Abstract
Aim
Empathy is a crucial component of the nurse–patient relationship, but knowledge is lacking as to when empathy develops during nursing education. The aim of the present study was to compare empathy levels at different stages of undergraduate nursing education and different master's nursing programmes.
Design
The design was a comparative cross‐sectional study.
Methods
A total of 329 participants in Sweden, comprised of nursing students in their second and sixth semesters in an undergraduate nursing programme as well as master's nursing students, rated their own empathy using the Jefferson Scale of Physician Empathy.
Results
Students in their sixth semester in an undergraduate nursing programme expressed more empathy than did students in their second semester and master's nursing students. Among the five master's programmes, public‐health nursing students expressed the most empathy and intensive‐care nursing students the least.
Keywords: empathy, Jefferson Scale of Physician Empathy, nursing education, nursing student, patient–nurse relationship
1. INTRODUCTION
1.1. Empathy
Located on the borders between self and other, cognition and emotion, science and practice, empathy is a core phenomenon in all human interactions, a crucial component of the nurse–patient relationship (Cunico, Sartori, Marognolli, & Meneghini, 2012) that has been shown to improve patient satisfaction (Derksen, Bensing, & Lagro‐Janssen, 2013). Still, patients perceive that empathy is frequently lacking in the nurse–patient relationship (Williams & Stickley, 2010). However, empathy is something that can be taught (Cunico et al., 2012). For example, one study showed that nursing students’ empathy increased after practice encounters with professional actors playing roles as patients and relatives (Soderberg, Sundbaum, & Engstrom, 2017).
American psychologist and therapist Carl Rogers introduced a new perspective on personality change and therapy, of which empathy was a core component (Rogers, 1957,1975). In fact, much of the popularity of empathy within today's psychology and nursing science can, in some way, be traced back to Rogers. Although researchers today agree on the importance of empathy, diverse opinions exist concerning whether and to what extent, for example, emotion, cognition, motivation, identification and self‐other differentiation should be part of its definition. For instance, Batson, Eklund, Chermok, Hoyt, and Ortiz (2007) define empathy in purely emotional terms, as an other‐oriented emotional response elicited by and congruent with the perceived welfare of a person in need. Along with Hojat et al. (2002) who developed the Jefferson Scale of Physician Empathy, we define empathy in patient‐care situations as an attribute involving an ability to understand each patient's inner experiences and perspectives, and the capability to communicate this understanding. This definition of empathy entails the ability to understand, rather than feel, combined with the capability to communicate this understanding (Hojat, 2007).
1.2. Empathy in medicine and nursing
Empathy is a central aspect of the patient–nurse relationship (Derksen et al., 2017; Haslam, 2007; Richardson, Macleod, & Kent, 2012; Ward et al., 2009). Also, a brief encounter between a patient and an empathic nurse can be beneficial for the patient (Halpern, 2001); that is, empathy can strengthen the relationship between nurse and patient, making the treatment work more efficiently (Haslam, 2007). In a study, Derksen et al. (2017) found that empathy makes patients more relaxed, motivated and willing to cooperate. The patients in the study also revealed that a lack of empathy in health providers leaves them frustrated and unwilling to return to the healthcare facility.
The extant literature is mixed regarding whether empathy declines among medical and nursing students during their education. Ferri, Guerra, Marcheselli, Cunico, and Lorenzo (2015), as well as Nunes, Williams, Sa, and Stevenson (2011), found that empathy declined among students in healthcare professions throughout their education years. Hojat et al. (2009) using the Jefferson Scale of Physician Empathy measured empathy in medical students upon entry into medical school and at the end of each academic year. Empathy levels did not change during the first two years, but at the end of the third year a decline was noted in empathy among men and women, in both technology‐oriented specialties and people‐oriented fields. This decline persisted until graduation. In a longitudinal study using the Jefferson Scale of Physician Empathy, Ward, Cody, Schaal, and Hojat (2012) found a decline in empathy during one year of an undergraduate nursing programme. The decline was greatest among those students who had the most clinical encounters and among those with prior work experience in health care. However, in an intervention study using standardized actors during the last year of a nursing programme, Ward (2016) found that the typical decline in empathy could be hindered. In a review of studies using the Jefferson Scale of Physician Empathy‐student version, Roff (2015) found a lack of evidence of a decline in empathy over time among medical students.
Brunero, Lamont, and Coates (2010) reviewed the evidence for the effectiveness of empathy training in undergraduate and postgraduate nursing programmes. Seventeen qualitative and quantitative studies met their inclusion criteria, and eleven of these showed statistically significant improvements in empathy. Brunero et al. (2010) concluded that it is possible to improve nurses’ empathic tendencies and that the education types that used experiential learning styles were the most promising. Examples of experiential learning included role play and case‐scenario‐based experiential work.
Petrucci, La Cerra, Aloisio, Montanari, and Lancia (2016) conducted a cross‐sectional study at an Italian university on health professional students, using the Jefferson Scale of Physician Empathy. Undergraduate nursing students showed significantly higher levels of empathy than students of other healthcare professions. Another Italian study tested whether a specific training course would enhance empathy in nursing students during a three‐year degree course. The study showed that the training was effective, especially on women's empathy, which increased over three years (Cunico et al., 2012). Similarly, Lee, Yu, Hsieh, Li, and Chao (2018) noted an increase in empathy among nursing students as a result of a four‐month training programme that included role play, self‐reflection, situated learning and acting.
As empathy is crucial for nurse–patient encounters, and also for clinical outcomes, it should be a high priority in nursing education as well as in master's nursing programmes. In theories on nursing, empathy is of high importance, and the rapport with the patient is crucial in practicing high‐quality care. Whether empathy somehow increases or declines during nursing education is unclear, according to the aforementioned studies. Focusing on differences in empathy among undergraduate nursing students and among master's nursing students could provide indications of differences in these educational paths, which could be of interest to clinical practice and nurse‐education realms. To our knowledge, these kinds of studies are lacking in the extant literature.
2. OBJECTIVE
To compare empathy levels at different stages of undergraduate nursing education and different master's nursing programmes. Specifically, the research question was the following: Are there differences in subjective empathy levels in nursing students when comparing (a) the second semester of an undergraduate nursing programme, (b) the sixth semester of the programme, and (c) master's nursing students programmes (anaesthesia, intensive‐care nurse, midwifery, psychiatry, public health)?
3. METHODS
3.1. Design
The study was a quantitative, comparative study among undergraduate and master's‐level nursing students at a university in Sweden.
3.2. Participants and setting
A convenience sample of nursing students was drawn from undergraduates in the second and final (sixth) semesters of the undergraduate nursing programme and from five master's nursing programmes at a university in Sweden. The undergraduate nursing programme follows the regulations for nursing education established by the Swedish government. This three‐year programme comprises 180 credits in the European Credit Transfer System, resulting in a bachelor's degree. According to Sweden's higher‐education regulatory group, empathy is a skill that nursing students must possess. Specialized nursing programmes follow national guidelines, resulting in a master's degree.
During the second semester, 142 of 164 students, aged 21–67 years (M = 28.71, SD = 7.70), agreed to participate. Out of their ranks, 81.6% classified themselves as female, while the others did not provide gender information. In the sixth semester, 93 of 107 students, aged 24–56 years (M = 29.73, SD = 6.70), agreed to participate. Among them, 88.3% classified themselves as female and 1% as male, while the others did not provide gender information.
Among the master's nursing students, 94 of 98 agreed to participate. There were students in the sample from five master's programmes in nursing, ranging in duration from a year to a year and a half: anaesthesia [N = 16], intensive care [N = 16], midwifery [N = 26], psychiatry [N = 22] and public health [N = 14]. The master's nursing students ranged in age between 24–55 years (M = 33.96, SD = 7.58). Most (79.8%) classified themselves as female, and the others as male. The master's nursing students’ experience working as registered nurses ranged from 1–21 years (M = 5.55, SD = 4.62).
3.3. Data collection
Data were collected in classroom settings. In previous research, empathy has been measured in a variety of ways, ranging from more subjective (eg self‐ratings) to more objective methods (eg fMRI). Among the most commonly used self‐rating scales are Davis’ IRI (Davis, 1983), Batson's ERS, (Batson et al., 2007) and the Jefferson Scale of Physician Empathy (Hojat et al., 2001). For the present study, we selected the Jefferson Scale of Physician Empathy, since it is the most commonly used empathy scale in nursing. Developed at Jefferson Medical College, it is a 20‐item, self‐rating instrument in which each item is rated from 1 (strongly disagree)–7 (strongly agree). Since its creation, it has been translated into approximately 50 languages and applied to other areas, such as nursing. Several extant studies have provided support for its validity and reliability.
A questionnaire consisting of the Jefferson Scale of Physician Empathy (Hojat et al., 2001) and background questions (gender, age, education, etc.) was distributed. The Jefferson Scale of Physician Empathy consists of three dimensions: perspective taking, compassionate care and standing in the patient's shoes. In the Jefferson Scale of Physician Empathy for health providers, nurses’ understanding of the emotional status of their patients, as well as that of the patients’ families, is an important component of the nurse–patient relationship, as is the notion that nurses should try to stand in their patients’ shoes when providing care to them. Ten of the 20 items on the scale are negatively worded, thereby reversing the scoring. The sum score for the 20 items ranges from 20–140, with higher scores reflecting more empathy. The mean score for undergraduate nursing students in general is 114 (Ward et al., 2009). In a study of Norwegian and Swedish third‐year undergraduate nursing students using this scale, the mean score was 115 (Sundling, Sundler, Holmstrom, Kristensen, & Eide, 2017). Cronbach's alpha for the undergraduates in the present study was 0.80, and for the master's nursing students, it was 0.74. No compensation for participation was offered.
3.4. Data analysis
Data were analysed using SPSS (Statistical Package for the Social Sciences) version 24 (SPSS Inc., Chicago, IL, USA). One‐way and two‐way ANOVAs were conducted with the significance level p < 0.05 and were then followed up with post hoc tests (Bonferroni). There were too few men in the sample to conduct meaningful tests on gender effects, so we omitted gender as a factor and only reported results for the group as a whole. There was only a weak, insignificant correlation between age and empathy; therefore, we have not included age as a covariate in the ANOVAs.
3.5. Ethical considerations
The university's local institutional ethical board and the students’ union approved the study, which follows the ethical standards for research and conforms with the Declaration of Helsinki (World Medical Association, 2008) and with ethical regulations and guidelines according to Swedish law (Sweden, Ministry of Education and Research, 2003). Participants were given oral and written information about the research, their participation and their rights as participants, as well as how the data would be handled, stored and presented/published. All participants had to provide written and informed consent to participate. They were also made aware of their right to withdraw their participation at any time. All participants were anonymous.
4. RESULTS
The data were subjected to a two‐way ANOVA based on healthcare work experience prior to entering the programme (worked in health care/not worked in health care) and education level (second semester, sixth semester, master's student) as between‐subjects factors and empathy as dependent variable. There was a significant main effect of previous work experience: F (1, 327) = 4.46, p < 0.05, η 2 = 0.014 (see Table 1). There was also a significant main effect of previous education level: F (2, 327) = 8.01, p < 0.001, η 2 = 0.047. A post hoc test (Bonferroni) revealed that the students in their sixth semester (M = 117.29, SD = 11.32) expressed more empathy than those in their second semester (M = 111.58, SD = 11.37) (p < 0.001) and the master's nursing students (M = 111.62, SD = 0.57) (p = 0.005). However, no reliable differences were detected between the students in their second semester and the master's nursing students (see Table 1 and Figure 1). There was no interaction effect of previous work experience and education level.
Table 1.
Subjective empathy levels (and SD) at the second semester, sixth semester and master's programmes for students with and without healthcare working experience prior to entering the undergraduate nursing programme
| Second semester | Sixth semester | Master's programme | Total | |
|---|---|---|---|---|
| Work experience | 114.2 (12.3) | 117.8 (11.5) | 112.5 (11.0) | 114.7 (11.8) |
| No work experience | 109.2 (11.2) | 116.7 (11.2) | 110.3 (12.2) | 111.6 (11.8) |
| Total | 111.6 (12.0) | 117.3 (11.3) | 111.6 (11.4) | 113.2 (11.9) |
Figure 1.
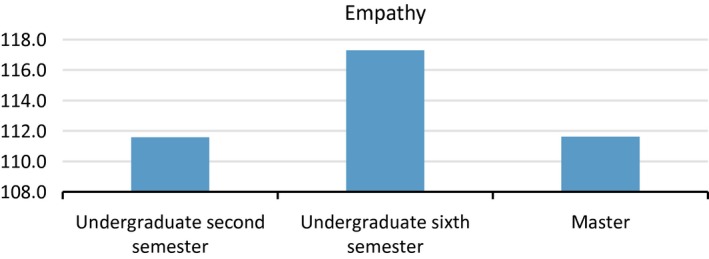
Subjective empathy levels for the second semester, sixth semester and master's programmes
The data were subjected to a one‐way ANOVA with type of master's programme (anaesthesia, intensive‐care nurse, midwifery, psychiatry, public health) as a between‐subjects factor and empathy as a dependent variable. There was a significant main effect: F (4, 89) = 2.82, p < 0.05, η 2 = 0.11. A post hoc test (Bonferroni) revealed that public‐health nursing students (M = 117.07 SD = 5.81) expressed significantly more empathy than did intensive‐care students (M = 105.38, SD = 10.50) (p < 0.05). There were no other significant differences among the master's programmes (See Figure 2).
Figure 2.
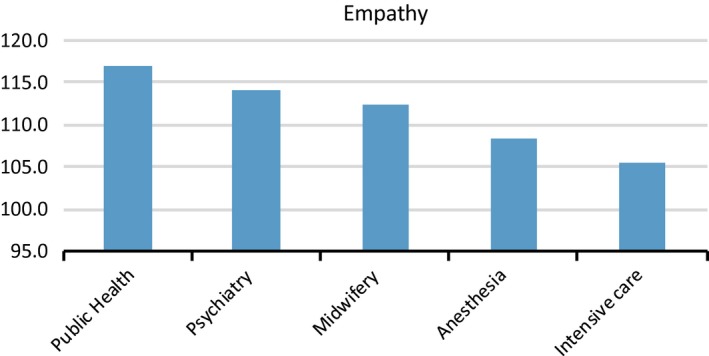
Subjective empathy levels among master's nursing students (anaesthesia, public health, intensive‐care nurse, midwifery, psychiatry)
5. DISCUSSION
In the present study, students in their sixth semester expressed more empathy than did those in their second semester and master's students. The mean score for the second and the sixth semesters combined is near the mean scores found in previous studies of undergraduate nursing students (Ward et al., 2009). Among the five one‐year master's programmes, public‐health nursing students expressed the most empathy, followed by psychiatry, midwifery, anaesthesia and intensive‐care students.
There was also an effect on empathy of healthcare work experience prior to entering the undergraduate nursing programme. Students who had such work experience expressed more empathy than those who did not. The difference was greatest among the students in the second semester, which suggests that the undergraduate nursing programme can reduce differences by increasing non‐work‐experienced students’ empathy more than work‐experienced students’ empathy. While there seems to be a lack of research regarding the effects of previous work experience on nursing students’ empathy, there is research on empathy in general that supports the idea that previous experience can increase empathy. For example, Eklund, Andersson‐Straberg, and Hansen (2009) found that participants with prior experience of grief or fear had more empathy for a person experiencing grief or fear than did participants without such experience. Hodges, Kiel, Kramer, Veach, and Villanueva (2010) found that having had a similar experience had an effect on empathic concern, empathic accuracy and the target's perceived empathy.
The finding that students in their sixth semester expressed more empathy than did those in their second semester was expected. As mentioned, one can imagine that studying nursing would increase empathy. While the students in our study did not receive any explicit empathy training in their education, empathy is implicitly a major part of their training, which could explain the higher empathy scores. Increased empathy also has been found among nursing students in programmes that explicitly include empathy training (Cunico et al., 2012; Lee et al., 2018). Conversely, Ward et al. (2012) found that empathy declined over the course of one year of an undergraduate nursing programme among those who had more contact with patients than others. However, a later study by Ward (2016) in which role play was part of empathy training for nursing students showed that the usual decline in empathy did not occur. Role play seems to be effective for empathy, as increased empathy was also found in studies by Soderberg et al. (2017) and Lee et al. (2018) in which role play was part of empathy training. Soderberg et al. (2017) suggested that role play might create empathy in nursing students because it involves eye contact and seeing the other's reactions when trying different things in encounters. This indicates that a successful part of empathy training might involve practicing with real encounters – “human human‐to‐human” practice such as in role play. If role play with an explicit focus on empathy were to be included in the programmes, empathy levels might increase.
In the present study, the one‐year master's students expressed less empathy than did the undergraduate students in their sixth semester. One possible explanation for this is the fact that while the students in their sixth semester had spent the previous three years in an educational setting where empathy played a substantial part, the one‐year master's students had only recently returned to this kind of setting after having worked as nurses in clinical settings. In the undergraduate programme, reflective discussions are a crucial part of education related to caring, while such activities might not be prioritized to the same degree in clinical settings. Bas‐Sarmiento, Fernandez‐Gutierrez, Baena‐Banos, and Romero‐Sanchez (2017) and Percy and Richardson (2018) specifically point to reflective discussions as a means of increasing nursing students’ empathy, which might suggest a need for continuous educational activities, including reflective discussions, during clinical work as well. It is also possible that the master's nursing students, during their work as nurses, experienced stress, limited resources, compassion fatigue, and an inability to provide care on the level they wished. In previous studies, it was found that nurses encounter several stressful situations in their work (Purcell, Kutash, & Cobb, 2011) and are at risk of compassion fatigue (Duarte & Pinto‐Gouveia, 2017).
Our study also found that intensive‐care and anaesthesia students expressed lower levels of empathy than did public‐health nursing, midwifery and psychiatry students. However, we must be cautious when drawing conclusions from these differences, as the student groups from the five master's programmes were small. Still, one explanation for these differences might be the greater technical focus on intensive care and anaesthesia in these programmes than in the other three. Holm (1985) found that medical students’ empathy was lower during the more technical parts of their education, when they focused on body parts rather than on patients as sentient human beings. Similarly, in a study on empathy antecedents, Håkansson Eklund (2006) showed that a negative relationship exists between empathy and objectifying someone. At the same time, as for the anaesthesia and intensive‐care students, their future work will be partly technical in nature, but they will also have contact with severely ill patients, for whom empathy is most needed. Thus, empathy training should be a high priority in their education.
Empathy is an essential part of the nurse–patient relationship. However, the present study found lower levels of empathy among master's students, who had spent a period of time working as nurses in clinical settings, unlike the undergraduates. According to Crawford, Brown, Kvangarsnes, and Gilbert (2014) and Percy and Richardson (2018), mutual responsibility exists among educators and stakeholders in practical settings to cultivate and maintain nurses’ empathy levels. It is important to prepare nurses for how to treat patients with complex illnesses as well as their relatives, and to keep practicing the essence of nursing, in which empathy and compassion are crucial. Less‐empathic healthcare professionals not only lead to unsatisfied patients and relatives but also, according to Halpern, (Halpern, 2001) risk eliciting incorrect diagnoses, poor patient adherence to therapy, and decreased patient engagement. Rush and Cook (2006) have found that patients and their relatives highly value empathic attitudes among nurses. In their study, Haron and Tran (2014) found that what patients valued most was being respected as whole people rather than merely viewed and treated as illness cases, and receiving emotional support.
5.1. Limitations
The present study has some limitations that may influence interpretations of the results. One limitation is the use of self‐ratings only. It is well‐known that in empathy studies using self‐ratings, people tend to overrate their empathy due to such processes as social desirability. Other limitations include the relatively small sample of master's nursing students and men in the participant sample. In addition, the cross‐sectional design has obvious disadvantages when compared with the longitudinal design. The comparisons we made were between different groups of students, so there is a risk that the groups differ in respects that might have influenced the results. It would be interesting to conduct a longitudinal study, with the same student group measured at various points over time. Another limitation is that we conducted the study at only one university.
6. CONCLUSIONS
The present study's results suggest that nursing students’ empathic tendencies vary across stages of their education, as well as among different kinds of specializations on the master's level. These findings can offer teachers and others involved in the development of nursing programmes insights into students’ empathic tendencies at different stages of their nursing education. More generally, clinicians and other relevant decision makers in the sector, as well as nurse educators, need to take seriously the present study's finding that students seem to be less empathic after a period of time working as nurses than when they left school. This indicates a need for continuous reflection and educational activities as part of their clinical work as nurses in order to preserve empathic attitudes.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
JHE, LMH, IKH, AOL, AJS: Study design. JHE, AOL, JH: Study analysis. JHE, LMH, IKH, AOL, JH, AJS: Drafting of the article.
Håkansson Eklund J, Holmström IK, Ollén Lindqvist A, Sundler AJ, Hochwälder J, Marmstål Hammar L. Empathy levels among nursing students: A comparative cross‐sectional study. Nursing Open. 2019;6:983–989. 10.1002/nop2.280
Funding information
This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
REFERENCES
- Bas‐Sarmiento, P. , Fernandez‐Gutierrez, M. , Baena‐Banos, M. , & Romero‐Sanchez, J. M. (2017). Efficacy of empathy training in nursing students: A quasi‐experimental study. Nurse Education Today, 59, 59–65. 10.1016/j.nedt.2017.08.012 [DOI] [PubMed] [Google Scholar]
- Batson, C. D. , Eklund, J. H. , Chermok, V. L. , Hoyt, J. L. , & Ortiz, B. G. (2007). An additional antecedent of empathic concern: Valuing the welfare of the person in need. Journal of Personality and Social Psychology, 93(1), 65–74. 10.1037/0022-3514.93.1.65 [DOI] [PubMed] [Google Scholar]
- Brunero, S. , Lamont, S. , & Coates, M. (2010). A review of empathy education in nursing. Nursing Inquiry, 17(1), 65–74. 10.1111/j.1440-1800.2009.00482.x [DOI] [PubMed] [Google Scholar]
- Crawford, P. , Brown, B. , Kvangarsnes, M. , & Gilbert, P. (2014). The design of compassionate care. Journal of Clinical Nursing, 23(23–24), 3589–3599. 10.1111/jocn.12632 [DOI] [PubMed] [Google Scholar]
- Cunico, L. , Sartori, R. , Marognolli, O. , & Meneghini, A. M. (2012). Developing empathy in nursing students: A cohort longitudinal study. Journal of Clinical Nursing, 21(13–14), 2016–2025. 10.1111/j.1365-2702.2012.04105.x [DOI] [PubMed] [Google Scholar]
- Davis, M. H. (1983). Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology, 44(113–126). 10.1037/0022-3514.44.1.113 [DOI] [Google Scholar]
- Derksen, F. , Bensing, J. , & Lagro‐Janssen, A. (2013). Effectiveness of empathy in general practice: A systematic review. British Journal of General Practice, 63(606), e76–84. 10.3399/bjgp13X660814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derksen, F. , Olde Hartman, T. C. , van Dijk, A. , Plouvier, A. , Bensing, J. , & Lagro‐Janssen, A. (2017). Consequences of the presence and absence of empathy during consultations in primary care: A focus group study with patients. Patient Education and Counseling, 100(5), 987–993. 10.1016/j.pec.2016.12.003 [DOI] [PubMed] [Google Scholar]
- Duarte, J. , & Pinto‐Gouveia, J. (2017). The role of psychological factors in oncology nurses' burnout and compassion fatigue symptoms. European Journal of Oncology Nursing, 28, 114–121. 10.1016/j.ejon.2017.04.002 [DOI] [PubMed] [Google Scholar]
- Eklund, J. , Andersson‐Straberg, T. , & Hansen, E. M. (2009). "I've also experienced loss and fear": Effects of prior similar experience on empathy. Scandinavian Journal of Psychology, 50(1), 65–69. 10.1111/j.1467-9450.2008.00673.x [DOI] [PubMed] [Google Scholar]
- Ferri, P. , Guerra, E. , Marcheselli, L. , Cunico, L. , & Di Lorenzo, R. (2015). Empathy and burnout: An analytic cross‐sectional study among nurses and nursing students. Acta Biomedica, 86(Suppl 2), 104–115. [PubMed] [Google Scholar]
- Håkansson Eklund, J. (2006). Empathy and viewing the other as a subject. Scandinavian Journal of Psychology, 47, 399–409. 10.1111/j.1467-9450.2006.00521.x [DOI] [PubMed] [Google Scholar]
- Halpern, J. (2001). From detached concern to empathy: Humanizing medical practice. Oxford,UK: Oxford University Press. [Google Scholar]
- Haron, Y. , & Tran, D. (2014). Patients' perceptions of what makes a good doctor and nurse in an Israeli mental health hospital. Issues in Mental Health Nursing, 35(9), 672–679. 10.3109/01612840.2014.897778 [DOI] [PubMed] [Google Scholar]
- Haslam, N. (2007). Empathy in patient care: Antecedents, development, measurement, and outcomes by Mohammadreza Hojat. The New England Journal of Medicine, 356: 1792. [Google Scholar]
- Hodges, S. D. , Kiel, K. J. , Kramer, A. D. , Veach, D. , & Villanueva, B. R. (2010). Giving birth to empathy: The effects of similar experience on empathic accuracy, empathic concern, and perceived empathy. Personality and Social Psychology Bulletin, 36(3), 398–409. 10.1177/0146167209350326 [DOI] [PubMed] [Google Scholar]
- Hojat, M. (2007). Empathy in patient care: Antecedents, development, measurement, and outcomes. New York, NY: Springer. [Google Scholar]
- Hojat, M. , Gonnella, J. S. , Nasca, T. J. , Mangione, S. , Vergare, M. , & Magee, M. (2002). Physician empathy: Definition, components, measurement, and relationship to gender and specialty. The American Journal of Psychiatry, 159(9), 1563–1569. 10.1176/appi.ajp.159.9.1563 [DOI] [PubMed] [Google Scholar]
- Hojat, M. , Mangione, S. , Nasca, T. J. , Cohen, M. J. M. , Gonnella, J. S. , Erdmann, J. B. , … Magee, M. (2001). The Jefferson scale of physician empathy: Development and preliminary psychometric data. Educational and Psychological Measurement, 61, 349–365. 10.1177/00131640121971158 [DOI] [Google Scholar]
- Hojat, M. , Vergare, M. J. , Maxwell, K. , Brainard, G. , Herrine, S. K. , Isenberg, G. A. , … Gonnella, J. S. (2009). The devil is in the third year: A longitudinal study of erosion of empathy in medical school. Academic Medicine, 84(9), 1182–1191. 10.1097/ACM.0b013e3181b17e55 [DOI] [PubMed] [Google Scholar]
- Holm, U. (1985). Empati i läkar‐patientrelationen: En teoretisk och empirisk analys (Empathy in the doctor‐patient relationship: A theoretical and empirical analysis). Uppsala Studies in Education, 24, 983–275. [Google Scholar]
- Lee, K. C. , Yu, C. C. , Hsieh, P. L. , Li, C. C. , & Chao, Y. C. (2018). Situated teaching improves empathy learning of the students in a BSN program: A quasi‐experimental study. Nurse Education Today, 64, 138–143. 10.1016/j.nedt.2018.02.013 [DOI] [PubMed] [Google Scholar]
- Nunes, P. , Williams, S. , Sa, B. , & Stevenson, K.. (2011). A study of empathy decline in students from five health disciplines during their first year of training. International Journal of Medical Education, 2, 12–17. 10.5116/ijme.4d47.ddb0 [DOI] [Google Scholar]
- Percy, M. , & Richardson, C. (2018). Introducing nursing practice to student nurses: How can we promote care compassion and empathy. Nurse Education in Practice, 29, 200–205. 10.1016/j.nepr.2018.01.008 [DOI] [PubMed] [Google Scholar]
- Petrucci, C. , La Cerra, C. , Aloisio, F. , Montanari, P. , & Lancia, L. (2016). Empathy in health professional students: A comparative cross‐sectional study. Nurse Education Today, 41, 983–5. 10.1016/j.nedt.2016.03.022 [DOI] [PubMed] [Google Scholar]
- Purcell, S. R. , Kutash, M. , & Cobb, S. (2011). The relationship between nurses' stress and nurse staffing factors in a hospital setting. Journal of Nursing Management, 19(6), 714–720. 10.1111/j.1365-2834.2011.01262.x [DOI] [PubMed] [Google Scholar]
- Richardson, K. , Macleod, R. , & Kent, B. (2012). A Steinian approach to an empathic understanding of hope among patients and clinicians in the culture of palliative care. Journal of Advanced Nursing, 68(3), 686–694. 10.1111/j.1365-2648.2011.05793.x [DOI] [PubMed] [Google Scholar]
- Roff, S. (2015). Reconsidering the "decline" of medical student empathy as reported in studies using the Jefferson Scale of Physician Empathy‐Student version (JSPE‐S). Medical Teacher, 37(8), 783–786. 10.3109/0142159X.2015.1009022 [DOI] [PubMed] [Google Scholar]
- Rogers, C. R. (1957). The necessary and sufficient conditions of therapeutic personality change. Journal of Consulting Psychology, 21(2), 95–103. 10.1037/h0045357 [DOI] [PubMed] [Google Scholar]
- Rogers, C. R. (1975). Empathic: An unappreciated way of being. The Counseling Psychologist, 5, 2–11. 10.1177/001100007500500202 [DOI] [Google Scholar]
- Rush, B. , & Cook, J. (2006). What makes a good nurse? Views of patients and carers. British Journal of Nursing, 15, 382–385. 10.12968/bjon.2006.15.7.20901 [DOI] [PubMed] [Google Scholar]
- Soderberg, A. , Sundbaum, J. K. , & Engstrom, A. (2017). Nursing Students' Reflections After Meetings With Patients and Their Relatives Enacted by Professional Actors: Being Touched and Feeling Empathy. Issues in Mental Health Nursing, 38(2), 139–144. 10.1080/01612840.2016.1251517 [DOI] [PubMed] [Google Scholar]
- Sundling, V. , Sundler, A. J. , Holmstrom, I. K. , Kristensen, D. V. , & Eide, H. (2017). Mindfulness predicts student nurses' communication self‐efficacy: A cross‐national comparative study. Patient Education and Counseling, 100(8), 1558–1563. 10.1016/j.pec.2017.03.016 [DOI] [PubMed] [Google Scholar]
- Ward, J. (2016). The Empathy Enigma: Does It Still Exist? Comparison of Empathy Using Students and Standardized Actors. Nurse Educator, 41(3), 134–138. 10.1097/NNE.0000000000000236 [DOI] [PubMed] [Google Scholar]
- Ward, J. , Cody, J. , Schaal, M. , & Hojat, M. (2012). The empathy enigma: An empirical study of decline in empathy among undergraduate nursing students. Journal of Professional Nursing, 28(1), 34–40. 10.1016/j.profnurs.2011.10.007 [DOI] [PubMed] [Google Scholar]
- Ward, J. , Schaal, M. , Sullivan, J. , Bowen, M. E. , Erdmann, J. B. , & Hojat, M. (2009). Reliability and validity of the Jefferson Scale of Empathy in undergraduate nursing students. Journal of Nursing Measurement, 17(1), 73–88. 10.1891/1061-3749.17.1.73 [DOI] [PubMed] [Google Scholar]
- Williams, J. , & Stickley, T. (2010). Empathy and nurse education. Nurse Education Today, 30(8), 752–755. 10.1016/j.nedt.2010.01.018 [DOI] [PubMed] [Google Scholar]


