Abstract
Background
Anxiety and depression are implicated as contributors to abdominal pain in pediatric irritable bowel syndrome (IBS) but is unclear if this pain is associated with other psychological factors. The study objective was to test if the impact of anxiety or depression on IBS symptom severity is mediated by somatization and/or pain catastrophizing.
Methods
We utilized baseline data from local pediatric IBS clinical studies. Through mediation analysis, we assessed whether somatization or pain catastrophizing mediated (either independently or combined) the separate relationships of anxiety or depression with IBS abdominal pain severity.
Key Results
We analyzed 261 participants. All psychological factors were positively correlated with one another and IBS abdominal pain severity. The association of anxiety with IBS abdominal pain was mediated by both somatization and pain catastrophizing in individual analyses (each mediated standardized coefficient [β] 0.11, CI 0.05 – 0.18) and in multiple analysis (mediated standardized β 0.18, CI 0.09 – 0.27). The association of depression with IBS abdominal pain was also mediated by somatization (mediated standardized β 0.08, CI 0.02 – 0.14) and pain catastrophizing (mediated standardized β 0.06, CI 0.01 – 0.11) in individual analyses and in multiple analysis (mediated standardized β 0.19, CI 0.04 – 0.19).
Conclusions & Inferences
Somatization and pain catastrophizing mediate the relationships between anxiety/depression and IBS abdominal pain severity. These findings suggest that somatization and pain catastrophizing may be better treatment targets than anxiety and depression. Clinicians should assess these psychological factors in pediatric IBS patients and refer for intervention to improve outcomes.
Keywords: psychological factors, anxiety, depression, somatization, pain catastrophizing, irritable bowel syndrome, pediatric, mediation analysis
Introduction
Irritable bowel syndrome (IBS) is characterized by chronic abdominal pain and changes in stool consistency and/or stooling frequency not attributable to specific anatomic or biochemical abnormality (1, 2). IBS affects about 9% of children worldwide (3). Over half of affected children have abdominal pain symptoms into adulthood, which is associated with a $30 billion annual economic burden in the United States (4–9).
Compared to healthy children, children with IBS demonstrate increased psychological distress, specifically anxiety and depression, though symptom severity does not typically reach the level of a clinical diagnosis of an anxiety or depressive disorder (10–21). Moderate elevations in distress also exist in children with organic chronic conditions, suggesting the elevated distress in IBS may be a reaction to chronic symptoms (22–24). Alternatively, the biopsychosocial model of IBS suggests anxiety and depression may be important contributing factors to IBS symptoms; some data support increased anxiety preceding an IBS diagnosis (25, 26). Further, anxiety and depression are associated with abdominal pain outcomes within the population of children with IBS (27, 28).
Though anxiety and depression are most often studied, other psychological factors should be considered relevant to IBS outcomes. van Tilburg and colleagues provided a framework for exploring multiple psychological factors potentially involved in the symptom experience (29). Somatization is defined as experiencing symptoms affecting multiple organ symptoms that cannot be explained medically (30). Pain catastrophizing is an irrational expectation of the worst and feeling helpless in response to an actual or anticipated painful event (31). In adults with IBS, the authors found somatization and pain catastrophizing each better explain the relationship between anxiety and IBS symptom severity (29). These results suggest somatization and pain catastrophizing as potential important targets for psychotherapy in adults with IBS.
Evidence exists suggesting this same relation may be true for children. Our research group has shown somatization is associated with abdominal pain symptoms in children with functional abdominal pain (32). In a sample of healthy children without a functional abdominal pain disorder, Lavigne and colleagues found somatization mediated the relation between anxiety/depression and abdominal pain (33). Further, van Tilburg and colleagues demonstrated changes in pain catastrophizing, rather than anxiety or depression, explained the effect of cognitive behavioral therapy treatment on pediatric IBS pain (34). However, no study to date has specifically tested if the effects of anxiety/depression on IBS abdominal pain is better explained by somatization and pain catastrophizing. Therefore, we examined whether somatization or pain catastrophizing, either individually or combined, mediates the association of anxiety/depression and IBS abdominal pain symptom severity in children with IBS. We hypothesized that somatization and pain catastrophizing would both mediate the association of anxiety/depression with IBS abdominal pain severity and thereby identify a stronger association compared to the original relationship excluding these maladaptive processes.
Materials and Methods
Participants
This study utilized previously collected clinical study data from children with IBS. The participants’ data were collected from a total of four observational and interventional pediatric clinical trials conducted at Baylor College of Medicine and Texas Children’s Hospital in Houston, TX (35–38). One parent signed informed consent and the child provided assent prior to initiation of each study. Only participant baseline data prior to any intervention were utilized. At baseline each participant completed psychological and demographic measures and a validated two-week abdominal pain/stooling diary, which captured abdominal pain frequency and intensity during three periods throughout the day (morning, afternoon, and evening).
Demographics and IBS Abdominal Pain
Caregivers provided the child participants’ age, gender, and race/ethnicity at enrollment through a self-report questionnaire. The use of a 2-week validated abdominal pain/stooling diary defined our IBS cohort based on Rome III criteria and our previously published algorithm (39–43). The diary captured the number of pain episodes per day and intensity of the abdominal pain when it occurred (35). For this study, IBS abdominal pain was measured by multiplying the number of pain episodes over a two-week period by the mean pain intensity when a pain episode occurred as rated on a 10-point scale, which has been utilized as an outcome in other clinical studies in the field (44–50).
Psychological Instruments
Anxiety and Depression
Anxiety and depression were measured using the Behavior Assessment System for Children, which assesses behavioral and emotional problems in children and adolescents through parent proxy- and child self-report (51, 52). Only self-reported scores were used for this study. One of the four clinical studies used the original edition of the BASC instrument; the other three studies used the later version BASC-2 (51, 52). BASC scores were converted to BASC-2 scores as per the manual (52). All BASC-2 child-reported anxiety and depression scale T-scores were transformed into their respective Z-score based on each scales’ distribution in our cohort. These Z-scores were utilized for mediation analyses.
Somatization
Our studies captured child somatization using the Children’s Somatization Inventory (CSI) (53). Children indicated the extent to which they were bothered by 35 non-specific symptoms such as headaches and nausea using a 5-point Likert scale (ranging from “not at all” to “a whole lot”). All item responses were summed into a total score. Total scores were then transformed into a Z-score based on our sample’s distribution for mediation analysis to standardize our results.
Pain Catastrophizing
Pain catastrophizing was captured by two separate instruments for the four pediatric IBS clinical studies. Two of the four clinical studies used the child self-report of the Pain Catastrophizing Scale (PCS-C) (54, 55). The PCS-C is a validated 11-item survey answered on a 5-point Likert scale ranging from 0 to 4 (56, 57). All items are summed for a total score. Subscales for this survey includes Rumination (cannot stop thinking about pain), Magnification (concern about the seriousness of the pain), and Helplessness (how overwhelming the pain is). A Z-score was assigned to the total score value based on this instrument’s sample distribution.
The two other clinical studies used the Pain Response Inventory (PRI), a validated 60-item survey designed to assess coping skills for children with chronic pain using a 5-point Likert scale ranging from 0 to 4 (45, 58, 59). We used questions from the Catastrophizing and Distract/Ignore subscales, which were very similar to the PCS-C questions and reflected the Rumination, Magnification, and Helplessness dimensions described above. To calculate our PRI-derived catastrophizing total score variable, we summed the responses from the PRI Catastrophizing Scale and reverse coded 3 item responses from the PRI Distract/Ignore Scale (items 34, 44, and 48) (e.g., Try to think of something pleasant to take you mind off the pain). The 8 items were summed and Z-scores were calculated based on the sample distribution for this specific instrument (Supplementary Table C). Then the Z-scores from both the PCS-C and PRI were combined to create a single pain catastrophizing variable that was utilized for all analyses.
Statistical Analysis
Age, gender, and race/ethnicity were covariates for all analyses. We included only participants who had complete data for all variables and covariates of interest. A sensitivity analysis was conducted to compare excluded participants and the original cohort to assess for any biases in our cohort.
Bivariate correlation analysis evaluated the association between each of the psychological variables and IBS abdominal pain. Multiple linear regression modeling then assessed concurrently the association of the psychological variables with IBS abdominal pain. Statistical significance in multiple linear regression modeling for anxiety and depression predicting IBS abdominal pain severity was a required precondition for proceeding to mediation analyses to assess the whether these relationships are affected by somatization and pain catastrophizing. Multicollinearity was also assessed via the variance inflation factor, indicating that multicollinearity was not problematic (i.e., variance inflation factor < 4 for all variables).
Mediation Analysis
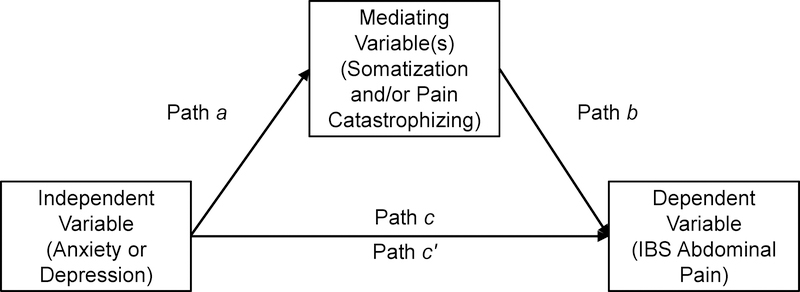
Mediation can be described as the introduction of a third variable that explains the relationship of an established two-variable system (60). In other words, the association between two variables may be significant, but a third mediating variable accounts for the variance initially attributed to the original two variable relationship. Figure 1 represents a generic model for mediation analysis in this study. We examined whether the association between anxiety or depression (independent variables) and the dependent variable of IBS abdominal pain can be better explained alone (path c) or in the presence of a mediating variable(s) (paths a and b). When mediation occurs, the indirect relationship summarized in path c′ is smaller than the direct relationship summarized in path c (Figure 1).
Figure 1. Conceptual Model of Mediation Analysis for Psychological Factors on IBS Abdominal Pain.
Path a represents the effect of the independent variable on the mediator(s).
Path b represents the effect of the mediator(s) on the dependent variable.
Path c illustrates the total effect which considers both the relationship of the independent variable on the dependent variable and other indirect or mediating effects.
Path c′ captures the direct effect of the independent variable on the dependent variable in the presence of other mediator(s).
We first conducted individual mediation analysis by evaluating separately the impact of a single mediator (i.e., somatization or pain catastrophizing Z-scores) on the relationship between our independent variables (i.e., anxiety or depression Z-scores) and the dependent variable of IBS abdominal pain severity Z-scores. Each analysis calculated the standardized coefficient (β) and its 95% confidence interval (CI) for each direct and indirect relationship (paths a, b, c, and c′). If both mediators were significant in individual mediation analysis, we then conducted multiple mediation analysis to assess to what degree anxiety/depression and IBS abdominal pain were affected by dual mediators of somatization and pain catastrophizing in a multiple mediation model.
Statistical analyses were performed in SPSS Statistics 25 for Windows software (IBM Corporation, Armonk, NY). The average and standard deviation were calculated for age and proportions for the other demographic categorical variables. We computed the mean, standard deviation, range, and Z-score for all psychological variables and IBS abdominal pain. Statistical significance for all analyses was defined as P < 0.05. The mediation analysis was conducted in SPSS Statistics using PROCESS version 3.0 extension (61). Bootstrap estimation with 1,000 samples was used to test the indirect effects of the mediator(s) in the individual and multiple mediation tests. Significant mediation results were defined by a 95% confidence interval range that does not contain zero (61).
Results
Our initial cohort included 283 children with IBS who completed psychological instruments and a baseline 2-week abdominal pain/stooling diary (n=86 from an interventional clinical study and n=197 from non-interventional studies). Of this sample, 261 participants had completed data for all covariate and psychological variables. Sensitivity analysis between the original cohort and the 22 excluded participants revealed a small but clinically irrelevant difference in age (10.3 ± 2.5 vs 9.2 ± 1.6 years old, P=0.03) and no difference in regard to gender (P=0.14) or race/ethnicity (P=0.36) proportions (data not shown). Demographic characteristics of the IBS cohort are summarized in Table 1. Our cohort was mostly female (65.1%) (Table 1A). A range of races/ethnicities were represented.
Table 1.
Child Participant Demographics and Psychological and Abdominal Pain Characteristics
| A. Demographics | ||
| Demographics | Total Cohort (n=261) | |
| Age, mean (SD) (years old) | 10.4 (2.6) | |
| Gender Female, n (%) | 170 (65.1) | |
| Race/Ethnicity, n (%) | ||
| White, Non-Hispanic | 155 (59.4) | |
| Black, Non-Hispanic | 36 (13.8) | |
| Hispanic | 57 (21.8) | |
| Others | 13 (5.0) | |
| B. Psychological and Abdominal Pain Characteristics | ||
| Psychological and Abdominal Pain Factors | Mean (SD) Range | Z-Score Range |
| BASC-2 Child Self-Report Anxiety Scale T-Score* | 51.5 (11.0) (34 – 80) | −1.60 – 2.60 |
| BASC-2 Child Self-Report Depression Scale T-Score* | 47.8 (8.6) (40 – 86) | −0.91 – 4.45 |
| Child Self-Report Somatization Inventory Total Score | 28.5 (18.4) (0 – 104) | −1.54 – 4.10 |
| Pain Catastrophizing Z-scores** | 0.12 (0.9) (−2.38 – 2.5) | −2.38 – 2.50 |
| IBS Abdominal Pain Intensity and Frequency Composite Score | 48.0 (43.3) (2 – 224) | −1.06 – 4.06 |
Some participants BASC scale T scores were converted to BASC-2 scale T scores
This is based on either the 11-item Child Self-Reported Pain Catastrophizing Scale Z-scores or 8-item select questions from the Pain Response Inventory summed score Z-scores
BASC, Behavioral Assessment System for Children; BASC-2, Behavioral Assessment System for Children, 2nd Edition; IBS, irritable bowel syndrome
Descriptives of psychological variables and the IBS abdominal pain severity composite score are outlined in Table 1B. All variables showed wide variation, which was ideal for our planned mediation analyses (Table 1B). The bivariate correlation analysis of all psychological variables and the IBS abdominal pain severity composite Z-scores revealed significant positive correlations for all (Supplemental Table A).
Hierarchical multiple linear regression then examined how these psychological variables were associated with IBS abdominal pain using age, gender, and race/ethnicity as covariates. Model 0 demonstrated the effect of the covariates on IBS abdominal pain severity, with gender (P < 0.001) being the only significant variable in this model (Supplementary Table B). Model 1 and Model 3 illustrate that anxiety (P = 0.02) and depression (P < 0.001) were each significantly associated with IBS abdominal pain severity after adjustment for the covariates, respectively (Supplementary Table B), and these results met the required precondition to proceed with mediation analysis for both anxiety and depression and the dependent outcome of IBS abdominal pain severity. The addition of somatization and pain catastrophizing in Model 2 rendered anxiety no longer significant (Supplementary Table B). The addition of somatization and pain catastrophizing with depression did not change its statistical significance status in Model 4 (Supplementary Table B).
Meditation Analyses
We next assessed whether somatization or pain catastrophizing individually mediated the relationship between anxiety or depression and IBS abdominal pain severity (Table 2). Results revealed that both somatization (mediated standardized β 0.11) and pain catastrophizing (mediated standardized β 0.11) were each significant mediators of the relationship between anxiety and IBS abdominal pain severity (Table 2). Individual mediation analysis also revealed that both somatization (mediated standardized β 0.08) and pain catastrophizing (mediated standardized β 0.06) were significant mediators of the association between depression and IBS abdominal pain severity (Table 2).
Table 2.
Individual Mediation Analyses of Psychological Factors on IBS Abdominal Pain
| Independent Variable | Mediator | Path a β (CI) | Path b β (CI) | Path c β (CI) | Path c′ β (CI) | Mediated β (CI) |
|---|---|---|---|---|---|---|
| Anxiety | Somatization | 0.38 (0.27 – 0.50) | 0.28 (0.15 – 0.41) | 0.14 (0.02 – 0.26) | 0.03 (−0.09 – 0.16) | 0.11 (0.05 – 0.18) |
| Anxiety | Pain Catastrophizing | 0.45 (0.34 – 0.55) | 0.25 (0.11 – 0.39) | 0.14 (0.02 – 0.26) | 0.03 (−0.10 – 0.16) | 0.11 (0.05 – 0.18) |
| Depression | Somatization | 0.41 (0.31 – 0.52) | 0.18 (0.05 – 0.31) | 0.32 (0.21 – 0.43) | 0.25 (0.12 – 0.37) | 0.08 (0.02 – 0.14) |
| Depression | Pain Catastrophizing | 0.36 (0.26 – 0.47) | 0.16 (0.03 – 0.28) | 0.32 (0.21 – 0.43) | 0.27 (0.14 – 0.39) | 0.06 (0.01 – 0.11) |
β is the standardized coefficient of the specific interaction as outlined in the paths in Figure 1.
The CI in each path noted are the bootstrapping CIs with 95% confidence. Inclusion of 0 within the CI indicates statistical non-significance.
Model controlled for the covariates of age, gender, and race/ethnicity
CI, confidence interval; IBS, irritable bowel syndrome
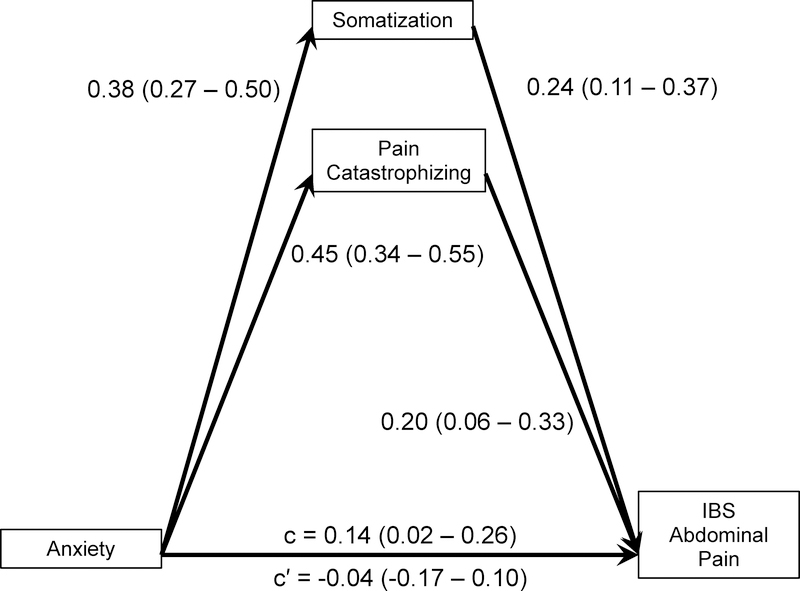
Multiple mediation analysis including both somatization and pain catastrophizing as mediators in the relationship between anxiety and IBS abdominal pain severity reinforced the findings of the previous individual mediation analyses (Figure 2). This multiple mediation model with anxiety predicting IBS abdominal pain severity indeed was mediated by both mediators and had a completely standardized mediated effect of 0.18 (95% CI 0.09 – 0.27). The mediated effect of somatization was a standardized effect of 0.09 or 51% of the total mediated effect, and the mediated effect of pain catastrophizing was 0.09 or 49% of the total mediated effect.
Figure 2. Mediation of Anxiety and Multiple Psychological Mediators on IBS Abdominal Pain by Somatization and Pain Catastrophizing.
Denotes standardized coefficients (bootstrapping 95% confidence interval) between psychological factors and/or dependent variable. Statistical significance is defined as the confidence interval not containing 0.
Model is adjusted by the covariates of age, gender, and race/ethnicity.
The indirect effect of the mediators somatization and pain catastrophizing present: 0.18 (95% CI 0.09 – 0.28).
IBS, irritable bowel syndrome
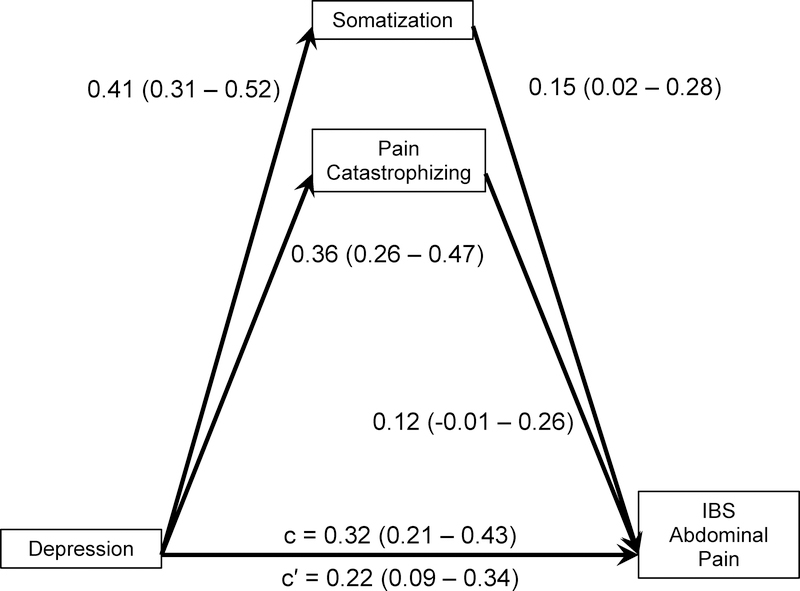
Similarly, somatization and pain catastrophizing were dual mediators of the association between depression and IBS abdominal pain severity (completely standardized mediated effect of 0.11; 95% CI 0.04 – 0.19). The mediated effect of somatization was a standardized mediated effect of 0.06 or explains 59% of the total mediated effect. As expected, pain catastrophizing accounts for the remaining standardized mediated effect of 0.05 or 41% of the total mediated effect (Figure 3).
Figure 3. Mediation of Depression and Multiple Psychological Mediators on IBS Abdominal Pain by Somatization and Pain Catastrophizing.
Denotes standardized coefficients (bootstrapping 95% confidence interval) between psychological factors and/or dependent variable. Statistical significance is defined as the confidence interval not containing 0.
Model is adjusted by the covariates of age, gender, and race/ethnicity.
The indirect effect of the mediators somatization and pain catastrophizing present in the model: 0.11 (95% CI 0.04 – 0.18).
IBS, irritable bowel syndrome
Discussion
Our study found that somatization and pain catastrophizing mediate the association between anxiety/depression and IBS abdominal pain severity in children. To our knowledge, this is the first study to examine associations of such a diverse set of psychological variables with abdominal pain severity in a well-characterized pediatric IBS patient sample. The findings may mean that the effects of anxiety and depression on IBS outcomes are indirect and through changes in somatization and pain catastrophizing. These results inform the structure of a comprehensive model explaining how multiple psychosocial measures impact symptomatology in children with IBS.
As all these psychological factors are amenable to treatment such as CBT, our findings suggest that focusing on reducing somatization and pain catastrophizing may have more direct effects on pain than reducing anxiety or depression. In fact, CBT treatment outcomes in both in adults and pediatric patients have been shown not to be explained through changes in anxiety but rather changes in pain catastrophizing (34, 62).
Our findings are in agreement with previous work by van Tilburg and colleagues in adults who found that somatization and pain catastrophizing mediate the association between anxiety and abdominal pain symptoms (29). Furthermore, a community based study in a non-clinical sample of children and adolescents, found that somatization mediated the relationships of anxiety/depression and abdominal pain (33). Williams and colleagues also reported that somatization is more strongly associated with pain severity than anxiety, although they did not test for mediation (32). Other studies suggest that these maladaptive thought processes may also effect other health outcomes in children with abdominal pain. For example, pain catastrophizing is positively associated with functional disability and maintenance of pain (63, 64). Somatization has been associated with increased medical health visits as well as pain maintenance into adulthood (65, 66). These findings support the notion that pain catastrophizing and somatization may need to be considered in the diagnoses, treatment, and management of children with IBS.
Although we have evidence that pain catastrophizing can be changed with CBT, there is limited evidence of how to reduce somatization in either children or adults with IBS. Given the importance of both pain catastrophizing and somatization, there is a clear need to develop better efficacious treatments to reduce these maladaptive factors in affected children.
Limitations of this study includes the inability to determine causation based on the cross sectional nature of our data. The study outcome is a composite value of abdominal pain frequency and intensity thus we are not able to determine which pain characteristic is the key determinate of our observed results. However, there is lack of consensus whether abdominal pain frequency or intensity should be the primary pain outcome for IBS clinical trials (67, 68). In addition, the pain catastrophizing variable utilized was based on two separate methodologies and a universal score based on the respective instrument’s Z score. Nonetheless, the two instruments utilized were derived from validated instruments with similar questions and they both capture similar related information. The strength of this study is the ability to analyze multiple pertinent psychological measurements concurrently in a large group of children with IBS. In addition, we utilized a well-characterized IBS cohort.
In conclusion, our study illustrates the importance of evaluating and treating somatization and pain catastrophizing to improve abdominal pain symptomatology in children with IBS. More research is needed to determine how to best address these psychological factors in affected children to optimize psychological treatment efficacy and minimize IBS abdominal pain severity.
Supplementary Material
Key Points.
Anxiety, depression, somatization, and pain catastrophizing are associated with abdominal pain in children with irritable bowel syndrome (IBS). The interrelationships among these psychological conditions are unclear. Understanding how these factors are related may be important for the development of psychological treatments.
We discovered that both somatization and pain catastrophizing, individually and combined, mediate the individual associations between anxiety/depression and IBS abdominal pain.
Identifying and clinically treating somatization and pain catastrophizing in children with IBS may improve abdominal pain outcomes.
Acknowledgements
This work was supported by NIH R01 NR05337 and NR013497 (RJS), RC2 NR011959 (RJS and MH), the US Department of Agriculture/ARS under Cooperative Agreement 6250-51000-043 (RJS), and NIH P30 DK056338 which supports the Texas Medical Center Digestive Diseases Center. The contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement from the US Government.
Abbreviations
- IBS
irritable bowel syndrome
- BASC
Behavior Assessment System for Children
- BASC-2
Behavior Assessment System for Children, 2nd edition
- CSI
Child Somatization Inventory
- PCS-C
pain catastrophizing scale-child self-report
- PRI
Pain Response Inventory
Footnotes
Disclosures
There are no conflicts of interest to report.
Literature Cited
- 1.Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Functional Disorders: Children and Adolescents. Gastroenterology 2016. [DOI] [PubMed] [Google Scholar]
- 2.Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 2006; 130: 1527–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korterink JJ, Diederen K, Benninga MA, Tabbers MM. Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PloS one 2015; 10: e0126982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apley J, Hale B. Children with recurrent abdominal pain: how do they grow up? British medical journal 1973; 3: 7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christensen MF, Mortensen O. Long-term prognosis in children with recurrent abdominal pain. Archives of disease in childhood 1975; 50: 110–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magni G, Pierri M, Donzelli F. Recurrent abdominal pain in children: a long term follow-up. European journal of pediatrics 1987; 146: 72–74. [DOI] [PubMed] [Google Scholar]
- 7.Miele E, Simeone D, Marino A, et al. Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics 2004; 114: 73–78. [DOI] [PubMed] [Google Scholar]
- 8.Walker LS, Guite JW, Duke M, Barnard JA, Greene JW. Recurrent abdominal pain: a potential precursor of irritable bowel syndrome in adolescents and young adults. The Journal of pediatrics 1998; 132: 1010–1015. [DOI] [PubMed] [Google Scholar]
- 9.Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology 2002; 122: 1500–1511. [DOI] [PubMed] [Google Scholar]
- 10.Campo JV, Di Lorenzo C, Chiappetta L, et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics 2001; 108: E1. [DOI] [PubMed] [Google Scholar]
- 11.Di Lorenzo C, Youssef NN, Sigurdsson L, Scharff L, Griffiths J, Wald A. Visceral hyperalgesia in children with functional abdominal pain. The Journal of pediatrics 2001; 139: 838–843. [DOI] [PubMed] [Google Scholar]
- 12.Kuttner L, Chambers CT, Hardial J, Israel DM, Jacobson K, Evans K. A randomized trial of yoga for adolescents with irritable bowel syndrome. Pain research & management : the journal of the Canadian Pain Society = journal de la societe canadienne pour le traitement de la douleur 2006; 11: 217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saps M, Youssef N, Miranda A, et al. Multicenter, randomized, placebo-controlled trial of amitriptyline in children with functional gastrointestinal disorders. Gastroenterology 2009; 137: 1261–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waters AM, Schilpzand E, Bell C, Walker LS, Baber K. Functional gastrointestinal symptoms in children with anxiety disorders. Journal of abnormal child psychology 2013; 41: 151–163. [DOI] [PubMed] [Google Scholar]
- 15.Walter SA, Jones MP, Talley NJ, et al. Abdominal pain is associated with anxiety and depression scores in a sample of the general adult population with no signs of organic gastrointestinal disease. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society 2013; 25: 741–e576. [DOI] [PubMed] [Google Scholar]
- 16.Jamil O, Sarwar S, Hussain Z, Fiaz RO, Chaudary RD. Association Between Functional Dyspepsia and Severity of Depression. J Coll Physicians Surg Pak 2016; 26: 513–516. [PubMed] [Google Scholar]
- 17.Van Oudenhove L, Tornblom H, Storsrud S, Tack J, Simren M. Depression and Somatization Are Associated With Increased Postprandial Symptoms in Patients With Irritable Bowel Syndrome. Gastroenterology 2016; 150: 866–874. [DOI] [PubMed] [Google Scholar]
- 18.Endo Y, Shoji T, Fukudo S, et al. The features of adolescent irritable bowel syndrome in Japan. Journal of gastroenterology and hepatology 2011; 26 Suppl 3: 106–109. [DOI] [PubMed] [Google Scholar]
- 19.Son YJ, Jun EY, Park JH. Prevalence and risk factors of irritable bowel syndrome in Korean adolescent girls: a school-based study. Int J Nurs Stud 2009; 46: 76–84. [DOI] [PubMed] [Google Scholar]
- 20.Dong L, Dingguo L, Xiaoxing X, Hanming L. An epidemiologic study of irritable bowel syndrome in adolescents and children in China: a school-based study. Pediatrics 2005; 116: e393–396. [DOI] [PubMed] [Google Scholar]
- 21.Park H, Lim S. Frequency of irritable bowel syndrome, entrance examination-related stress, mental health, and quality of life in high school students. Gastroenterology nursing : the official journal of the Society of Gastroenterology Nurses and Associates 2011; 34: 450–458. [DOI] [PubMed] [Google Scholar]
- 22.Neuendorf R, Harding A, Stello N, Hanes D, Wahbeh H. Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review. Journal of psychosomatic research 2016; 87: 70–80. [DOI] [PubMed] [Google Scholar]
- 23.Bakshi N, Lukombo I, Shnol H, Belfer I, Krishnamurti L. Psychological Characteristics and Pain Frequency Are Associated With Experimental Pain Sensitivity in Pediatric Patients With Sickle Cell Disease. The journal of pain : official journal of the American Pain Society 2017; 18: 1216–1228. [DOI] [PubMed] [Google Scholar]
- 24.Huguet A, Tougas ME, Hayden J, et al. Systematic Review of Childhood and Adolescent Risk and Prognostic Factors for Recurrent Headaches. The journal of pain : official journal of the American Pain Society 2016; 17: 855–873 e858. [DOI] [PubMed] [Google Scholar]
- 25.Shelby GD, Shirkey KC, Sherman AL, et al. Functional abdominal pain in childhood and long-term vulnerability to anxiety disorders. Pediatrics 2013; 132: 475–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 2004; 113: 817–824. [DOI] [PubMed] [Google Scholar]
- 27.Cunningham NR, Nelson S, Jagpal A, et al. Development of the Aim to Decrease Anxiety and Pain Treatment for Pediatric Functional Abdominal Pain Disorders. Journal of pediatric gastroenterology and nutrition 2018; 66: 16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Gontard A, Moritz AM, Thome-Granz S, Equit M. Abdominal pain symptoms are associated with anxiety and depression in young children. Acta paediatrica 2015; 104: 1156–1163. [DOI] [PubMed] [Google Scholar]
- 29.van Tilburg MA, Palsson OS, Whitehead WE. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. Journal of psychosomatic research 2013; 74: 486–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palermo TM, Krell H, Janosy N, Zeltzer LK. CHAPTER 21 - Pain and Somatoform Disorders In: Wolraich ML, Drotar DD, Dworkin PH, Perrin EC, eds. Developmental-Behavioral Pediatrics. Philadelphia: Mosby, 2008: 711–741. [Google Scholar]
- 31.Leung L Pain catastrophizing: an updated review. Indian J Psychol Med 2012; 34: 204–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams AE, Czyzewski DI, Self MM, Shulman RJ. Are child anxiety and somatization associated with pain in pain-related functional gastrointestinal disorders? Journal of health psychology 2015; 20: 369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lavigne JV, Saps M, Bryant FB. Models of anxiety, depression, somatization, and coping as predictors of abdominal pain in a community sample of school-age children. Journal of pediatric psychology 2014; 39: 9–22. [DOI] [PubMed] [Google Scholar]
- 34.Levy RL, Langer SL, Romano JM, et al. Cognitive mediators of treatment outcomes in pediatric functional abdominal pain. The Clinical journal of pain 2014; 30: 1033–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shulman RJ, Eakin MN, Jarrett M, Czyzewski DI, Zeltzer LK. Characteristics of pain and stooling in children with recurrent abdominal pain. Journal of pediatric gastroenterology and nutrition 2007; 44: 203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shulman RJ, Öhman L, Stridsberg M, Cain K, Simrén M, Heitkemper M. Evidence of Increased Fecal Granins in Children with Irritable Bowel Syndrome and Correlates with Symptoms. Neurogastroenterology and Motility in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jarrett ME, Han CJ, Cain KC, et al. Relationships of abdominal pain, reports to visceral and temperature pain sensitivity, conditioned pain modulation, and heart rate variability in irritable bowel syndrome. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society 2016; 28: 1094–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shulman RJ, Hollister EB, Cain K, et al. Psyllium Fiber Reduces Abdominal Pain in Children With Irritable Bowel Syndrome in a Randomized, Double-Blind Trial. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 2017; 15: 712–719 e714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lane MM, Czyzewski DI, Chumpitazi BP, Shulman RJ. Reliability and validity of a modified Bristol Stool Form Scale for children. The Journal of pediatrics 2011; 159: 437–441 e431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.von Baeyer CL, Spagrud LJ, McCormick JC, Choo E, Neville K, Connelly MA. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain 2009; 143: 223–227. [DOI] [PubMed] [Google Scholar]
- 41.Ragnarsson G, Bodemar G. Division of the irritable bowel syndrome into subgroups on the basis of daily recorded symptoms in two outpatients samples. Scandinavian journal of gastroenterology 1999; 34: 993–1000. [DOI] [PubMed] [Google Scholar]
- 42.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology 2006; 130: 1480–1491. [DOI] [PubMed] [Google Scholar]
- 43.Czyzewski DI, Lane MM, Weidler EM, Williams AE, Swank PR, Shulman RJ. The interpretation of Rome III criteria and method of assessment affect the irritable bowel syndrome classification of children. Alimentary pharmacology & therapeutics 2011; 33: 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Laird KT, Sherman AL, Smith CA, Walker LS. Validation of the Abdominal Pain Index using a revised scoring method. Journal of pediatric psychology 2015; 40: 517–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walker LS, Smith, Craig A,Judy Garber,Van Slyke, Deborah A. Development and validation of the pain response inventory for children. Psychological Assessment 1997; 9: 392–405. [Google Scholar]
- 46.Hubbard CS, Becerra L, Heinz N, et al. Abdominal Pain, the Adolescent and Altered Brain Structure and Function. PloS one 2016; 11: e0156545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van der Veek SM, Derkx BH, Plak RD, et al. Attentional bias to activity of different parts of the body in children with functional abdominal pain: an experimental study. Journal of pediatric psychology 2014; 39: 438–449. [DOI] [PubMed] [Google Scholar]
- 48.van der Veek SM, Derkx HH, de Haan E, Benninga MA, Boer F. Abdominal pain in Dutch schoolchildren: relations with physical and psychological comorbid complaints in children and their parents. Journal of pediatric gastroenterology and nutrition 2010; 51: 481–487. [DOI] [PubMed] [Google Scholar]
- 49.van der Veek SM, Derkx HH, de Haan E, Benninga MA, Boer F. Emotion awareness and coping in children with functional abdominal pain: a controlled study. Social science & medicine 2012; 74: 112–119. [DOI] [PubMed] [Google Scholar]
- 50.van Tilburg MA, Chitkara DK, Palsson OS, et al. Audio-recorded guided imagery treatment reduces functional abdominal pain in children: a pilot study. Pediatrics 2009; 124: e890–897. [DOI] [PubMed] [Google Scholar]
- 51.Reynolds CR, Kamphaus RW. Behavior Assessment System for Children manual. Circle Pines, MN: American Guidance Service, 1998. [Google Scholar]
- 52.Reynolds CR, Kamphaus RW. BASC-2: Behavior Assessment System for Children Second Edition Manual. Circle Pines, MN: AGS Publishing, 2004. [Google Scholar]
- 53.Walker LS, Beck JE, Garber J, Lambert W. Children’s Somatization Inventory: psychometric properties of the revised form (CSI-24). Journal of pediatric psychology 2009; 34: 430–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sullivan MJL. The Pain Catastrophizing Scale: User Manual. Montreal, Quebec: McGill University, 2009. [Google Scholar]
- 55.Stone AL, Walker LS, Laird KT, Shirkey KC, Smith CA. Pediatric Pain Beliefs Questionnaire: Psychometric Properties of the Short Form. The journal of pain : official journal of the American Pain Society 2016; 17: 1036–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Crombez G, Bijttebier P, Eccleston C, et al. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain 2003; 104: 639–646. [DOI] [PubMed] [Google Scholar]
- 57.Pielech M, Ryan M, Logan D, Kaczynski K, White MT, Simons LE. Pain catastrophizing in children with chronic pain and their parents: Proposed clinical reference points and reexamination of the Pain Catastrophizing Scale measure. PAIN® 2014; 155: 2360–2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stone AL, Walker LS, Laird KT, Shirkey KC, Smith CA. Pediatric Pain Beliefs Questionnaire: Psychometric Properties of the Short Form. The Journal of Pain; 17: 1036–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the Pain Response Inventory for children. Psychological Assessment 1997; 9: 392–405. [Google Scholar]
- 60.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol 2007; 58: 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hayes AF. Introduction to mediation, moderation, and conditional process analysis : a regression-based approach. Second edn. New York: Guilford Press, 2018. [Google Scholar]
- 62.Chilcot J, Moss-Morris R. Changes in illness-related cognitions rather than distress mediate improvements in irritable bowel syndrome (IBS) symptoms and disability following a brief cognitive behavioural therapy intervention. Behaviour research and therapy 2013; 51: 690–695. [DOI] [PubMed] [Google Scholar]
- 63.Langer SL, Romano JM, Levy RL, Walker LS, Whitehead WE. Catastrophizing and Parental Response to Child Symptom Complaints. Children’s health care : journal of the Association for the Care of Children’s Health 2009; 38: 169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain 2012; 153: 1798–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Horst S, Shelby G, Anderson J, et al. Predicting persistence of functional abdominal pain from childhood into young adulthood. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 2014; 12: 2026–2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou H, Li D, Cheng G, Fan J, Lu H. An epidemiologic study of irritable bowel syndrome in adolescents and children in South China: a school-based study. Child: care, health and development 2010; 36: 781–786. [DOI] [PubMed] [Google Scholar]
- 67.Saps M, van Tilburg MA, Lavigne JV, et al. Recommendations for pharmacological clinical trials in children with irritable bowel syndrome: the Rome foundation pediatric subcommittee on clinical trials. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society 2016; 28: 1619–1631. [DOI] [PubMed] [Google Scholar]
- 68.Administration USDoHaHSFaD. Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. 2009. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.