Abstract
Background:
No therapeutic intervention is universally accepted as the most effective treatment for adhesive capsulitis. An intra-articular corticosteroid injection (IAI) with a suprascapular nerve block (SSNB), a common treatment for this disease, is a safe and effective method for the resolution of pain and restoration of shoulder range of motion (ROM).
Purpose:
To compare the efficacy of combined SSNB and IAI with that of IAI alone in the treatment of adhesive capsulitis.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
We performed a retrospective review of 102 patients with adhesive capsulitis who were treated at an outpatient clinic from July 2016 to January 2017. A combined SSNB with IAI was performed in 48 patients (SSNB + IAI group), and an IAI alone was performed in 54 patients (IAI group). Patients were assessed before the intervention and at 2 weeks and 2 months after the intervention. ROM and pain and function visual analog scales (PVAS and FVAS, respectively), the American Shoulder and Elbow Surgeons (ASES) score, the Korean Shoulder Scoring System (KSS), the Constant score, the Simple Shoulder Test (SST), and the Shoulder Pain and Disability Index (SPADI) were used for clinical assessments. PVAS, FVAS, and ASES scores at a minimum of 1 year after the intervention were assessed for 82 patients.
Results:
At the 2-month assessment, all parameters significantly improved in both the SSNB + IAI and IAI groups (P < .05), however, improvements in forward flexion (FF) and abduction (ABD) between the 2-week and 2-month assessments were better in the SSNB + IAI group. At the 2-month assessment, improvements in the FVAS, ASES, SST, and SPADI scores and FF and ABD values were statistically significantly greater in the SSNB + IAI group compared with the IAI group. Improvements in FVAS and ASES scores were significantly greater in the SSNB + IAI group at a minimum of 1 year.
Conclusion:
Both a combined SSNB and IAI and an IAI alone significantly improved pain and functional outcomes in patients with adhesive capsulitis. The use of an SSNB with an IAI further increased treatment efficacy, as per the FVAS, ASES, SST, and SPADI scores and FF and ABD values. Patients who underwent SSNB combined with an IAI showed better improvements in the FVAS and ASES scores compared with IAI alone at a minimum of 1 year after the intervention. Therefore, an SSNB combined with an IAI may be a good treatment choice for adhesive capsulitis.
Keywords: adhesive capsulitis, shoulder, suprascapular nerve block, intra-articular corticosteroid injection
Adhesive capsulitis, or “frozen shoulder,” is a painful condition commonly encountered in outpatient orthopaedic clinics. It has a prevalence of 2% to 5% among outpatients but of about 20% to 30% in patients with diabetes mellitus (DM).21,23 The pathogenesis of this condition remains unclear, although associated factors include female sex, trauma, age over 40 years, DM, prolonged immobilization, thyroid disease, stroke, myocardial infarction, and autoimmune disease.3
Common nonoperative regimens for adhesive capsulitis include supervised neglect with analgesia, supervised physical therapy, an intra-articular corticosteroid injection (IAI), a suprascapular nerve block (SSNB), manual brisement, and saline dilatation.13,15,17,22 No therapeutic intervention is currently universally accepted as most effective for restoring range of motion (ROM) and decreasing pain in patients with this disease.19 It is widely accepted that physical therapy and stretching with use of analgesics are useful in the treatment of adhesive capsulitis, leading to improved joint mobility and the restoration of function.2,17,33 However, these interventions are usually painful, which negatively affects patient compliance during the rehabilitation program. Therefore, an IAI or SSNB may be beneficial before physical therapy.6,27,37 An IAI, one of the most common procedures, can lead to satisfactory results in the treatment of adhesive capsulitis, with improved ROM and prompt pain reduction.3,4,6,15,21,23,30 Previous studies have shown that an SSNB is also safe and effective, with faster and more efficient resolution of pain and restoration of ROM.11,27,37
We assumed that a combination of these 2 safe and effective modalities might be a good treatment option because of its cost-effectiveness and acceptance among patients with adhesive capsulitis. The purpose of our study was to compare the efficacy of combined SSNB and IAI with that of IAI alone in the treatment of adhesive capsulitis. We hypothesized that combined SSNB and IAI will improve pain and function better than IAI alone.
Methods
Patient Selection
We performed a retrospective review of 102 consecutive patients diagnosed with adhesive capsulitis who were treated at an outpatient clinic from July 2016 to January 2017. This study was approved by an institutional review board, and the requirement for obtaining informed consent was waived. Among the 102 patients, magnetic resonance imaging (MRI) was performed on 55 (53.9%) patients; 44 patients underwent noncontrast MRI at another hospital, and 11 patients underwent noncontrast MRI at our institute. The inclusion criteria were (1) adhesive capsulitis diagnosed by 2 orthopaedic specialists and (2) a minimum functional and radiological follow-up of 2 months. The exclusion criteria were (1) rheumatoid arthritis, (2) osteoarthritis, (3) postoperative stiff shoulders, (4) sequelae of infection, and (5) partial- or full-thickness rotator cuff tears as confirmed by MRI or ultrasonography.
An SSNB with an IAI (SSNB + IAI) was performed in 48 patients treated between July 2016 and October 2016, whereas an IAI alone was performed in 54 patients treated between November 2016 and January 2017. All patients were assessed before the intervention and at 2 weeks and 2 months after the intervention. Missing subjective outcome data were completed with telephone interviews. Through the telephone calls, follow-up data of more than 1 year (mean, 19 months [range, 17-23 months]) for the American Shoulder and Elbow Surgeons (ASES) score, function visual analog scale (FVAS), and pain visual analog scale (PVAS) were available. After the initial intervention, nonsteroidal anti-inflammatory drugs were given in both groups. All patients in both groups underwent a shoulder rehabilitation program consisting of active and passive ROM exercises as well as strengthening exercises of the rotator cuff and scapular stabilizing muscles at the outpatient clinic on the day of the first intervention.
Interventions
Intra-articular Corticosteroid Injection
All injections were performed at the same site using the posterior route under ultrasonographic guidance. Each injection contained 40 mg (1 mL) of triamcinolone acetonide and 4.5 mL of 2% lidocaine. After thorough sterilization, 5 mL of the combined solution was injected from the lateral to medial direction using the in-plane technique to place the tip within the joint capsule. If the patient had a PVAS score of ≥3 at the 2-week assessment, 1 more IAI was performed.
SSNB + IAI
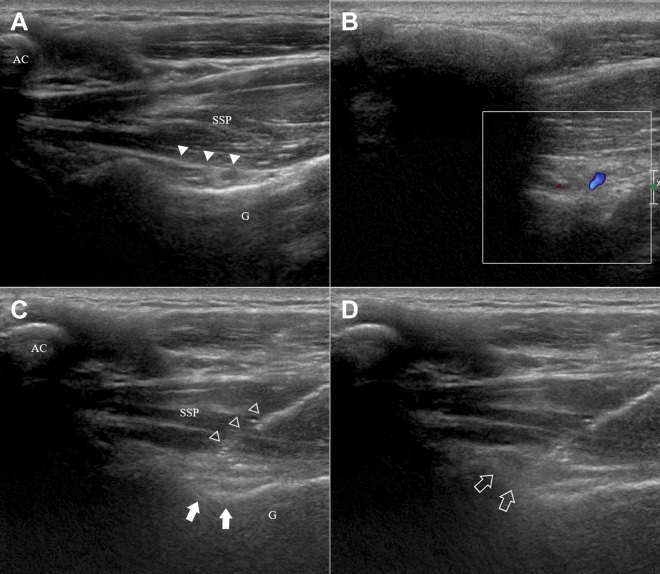
An SSNB was conducted using ultrasonography. With the patient seated, the spine of the scapula was identified. A transverse scan of the scapular spine (which could be identified by palpation) was first obtained, followed by a scan of the spinoglenoid notch. Color Doppler sonography might be useful at this stage to identify the suprascapular artery, which usually courses medially to the nerve. From this site, the nerve could then be easily tracked up to the coracoid notch. A needle was positioned at the desired location in the notch around the nerve using an in-plane approach. For this injection, 9.5 mL of 0.5% bupivacaine and 20 mg (0.5 mL) of triamcinolone acetonide were used (Figure 1). In the SSNB + IAI group, 20 mg (0.5 mL) of triamcinolone acetonide and 4.5 mL of 2% lidocaine were used for the IAI to match the total amount of corticosteroid (40 mg) used in the IAI group. If the patient had a PVAS score of ≥3 at the 2-week assessment, 1 more IAI was performed.
Figure 1.
Ultrasonographic images of the suprascapular nerve block (SSNB) at the spinoglenoid notch. (A) An ultrasonographic image of the suprascapular nerve. The hyperechoic line (solid arrowheads) is the inferior fascia of the supraspinatus (SSP). The suprascapular artery and nerve are located below this line. (B, C) After locating the suprascapular artery with a Doppler scan, the needle (open arrowheads) is inserted using a medial in-plane approach such that the tip is placed close to the spinoglenoid notch (solid arrows), where the suprascapular neurovascular bundle is located. As the bundle is barely visible, particular caution should be taken when performing this procedure. AC, acromion; G, glenoid. (D) Local anesthetic spreading around the suprascapular nerve after the injection (open arrows).
Clinical Evaluation
Patients were regularly evaluated in the outpatient clinic. The medical records of all patients were reviewed independently.
Clinical results were assessed using the PVAS, FVAS, ASES score,25 Korean Shoulder Scoring System (KSS),34 Constant score,10 Simple Shoulder Test (SST),18 and Shoulder Pain and Disability Index (SPADI)8,29 before the intervention and at 2 weeks and 2 months after the intervention. ROM, including forward flexion (FF), external rotation (ER) of the side, and abduction of the shoulder (ABD), was measured using a goniometer before the intervention and at each follow-up. ROM of the contralateral shoulder was measured before the intervention to verify the difference between the involved and contralateral sides, thus clarifing the diagnosis. Internal rotation of the back was not measured with goniometry; instead, it was scored from 0 to 14 points for the region from the buttock to T4 along the level of the vertebra. The patients were asked if they had any history of DM, thyroid disease, or trauma, as these are major secondary causes of adhesive capsulitis of the shoulder.
Statistical Analysis
Statistical analysis was performed using SAS version 9.4 (SAS Institute). A power analysis revealed that a sample of 51 patients in each group was required to detect a 1-point difference on the FVAS with a power of 80% and an α of 0.05, and a sample of 42 patients in each group was required to detect a 5-point difference on the ASES with a power of 80% and an α of 0.05. In the analysis of differences between the 2 groups, the normality hypothesis was tested with the Shapiro-Wilk test; the Student t test and Wilcoxon rank-sum test were then used for parameters following and deviating from the normal distribution, respectively. The chi-square test was used to examine the association between 2 categorical variables in demographic data. In the analysis of changes according to time, all the measurements in both groups had a normal distribution, and the paired t test was applied. To control for the duration of symptoms and presence of the DM (the 2 confounding variables that had P values <.2 on the t test, Wilcoxon rank-sum test, or chi-square test; P = .074 and .110, respectively), a linear regression analysis was used. A P value <.05 was considered to represent a statistically significant difference.
Results
The 102 study patients consisted of 28 men and 74 women with a mean age of 54.17 ± 7.12 years. In the SSNB + IAI group, there were 14 men and 34 women with a mean age of 54.31 ± 6.47 years (range, 42-67 years). Eleven (22.9%), 9 (18.8%), and 8 (16.7%) patients, respectively, named DM, thyroid disease, and trauma as the causative event. The mean duration of symptoms was 7.73 ± 7.59 months (range, 1-48 months), and the dominant shoulder was affected in 26 (54.2%) patients (Table 1).
TABLE 1.
Demographic Data of Patientsa
| SSNB + IAI (n = 48) | IAI (n = 54) | P | |
|---|---|---|---|
| Age, y | 54.31 ± 6.47 | 54.04 ± 7.71 | .847 |
| Sex | .714 | ||
| Male | 14 (29.2) | 14 (25.9) | |
| Female | 34 (70.8) | 40 (74.1) | |
| Shoulder | .743 | ||
| Left | 26 (54.2) | 31 (57.4) | |
| Right | 22 (45.8) | 23 (42.6) | |
| Dominant shoulder | 26 (54.2) | 28 (51.9) | .815 |
| Duration of symptoms, mo | 7.73 ± 7.59 | 6.26 ± 7.51 | .328 |
| Diabetes mellitus | 11 (22.9) | 6 (11.1) | .112 |
| Thyroid disease | 9 (18.8) | 14 (25.9) | .389 |
| Trauma | 8 (16.7) | 6 (11.1) | .418 |
aValues are presented as mean ± SD or n (%). IAI, intra-articular corticosteroid injection; SSNB, suprascapular nerve block.
In the IAI group, there were 14 men and 40 women with a mean age of 54.04 ± 7.71 years (range, 40-79 years). Six (11.1%), 14 (25.9%), and 6 (11.1%) patients, respectively, had a history of DM, thyroid disease, and trauma. The mean duration of symptoms was 6.26 ± 7.51 months (range, 1-44 months), and the dominant shoulder was affected in 28 (51.9%) patients (Table 1).
No complications occurred in either group. There were no significant differences between the groups in demographics and clinical characteristics before the intervention, except in the FVAS and SPADI scores (P > .05) (Tables 1 and 2). ROM of the involved shoulder before the intervention was significantly lower compared with that of the contralateral shoulder (Table 3).
TABLE 2.
Clinical Characteristics Before Interventiona
| SSNB + IAI | IAI | P Value | |
|---|---|---|---|
| PVAS | 6.73 ± 1.33 | 6.30 ± 1.46 | .158 |
| FVAS | 3.75 ± 1.87 | 4.91 ± 1.40 | .001 |
| ASES | 31.17 ± 11.01 | 35.22 ± 11.31 | .070 |
| Constant | 35.50 ± 8.81 | 38.91 ± 10.08 | .074 |
| KSS | 40.38 ± 11.55 | 39.98 ± 10.38 | .857 |
| SST | 3.15 ± 1.47 | 3.26 ± 1.31 | .770 |
| SPADI pain | 59.92 ± 14.17 | 52.28 ± 14.01 | .007 |
| SPADI disability | 63.44 ± 15.28 | 57.78 ± 13.38 | .049 |
| SPADI total | 62.44 ± 14.07 | 55.61 ± 12.78 | .020 |
| FF | 121.46 ± 22.31 | 126.85 ± 23.05 | .181 |
| ER | 33.33 ± 13.26 | 35.00 ± 15.14 | .617 |
| IR | 4.67 ± 3.19 | 5.09 ± 3.67 | .479 |
| ABD | 102.50 ± 29.21 | 112.41 ± 32.44 | .090 |
aValues are presented as mean ± SD. Bolded P values indicate statistically significant between-group differences (P < .05). ABD, abduction; ASES, American Shoulder and Elbow Surgeons; ER, external rotation; FF, forward flexion; FVAS, function visual analog scale; IAI, intra-articular corticosteroid injection; IR, internal rotation; KSS, Korean Shoulder Scoring System; PVAS, pain visual analog scale; SPADI, Shoulder Pain and Disability Index; SSNB, suprascapular nerve block; SST, Simple Shoulder Test.
TABLE 3.
ROM Between Involved and Contralateral Shoulders Before Interventiona
| SSNB + IAI | IAI | |||||
|---|---|---|---|---|---|---|
| Involved | Contralateral | P Value | Involved | Contralateral | P Value | |
| FF | 121.46 ± 22.31 | 159.79 ± 10.20 | <.001 | 126.85 ± 23.05 | 163.70 ± 8.96 | <.001 |
| ER | 33.33 ± 13.26 | 63.12 ± 17.03 | <.001 | 35.00 ± 15.14 | 67.22 ± 10.88 | <.001 |
| IR | 4.67 ± 3.19 | 11.37 ± 1.99 | <.001 | 5.09 ± 3.67 | 12.18 ± 1.86 | <.001 |
| ABD | 102.50 ± 29.21 | 157.50 ± 15.64 | <.001 | 112.41 ± 32.44 | 163.33 ± 8.01 | <.001 |
aValues are presented as mean ± SD. There were significant differences between the involved and contralateral shoulders on all ROM parameters (P < .05). ABD, abduction; ER, external rotation; FF, forward flexion; IAI, intra-articular corticosteroid injection; IR, internal rotation; ROM, range of motion; SSNB, suprascapular nerve block.
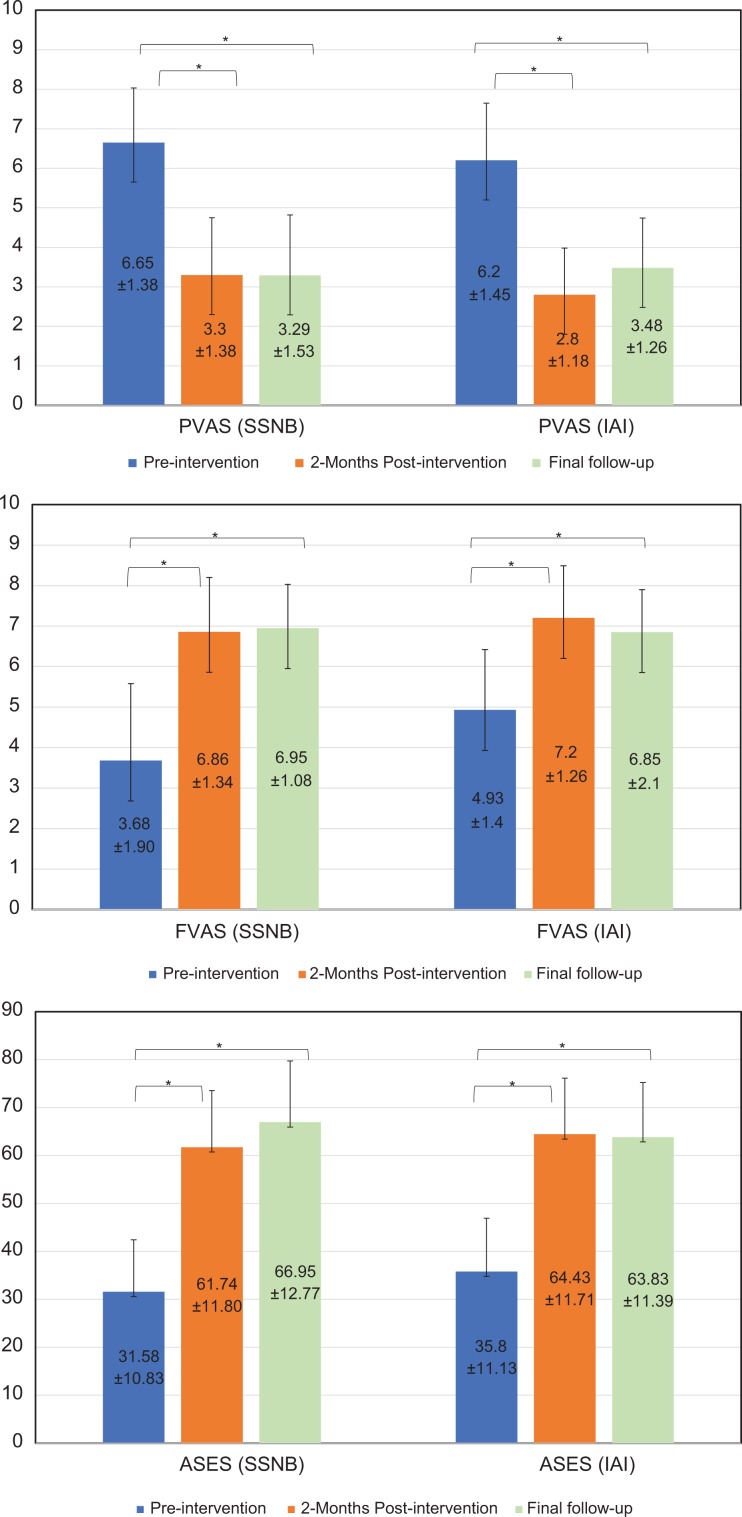
At the 2-week and 2-month assessments, all the follow-up parameters significantly improved in both the SSNB + IAI and the IAI groups (Tables 4 and 5). There was no significant difference between groups in the number of patients who received an additional IAI during the second week after the intervention (n = 31 [64.6%] in SSNB + IAI group vs n = 32 [59.3%] in IAI group; P = .581) (Table 6). In addition, the ASES, FVAS, and PVAS scores at a minimum of 1-year follow-up (mean, 19 months [range, 17-23 months]) were available. The improvements from baseline scores also remained significant at 1-year follow-up among these 3 clinical measures in both groups. However, there were no significant differences in scores between the 2-month and 1-year follow-ups (Figure 2).
TABLE 4.
Differences in Follow-up Parameters in the SSNB + IAI Groupa
| After Intervention | |||||
|---|---|---|---|---|---|
| Before Intervention | 2 wk | P Value | 2 mo | P Value | |
| PVAS | 6.73 ± 1.33 | 4.27 ± 1.65 | .001 | 3.25 ± 1.31 | <.001 |
| FVAS | 3.75 ± 1.87 | 5.73 ± 1.83 | <.001 | 6.77 ± 1.29 | <.001 |
| ASES | 31.17 ± 11.01 | 54.06 ± 13.35 | <.001 | 64.21 ± 11.05 | <.001 |
| Constant | 35.50 ± 8.81 | 52.04 ± 10.73 | <.001 | 60.73 ± 10.32 | <.001 |
| KSS | 40.38 ± 11.55 | 58.46 ± 12.26 | .001 | 66.00 ± 11.22 | <.001 |
| SST | 3.15 ± 1.47 | 5.44 ± 1.43 | .005 | 6.90 ± 1.29 | <.001 |
| SPADI pain | 59.92 ± 14.17 | 38.92 ± 14.01 | <.001 | 31.10 ± 11.24 | <.001 |
| SPADI disability | 63.44 ± 15.28 | 45.25 ± 13.72 | <.001 | 35.00 ± 11.63 | <.001 |
| SPADI total | 62.44 ± 14.07 | 42.83 ± 12.87 | <.001 | 34.15 ± 11.10 | <.001 |
| FF | 121.46 ± 22.31 | 143.13 ± 20.44 | <.001 | 153.13 ± 17.15 | <.001 |
| ER | 33.33 ± 13.26 | 46.46 ± 13.45 | .010 | 54.79 ± 13.84 | <.001 |
| IR | 4.67 ± 3.19 | 7.81 ± 3.11 | .009 | 9.02 ± 2.76 | .005 |
| ABD | 102.50 ± 29.21 | 134.79 ± 23.97 | <.001 | 151.25 ± 20.28 | <.001 |
aValues are presented as mean ± SD. All parameters at both follow-up times showed significant improvements compared with before intervention (P < .05). ABD, abduction; ASES, American Shoulder and Elbow Surgeons; ER, external rotation; FF, forward flexion; FVAS, function visual analog scale; IAI, intra-articular corticosteroid injection; IR, internal rotation; KSS, Korean Shoulder Scoring System; PVAS, pain visual analog scale; SPADI, Shoulder Pain and Disability Index; SSNB, suprascapular nerve block; SST, Simple Shoulder Test.
TABLE 5.
Differences in Follow-up Parameters in the IAI Groupa
| After Intervention | |||||
|---|---|---|---|---|---|
| Before Intervention | 2 wk | P Value | 2 mo | P Value | |
| PVAS | 6.30 ± 1.46 | 3.48 ± 1.51 | <.001 | 2.81 ± 1.29 | <.001 |
| FVAS | 4.91 ± 1.40 | 6.31 ± 1.49 | <.001 | 7.13 ± 1.26 | <.001 |
| ASES | 35.22 ± 11.31 | 57.11 ± 13.19 | <.001 | 63.76 ± 11.49 | <.001 |
| Constant | 38.91 ± 10.08 | 53.59 ± 11.59 | <.001 | 61.09 ± 10.34 | <.001 |
| KSS | 39.98 ± 10.38 | 58.48 ± 12.61 | .009 | 67.35 ± 1.51 | <.001 |
| SST | 3.26 ± 1.31 | 5.52 ± 1.59 | .010 | 6.56 ± 1.48 | <.001 |
| SPADI pain | 52.28 ± 14.01 | 34.52 ± 12.12 | <.001 | 29.54 ± 10.01 | <.001 |
| SPADI disability | 57.78 ± 13.38 | 41.26 ± 14.19 | <.001 | 34.76 ± 12.41 | <.001 |
| SPADI total | 55.61 ± 12.78 | 38.20 ± 12.30 | <.001 | 32.44 ± 10.23 | <.001 |
| FF | 126.85 ± 23.05 | 142.41 ± 19.32 | <.001 | 151.48 ± 16.53 | <.001 |
| ER | 35.00 ± 15.14 | 47.41 ± 14.94 | .029 | 55.00 ± 12.70 | <.001 |
| IR | 5.09 ± 3.67 | 7.80 ± 3.59 | .013 | 9.24 ± 3.35 | <.001 |
| ABD | 112.41 ± 32.44 | 135.93 ± 29.17 | <.001 | 148.33 ± 22.04 | <.001 |
aValues are presented as mean ± SD. All parameters at both follow-up times showed significant improvements compared with before intervention (P < .05). ABD, abduction; ASES, American Shoulder and Elbow Surgeons; ER, external rotation; FF, forward flexion; FVAS, function visual analog scale; IAI, intra-articular corticosteroid injection; IR, internal rotation; KSS, Korean Shoulder Scoring System; PVAS, pain visual analog scale; SPADI, Shoulder Pain and Disability Index; SST, Simple Shoulder Test.
TABLE 6.
Differences in Improvements Between Groups From Before Interventiona
| Before Intervention to 2 wk | Before Intervention to 2 mo | |||||
|---|---|---|---|---|---|---|
| SSNB + IAI | IAI | P Value | SSNB + IAI | IAI | P Value | |
| PVAS | –2.46 ± 1.38 | –2.81 ± 1.26 | .148 | –3.48 ± 1.27 | –3.48 ± 1.40 | .928 |
| FVAS | 1.98 ± 1.80 | 1.41 ± 1.28 | .076 | 3.02 ± 1.85 | 2.22 ± 1.50 | .015 |
| ASES | 22.90 ± 11.04 | 21.89 ± 10.51 | .636 | 33.04 ± 10.57 | 28.54 ± 11.11 | .039 |
| Constant | 16.54 ± 7.95 | 14.69 ± 8.23 | .277 | 25.23 ± 8.31 | 22.19 ± 8.22 | .060 |
| KSS | 18.08 ± 10.59 | 18.50 ± 8.67 | .696 | 25.63 ± 10.81 | 27.37 ± 9.50 | .326 |
| SST | 2.29 ± 1.11 | 2.26 ± 1.20 | .928 | 3.75 ± 0.86 | 3.30 ± 1.16 | .042 |
| SPADI pain | –21.00 ± 13.68 | –17.76 ± 11.68 | .241 | –28.81 ± 14.32 | –22.74 ± 12.22 | .029 |
| SPADI disability | –18.19 ± 13.54 | –16.52 ± 11.31 | .578 | –28.44 ± 14.18 | –23.02 ± 12.51 | .047 |
| SPADI total | –19.60 ± 12.72 | –17.41 ± 10.74 | .412 | –28.29 ± 13.53 | –23.17 ± 11.61 | .048 |
| FF | 21.67 ± 12.77 | 15.56 ± 11.92 | .018 | 31.67 ± 14.04 | 24.63 ± 12.24 | .009 |
| ER | 13.13 ± 10.35 | 12.41 ± 8.89 | .657 | 21.46 ± 9.89 | 20.00 ± 9.71 | .377 |
| IR | 3.15 ± 2.04 | 2.70 ± 2.47 | .242 | 4.35 ± 2.34 | 4.15 ± 2.57 | .568 |
| ABD | 32.29 ± 18.36 | 23.52 ± 22.92 | .045 | 48.75 ± 22.09 | 35.93 ± 23.59 | .007 |
| Additional IAI, n (%) | 31 (64.6) | 32 (59.3) | .581 | |||
aValues are presented as mean ± SD unless otherwise specified. Bolded P values indicate statistically significant between-group differences (P < .05). ABD, abduction; ASES, American Shoulder and Elbow Surgeons; ER, external rotation; FF, forward flexion; FVAS, function visual analog scale; IAI, intra-articular corticosteroid injection; IR, internal rotation; KSS, Korean Shoulder Scoring System; PVAS, pain visual analog scale; SPADI, Shoulder Pain and Disability Index; SSNB, suprascapular nerve block; SST, Simple Shoulder Test.
Figure 2.
Clinical outcomes of both groups between before intervention, 2 months, and final follow-up. *Significant difference (P < .05). ASES, American Shoulder and Elbow Surgeons; FVAS, function visual analog scale; IAI, intra-articular corticosteroid injection; PVAS, pain visual analog scale; SSNB, suprascapular nerve block.
A comparison of the groups at the 2-week assessment revealed better FF and ABD values in the SSNB + IAI group (P = .018 and P = .045, respectively) (Table 6). At the 2-month assessment, the improvements in the FVAS, ASES, SST, and SPADI scores and FF and ABD values were significantly larger in the SSNB + IAI group than in the IAI group (Table 6). Additionally, the improvements in the PVAS, ASES, SST, and SPADI scores between the 2-week and 2-month assessments were significantly better in the SSNB + IAI group (Table 7).
TABLE 7.
Differences in Improvements Between Groups From 2-Week to 2-Month Assessmentsa
| SSNB + IAI | IAI | P Value | |
|---|---|---|---|
| PVAS | –1.02 ± 1.00 | –0.67 ± 0.75 | .043 |
| FVAS | 1.04 ± 1.46 | 0.81 ± 1.10 | .286 |
| ASES | 10.15 ± 6.23 | 6.65 ± 6.18 | .005 |
| Constant | 8.69 ± 5.36 | 7.50 ± 4.40 | .161 |
| KSS | 7.54 ± 5.05 | 8.87 ± 5.80 | .258 |
| SST | 1.46 ± 0.62 | 1.04 ± 0.67 | .002 |
| SPADI pain | –7.81 ± 7.82 | –4.98 ± 5.92 | .037 |
| SPADI disability | –10.25 ± 5.65 | –6.50 ± 7.11 | .002 |
| SPADI total | –8.69 ± 6.42 | –5.76 ± 6.58 | .019 |
| FF | 10.00 ± 8.25 | 9.07 ± 8.30 | .535 |
| ER | 8.33 ± 9.07 | 7.59 ± 6.71 | .580 |
| IR | 1.21 ± 1.47 | 1.44 ± 1.74 | .440 |
| ABD | 16.46 ± 11.76 | 12.41 ± 15.65 | .135 |
aValues are presented as mean ± SD. Bolded P values indicate statistically significant between-group differences (P < .05). ABD, abduction; ASES, American Shoulder and Elbow Surgeons; ER, external rotation; FF, forward flexion; FVAS, function visual analog scale; IAI, intra-articular corticosteroid injection; IR, internal rotation; KSS, Korean Shoulder Scoring System; PVAS, pain visual analog scale; SPADI, Shoulder Pain and Disability Index; SSNB, suprascapular nerve block; SST, Simple Shoulder Test.
A comparison of the groups at a minimum 1-year follow-up also revealed significantly better ASES and FVAS scores in the SSNB + IAI group. The improvements on the PVAS were larger in the SSNB + IAI group than in the IAI, although this difference was not statistically significant (Table 8).
TABLE 8.
Differences in Improvements Between Groups From Before Intervention to Final Follow-upa
| SSNB + IAI | IAI | P Value | |
|---|---|---|---|
| PVAS | –3.35 ± 1.57 | –2.73 ± 1.57 | .084 |
| FVAS | 3.27 ± 2.13 | 1.93 ± 1.56 | .005 |
| ASES | 35.46 ± 13.86 | 28.03 ± 12.24 | .015 |
aValues are presented as mean ± SD. Bolded P values indicate statistically significant between-group differences (P < .05). ASES, American Shoulder and Elbow Surgeons; FVAS, function visual analog scale; IAI, intra-articular corticosteroid injection; PVAS, pain visual analog scale; SSNB, suprascapular nerve block.
Discussion
In general, the symptoms of adhesive capsulitis, severe pain and limitation of ROM, peak at 3 to 6 months after the onset of this disease.14,17 It is the physician’s task to alleviate this flare. Therefore, an early intervention, such as an IAI or SSNB, during this period is crucial and may precede physical therapy to allow patients to fully participate in a rehabilitation program.6,27,37 This study investigated whether the combined effect of an SSNB and IAI improves pain and functional scores during this severe flare phase. Based on our findings, both SSBI + IAI and IAI alone resulted in significantly improved outcome parameters at 2-week and 2-month follow-ups, including pain and functional status. Moreover, at 2-month follow-up, SSBI combined with IAI led to greater improvements in FVAS, ASES, SST, and SPADI scores and FF and ABD values compared with IAI alone, and at 1-year follow-up, FVAS and ASES scores were significantly improved in the SSNB + IAI group compared with the IAI group. However, there were no significant differences between the 2 groups in PVAS, Constant, and KSS scores or in ER and IR at any follow-up time point. Among these parameters, the Constant and KSS scores are similar in that they both include ROM in the score items. According to the results of this study, the combination of an SSNB with an IAI seems to improve function and disability parameters but not ROM, especially in rotations of the shoulder.
Our findings on the use of an IAI for the treatment of adhesive capsulitis are consistent with those in the literature.3,4,6,15,21,23,30 Previous systematic reviews on the use of corticosteroids mostly found evidence of their short-term effectiveness.4,5,24,32 In 2016, Koh21 performed a systematic review of randomized clinical trials on the use of corticosteroid injections in adhesive capsulitis. The authors concluded that a corticosteroid injection is superior to placebo and physical therapy in the short term (up to 12 weeks). Therefore, patients in the early stage of the disease, where the predominant symptom is pain, may consider an early corticosteroid injection, which might help resolve the symptoms quickly, before undergoing physical therapy or performing exercises at home.
Many studies have compared the effectiveness of an SSNB with that of a series of IAIs in the treatment of adhesive capsulitis. Although some concluded that SSNB and IAI had similar efficacy,7,37 others demonstrated that SSNB provided better pain relief and greater functional improvement than IAI.1,13,20
In terms of the effects of SSNB in the treatment of adhesive capsulitis, our study is in agreement with previous studies.11,27,37 Ozkan et al27 compared the effects of SSNB in patients with adhesive capsulitis unresponsive to IAI. In that study, patients’ simple pain scores and total pain scores, as well as ABD, ER, and internal rotation values, improved significantly after SSNB. A double-blind randomized clinical trial by Dahan et al11 compared a treatment group that received 10 mL of bupivacaine SSNB with a placebo group that received 10 mL of physiological saline. The authors concluded that the bupivacaine SSNB was effective in reducing pain in adhesive capsulitis at 1 month. In contrast, the present study compared the effectiveness of 2 treatment methods: the combination of SSNB with IAI versus IAI alone. This makes it different from the previous studies.
We performed an additional IAI in patients with a PVAS score of ≥3 at 2-week follow-up. A systematic review of randomized trials using multiple corticosteroid injections in adhesive capsulitis32 suggested that multiple injections are beneficial until 16 weeks from the date of the first injection. Up to 3 injections were beneficial, and there was limited evidence that 4 to 6 injections also had a positive effect. There was no evidence to support more than 6 injections.
We used a common combination of 9.5 mL of 0.5% bupivacaine and 0.5 mL (20 mg) of triamcinolone acetonide for the SSNB in this study. Bupivacaine is the first choice for regional anesthesia owing to its effectiveness, long duration, and milder motor blockade. In addition, some studies have suggested that a combination of corticosteroids with local anesthetics prolongs the efficacy of nerve blockage up to 1.5 to 2 times and decreases pain scores.28,39 Therefore, a combination with a corticosteroid was selected in this study to prolong the blockage duration and increase the analgesic effects. Although bupivacaine is the most widely used long-acting local anesthetic agent, it is associated with various central nervous system and cardiac toxicities.9,26,35 Ropivacaine has been proposed as a promising drug with fewer cardiovascular and central nervous system toxicity effects compared with bupivacaine.31 However, comparative studies of cardiovascular safety have reported that these 2 anesthetic agents have similar efficacy and incidences of cardiotoxicity.16,38 There were no cardiovascular adverse effects in our study.
Our study has several limitations. First, although a sample of 51 patients in each group was required according to the power analysis, loss to follow-up reduced the size of our SSNB + IAI group to 48 patients. Nevertheless, a sample of 42 patients in each group was fulfilled in the case of the ASES score. Second, our study showed significantly lower preintervention SPADI and FVAS scores in the SSNB + IAI group than in the IAI group. This may be because of the inherent weakness of a retrospective cohort study. However, the SSNB + IAI group showed significantly better improvements in the SPADI and FVAS scores than the IAI group at 2-month follow-up, despite the initially inferior clinical scores. This strongly emphasizes the efficacy of the SSNB in our study. Third, 2-month follow-up may be considered to be short. Although a minimum 1-year follow-up was available for ASES, PVAS, and FVAS scores, the final follow-up rate of telephone interviews was 80%. An analysis of a longer follow-up period with the rest of the outcome measures might be beneficial. However, the main question of the present study was whether the 2 procedures had immediate effects on pain and function to facilitate further rehabilitation. Furthermore, it is unclear whether a longer follow-up than 1 year would be informative considering the natural history of this disease. In our study, the ASES, FVAS, and PVAS did not show statistically significant improvements at final follow-up compared with 2 months.
A fourth limitation was that at both 2-month and final follow-up, each group met the minimal clinically important difference (MCID) compared with before the intervention; however, the MCID between the groups might not be fulfilled. The MCID has been reported to be around a 12- to 17-point change on the ASES score after conservative treatment for tendinitis or rotator cuff tears,36 and others have reported that the MCID after treating chronic shoulder pain was a reduction of approximately 2 points on an 11-point numerical pain rating scale.12 However, to our knowledge, there is no previous literature on the MCID of the ASES score or FVAS after conservative treatment for adhesive capsulitis. Fifth, it was difficult to conclude that the SSNB + IAI group had significantly improved outcomes versus the IAI group at final follow-up because of the less than 100% follow-up rate, even after the telephone survey. Sixth, we did not have a control or SSNB-only group. Performing an IAI after an SSNB only took an additional 5 minutes, even with ultrasonographic guidance in our study; hence, we performed an IAI in all cases. Further study would be beneficial to compare the effectiveness between SSNB-only, IAI-only, and SSNB + IAI. Seventh, MRI, which might have been helpful to exclude other comorbidities that may affect the clinical results, was not performed on all patients. However, a thorough ultrasonographic examination was performed in all patients to locate other possible shoulder lesions such as rotator cuff tears. In addition, relatively expensive MRI was not easy to perform routinely on a cost-sensitive outpatient basis. Finally, it was uncertain whether the patients of both groups underwent additional professional rehabilitation. A frozen shoulder is an easily overlooked condition in South Korea, so patients usually do not receive consistent and professional physical therapy outside of a university hospital. Therefore, we assume that the rate of postintervention rehabilitation was not very different between the groups.
Conclusion
Both SSNB + IAI and IAI alone significantly improved pain and functional outcomes in patients with adhesive capsulitis. Moreover, the application of an SSNB with IAI further increased the efficacy, as per the FVAS, ASES, SST, and SPADI scores and FF and ABD values. Furthermore, SSNB + IAI treatment led to greater improvements in FVAS and ASES scores compared with IAI alone at a minimum of 1 year after the intervention. Therefore, an SSNB with an IAI may be a better choice for the treatment of adhesive capsulitis accompanied with severe pain and functional loss.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Samsung Medical Center Institutional Review Board (No. 2017-09-006).
References
- 1. Abdelshafi ME, Yosry M, Elmulla AF, Al-Shahawy EA, Adou Aly M, Eliewa EA. Relief of chronic shoulder pain: a comparative study of three approaches. Middle East J Anaesthesiol. 2011;21:83–92. [PubMed] [Google Scholar]
- 2. Anton HA. Frozen shoulder. Can Fam Physician. 1993;39:1773–1778. [PMC free article] [PubMed] [Google Scholar]
- 3. Bal A, Eksioglu E, Gulec B, Aydog E, Gurcay E, Cakci A. Effectiveness of corticosteroid injection in adhesive capsulitis. Clin Rehabil. 2008;22:503–512. [DOI] [PubMed] [Google Scholar]
- 4. Blanchard V, Barr S, Cerisola FL. The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: a systematic review. Physiotherapy. 2010;96:95–107. [DOI] [PubMed] [Google Scholar]
- 5. Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 2003;(1):CD004016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carette S, Moffet H, Tardif J, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis Rheum. 2003;48:829–838. [DOI] [PubMed] [Google Scholar]
- 7. Chang KV, Hung CY, Wu WT, Han DS, Yang RS, Lin CP. Comparison of the effectiveness of suprascapular nerve block with physical therapy, placebo, and intra-articular injection in management of chronic shoulder pain: a meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2016;97:1366–1380. [DOI] [PubMed] [Google Scholar]
- 8. Choi Y, Park JW, Noh S, Kim MS, Park YH, Sung DH. Reliability, validity, and responsiveness of the Korean version of the Shoulder Disability Questionnaire and Shoulder Rating Questionnaire. Ann Rehabil Med. 2015;39:705–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Clarkson CW, Hondeghem LM. Mechanism for bupivacaine depression of cardiac conduction: fast block of sodium channels during the action potential with slow recovery from block during diastole. Anesthesiology. 1985;62:396–405. [PubMed] [Google Scholar]
- 10. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 11. Dahan TH, Fortin L, Pelletier M, Petit M, Vadeboncoeur R, Suissa S. Double blind randomized clinical trial examining the efficacy of bupivacaine suprascapular nerve blocks in frozen shoulder. J Rheumatol. 2000;27:1464–1469. [PubMed] [Google Scholar]
- 12. Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. [DOI] [PubMed] [Google Scholar]
- 13. Favejee MM, Huisstede BM, Koes BW. Frozen shoulder: the effectiveness of conservative and surgical interventions. Systematic review. Br J Sports Med. 2011;45:49–56. [DOI] [PubMed] [Google Scholar]
- 14. Georgiannos D, Markopoulos G, Devetzi E, Bisbinas I. Adhesive capsulitis of the shoulder: is there consensus regarding the treatment? A comprehensive review. Open Orthop J. 2017;11:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Griesser MJ, Harris JD, Campbell JE, Jones GL. Adhesive capsulitis of the shoulder: a systematic review of the effectiveness of intra-articular corticosteroid injections. J Bone Joint Surg Am. 2011;93:1727–1733. [DOI] [PubMed] [Google Scholar]
- 16. Hamaji A, Rezende MR, Mattar R, Jr, Vieira JE, Auler JO., Jr Comparative study related to cardiovascular safety between bupivacaine (S75-R25) and ropivacaine in brachial plexus block. Braz J Anesthesiol. 2013;63:322–326. [DOI] [PubMed] [Google Scholar]
- 17. Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA. Current review of adhesive capsulitis. J Shoulder Elbow Surg. 2011;20:502–514. [DOI] [PubMed] [Google Scholar]
- 18. Hsu JE, Russ SM, Somerson JS, Tang A, Warme WJ, Matsen FA., 3rd Is the Simple Shoulder Test a valid outcome instrument for shoulder arthroplasty? J Shoulder Elbow Surg. 2017;26:1693–1700. [DOI] [PubMed] [Google Scholar]
- 19. Johnson AJ, Godges JJ, Zimmerman GJ, Ounanian LL. The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. J Orthop Sports Phys Ther. 2007;37:88–99. [DOI] [PubMed] [Google Scholar]
- 20. Jones DS, Chattopadhyay C. Suprascapular nerve block for the treatment of frozen shoulder in primary care: a randomized trial. Br J Gen Pract. 1999;49:39–41. [PMC free article] [PubMed] [Google Scholar]
- 21. Koh KH. Corticosteroid injection for adhesive capsulitis in primary care: a systematic review of randomised clinical trials. Singapore Med J. 2016;57:646–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Levine WN, Kashyap CP, Bak SF, Ahmad CS, Blaine TA, Bigliani LU. Nonoperative management of idiopathic adhesive capsulitis. J Shoulder Elbow Surg. 2007;16:569–573. [DOI] [PubMed] [Google Scholar]
- 23. Lorbach O, Anagnostakos K, Scherf C, Seil R, Kohn D, Pape D. Nonoperative management of adhesive capsulitis of the shoulder: oral cortisone application versus intra-articular cortisone injections. J Shoulder Elbow Surg. 2010;19:172–179. [DOI] [PubMed] [Google Scholar]
- 24. Maund E, Craig D, Suekarran S, et al. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2012;16:1–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587–594. [DOI] [PubMed] [Google Scholar]
- 26. Moller R, Covino BG. Cardiac electrophysiologic properties of bupivacaine and lidocaine compared with those of ropivacaine, a new amide local anesthetic. Anesthesiology. 1990;72:322–329. [DOI] [PubMed] [Google Scholar]
- 27. Ozkan K, Ozcekic AN, Sarar S, Cift H, Ozkan FU, Unay K. Suprascapular nerve block for the treatment of frozen shoulder. Saudi J Anaesth. 2012;6:52–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Parrington SJ, O’Donnell D, Chan VW, et al. Dexamethasone added to mepivacaine prolongs the duration of analgesia after supraclavicular brachial plexus blockade. Reg Anesth Pain Med. 2010;35:422–426. [DOI] [PubMed] [Google Scholar]
- 29. Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a Shoulder Pain and Disability Index. Arthritis Care Res. 1991;4:143–149. [PubMed] [Google Scholar]
- 30. Ryans I, Montgomery A, Galway R, Kernohan WG, McKane R. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology (Oxford). 2005;44:529–535. [DOI] [PubMed] [Google Scholar]
- 31. Scott DB, Lee A, Fagan D, Bowler GM, Bloomfield P, Lundh R. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg. 1989;69:563–569. [PubMed] [Google Scholar]
- 32. Shah N, Lewis M. Shoulder adhesive capsulitis: systematic review of randomised trials using multiple corticosteroid injections. Br J Gen Pract. 2007;57:662–667. [PMC free article] [PubMed] [Google Scholar]
- 33. Struyf F, Meeus M. Current evidence on physical therapy in patients with adhesive capsulitis: what are we missing? Clin Rheumatol. 2014;33:593–600. [DOI] [PubMed] [Google Scholar]
- 34. Tae SK, Rhee YG, Park TS, et al. The development and validation of an appraisal method for rotator cuff disorders: the Korean Shoulder Scoring System. J Shoulder Elbow Surg. 2009;18:689–696. [DOI] [PubMed] [Google Scholar]
- 35. Tanz RD, Heskett T, Loehning RW, Fairfax CA. Comparative cardiotoxicity of bupivacaine and lidocaine in the isolated perfused mammalian heart. Anesth Analg. 1984;63:549–556. [PubMed] [Google Scholar]
- 36. Tashjian RZ, Deloach J, Green A, Porucznik CA, Powell AP. Minimal clinically important differences in ASES and Simple Shoulder Test scores after nonoperative treatment of rotator cuff disease. J Bone Joint Surg Am. 2010;92:296–303. [DOI] [PubMed] [Google Scholar]
- 37. Taskaynatan MA, Yilmaz B, Ozgul A, Yazicioglu K, Kalyon TA. Suprascapular nerve block versus steroid injection for non-specific shoulder pain. Tohoku J Exp Med. 2005;205:19–25. [DOI] [PubMed] [Google Scholar]
- 38. Venkatesh RR, Kumar P, Trissur RR, George SK. A randomized controlled study of 0.5% bupivacaine, 0.5% ropivacaine and 0.75% ropivacaine for supraclavicular brachial plexus block. J Clin Diagn Res. 2016;10:UC09–UC12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vieira PA, Pulai I, Tsao GC, Manikantan P, Keller B, Connelly NR. Dexamethasone with bupivacaine increases duration of analgesia in ultrasound-guided interscalene brachial plexus blockade. Eur J Anaesthesiol. 2010;27:285–288. [DOI] [PubMed] [Google Scholar]