. The authors wish to acknowledge the support of the I2 WUSM ICS, Siteman Comprehensive Cancer Center, and NCI Cancer Center Support Grant P30 CA091842 for supporting the REDCap clinical data capture service as a research resource at WUSM.
FUNDING: The study was supported by the NIH/NICHD/NCMRR [grant number R01 HD047709], the Foundation for Physical Therapy Promotion of Doctoral Studies Scholarship, the Dr. Hans and Clara Davis Zimmerman Foundation Health Scholarship, the Clinical and Translational Science Award Grant [grant number UL1 TR000448], and the Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant [grant number P30 CA091842].
Financial Support: The study was supported by the NIH/NICHD/NCMRR [grant number R01 HD047709], the Foundation for Physical Therapy Promotion of Doctoral Studies Scholarship, the Dr. Hans and Clara Davis Zimmerman Foundation Health Scholarship, the Clinical and Translational Science Award Grant grant number UL1 TR000448], and the Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant [grant number P30 CA091842]. We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
List of Abbreviations:
- LBP
low back pain
- mODQ
modified Oswestry Low Back Pain Disability Questionnaire
- MST
motor skill training
- NRS
numerical rating scale
- REDCap
Research Electronic Data Capture
- SF
strength and flexibility
- TPA
treatment preference assessment
Footnotes
Presentation: This material was presented in abstract form at the Combined Sections Meeting of the American Physical Therapy Association in Anaheim, CA (February, 2016).
SUPPLIERS
aSAS Institute Inc., 100 SAS Campus Drive, Cary, NC, 27513
Clinical Trial Registration: The primary trial from which this data was taken was registered on ClinicalTrials.gov (NCT02027623).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318:291–300. 10.1056/NEJM198802043180506 [DOI] [PubMed] [Google Scholar]
- 2.Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379:482–91. 10.1016/S0140-6736(11)60610-7 [DOI] [PubMed] [Google Scholar]
- 3.Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. BMJ. 1998;316:1356–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005:CD000335 10.1002/14651858.CD000335.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol. 2010;24:193–204. 10.1016/j.berh.2010.01.002 [DOI] [PubMed] [Google Scholar]
- 6.Van Dillen LR, Norton BJ, Sahrmann SA, Evanoff BA, Harris-Hayes M, Holtzman GW, Earley J, Chou I, Strube MJ. Efficacy of classification-specific treatment and adherence on outcomes in people with chronic low back pain. A one-year follow-up, prospective, randomized, controlled clinical trial. Man Ther. 2016;24:52–64. 10.1016/j.math.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776–85. [DOI] [PubMed] [Google Scholar]
- 8.Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: what works? Pain. 2004;107:176–90. [DOI] [PubMed] [Google Scholar]
- 9.Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010:CD005956 10.1002/14651858.CD005956.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–99. [PMC free article] [PubMed] [Google Scholar]
- 11.Sidani S, Epstein DR, Bootzin RR, Moritz P, Miranda J. Assessment of preferences for treatment: validation of a measure. Res Nurs Health. 2009;32:419–31. 10.1002/nur.20329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowling A, Ebrahim S. Measuring patients’ preferences for treatment and perceptions of risk. Qual Health Care. 2001;10:i2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Preference Collaborative Review Group. Patients’ preferences within randomised trials: systematic review and patient level meta-analysis. BMJ. 2008;337:a1864 10.1136/bmj.a1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherman KJ, Cherkin DC, Ichikawa L, Avins AL, Delaney K, Barlow WE, Khalsa PS, Deyo RA. Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine (Phila Pa 1976). 2010;35:1471–7. 10.1097/BRS.0b013e3181c2a8d3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.George SZ, Robinson ME. Preference, expectation, and satisfaction in a clinical trial of behavioral interventions for acute and sub-acute low back pain. J Pain. 2010;11:1074–82. 10.1016/j.jpain.2010.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bowling A, Rowe G. “You decide doctor”. What do patient preference arms in clinical trials really mean? J Epidemiol Community Health. 2005;59:914–5. 10.1136/jech.2005.035261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sidani S, Miranda J, Epstein D, Fox M. Influence of treatment preferences on validity: a review. Can J Nurs Res. 2009;41:52–67. [PubMed] [Google Scholar]
- 18.Sidani S, Fox M, Streiner DL, Miranda J, Fredericks S, Epstein DR. Examining the influence of treatment preferences on attrition, adherence and outcomes: a protocol for a two-stage partially randomized trial. BMC Nurs. 2015;14:57 10.1186/s12912-015-0108-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aboagye E Valuing individuals’ preferences and health choices of physical exercise. Pain Ther. 2017;6:85–91. 10.1007/s40122-017-0067-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765–75. [DOI] [PubMed] [Google Scholar]
- 21.Delitto A, George SZ, Van Dillen LR, Whitman JM, Sowa G, Shekelle P, Denninger TR, Godges JJ. Low back pain. J Orthop Sports Phys Ther. 2012;42:A1–57. 10.2519/jospt.2012.0301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saragiotto BT, Maher CG, Yamato TP, Costa LO, Costa LC, Ostelo RW, Macedo LG. Motor control exercise for nonspecific low back pain: A Cochrane review. Spine (Phila Pa 1976). 2016;41:1284–95. 10.1097/BRS.0000000000001645 [DOI] [PubMed] [Google Scholar]
- 23.Sidani S, Miranda J, Epstein DR, Bootzin RR, Cousins J, Moritz P. Relationships between personal beliefs and treatment acceptability, and preferences for behavioral treatments. Behav Res Ther. 2009;47:823–9. 10.1016/j.brat.2009.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sidani S, Epstein DR, Fox M, Miranda J. Psychometric properties of the Treatment Perception and Preferences measure [published online ahead of print June 13 2016]. Clin Nurs Res. 2016. 10.1177/1054773816654137 [DOI] [PubMed] [Google Scholar]
- 25.Sidani S, Epstein D, Miranda J. Eliciting patient treatment preferences: A strategy to integrate evidence-based and patient-centered care. Worldviews Evid Based Nurs. 2006;3:116–23. 10.1111/j.1741-6787.2006.00060.x [DOI] [PubMed] [Google Scholar]
- 26.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70:351–79. 10.1177/1077558712465774 [DOI] [PubMed] [Google Scholar]
- 27.Von Korff M Studying the natural history of back pain. Spine (Phila Pa 1976). 1994;19:2041S–46S. [DOI] [PubMed] [Google Scholar]
- 28.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–88. [DOI] [PubMed] [Google Scholar]
- 29.Friedman LM, Furberg C, DeMets DL. Fundamentals of Clinical Trials. 4th ed. New York: Springer; 2010. [Google Scholar]
- 30.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–92. [DOI] [PubMed] [Google Scholar]
- 31.Stanton TR, Latimer J, Maher CG, Hancock MJ. A modified Delphi approach to standardize low back pain recurrence terminology. Eur Spine J. 2011;20:744–52. 10.1007/s00586-010-1671-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–68. [DOI] [PubMed] [Google Scholar]
- 33.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–49. [DOI] [PubMed] [Google Scholar]
- 34.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine (Phila Pa 1976). 1995;20:1899–908. [DOI] [PubMed] [Google Scholar]
- 35.Turpin RS, Ozminkowski RJ, Sharda CE, Collins JJ, Berger ML, Billotti GM, Baase CM, Olson MJ, Nicholson S. Reliability and validity of the Stanford Presenteeism Scale. J Occup Environ Med. 2004;46:1123–33. [DOI] [PubMed] [Google Scholar]
- 36.Saris-Baglama RN, Dewey CJ, Chisholm GB, Kosinski M, Bjorner JB, Ware JE Jr. SF Health Outcomes Scoring Software User’s Guide. Lincoln, RI: QualityMetric Incorporated; 2004. [Google Scholar]
- 37.Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976). 2000;25:3130–9. [DOI] [PubMed] [Google Scholar]
- 38.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. [DOI] [PubMed] [Google Scholar]
- 40.Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 41.Bishop MD, Bialosky JE, Cleland JA. Patient expectations of benefit from common interventions for low back pain and effects on outcome: secondary analysis of a clinical trial of manual therapy interventions. J Man Manip Ther. 2011;19:20–5. 10.1179/106698110X12804993426929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.May S Patients’ attitudes and beliefs about back pain and its management after physiotherapy for low back pain. Physiother Res Int. 2007;12:126–35. 10.1002/pri.367 [DOI] [PubMed] [Google Scholar]
- 43.Costa LO, Maher CG, Latimer J, Hodges PW, Herbert RD, Refshauge KM, McAuley JH, Jennings MD. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther. 2009;89:1275–86. 10.2522/ptj.20090218 [DOI] [PubMed] [Google Scholar]
- 44.Dean SG, Smith JA, Payne S, Weinman J. Managing time: an interpretative phenomenological analysis of patients’ and physiotherapists’ perceptions of adherence to therapeutic exercise for low back pain. Disabil Rehabil. 2005;27:625–36. 10.1080/0963820500030449 [DOI] [PubMed] [Google Scholar]
- 45.Campbell R, Evans M, Tucker M, Quilty B, Dieppe P, Donovan JL. Why don’t patients do their exercises? Understanding non-compliance with physiotherapy in patients with osteoarthritis of the knee. J Epidemiol Community Health. 2001;55:132–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Slade SC, Patel S, Underwood M, Keating JL. What are patient beliefs and perceptions about exercise for nonspecific chronic low back pain? A systematic review of qualitative studies. Clin J Pain. 2014;30:995–1005. 10.1097/AJP.0000000000000044 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.