Abstract
Background
Clinicians are expected to screen their adolescent patients for an increasing number of health behaviors and intervene when they uncover risky behaviors, yet, the clinic time allotted to screen, intervene, and provide resources is insufficient. Brief motivational interviewing (MI) offers succinct behavior change counseling; however, for implementation, clinicians need training, skill, and time. Computerized screening and counseling adjuvants may help clinicians increase their scope of behavioral screening, especially with sensitive topics such as sexual health, and provide risk-reduction interventions without consuming provider time during visits.
Objective
The objectives of this study were to (1) understand the extent to which health care providers use brief MI for sexual health discussions with adolescent patients and (2) assess the acceptability of incorporating a brief MI-based intervention to reduce sexual risk behaviors into their clinical practice delivered by either themselves or a computer.
Methods
At a national medical conference, surveys were administered to clinicians who provide sexual health care to adolescents. They were asked about their current use of MI for sexual risk behavior discussions and their willingness to implement computerized sexual health screening and computerized sexual risk behavior interventions into their clinical practice.
Results
The large majority (87.6%, 170/194) of clinicians already used MI with their patients with less than half (72/148, 48.6%) reporting they had been formally trained in MI. Despite all (195/195, 100.0%) clinicians feeling very or completely comfortable discussing sexual risk behaviors with their patients, the large majority (160/195, 82.1%) reported it would be useful, very useful, or extremely useful for a computerized program to do it all: screen their patients, generate risk profiles, and provide the risk-reduction counseling rather than doing it themselves.
Conclusions
In this study, most clinicians used some form of brief MI or client-centered counseling when discussing sexual risk behaviors with adolescents and are very comfortable doing so. However, the large majority would prefer to implement computerized sexual health screening, risk assessment, and sexual risk behavior interventions into their clinical care of adolescents.
Keywords: sexual health, risk behaviors, adolescent, healthcare providers, computer-assisted diagnosis, teen health, preventive care
Introduction
Background
Clinician sexual health discussions with adolescents remain suboptimal in real-world clinical practice [1-4]. Health care providers continue to search for optimal ways to communicate with adolescents about sexual health and risk behaviors. Some behavioral interventions have been shown to increase the knowledge of risk-reduction strategies (eg, condom and birth control use and negotiating safe sex with partners) and decrease self-reported unprotected sex; however, these interventions were tested in nonclinical settings and with specific populations of adolescents. Such interventions have yet to be tested or implemented in real-world outpatient settings and delivered by clinicians [5-9].
Barriers to Screening
Even experienced clinicians in busy practices may not have the time to engage adolescents in discussions, which are needed to build rapport and uncover risk behaviors. Adolescents may have concerns about talking face-to-face with clinicians about sex or may not be granted enough time for confidential conversations during their visit [10-12]. Brief motivational interviewing (MI) has gained popularity as a means to engage adolescents in behavior change [13-20]; however, there are barriers to clinicians in adopting MI. It takes time to be trained and become proficient in MI, and effectively using MI requires already precious clinic visit time [21-22].
Computer-Assisted Screening
Computerized screening with brief MI may serve to alleviate the time burden for health care providers and any discomfort in discussing sensitive health topics for both the clinician and patient. Computer screening improves adolescents’ perceptions of medical visits [23-25]. The literature provides evidence that adolescents may prefer computerized sexual health screening to face-to-face interviews. A study of adolescents seeking care in a pediatric emergency department tested computerized sexual health screening and found that it was acceptable to adolescents, preferable to in-person interviews, and feasible for providers to implement in the emergency department [26]. A personal digital assistant screening tool that screened for several risk behaviors, including unprotected sex, was tested in primary care clinics before adolescent well visits and resulted in higher patient ratings for visit satisfaction, perceived confidentiality, and feeling listened to carefully [23].
Computerized Interventions
Incorporating sexual behavior risk-reduction interventions into the computerized screening session takes these interventions one step further. Such interventions may be interactive and provide personalized feedback to the adolescent. Only a few computerized sexual health interventions for adolescents have been tested in real-world clinic settings, and these did not assess clinician acceptability of integrating the interventions into clinical practice [27-30]. Existing provider acceptability studies of computerized health screening and interventions are of adult patient populations, have small sample sizes, and may not include sexual health as a risk behavior [31-33]. We are not aware of any large studies assessing clinician willingness to be trained in brief MI for promoting adolescent sexual health. We were likewise unable to identify any studies assessing provider acceptability of incorporating computerized sexual health screening and interventions into visits with their adolescent patients. The objectives of this study were (1) to understand the extent to which health care providers use MI for sexual health with adolescent patients and (2) to assess the acceptability of incorporating a brief MI-based intervention to reduce sexual risk behaviors into their clinical practice delivered by either themselves or a computer.
Methods
Recruitment
In March 2009, we administered a 28-item survey to clinicians at a national medical conference, with attendees representing a wide geographic range in the United States. For the purposes of this study, clinicians were asked about sexually transmitted infection (STI) testing and positive STI diagnoses in the past 3 months to characterize their patient population and practice experience. The inclusion criteria were clinicians practicing in the United States who provided sexual and reproductive health care to adolescents. The exclusion criteria were not providing such care to adolescents or being in training. A total of 365 surveys were initially distributed and 18 were omitted from the final denominator (n=347) for the following reasons: the attendee returned the survey blank (n=8); the survey was lost by the participant and a replacement survey was provided (n=8); or the survey was defective because of printing error and was replaced with a corrected survey (n=2). Of the 347 surveys distributed, 81.8% (284/347) were completed. The University of Washington Human Subjects Division approved this study.
Sample for Analysis
Of the 284 completed surveys, an additional 88 were ineligible because the attendee was in training (n=45), practicing outside the United States (n=10), not providing sexual and reproductive healthcare or not in practice or nonclinical (n=30), or did not indicate their degree or level of training (n=3). A total of 196 clinicians qualified for the study as they provided such care to adolescents, including the diagnosis and management of STIs and unintended pregnancy; identified themselves as medical doctor (MD)/doctor of osteopathy (DO), physician assistant (PA), or nurse practitioner (NP) and were not currently in training (Figure 1). STATA 11.0 by StataCorp LLC, was used for data analysis. T tests and chi-square tests were used to evaluate associations.
Figure 1.
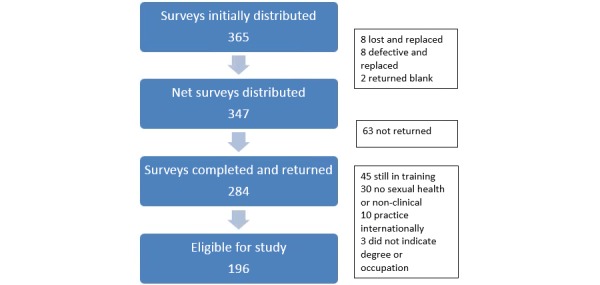
Flow diagram of sample for analysis.
Results
Demographic and Clinical Practice Characteristics
Physicians (MDs and DOs) comprised the majority of the sample (181/196, 92.3%), with (13/196, 6.6%) NPs and (2/196, 1.0%) PAs. In addition, 65.3% (128/196) of them were female. The most common practice type was academic (121/196, 61.7%) with a comparable proportion in private practice (19/196, 9.6%) and public health/community clinics (18/196, 9.2%). Over half (118/195, 60.1%) of the clinicians provided care only to adolescents (defined as ages 11 to 21 years). The number of years providers reported being in clinical practice ranged from less than 1 year to greater than 30 years and was evenly distributed across decades of practice. Through the use of Likert scales, we elicited information about clinical practice and patient population characteristics. The large majority (175/196, 89.3%) of clinicians provided care to 10 or more patients in a typical week. In the past 3 months, the majority (160/195, 82.1%) of clinicians tested 10 or more of their patients for STIs (Neisseria gonorrhoeae, Chlamydia trachomatis, trichomonas, genital warts, syphilis, and HIV) with the vast majority (178/196, 90.8%) of clinicians reporting 1 or more adolescents testing positive for an STI in the same time period (Table 1).
Table 1.
Demographic characteristics of clinicians (N=196).
| Demographic characteristic | Statistics, n (%) | |
| Gender | ||
| Female | 128 (65.3) | |
| Male | 68 (34.7) | |
| Clinician type | ||
| Medical doctor | 181 (92.4) | |
| Nurse practitioner/physician assistant | 15 (7.6) | |
| Years in clinical practice (N=193), n (%) | ||
| ≤10 | 67 (34.7) | |
| 11-20 | 64 (33.2) | |
| >20 | 62 (32.1) | |
| Patient type (N=195), n (%) | ||
| Adolescents only (aged 11-21 years) | 118 (60.5) | |
| Children and adolescents (aged 0-21 years) | 30 (15.4) | |
| All ages (0 through adulthood) | 19 (9.7) | |
| Adolescents and adults (aged 11 years through adult) | 28 (14.4) | |
| Practice type (N=195), n (%) | ||
| Academic | 121 (62.0) | |
| Private | 20 (10.3) | |
| Community/public health | 23 (11.8) | |
| Other | 31 (15.9) | |
| Adolescent patients per week | ||
| <10 | 21 (10.7) | |
| 10-29 | 87 (44.4) | |
| ≥30 | 88 (44.9) | |
| STIa tests on patients per 3 months (N=195), n (%) | ||
| <10 | 35 (17.9) | |
| 10-29 | 59 (30.2) | |
| ≥30 | 101 (51.9) | |
| Positive STIa tests per 3 months | ||
| <10 | 123 (62.7) | |
| 10-29 | 55 (28.1) | |
| ≥30 | 18 (9.2) | |
aSTI: sexually transmitted infection, including chlamydia, gonorrhea, trichomonas, herpes, genital warts, syphilis, and HIV.
Current Use of Motivational Interviewing in Clinical Practice
All clinicians reported that they felt at least very comfortable and a large majority felt completely comfortable (195/195, 100.0%; missing date, n=1) discussing sexual risk behaviors (eg, inconsistent or lack of condom use/hormonal birth control; multiple partners/concurrency; HIV/STI; unintended pregnancy) with their patients. Although all except 3 clinicians reported feeling that they were at least somewhat effective in changing sexual risk behaviors of their adolescent patients, only 22.1% (43/195) felt very or completely effective. Many clinicians reported they saw themselves as more effective at changing patient behaviors than other clinicians.
The vast majority of clinicians were familiar with MI defined in the survey as “… a directive, client-centered counseling style for eliciting behavior change by helping to explore and resolve ambivalence” [34]. The large majority of clinicians (170/194, 87.6%) already used MI with their patients. These 170 clinicians were asked if they were formally trained in MI and of 148 (missing data=22) respondents, less than half, 48.6% (72/148), reported formal training. Clinicians reported having used MI for many health topics, including obesity (93%), smoking (90%), alcohol (82%), substance abuse (87%), and sexual health (96%). Only half (52%) of the clinicians said they used it to discuss injury prevention (bike helmets/seat belts). Most clinicians (140/170, 82.4%) employ MI greater than half the time when discussing sexual health with their patients and feel they are more effective in communicating with their patient when they use MI compared with when they do not (Table 2).
Table 2.
Clinician perspective of sexual risk behaviors and motivational interviewing (MI; N=196).
| Clinician perspectives | Statistics, n (%) | |
| Comfort talking about sexual risk behaviorsa (N=195), n (%) | ||
| Not comfortable | 0 (0) | |
| Somewhat comfortable | 0 (0) | |
| Comfortable | 0 (0) | |
| Very comfortable | 27 (13.8) | |
| Completely comfortable | 168 (86.2) | |
| Clinician effectiveness in changing sexual risk behaviors (N=194), n (%) | ||
| Not effective | 8 (4.1) | |
| Somewhat effective | 89 (45.9) | |
| Effective | 68 (35.0) | |
| Very effective | 29 (15.0) | |
| Completely effective | 0 (0) | |
| Personal effectiveness in changing behavior (N=195), n (%) | ||
| Not effective | 3 (1.5) | |
| Somewhat effective | 76 (39.0) | |
| Effective | 73 (37.5) | |
| Very effective | 42 (21.5) | |
| Completely effective | 1 (0.5) | |
| Use of MI with patient | ||
| Yes | 170 (87.6) | |
| No | 24 (12.4) | |
| Formally trained in MI (N=170)a,b (n=148), n (%) | ||
| Yes | 72 (48.6) | |
| No | 76 (51.4) | |
| Types of behavioral issues addressed | ||
| Sexual risk behavior | 163 (96.4) | |
| Obesity | 155 (92.8) | |
| Smoking cigarettes | 147 (89.6) | |
| Drinking alcohol | 133 (82.1) | |
| Substance abuse | 140 (87.0) | |
| Injury prevention (bike helmets/seat belts) | 83 (52.2) | |
| Frequency of use of MI with patients for sexual risk behavior | ||
| Never | 2 (1.2) | |
| 25% of time | 28 (16.5) | |
| 50% of time | 41 (24.1) | |
| 75% of time | 53 (31.2) | |
| Almost always | 46 (27.0) | |
| Provider effectiveness in changing behavior when using MI versus when not (N=163), n (%) | ||
| Much less effective | 1 (0.6) | |
| Somewhat less effective | 4 (2.4) | |
| No difference | 22 (13.5) | |
| More effective | 120 (73.6) | |
| Much more effective | 16 (9.8) | |
aNo difference by number practice years or frequency sexually transmitted infection testing.
bRemaining survey questions only asked if ever used motivational interviewing, n=170.
Motivational Interviewing Acceptability and Feasibility in Practice
The vast majority of clinicians would be willing to use MI or another type of client-centered counseling technique in their practice, if effective at reducing sexual risk behaviors in adolescents. Although 93% of them were willing to attend training for such an intervention, they preferred the length of training be limited to less than 1 day. Clinicians are willing to spend a maximum of 10 min per patient to deliver the intervention. Approximately half the clinicians (103/195, 52.8%) were willing to have follow-up contact with their patients as part of the sexual health intervention. However, 21.0% (41/195) of them would only do so if reimbursed. Clinicians were willing to do at least 1 monthly follow-up with their patients lasting less than 10 min per encounter. Preferred modes of follow-up in order of preference were telephone, email, text message, and social media (Table 3).
Table 3.
Clinician perspective of self-delivered motivational interviewing (MI).
| Clinician perspective | Statistics | |
| Willing to attend MI training (N=186), n (%) | ||
| Yes | 174 (93.6) | |
| No | 12 (6.4) | |
| Maximum length training (N=177), n (%) | ||
| ≤2 hours | 22 (12.4) | |
| Half day | 58 (32.8) | |
| 1 day | 54 (30.5) | |
| ≥2 days | 43 (24.3) | |
| Maximum length of MI session with patient (N=192), n (%) | ||
| ≤5 min | 16 (8.3) | |
| 5 min | 62 (32.3) | |
| 10 min | 67 (34.9) | |
| 15 min | 30 (15.6) | |
| ≥20 min | 17 (8.9) | |
| Feasible for clinician follow-up with patient (N=195), n (%) | ||
| Yes | 103 (52.8) | |
| No | 51 (26.2) | |
| Only if reimbursed | 41 (21.0) | |
| Maximum length of MI follow-up session (N=152), n (%) | ||
| ≤5 min | 99 (65.1) | |
| 10 min | 31 (20.4) | |
| 15 min | 12 (7.9) | |
| ≥20 min | 10 (6.6) | |
| Maximum number of monthly follow-up contacts (N=158), n (%) | ||
| 1 | 30 (19.0) | |
| 2 | 39 (24.7) | |
| 3 | 23 (14.6) | |
| 4-5 | 29 (18.3) | |
| 6 | 37 (23.4) | |
| Follow-up method willing to use, n/N (%) | ||
| Phone call | 122/149 (81.9) | |
| Text message | 90/144 (62.5) | |
| 124/149 (83.2) | ||
| Social media | 30/139 (21.6) | |
Computer-Delivered Risk-Reduction Acceptability
The large majority of clinicians (165/192, 85.9%) found it more feasible for a computer to provide the sexual risk behavior screening intervention to their patients rather than themselves and would use a computer-generated sexual risk profile printout to facilitate discussion with their patients. The large majority of clinicians (160/195, 82.1%) also thought it would be useful, very useful, or extremely useful for the computer do it all: screen their patient, generate their sexual risk profile, and provide the risk-reduction counseling itself, requiring the provider to review only the findings with their patients afterward.
Preference for Computerized Risk Screening and Risk-Reduction Counseling
No associations were found when comparing the number of years in clinical practice and comfort discussing sexual risk behaviors with adolescents; being trained in MI; or preferring computerized sexual risk screening and risk-reduction counseling. There was also no association between preference for computerized risk screening and counseling by clinician gender, type of practice, number of patients seen per week, and number of patients tested or testing positive for an STI in the past 3 months (Table 4).
Table 4.
Clinician perspective of motivational interviewing (MI) and computer-delivered risk reduction for sexual health (N=196).
| Clinician perspective | Statistics, n (%) | |
| If MI sexual behavior risk reduction effectively delivered via clinician would it be feasible for you to do yourself?a,b | ||
| Yes | 183 (95.8) | |
| No | 8 (4.2) | |
| If sexual behavior risk reduction effectively delivered via computer would that be more feasible for you than doing it yourself?b,c | ||
| Yes | 165 (85.9) | |
| No | 27 (14.1) | |
| Likeliness to use computer printout of sexual risk behavior profile to facilitate risk-reduction counseling | ||
| Not likely | 8 (4.1) | |
| Somewhat likely | 34 (17.3) | |
| Likely | 59 (30.1) | |
| Very likely | 68 (34.7) | |
| Extremely likely | 27 (13.8) | |
| How useful would it be for you if computer generated a printout of sexual risk behavior profile AND provided risk-reduction counseling requiring you to do nothing further OR to simply review the findings with your adolescent patients?b,d | ||
| Not useful | 7 (3.6) | |
| Somewhat useful | 28 (14.4) | |
| Useful | 53 (27.2) | |
| Very useful | 59 (30.3) | |
| Extremely useful | 48 (24.6) | |
an=191.
bNo difference by number of years in clinical practice or frequency of sexually transmitted infection testing.
cn=192.
dn=195.
Discussion
Principal Findings
In a survey of clinicians who provide sexual health care to adolescents from varied geographic regions around the United States and a wide range of clinical experience, the vast majority reported being very comfortable discussing sexual health with their adolescent patients. The majority of clinicians reported using MI for sexual health counseling with their patients, although less than half of these reported formally training in MI. Surprisingly, this sample of clinicians espousing such comfort with adolescent sexual health discussions reported that it would be preferable for a computer to do it all: screen for sexual risk behaviors and provide their patients with risk-reduction counseling.
Comparison With Previous Work
There has been increasing focus on sexual health screening and MI in medical school curricula over the past 2 decades [35-40]. Other studies have found younger clinicians to be more comfortable discussing sexual health and using MI for behavior change as compared with older providers [41,3,1]. However, in this survey, providers with more than 30 years of clinical experience were just as likely as those with less than 10 years of clinical experience to report comfort in talking about sexual health and using MI with patients. The similarity in comfort across respondents with different practice longevity could be because of most clinicians in the study primarily taking care of adolescents and so were comfortable with the population. Also most clinicians were in academic practice, and may be early adopters of evolving clinical practice approaches over the years.
Most providers felt they were at least somewhat effective at influencing the sexual behavior of their patients. This sentiment echoes a qualitative study, with physicians reporting they had influence in the choice of contraception with their female patients [42]. In our study, most respondents considered themselves more effective when using MI than when not, and the majority of them considered themselves more effective at encouraging patients’ behavior change compared with other clinicians. Although there were no studies found in the literature that addressed providers’ perceptions of their effectiveness with MI, there are existing studies that demonstrate clinician use of MI for behavior change to be efficacious in changing health risk behaviors [13-18].
Although respondents were very comfortable discussing sex with adolescents and even felt they were effective at eliciting behavior change, they considered it more feasible for a computer to administer the screening and counseling rather than doing so themselves. To our knowledge, this finding is novel in the literature. For this population of providers, preferring a computerized approach to sexual health risk-reduction counseling may reflect time limitations for patient visits rather than reticence to discuss sexual health. Most providers were willing to be trained in an MI sexual risk behavior intervention that includes at least 1 follow-up session; however, 20% of providers indicated they would only do a follow-up session with patients if they were reimbursed, which may also reflect increasing pressures on clinicians for productivity.
Limitations
A limitation of this study is that we did not define MI in detail or what is required for training and proficiency in true MI. In the survey, we defined MI as “… a directive, client-centered counseling style for eliciting behavior change by helping clients explore and resolve ambivalence” [34]. It is possible that participants have different definitions for and experience in the use of MI, which may have biased the responses to questions about the use of and training in MI. In addition, the proposed computerized screening and intervention was theoretical, so clinicians were not providing feedback on a tangible product for which they may have different opinions. As most clinicians practiced in academic settings, the findings may not be generalizable to clinicians in other practice types. The decision was made to focus on clinicians practicing in the United States to account for the large variation worldwide in attitudes toward adolescent sexual and reproductive health and clinical practice. The authors acknowledge that this was a missed opportunity to learn about international clinician practice.
MI has gained increasing popularity over the past decade since this study. Brief MI is used for many different health behaviors, and we anticipate an even higher acceptability by medical providers. However, the issue of lack of provider time with patients has also escalated over the past decade. These data are relevant as providers have not yet found an answer and continue to strategize on how they can provide comprehensive health care in the limited minutes they have for adolescent patient visits. Such an intervention as presented in this study is a possible solution.
Conclusions
Clinicians are increasingly pressed for time when providing care to patients and researchers and practitioners have not yet found the most effective way to consistently discuss sexual health with adolescents or promote healthy sexual behaviors. Computerized interventions, which incorporate both behavioral screening and risk-reduction counseling, may provide solutions to both issues. The development of computerized health interventions is a rapidly growing field and further research is needed to create and test such interventions in real-world clinical practice.
Acknowledgments
The authors would like to acknowledge the Funding Agency: Eunice Kennedy Shriver National Institute of Child Health and Human Development NICHD Grant No: 5K23HD052621, eGC1 Number: A66661; Project Title: Brief Clinician Intervention for High-Risk Behaviors in Adolescents, Grant Principal Investigator: TS; Project Period Dates: 7/1/07-5/31/13. All of those who have contributed significantly to this study are listed. This study was presented as a poster: TS, DMM, MRG, and KKH. “Acceptability to health care providers of using motivational interviewing delivered via clinician or computer in clinical practice to reduce sexual risk behaviors in adolescents,” at the 2013 Annual Meeting of the Society for Adolescent Health and Medicine, Atlanta, Georgia March 2013.
Abbreviations
- DO
doctor of osteopathy
- MD
medical doctor
- MI
motivational interviewing
- NP
nurse practitioner
- PA
physician assistant
- STI
sexually transmitted infection
Footnotes
Conflicts of Interest: None declared.
References
- 1.Alexander SC, Fortenberry JD, Pollak KI, Bravender T, Davis JK, Ostbye T, Tulsky JA, Dolor RJ, Shields CG. Sexuality talk during adolescent health maintenance visits. JAMA Pediatr. 2014 Feb;168(2):163–9. doi: 10.1001/jamapediatrics.2013.4338. http://europepmc.org/abstract/MED/24378686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marcell AV, Bell DL, Lindberg LD, Takruri A. Prevalence of sexually transmitted infection/human immunodeficiency virus counseling services received by teen males, 1995-2002. J Adolesc Health. 2010 Jun;46(6):553–9. doi: 10.1016/j.jadohealth.2009.12.002. http://europepmc.org/abstract/MED/20472212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelts EA, Allan MJ, Klein JD. Where are we on teen sex?: Delivery of reproductive health services to adolescents by family physicians. Fam Med. 2001 May;33(5):376–81. [PubMed] [Google Scholar]
- 4.Blum RW, Beuhring T, Wunderlich M, Resnick MD. Don't ask, they won't tell: the quality of adolescent health screening in five practice settings. Am J Public Health. 1996 Dec;86(12):1767–72. doi: 10.2105/ajph.86.12.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jemmott JB, Jemmott LS, Fong GT, Morales KH. Effectiveness of an HIV/STD risk-reduction intervention for adolescents when implemented by community-based organizations: a cluster-randomized controlled trial. Am J Public Health. 2010 Apr;100(4):720–6. doi: 10.2105/AJPH.2008.140657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jemmott JB, Jemmott LS, O'Leary A, Ngwane Z, Icard LD, Bellamy SL, Jones SF, Landis JR, Heeren GA, Tyler JC, Makiwane MB. School-based randomized controlled trial of an HIV/STD risk-reduction intervention for South African adolescents. Arch Pediatr Adolesc Med. 2010 Oct;164(10):923–9. doi: 10.1001/archpediatrics.2010.176. http://europepmc.org/abstract/MED/20921349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW, Oh MK, Crosby RA, Hertzberg VS, Gordon AB, Hardin JW, Parker S, Robillard A. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. J Am Med Assoc. 2004 Jul 14;292(2):171–9. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- 8.Heeren GA, Jemmott JB, Ngwane Z, Mandeya A, Tyler JC. A randomized controlled pilot study of an HIV risk-reduction intervention for sub-Saharan African university students. AIDS Behav. 2013 Mar;17(3):1105–15. doi: 10.1007/s10461-011-0129-2. http://europepmc.org/abstract/MED/22246515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morrison-Beedy D, Jones SH, Xia Y, Tu X, Crean HF, Carey MP. Reducing sexual risk behavior in adolescent girls: results from a randomized controlled trial. J Adolesc Health. 2013 Mar;52(3):314–21. doi: 10.1016/j.jadohealth.2012.07.005. http://europepmc.org/abstract/MED/23299011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKee M, Fletcher J, Schechter CB. Predictors of timely initiation of gynecologic care among urban adolescent girls. J Adolesc Health. 2006 Aug;39(2):183–91. doi: 10.1016/j.jadohealth.2005.11.022. [DOI] [PubMed] [Google Scholar]
- 11.Hoopes AJ, Benson SK, Howard HB, Morrison DM, Ko LK, Shafii T. Adolescent perspectives on patient-provider sexual health communication: a qualitative study. J Prim Care Community Health. 2017 Oct;8(4):332–7. doi: 10.1177/2150131917730210. http://europepmc.org/abstract/MED/28929860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fairbrother G, Scheinmann R, Osthimer B, Dutton MJ, Newell KA, Fuld J, Klein JD. Factors that influence adolescent reports of counseling by physicians on risky behavior. J Adolesc Health. 2005 Dec;37(6):467–76. doi: 10.1016/j.jadohealth.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Gayes LA, Steele RG. A meta-analysis of motivational interviewing interventions for pediatric health behavior change. J Consult Clin Psychol. 2014 Jun;82(3):521–35. doi: 10.1037/a0035917. [DOI] [PubMed] [Google Scholar]
- 14.Brown RA, Abrantes AM, Minami H, Prince MA, Bloom EL, Apodaca TR, Strong DR, Picotte DM, Monti PM, MacPherson L, Matsko SV, Hunt JI Motivational Interviewing to Reduce Substance Use in Adolescents with Psychiatric Comorbidity. J Subst Abuse Treat. 2015;59:20–9. doi: 10.1016/j.jsat.2015.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stanger C, Ryan SR, Delhey LM, Thrailkill K, Li Z, Budney AJ. A multicomponent motivational intervention to improve adherence among adolescents with poorly controlled type 1 diabetes: a pilot study. J Pediatr Psychol. 2013 Jul;38(6):629–37. doi: 10.1093/jpepsy/jst032. http://europepmc.org/abstract/MED/23699750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gourlan M, Sarrazin P, Trouilloud D. Motivational interviewing as a way to promote physical activity in obese adolescents: a randomised-controlled trial using self-determination theory as an explanatory framework. Psychol Health. 2013 Nov;28(11):1265–86. doi: 10.1080/08870446.2013.800518. [DOI] [PubMed] [Google Scholar]
- 17.Walton M, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. J Am Med Assoc. 2010 Aug 4;304(5):527–35. doi: 10.1001/jama.2010.1066. http://europepmc.org/abstract/MED/20682932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunningham RM, Chermack ST, Zimmerman MA, Shope JT, Bingham CR, Blow FC, Walton MA. Brief motivational interviewing intervention for peer violence and alcohol use in teens: one-year follow-up. Pediatrics. 2012 Jun;129(6):1083–90. doi: 10.1542/peds.2011-3419. http://europepmc.org/abstract/MED/22614776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gold MA, Tzilos GK, Stein LA, Anderson BJ, Stein MD, Ryan CM, Zuckoff A, DiClemente C. A randomized controlled trial to compare computer-assisted motivational intervention with didactic educational counseling to reduce unprotected sex in female adolescents. J Pediatr Adolesc Gynecol. 2016 Feb;29(1):26–32. doi: 10.1016/j.jpag.2015.06.001. http://europepmc.org/abstract/MED/26514957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnet B, Liu J, DeVoe M, Duggan AK, Gold MA, Pecukonis E. Motivational intervention to reduce rapid subsequent births to adolescent mothers: a community-based randomized trial. Ann Fam Med. 2009;7(5):436–45. doi: 10.1370/afm.1014. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=19752472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McKee MD, Rubin SE, Campos G, O'Sullivan LF. Challenges of providing confidential care to adolescents in urban primary care: clinician perspectives. Ann Fam Med. 2011;9(1):37–43. doi: 10.1370/afm.1186. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=21242559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001 Jan;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 23.Olson AL, Gaffney CA, Hedberg VA, Gladstone GR. Use of inexpensive technology to enhance adolescent health screening and counseling. Arch Pediatr Adolesc Med. 2009 Feb;163(2):172–7. doi: 10.1001/archpediatrics.2008.533. [DOI] [PubMed] [Google Scholar]
- 24.Brown JD, Wissow LS. Discussion of sensitive health topics with youth during primary care visits: relationship to youth perceptions of care. J Adolesc Health. 2009 Jan;44(1):48–54. doi: 10.1016/j.jadohealth.2008.06.018. http://europepmc.org/abstract/MED/19101458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zieve GG, Richardson LP, Katzman K, Spielvogle H, Whitehouse S, McCarty CA. Adolescents' perspectives on personalized e-feedback in the context of health risk behavior screening for primary care: qualitative study. J Med Internet Res. 2017 Dec 20;19(7):e261. doi: 10.2196/jmir.7474. http://www.jmir.org/2017/7/e261/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goyal MK, Shea JA, Hayes KL, Badolato G, Chamberlain JM, Zaoutis T, Fein J. Development of a sexual health screening tool for adolescent emergency department patients. Acad Emerg Med. 2016 Dec;23(7):809–15. doi: 10.1111/acem.12994. doi: 10.1111/acem.12994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peipert J, Redding CA, Blume J, Allsworth JE, Iannuccillo K, Lozowski F, Mayer K, Morokoff PJ, Rossi JS. Design of a stage-matched intervention trial to increase dual method contraceptive use (Project PROTECT) Contemp Clin Trials. 2007 Sep;28(5):626–37. doi: 10.1016/j.cct.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 28.Peipert JF, Redding CA, Blume JD, Allsworth JE, Matteson KA, Lozowski F, Mayer KH, Morokoff PJ, Rossi JS. Tailored intervention to increase dual-contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. Am J Obstet Gynecol. 2008 Jun;198(6):630.e1–8. doi: 10.1016/j.ajog.2008.01.038. http://europepmc.org/abstract/MED/18395692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Downs JS, Murray PJ, de Bruin WB, Penrose J, Palmgren C, Fischhoff B. Interactive video behavioral intervention to reduce adolescent females' STD risk: a randomized controlled trial. Soc Sci Med. 2004 Oct;59(8):1561–72. doi: 10.1016/j.socscimed.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 30.DiClemente RJ, Wingood GM, Rose ES, Sales JM, Lang DL, Caliendo AM, Hardin JW, Crosby RA. Efficacy of sexually transmitted disease/human immunodeficiency virus sexual risk-reduction intervention for african american adolescent females seeking sexual health services: a randomized controlled trial. Arch Pediatr Adolesc Med. 2009 Dec;163(12):1112–21. doi: 10.1001/archpediatrics.2009.205. [DOI] [PubMed] [Google Scholar]
- 31.Mackenzie SL, Kurth AE, Spielberg F, Severynen A, Malotte CK, St Lawrence J, Fortenberry JD. Patient and staff perspectives on the use of a computer counseling tool for HIV and sexually transmitted infection risk reduction. J Adolesc Health. 2007 Jun;40(6):572.e9–16. doi: 10.1016/j.jadohealth.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 32.Paul CL, Carey M, Yoong SL, D'Este C, Makeham M, Henskens F. Access to chronic disease care in general practice: the acceptability of implementing systematic waiting-room screening using computer-based patient-reported risk status. Br J Gen Pract. 2013 Sep;63(614):e620–6. doi: 10.3399/bjgp13X671605. http://bjgp.org/cgi/pmidlookup?view=long&pmid=23998842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahmad F, Skinner HA, Stewart DE, Levinson W. Perspectives of family physicians on computer-assisted health-risk assessments. J Med Internet Res. 2010 May 7;12(2):e12. doi: 10.2196/jmir.1260. http://www.jmir.org/2010/2/e12/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rollnick S, Miller WR. What is motivational interviewing? Behav Cogn Psychother. 2009 Jun 16;23(4):325–34. doi: 10.1017/S135246580001643X. [DOI] [PubMed] [Google Scholar]
- 35.Coleman E. Sexual health education in medical school: a comprehensive curriculum. Virtual Mentor. 2014 Nov 1;16(11):903–8. doi: 10.1001/virtualmentor.2014.16.11.medu1-1411. [DOI] [PubMed] [Google Scholar]
- 36.Bayer CR, Eckstrand KL, Knudson G, Koehler J, Leibowitz S, Tsai P, Feldman JL. Sexual health competencies for undergraduate medical education in North America. J Sex Med. 2017 Dec;14(4):535–40. doi: 10.1016/j.jsxm.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 37.Galletly C, Lechuga J, Layde JB, Pinkerton S. Sexual health curricula in U.S. medical schools: current educational objectives. Acad Psychiatry. 2010;34(5):333–8. doi: 10.1176/appi.ap.34.5.333. [DOI] [PubMed] [Google Scholar]
- 38.Poirier MK, Clark MM, Cerhan JH, Pruthi S, Geda YE, Dale LC. Teaching motivational interviewing to first-year medical students to improve counseling skills in health behavior change. Mayo Clin Proc. 2004 Mar;79(3):327–31. doi: 10.4065/79.3.327. [DOI] [PubMed] [Google Scholar]
- 39.Haeseler F, Fortin AH, Pfeiffer C, Walters C, Martino S. Assessment of a motivational interviewing curriculum for year 3 medical students using a standardized patient case. Patient Educ Couns. 2011 Jul;84(1):27–30. doi: 10.1016/j.pec.2010.10.029. https://linkinghub.elsevier.com/retrieve/pii/S0738-3991(10)00637-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.White LL, Gazewood JD, Mounsey AL. Teaching students behavior change skills: description and assessment of a new Motivational interviewing curriculum. Med Teach. 2007 May;29(4):e67–71. doi: 10.1080/01421590601032443. [DOI] [PubMed] [Google Scholar]
- 41.Henry-Reid LM, O'Connor KG, Klein JD, Cooper E, Flynn P, Futterman DC. Current pediatrician practices in identifying high-risk behaviors of adolescents. Pediatrics. 2010;125(4):e741–7. doi: 10.1542/peds.2009-0271. http://illinoisaap.org/wp-content/uploads/peds-2010.pdf. [DOI] [PubMed] [Google Scholar]
- 42.Henderson JT, Raine T, Schalet A, Blum M, Harper CC. "I wouldn't be this firm if I didn't care": preventive clinical counseling for reproductive health. Patient Educ Couns. 2011 Feb;82(2):254–9. doi: 10.1016/j.pec.2010.05.015. http://europepmc.org/abstract/MED/20558024. [DOI] [PMC free article] [PubMed] [Google Scholar]


